Modelling muscles in vitro: a finite element analysis study. University College London CoMPLEX
advertisement

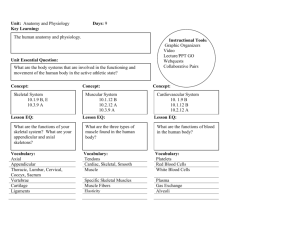
University College London CoMPLEX Mini Project 2 Modelling muscles in vitro: a finite element analysis study. Supervisors: Prof. Vivek Mudera Dr. Ryo Torii Author: David Hodgson March 6, 2015 Abstract The interaction between cells and the polymer chain constituents within a hydrogel has been extensively studied in the last few decades, including the rheological, chemical and biological properties of the physical gel and also the migration and alignment of the cells suspended within them. These studies have become especially relevant in the field of tissue engineering due to physiological similarities between the alignment and structure of cells within the contractive state of collagen hydrogels and the cellular structure of skeletal muscle tissue. Thus over the last decade there has been extensive experimental research into collagen hydrogels with muscle derived cells (MDCs) suspended within them with the aim of finding contractile constructs which have similar biological and physical properties as human skeletal muscle. Demonstrated in this project is a novel approach to this field of research using quantitive knowledge derived from previous biological experimentation and implementation of it into a finite element model to make predictions in silico about the deformed structure of collagen gels, and the migration and alignment of the MDCs suspended within them. Using this finite element method it has been shown that the model predicts with great accuracy the contractile shape of two hydrogels that have already been studied in vitro with different geometrical set ups. By also analysing the lines of principle strain within these constructs it is also possible to make predictions about the alignment and migration of MDCs over a seven day period. Contents 1 Introduction and Biological Background. 1.1 Motivation and Project Outline. . . . . . . . . . . . . . 1.2 Biological Background. . . . . . . . . . . . . . . . . . . . 1.2.1 Skeletal Muscle Physiology. . . . . . . . . . . . . 1.2.2 Mechanisms of self-repair within skeletal muscle. 1.2.3 Surgical methods of repair of skeletal muscle. . . 1.3 Skeletal muscular tissue engineering. . . . . . . . . . . . . . . . . . 2 2 2 2 3 3 4 . . . . . . . 4 4 5 5 5 6 6 6 . . . . . . . . . . . 6 6 6 7 7 7 7 8 8 10 10 11 4 Results. 4.1 Cuboidal Model. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4.2 Circular Model. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11 11 14 5 Discussions and Conclusion 5.1 Summary. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5.2 Limitations and Further Work. . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5.3 Conclusion. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18 18 18 19 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2 Experimental Procedure - Materials and Methods 2.1 Introduction. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.2 Cuboidal 3D Constructs. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.2.1 Cell Culture. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.2.2 Establishment and maintenance of MDC seeded cuboidal constructs. 2.3 Circular 3D Constructs. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.3.1 Cell Culture. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.3.2 Establishment and maintenance of C2C12 seeded circular constructs. 3 Mathematical Modelling. 3.1 Introduction. . . . . . . . . . . . . . . . . . 3.2 Meshing. . . . . . . . . . . . . . . . . . . . . 3.3 Finite Element Model Setup. . . . . . . . . 3.3.1 Material Properties. . . . . . . . . . 3.3.2 Solid Elements. . . . . . . . . . . . . 3.3.3 Contractile Elements. . . . . . . . . 3.4 Cell contraction. . . . . . . . . . . . . . . . 3.4.1 Quantifying cell-matrix interaction. . 3.5 Agent Based Modelling. . . . . . . . . . . . 3.5.1 Cell Alignment. . . . . . . . . . . . . 3.5.2 Cell Migration. . . . . . . . . . . . . 