Reduction in medical error rates when implementing a 48h EWTD-compliant rota
advertisement
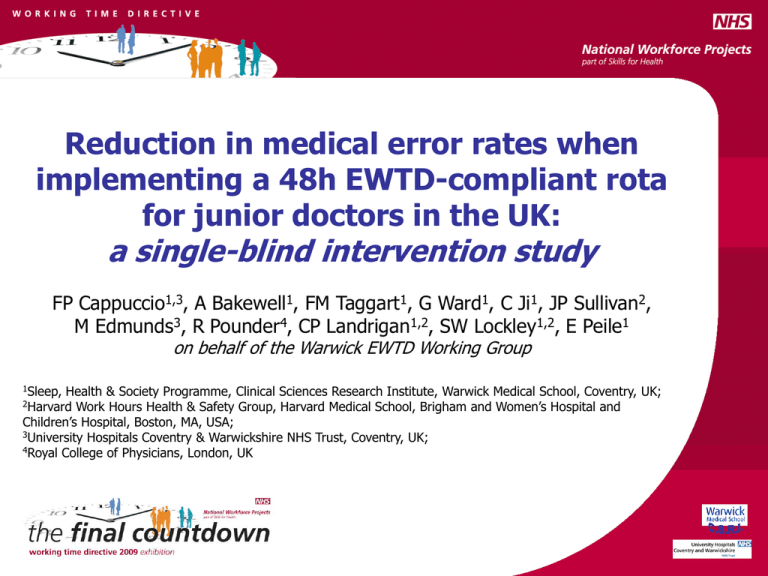
Reduction in medical error rates when implementing a 48h EWTD-compliant rota for junior doctors in the UK: a single-blind intervention study FP Cappuccio1,3, A Bakewell1, FM Taggart1, G Ward1, C Ji1, JP Sullivan2, M Edmunds3, R Pounder4, CP Landrigan1,2, SW Lockley1,2, E Peile1 on behalf of the Warwick EWTD Working Group 1Sleep, Health & Society Programme, Clinical Sciences Research Institute, Warwick Medical School, Coventry, UK; Work Hours Health & Safety Group, Harvard Medical School, Brigham and Women’s Hospital and Children’s Hospital, Boston, MA, USA; 3University Hospitals Coventry & Warwickshire NHS Trust, Coventry, UK; 4Royal College of Physicians, London, UK 2Harvard Background (1) • • • • • • • 1993 EWTD: limiting the maximum required working hours to 48/wk (average over up to 6 mo) to protect employees’ health and safety and improve patient safety 1998: adopted into UK law through the Working Time Regulations Extension up to 12 yrs before full implementation 2003 European Court ruling: resting and sleeping time during duty in hospital should be considered as working time Aug 2005: Changes affecting medical profession phased over 5 years (junior doctors’ six-monthly average weekly working hours reduced from 72 to 54) The New Deal: BMA negotiations with DoH to improve lives of junior doctors – key feature to reduce extended working hours and ensure adequate rest was built in rotas Aug 2009: EWTD-compliant rotas must be in place Background (2) 2004: UK Multidisciplinary Working Group of the Royal College of Physicians established to: – – develop practical advice for junior doctors working night shifts guide those designing rotas for junior doctors 2006 Recommendations of the UK EWTD WP of the RCP i. ii. iii. iv. v. Rotas involving seven consecutive 13h night shifts may increase risks to patients and staff, and should be avoided Number of night shifts in succession should be limited to a maximum of four, and their length reduced Encouraged to testing of three 9h shifts to cover 24h to achieve improved health, safety, teaching and supervision, and efficiency. Using an evidence-based approach, hospitals should implement optimal 48h rotas by 2009 A ‘cell’ of 10 junior doctors is necessary for any post that provides 24h cover, plus specialty work and training Need to implement EWTD competes with demands to – – – – maintain medical cover at all times provide safe and effective healthcare to patients ensure doctors access educational and training opportunities ensure safety and quality of life of doctors Background (3) • Considerable controversy – Concerns raised about – • Doctors’ and patients’ lives at risk (BMJ 2005;330:1404) • Reduced time available for training, with negative impact on clinical experience and quality of care (BMJ 2007;334:777. BMJ 2008;336:345. Clin Med 2008;8:126-7) Without exceptions, assertions based on opinions, anecdotes or non validated questionnaires (Occup Environ Med 2007;64:733-8. Ann R Coll Surg Engl 2008;90:60-3 and 68-70. BMA 2008) • Evidence – Studies in the US show that a reduction in total hours worked in a week and in the duration of each shift results in • • • • • More sleep (i.e. less fatigue) Fewer attentional failure Fewer serious medical errors Fewer car crashes when doctors’ driving home after a shift Fewer sharp injuries (NEJM 2004;351:1829-37 and 1838-48. NEJM 2005;352:125-34. JAMA 2006;296:1055-62. PLoS Med 2006;3:e487) No objective evidence in the UK and Europe Aims of our study • To study the effects of implementing an EWTD-compliant 48h week rota on – – – – Patients’ safety Doctors’ work-sleep patterns