1 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1 1.1 Introduction and Biological Background. Motivation and Project Outline. Skeletal muscle, also called striated muscle, is used to move the skeleton. Skeletal muscles are under the control of the somatic nervous system and can produce contractions ranging from quick twitches to sustained tension. Inherited myopathies, such as muscular dystrophy, are owing to defects in skeletal muscle proteins, thus causing damage to skeletal muscle tissue. The derogatory effects on patients who suffer from muscular dystrophy can include life-long weakness, difficulty respiring and even atrophy [5]. Other conditions such as traumatic injury and tumour ablation can also result in permanent damage to skeletal muscle tissue which can result in loss of mass and consequently function [2]. This functional loss occurs due to lack of availability of native tissue; thus the regeneration of such muscle tissues, in vivo and in vitro such that it can be used to substitute lost skeletal muscle, has been one of the ultimate goals of tissue engineering in the last few decades. In the following project, a brief introduction to skeletal muscle physiology is first introduced, followed by a brief literature review on modern methods of engineering muscular tissue using collagen hydrogels. In Section 2 descriptions of the geometries of two constructs to be modelled in silico are given as well as a brief description of the methods and techniques used to establish the cellularised collagen hydrogels in vitro. Section 3 gives a detailed introduction to the method of finite element modelling (FEM), explaining the process of finite element modelling, the use of ANSYS and Mathemetica as an agent based modeller, and the justification of the parameters and variables used in the derived models. The results of these simulations and comparison to their in vitro counterparts are displayed in Section 4. A discussion of the results, limitations of the model and ideas for further work are featured in the final section. 1.2 1.2.1 Biological Background. Skeletal Muscle Physiology. Myoblasts are embryonic progenitor cells which can fuse together in a process called myogenesis, resulting in multinucleated, cylindrical cells called muscle fibres (or myocytes) which is act as a major constituent of muscle tissue. Each muscle fibre contains myofibrils which run along the length of the cell and are formed of highly organised bands of myosin and actin called sarcomeres which act as the contractile unit of the cell giving muscles to ability to produce force and motion. Muscle fibres are grouped together by a sheath of connective tissue called the perimysium to form bundles of muscles fibres called fascicles. Fascicles are grouped together further to form muscle tissue which is enclosed in a sheath called the epimysium. The muscle tissue is then attached to the skeletal frame by collagen based fibres called tendons. This complex hierarchal structure is shown in Figure. 1.1. 2 The extracellular matrix (ECM) of muscle fibres plays an essential role in the alignment and differentiation of myoblasts [7, 3]. In vivo, the extracellular matrix of muscle fibres is aligned in an uniaxial manner which consequently promotes muscles to grow in a long linear fashion [4]. Therefore in order to engineer muscle tissue, a tissue culture must be constructed with a scaffold which is similar in geometry and structure to the ECM in vivo. Collagen is a main constituent of the ECM, therefore from the prospective of a tissue engineer, collagen-based hydrogels are a logical medium in which to attempt to grow skeletal Figure 1.1: Artist’s representation of the hierarmuscle [22]. chal structure of muscle tissue. 1.2.2 Mechanisms of self-repair within skeletal muscle. Within the extracellular matrix of skeletal muscle cells there exists a specilized myoblast subpopulation in the basal lamina of myofibres called satellite cells. These remain quiescent until damage occurs to the muscle cell, at which point they proliferate and fuse to damaged muscle cells as a mechanism of self-repair [6, 8]. Applying such damage over regular periods of time to muscle cells can thus increase muscle mass over time. However, when significant damage occurs to tissue, either from extreme traumatic injury or from aggressive myopathies, the local self-repair mechanism of satellite cells is not sufficient and thus external therapies must be utilised in order to regain muscle mass. 1.2.3 Surgical methods of repair of skeletal muscle. Free autologous tissue transfer is a surgical procedure whereby functional and aesthetic restoration of lost muscle is achieved by transferring muscle from a donor site to an area of significant muscle loss. This surgical intervention have shown limited success in attempts to restore normal function, but they are not perfect solutions [1], also the surgery results in significant donor site morbidity causing functional loss and volume deficit. As a result, the emergence of tissue engineering has presented a potential alternative form of treatment; where grown tissue substitutes are used for functional reconstruction of skeletal muscle tissue. 3 1.3 Skeletal muscular tissue engineering. The ultimate goal in the tissue growth of skeletal muscle is to be able to grow, in vitro, with consistency and ease, mature artificial muscle which have the morphology, ultrastructure and level of differentiation found in an adult cell. Vanderburgh’s work [21] put forward the first 3D cultivated contracting skeletal muscle tissue in vitro. Here, avian myotubes where embedded in a collagen gel matrix attached to a nylon support structure. This allowed the cells to be in a contractile state for up to three times longer than in previous 2D models and the structural integrity of the myotubes remained sound for this time. This collagen gel technique has been further developed papers in the following decades [19, 10, 17]. It has been shown the parallel orientation of muscle fibres guarantees the generation of longitudinal force after a contraction that is induced by motorneuron activity [1]. It has also been shown that the composition of the extracellular matrix plays an essential role in alignment and differentiation of myoblasts [7, 3], thus it became of natural interest to study the interaction between myoblasts and the collagen matrix in which it is suspended. Eastwood provided a quantitive method of measuring the contractile force within a collagen hydrogel between a single cell and the collagen lattice itself. This was done via a complex mechanisms called a culture force monitor (CFM), which provides quantitive values that can be analysed to find the forces generated by the suspended cells in a gel [13]. These CFMs became a popular tool for analysing cell-collagen interactions within hydrogels in the following decade [9], however, the intricate, meticulous nature and difficulty of use of engineered CFMs means that reproducibility of forces documented in other labs was difficult. It was noticed in later work that setting a cell seeded collagen hydrogel between two fixed points leads to a parallel arrangement of collagen along the lines of principle strain, and thus parallel arrangement of muscle fibres [12]. This lead to an optimised method of growing aligned myotubes in 3D culture [20]. 2 2.1 Experimental Procedure - Materials and Methods Introduction. In what follows; two MDC seeded 3D constructs with varying geometry will be analysed. One is the cuboidal structure (Figure 2.1a), with dimensions 30mm x 20mm x 12mm as observed in [20] whose lines of principal strain have already been well studied [12] - this will act a control for which the accuracy of the newly presented Finite element model can be compared. Once convinced of said models accuracy, a circular geometric arrangement (with radius 8.5mm) with two fixed points will be considered (Figure 2.1b) and further analysis will continue. 4 Cuboidal Construct (m3 ) 0.010 0.005 0.020 0.000 0.00 0.015 0.010 0.01 0.005 0.02 0.03 0.000 (a) Cuboidal Construct - Natural View. (b) Circular Construct - Natural View. Figure 2.1: Graphical interpretation of the two types of construct geometries that will be analysed. Here the Translucent red represents to cellulised collagen hydrogel and the grey represents fixed points in the gel. Both gels have been produced by different methods, the protocol for maintaining the cell cultures and the establishment of the seeded constructs for each geometry are outlined below. 2.2 Cuboidal 3D Constructs. The full protocol for construction of cellulised collagen gels is stated in detail elsewhere [20]. A brief explanation is provided in this section. 2.2.1 Cell Culture. Primary rat MDCs were isolated from skeletal muscle samples from one day old rats. The cells were suspended in growth media consisting of 20% fetal calf serum (FCS) (PAA, Somerset, UK), 1% penicillin (100U/ml) and streptomycin (100mg/ml) (P/S) in high glucose DMEM (GIBCO/Invitrogen). The cell number was calculated to be 5 × 106 MDCs/cm3 using a hemocytometer. 2.2.2 Establishment and maintenance of MDC seeded cuboidal constructs. For a 3ml collagen gel 300µl of 10x MEM solution was added to 2.6ml of 2.035mg/ml type 1 rat-tail collagen in 0.1M acetic acid (First Link, Birmingham, UK, )and mixed thoroughly. The solution was neutrilised with 5 M NaOH drop wise until a colour change was observed and then was mixed with a suspension of MDCs in 300µl GM. The solution was then pipetted into a single well chamber slide which had floatation bars at each end (Figure 2.1a). The chambers where placed in a humidified incubator at 37 degrees for 30 minutes to allow collagen to set. Once set, the collagen construct was detached from the base of the mould and 5 floated in GM at 37 degrees which was changed daily for a period of 14 days. 2.3 2.3.1 Circular 3D Constructs. Cell Culture. Skeletal muscle cells used were cells C2C12 from CH3 mice (Cell Bank, Surrey). The cells were incubated at 37% until 50%-60% confluent before being suspended in growth medium with 25ml DMEM (Gibco Life Technologies, USA) with a either 10% or 2% FCS. The cell number was calculated to be 4 × 106 cells/ml using a hemocytometer. 