Quality of life and well-being Quality of handover • Comparing the effects of an EWTD compliant 9h shift system versus a traditional rota for junior doctors at UHCW Methods (1) - Study period and design • 7th May – 31st July 2007 (12 weeks) – MTAS time!!! • 12-week single-blind intervention trial – Intervention group (9h shift system=48h/wk) – Traditional Group (traditional shift system=56h/wk) • Intervention group (n=9) – CDU and Endocrinology • Traditional group (n=10) – Respiratory and Care of the Elderly • Rota adjustment after 6 weeks (to increase day-time cover and extend night shift from 9h to a max of 11h) Methods (2): examples of junior doctor work and sleep patterns Day of week Subject #1 12:00 18:00 M T W T F S S M T W T F S S Subject #2 Day of week Clock time (h) 6:00 Subject #3 Clock time (h) 6:00 12:00 18:00 6:00 12:00 18:00 M T W T F S S M T W T F S S 6:00 12:00 18:00 Subject #4 M T W T F S S M T W T F S S M T W T F S S M T W T F S S Traditional 56-h rota Intervention 48-h rota Self-reported sleep times () and work hours () are shown for four junior doctors while working on either a 56-hour schedule (Subjects 1 and 2, left panels) or a 48hour schedule (Subjects 3 and 4, right panels). Methods (3) • Retrospective manual case note review Random selection 916 case notes out of 1677 admissions (55%) Episode of care >24 hours Institute for Healthcare Improvement Global Trigger Tool Trigger words e.g. confusion, warfarin, hypotension Clinical Adverse Event forms Incident identified - descriptive information collected Incidents submitted to physician review (2 or 3) Reviewers blind to allocated rota Error classification Error type • Statistical analysis Error rate per 1,000 patient-days Intervention effect by intention-to-treat analysis Hazard ratios Methods (4) - Incidents detected Preventable Adverse Event On warfarin, INR not monitored bled Intercepted Potential Adverse Event Prescribed contraindicated drugs (pharmacy note) Non-intercepted Potential Adverse Event Drug allergy not recorded on prescription chart (but not prescribed during stay) Minor error Blood tests not repeated as planned (but improved) Results (2) - Distribution of scheduled weekly work hours across 12 weeks by group 52.411.2 vs 43.27.7 h/week; p<0.001 Percentage of Scheduled Work Weeks 50 48 hr 56 hr 40 30 25% >58h 20 2% >58h 10 0 <28 28<38 38<48 48<58 58<68 Duration of Scheduled Work Week (hr) 10 56 hr rotas x 12 weeks 9 48 hr rotas x 12 weeks 100 68<78 Range: 26 to 60 h/week Range: 30 to 77 h/week Percentage of Scheduled Work Percentage of Scheduled Work 30 20 10 0 60 40 Results (3) – Distribution of work shift duration 20 Scheduled (n=19) <28 28<38 38<48 work 48<58 58<68 68<78 0 Duration of Scheduled Work Week 9.0 0.8 h [3.0 to 11.0; n=5](hr) vs 10 56 hr rotas x 12 weeks 9.91.8 h [4.5 to 12.5; n=4] 9 48 hr rotas x 12 weeks 48 hr 56 hr 60 25% >12h 40 Nil >12h 0 p<0.001 48 hr 56 hr 80 60 40 20 0 <10 10<12 >12 <10 Duration of Scheduled Work Shift (hr) 633 56 hr shifts, 520 48 hr shifts 10<12 >12 Duration of Self-Reported Work Shift (hr) 134 56 hr shifts, 114 48 hr shifts 100 80 Percentage of Self-Reported Work Shifts Percentage of Scheduled Work Shifts 9.20.8 h [5.5 to 11.5] vs 100 80 20 Self-reported work (n=9) <10 10<12 >12 Duration of Scheduled Work Shift (hr) 9.91.9 h [3.0 to 13.0] 633 56 hr shifts, 520 48 hr shifts p<0.001 100 d Work Shifts 48 hr 56 hr 80 48 hr 56 hr Results (4) - Comparison of average duration of sleep after each shift type during the two rotas Intervention rota Traditional rota 7.260.36h* 6.750.40h 8.68h 6.93h 6.28h 5.69h *p=0.095 vs traditional Results (5) - Wards’ characteristics Age P<0.001 100 90 Hospital stay P<0.001 35 70 30 60 Length on Study 25 40 P<0.001 20 25 15 