2.3.2 Establishment and maintenance of C2C12 seeded circular constructs. For a 5ml collagen gel, 0.5ml of 10x MEM solution (Gibco, Life Technologies, USA) was added to 4ml of 2.05 mg/ml Type I collagen in 0.6% Acetic acid (First Link, UK), and mixed thoroughly. The solution was neutralised with 5 M and 1 M NaOH drop wise until a colour change was observed and then was mixed with a suspension of cells in 0.5ml GM. The solution was then placed into a circular well with two fixation points at each end (Figure 2.1b). The chambers where placed in a humidified incubator at 37 degrees for 15 minutes to allow the collagen to set, at which point the addition of media is added with 10% FCS was added. After 24 hours the media was dropped to 2% FCS to enable differentiation; and was changed on alternate days until the experiments are terminated (up to 14 days.) 3 3.1 Mathematical Modelling. Introduction. Finite Element methods are numerical methods used for approximating the solutions to mathematical models. This is done by subdividing (meshing) the problem into simpler parts (or finite elements) and solving the problem by minimising an associated error function. It is a common technique used by engineers and physicists to try and understand the behaviour of structural geometries when certain pressures and forces are applied to them. Due to it’s versatility in both geometric construction and in force and pressure specification, it is possible to use this method to understand the interactions of cellular materials with collagen matrices. 3.2 Meshing. Mathematical models will be devised for the two geometries described above; the cuboidal and circular fixed point arrangements. For the former, the cuboidal volume was meshed with uniform hexahedral elements of size 1mm x 1mm x 1mm. This resulted in 7200 hexahedral elements based on 8463 nodes (Figure 3.1a). The circular model followed a similar arrangement, again meshing the cylindrical volume with hexahedral elements but this time of size 0.5mm x 0.5mm 6 x 0.5mm. This resulted in 7056 hexahedral elements based on 7336 nodes (Figure 3.1b). The reason for the uniform homogeneity of the meshing is to due to the assumption that the cells are distributed even within the hydrogel, thus contraction is initially constant across the whole volume. (a) Cuboidal mesh. (b) Circular mesh. Figure 3.1: The resulting mesh of the two geometries to be considered. Image generated by ANSYS. 3.3 Finite Element Model Setup. To produce the meshes above and for all the Finite Element Modelling which follows, the Static Structural analysis system of the finite element solver, ANSYS Mechanical APDL, was used. This produced and solved all of the following results. 3.3.1 Material Properties. In order to analyse the cellular interactions with the collagen gel, certain characteristic parameters of the collagen gel must defined. In the cuboidal model and the circular model, the initial Young’s modulus once the gel had set was set to 100KPa [14, 15], the density 1100kg/m3 from experimental observations and due to the fact that the gels are around 99% water, a poison ratio of 0.45 was chosen. 3.3.2 Solid Elements. The hexahedral 3D solid elements - SOLID185 - are isoparametrc and have three degrees of translational freedom. Each uniform hexahedral element that results from the mesh will be modelled by this ANSYS element, thus are used represent the main body of collagen material. Initially they are all cubes but as they deform over time they will distort into irregular hexahedral elements. 3.3.3 Contractile Elements. 7 In order to mimic the contractile forces within the collagen gels, an inner contraction force must be defined uniformly throughout the collage lattice. In order to do this the LINK10 element is used, which is a three dimensional spar element which has only uniaxial tension. These elements can be defined such that they have an initial strain which results in a contractile force acting uniaxially. This element will be defined on every edge of every hexahedral element throughout the model Figure 3.2: Example of element forces 3.2, thus resulting in a uniform inner contractile force used to mimic contractile collagen gel. throughout the entirety of the meshed solid, thus deThe SOLID185 element is shown in it’s forming each 3D SOLID185 element. initial cuboidal state and the LINK10 element is shown to be defined on it’s 3.4 Cell contraction. edge. 3.4.1 Quantifying cell-matrix interaction. The study of cellular interactions with collagen gels is long established due to it’s physiological relevance. Through various experimentation and analysis some useful properties have been defined. The major aim of this modelling is to analyse the migration and alignment of MDCs suspended in the collagen gel over a time period. Thus a relation must be found between the forces projected by the cell-matrix interaction and the initial strain of the LINK10 spar element in the finite element model. It is useful to remind ourself that the force exerted by LINK10 can be described as thus; F = AE (1) where F is the force produced by the element, A is the cross sectional area of the element over which the compression occurs, E is Young’s modulus, and is the initial deformation of the spar element. In the cuboidal model, the area, A, is defined to be 10−6 m2 for all elements inside the gel as to encapsulate all the material around it, and 5 × 10−7 m2 on elements along the edges as only one side of the spar has the relevant material. Similarly, in the circular model A is defined to be 2.5 × 10−7 for elements within the gel and 1.25 × 10−7 for elements surrounding the edge. Reminding ourselves of the preparation of the constructs; the cuboidal gel was seeded with 5 × 106 cells/ml and the circular gel was seeded with 4 × 106 cells/ml. Assuming a homogenous distribution, this implies that in the cuboidal model that each element (1mm3 ) has around 5000 cells on average and each element in the circular mesh (0.125mm3 ) has around 500 cell on average. Having calculated the number of cells in each element it would be of great use to find the contractive force exerted on each hexahedral element in the two meshes. Many studies using 8 the CFM have attempted to quantity the force exerted between a single cell and a collagen matrix. Results range from 10−8 to 10−10 N [13, 16, 11]. It is difficult to determine what region is accurate but as to not gain any extreme values, an arbitrary mid-point from these ranges, 10−9 N is chosen. Thus for the cuboidal construct, for each hexahedral element a contractile force of 5 × 10−6 N is emitted, which can be related to the initial strain on a LINK10 element by (1), thus the strain is 5 × 10−5 N on inner links and 10−4 N on outer links. Similar for the circular construct a contractile force of 5 × 10−7 N is emitted, which is equivalent to a initial strain of 2 × 10−5 N for inner elements and 4 × 10−5 N for edge elements. Thus applying this initial strain to every LINK10 in the model, ANSYS can be used to find the deformation and principal strains that emerge in that configuration. Assuming that cells produce this force every second, once the initial deformation geometry has been established, the initial strain can be applied again to every LINK10 element and a further deformed model can be analysed. Repeating and applying this process so as to make up a total of 1 day, the contour plots of the deformation are shown in Figure.3.3 and also, contour plots of the lines of Maximum principal strain (Figure.3.4). (b) Circular deformation. (a) Cuboidal deformation. Figure 3.3: Contour plots of the deformation of the nodal points after 1 day. Image generated by ANSYS. 9 (b) Circular strain. (a) Cuboidal strain. Figure 3.4: Contour plots of the deformation of the nodal points after 1 day. Image generated by ANSYS. 3.5 Agent Based Modelling. Once information such as the lines of principal strain and deformation have been computed in ANSYS for the time equivalent to one day, the information was then extracted and analysed using Mathematica to model to movement of 1000 randomly distributed cells over a one day period. In it well established in literature that in a strained collagen gel, cells which are suspended will align along the direction of maximum principal strain [12]. Also, cells migrate along the maximum principle strain axis [18] and tend to move to area of lower strain more quickly, that is they prefer a stiffer environment [15]. In [18] it is also established that when a collagen gel is deformed by a planar strain of 0.2, cells can move up to move at a rate of 455µm a day with an error of ±72µm. They also tend to move along the axis of maximum principal strain but with some variation of angle. In the deformation contour plots in Figure 3.3 one notices a after 24 hours the maximum deformation is around 470µm in the cuboidal construct and 672µm in the circular construct, thus the cell migration speed of the cells will be set to be what was observed in [18] for the cuboidal construct and for the circular construct it will be set to rate scaled 1.5 times this; 682.5µm a day with an error of ±108µm 3.5.1 Cell Alignment. Cells will be modelled as massless particles, as cell alignment is a geometric quality of the cell, it is thus difficult to quantify in our model. Therefore particles will be modelled as vectors of a small length, and the the direction of the vector will be defined such that it is parallel to the axis of maximal principal strain at the node nearest to it. Assuming that cells are initially spherical upon initial suspension in a gel, then this vector can be interpreted as the major axis 10 of the ellipsoid that would form in response to the cell alignment with the collagen matrix. 