Elderly (C) Respiratory (C) Endocrine (I) 20 10 5 Clinical Decisions Unit (I) Ward 15 0 Elderly (C) Days 50 Days Years 80 10 Respiratory (C) Endocrine (I) Clinical Decisions Unit (I) Ward 5 0 Elderly (C) Respiratory (C) Endocrine (I) Ward Clinical Decisions Unit (I) Results (6) - Characteristics of patients and episodes Traditional Intervention p-value Respiratory Endocrinology Admissions (n) 248 233 Patients (n) 244 230 71 (27) 71 (31) 0.14 10 (9) 9 (13) 0.37 7 (7) 7 (10) 0.61 Death Rate - n (%) 34 (13.7) 38 (16.3) 0.43 Death Rate (age adj.) - n (%) 34 (14.2) 38 (15.8) 0.62 Age (years) - median (IQR) Patient-days in hospital - median (IQR) Patient-days on study ward median (IQR) Results (7) -Adverse events and error rates between Traditional and Intervention rotas Traditional Intervention Respiratory Endocrinology Patient-days 2,315 2,467 Preventable Adverse Events n (rate*) 5 (2.2) 4 (1.6) HR: 0.63 (0.42 to 0.94) 16 (6.9) 3 (1.2) Intercepted Potential Adverse Events n (rate) HR: 0.16 (0.05 to 0.57) Non-Intercepted Potential Adverse Events n (rate) Minor Errors n (rate) Overall n (rate) Rate reduction % (95% C.I.)† p -27.3 (-85.1 to 249) 0.68 -82.6 (-97.7 to -38.5) 0.002 56 (24.2) 41 (16.6) -31.4 (-55.2 to 4.6) 0.067 18 (7.8) 20 (8.1) 3.8 (-52.2 to 91.0) 0.90 95 (41.0) 68 (27.6) -32.7 (-52.9 to -10.4) 0.006 HR: 0.62 (0.45 to 0.84) †: rate reduction = (rate of Endocrine – rate of Respiratory) * 100 / rate of Respiratory. *: rate is expressed as Number (per 1000 patient-days) Results (8) – Qualitative analysis • Workload issues and Perception of Patient Safety – Reduced day-time cover with potential for delay in investigations and treatments – Lack of time for team interaction • Learning opportunities – Drs in intervention felt educational opportunities were compromised • Rest and Sleep – Pro: less tired and performing better – Con: felt performing worse due to higher workload, though less tired • Quality of Life – Shifts at night and w/end impact negatively (irrespective of rotas) • Handover – Few concerns about quality – Several comments about number and timing (potential for missing things) Summary • • • First intervention study in the UK and Europe on the effects of a 48h/wk EWTDcompliant rota on patient care, as assessed objectively from medical error rates The results show that – 33% fewer medical errors occurred on the 48h/wk intervention rota – the new rota dramatically reduced the proportion of long work weeks – the experimental sequence facilitated sleep by providing opportunity for a long recovery sleep after the evening shift prior to starting the first night shift – implementation of a 48h work week can be accomplished without adverse effects of patients’ safety Limitations – Only tested in medical wards (generalisability > controlled studies needed) – Comparability of wards (case-mix and likelihood of medical errors) – Not designed to assess the impact on educational opportunities (need for validated educational outcomes) Conclusions • Patient care can be safely provided on a 2009 EWTD-compliant rota • Although our findings may not be directly applicable to all specialties, they do not indicate that a reduction in work hours inevitably leads to a reduction in the quality of patient care • There is a need for a wider re-engineering of shift systems and hospital processes to ensure that the safety gains for patients cared for by less tired doctors are not compromised by difficulties in managing the routine daytime workload • Evidence-based policy decisions must be made for work hours in the same way as evidence-based medicine is used for clinical decisions • Concerns remain regarding reduced educational opportunities. More objective research is needed around these areas