3.5.2 Cell Migration. In order to model the stochastic behaviour of the cells, they will assume to move according to a random walk method. Each day, each cell will jump a distance following a random walk which follows Gaussian distribution along the maximum principle axis of strain of the nearest node. In the cuboidal model the distribution is given by N (455µm, 36µm) and in the circular construct it is given by N (682µm, 54µm). The simulation is run for then 7 days and the final positions and alignment of the cells are then plotted. 4 Results. Pairing ANSYS and the agent based modelling, the following results are produced for the circular and cuboidal constructs. 4.1 Cuboidal Model. (a) Day 1. (b) Day 4. (c) Day 7. Figure 4.1: ANSYS images showing the deformation of the cellulised collagen gel after 1, 4 and 7 days. Figure 4.1 shows the bowing pattern observed in various papers that have previously studied such cuboidal geometries. Figure 4.2 similarly shows the position of the nodal points which define the mesh over time. The contractile action of the collagen can clearly be observed. 11 (a) Initial Configuration. (b) Day 4. (c) Day 7. Figure 4.2: Point plot of the nodal points after 1, 4 and 7 days. Consruct Area mm2 Attempts at quantifying the cuboidal conContraction of collagen gel 600 traction for collagen constructs in vitro was performed in [20], whereby the arial 2D sur400 face of the cuboidal was analysed over time. In Silico A similar calculation with our in silico model In Vitro 200 is also performed here, results being shown in Figure 4.3. It is clear there is an almost ex0 act correlation between the two; the in vitro 0 2 4 6 Days after Seeding model experiencing a 39% decrease in surface area and the in silico model experiencing a Figure 4.3: Line graph showing the decrease in 36% decrease in surface area. Thus provid- surface area for the in silico and in vitro model. ing convincing evidence that the mathematical modelling accurately represents the contractile behaviour of the collagen. Leading on fromt the modelling of the contractile action of the collagen gel, modelling of the cellular behaviour will now be analysed. Figure 4.4 shows the regions of principal strain over the 7 day time period. As discussed before it is expected that cells will migrate to regions of lower strain and also align parallel to the axis of strains denoted by the change in colour in the ANSYS images. 12 (a) Day 1. (b) Day 4. (c) Day 7. Figure 4.4: ANSYS images showing the regions of principal strain in a cuboidal block over a period of time. Figure 4.5 shows the initial distribution of 1000 randomly places cells in the collagen gel with a random alignment. The subsequent images (Figure 4.6) shows the alignment of the cells after a 24 hours. (a) Default View. (b) Top View. (c) Front View. Figure 4.5: Initial random alignment and distribution of cells. (a) Default View. (b) Top View. (c) Front View. Figure 4.6: Cells which have aligned along the lines of principal strain. The final two figures (Figure 4.7 and 4.8) show the alignment of the cells in the collagen for days 4 and 7, notice how they still align according to the lines of principal strain, similar to what has been observed in vitro. 13 0.020 0.010 0.005 0.000 0.010 0.015 0.010 0.005 0.005 0.010 0.020 0.015 0.010 0.005 0.020 0.000 0.00 0.000 0.000 0.00 0.015 0.01 0.02 0.03 0.005 0.01 0.010 0.005 0.02 0.000 0.00 0.03 0.01 0.02 0.03 0.000 (c) Front View. (b) Top View. (a) Default View. Figure 4.7: Cells which have aligned along the lines of principal strain at day 4. 0.020 0.010 0.005 0.000 0.010 0.015 0.010 0.005 0.005 0.010 0.020 0.015 0.010 0.005 0.020 0.000 0.00 0.000 0.000 0.00 0.015 0.01 0.02 0.03 0.005 0.01 0.010 0.005 0.02 0.000 0.00 0.03 0.01 0.02 0.03 0.000 (a) Default View. (b) Top View. (c) Front View. Figure 4.8: Cells which have aligned along the lines of principal strain at Day 7. 4.2 Circular Model. The results of the circular arrangement will now be displayed, including an analysis the lines of principal strain, cell migration and alignment. (a) Day 1. (b) Day 4. (c) Day 7. Figure 4.9: ANSYS images showing the deformation of the cellulised collagen gel after 1, 4 and 7 days. Figure 4.9 shows the deformation that emerges from the cell-collagen contraction and Figure 4.10 similarly shows the position of the nodal points which define the mesh over time. The 14 contractile action of the collagen mimics what has been observed experimentally. (a) Initial Configuration. (b) Day 4. (c) Day 7. Figure 4.10: Point plot of the nodal points after 1, 4 and 7 days. Contraction of collagen gel 300 250 Consruct Area mm2 As before, the collagen gel contraction will be quantified by measuring the change in surface areas across an arial plane. From experimental observations, it is noticed that for the collagen gel in vitro a decrease in surface area of 40% occurs in 7 days, whereas analysis of the images produced in silico to show a decrease in area of around 31% (Figure 4.11). Though not as consistent as it’s cuboidal counterpart, it still remains a fairly accurate model of the experimentally observed situation. 200 In Silico 150 In Vitro 100 50 0 0 2 4 6 Days after Seeding Figure 4.11 Figure 4.12 shows the regions of high strain within the construct over the 7 days, giving one an idea about the alignment and migration of the cells. (a) Day 1. (b) Day 4. (c) Day 7. Figure 4.12: ANSYS images showing the regions of principal strain in a circular construct with two fixed points over a period of time. 15 Modelling the cellular behaviour, Figure 4.13 shows the initial distribution of 1000 randomly places cells in the circular collagen gel with a random alignment. The subsequent figure (Figure 4.14) shows the alignment of the cells after a 24 hours, which is along the lines of principal strain. (c) Front View. (a) Default View. (b) Top View. Figure 4.13: Initial random alignment and distribution of cells. (c) Front View. (a) Default View. (b) Top View. Figure 4.14: Cells which have aligned along the lines of principal strain. The final two figures (Figure 4.15, 4.16) show the alignment of the cells in the collagen for days 4 and 7, and how they still follow along the lines of principal strain, as would be expected. 16 (c) Front View. (a) Default View. (b) Top View. Figure 4.15: Cells which have aligned along the lines of principal strain at day 4. (c) Front View. (a) Default View. (b) Top View. Figure 4.16: Cells which have aligned along the lines of principal strain at Day 7. 17 5 5.1 Discussions and Conclusion Summary. A combination of Finite Element analysis software and agent based modelling has been implemented to calculate regions of principal strain for two relevant gel geometries and to predict the migration and alignment of cells within these collagen based gels. Using FEA results have been reproduced for the already well established cuboidal model, including finding the lines of principal strain and extending these observations by finding regions of principal strain, within the 3-D constructs. Similarly, the regions of principle strain were found in a circular construct. By using this information, previously studied observations of cells behaviour in response to strain can be quantitfied to predict the movement of cells within a 3-D environment. Further use of these models would allow arbitrary geometries to be analysed and the migration and alignment of cells within a 3-D collagen construct could be predicted before expensive laboratory experiments are carried out, thus reducing the time to find optimal geometries. 5.2 Limitations and Further Work. Presented here is a mathematical model for 3-D muscle tissue growth in vivo. Though the model has tried to include the most important factors with regards to the modelling of both the cellular alignment and migration there are many ways in which this model could be refined and improved. One of the most notable ways would be to include the stiffening effect on cell migration which is has been proven to be a significant factor within a collagen gel [15]. A constant Young’s modulus has been used throughout the process, utilising the effect of varying strain to mimic the changing force of compression. With more time, the model could be extended so that the Young’s modulus could be found for each element after each time step, and then the linear relation between stiffening and cell migration could be used to modify the migration rate, as oppose to using a random walk. One other way to dramatically increase the accuracy of results would be to analyse the force relations between c2c12 cells and the collagen matrix presented here. The measure of such interactions are difficult and the literature provides results which vary greatly in magnitude. An accurate measure of this force would allow the model to produce more reliable results. Also an extensive study of the rheology of this cellularised collagen gel over time would allow more accurate determination the Young’s modulus and poisson ratio thus allowing a more accurate prediction of the cell migration over time. The Agent Based modelling could also undergo a extensive work to more accurately model the suspended cells. This includes proliferation of cells (noted to increase under areas of greater stiffness [14]), death, and fusion of cells to form multinucleated myotubes. There are other 18 arbitrary factors that could increase the accuracy of such models, including the use of more agents, longer simulations, finer meshes, all which could be simply extended with time and sufficient computing power. 5.3 Conclusion. This project puts forward a novel approach towards skeletal muscle tissue engineering. By taking data from various biological observations over the last few decades, a mathematical model has been devised which can predict the resulting contractile structure of cellularised collagen hydrogels and the migration of alignment of MDCs suspended within them. Though the model presented is relatively primitive, with many material and cellular properties not being considered, the results produced are very accurate to what is observed in vitro. Refining parameters used in the model, both from the rheology of the collagen gels itself and from in cell-collagen gel interactions, one could not only increase the accuracy of results but also implement arbitrary tissue culture geometries and make informed predictions about the resulting contractile gel. This in silico analysis has to potential to accelerate tissue engineering research towards the goal of growing adult skeletal muscle in vitro, reducing the need for trial-and-error lab experimentation thus saving time and expenses. By being able to grow adult skeletal muscle tissue in vitro it could become possible not only replace lost muscle mass in patients who suffer from muscular dystrophies, but also reduce the need for animal experimentation by being able to perform drug experimentation on said grown tissue as oppose to animal specimens; thus making it cheaper to test the effects of drugs (such a statins) and treatments which may have derogatory effects on muscle growth. References [1] AD Bach, JP Beier, J Stern-Staeter, and RE Horch. Skeletal muscle tissue engineering. Journal of cellular and molecular medicine, 8(4):413–422, 2004. [2] L Baoge, ELKE Van Den Steen, Steven Rimbaut, N Philips, E Witvrouw, KF Almqvist, G Vanderstraeten, and LC Vanden Bossche. Treatment of skeletal muscle injury: a review. International Scholarly Research Notices, 2012, 2012. [3] Tanyarut Boontheekul, Elliott E Hill, Hyun-Joon Kong, and David J Mooney. Regulating myoblast phenotype through controlled gel stiffness and degradation. Tissue engineering, 13(7):1431–1442, 2007. [4] Jean-Michel Bourget, François A Auger, Lucie Germain, Maxime Guillemette, and Teodor Veres. Alignment of Cells and Extracellular Matrix Within Tissue-Engineered Substitutes. INTECH Open Access Publisher, 2013. [5] Kevin P Campbell. Three muscular dystrophies: loss of cytoskeleton-extracellular matrix linkage. Cell, 80(5):675–679, 1995. 19 [6] Dennis R Campion. The muscle satellite cell: a review. International review of cytology, 87:225–251, 1984. [7] Oliver Cassell, Wayne A Morrison, Aurora Messina, Anthony J Penington, Erik W Thompson, Geoffrey W Stevens, Jilska M Perera, Hynda K Kleinman, John V Hurley, Rosalind Romeo, et al. The influence of extracellular matrix on the generation of vascularized, engineered, transplantable tissue. Annals of the New York Academy of Sciences, 944(1):429–442, 2001. [8] Sophie BP Charge and Michael A Rudnicki. Cellular and molecular regulation of muscle regeneration. Physiological reviews, 84(1):209–238, 2004. [9] U Cheema, S-Y Yang, V Mudera, GG Goldspink, and RA Brown. 3-d in vitro model of early skeletal muscle development. Cell motility and the cytoskeleton, 54(3):226–236, 2003. [10] Umber Cheema, Robert Brown, Vivek Mudera, Shi Yu Yang, Gus McGrouther, and Geoffrey Goldspink. Mechanical signals and igf-i gene splicing in vitro in relation to development of skeletal muscle. Journal of cellular physiology, 202(1):67–75, 2005. [11] Pierre Delvoye, Philippe Wiliquet, Jean-Luc Levêque, Betty V Nusgens, and Charles M Lapière. Measurement of mechanical forces generated by skin fibroblasts embedded in a three-dimensional collagen gel. Journal of Investigative Dermatology, 97(5):898–902, 1991. [12] M Eastwood, VC Mudera, DA McGrouther, and RA Brown. Effect of precise mechanical loading on fibroblast populated collagen lattices: morphological changes. Cell motility and the cytoskeleton, 40(1):13–21, 1998. [13] Mark Eastwood, D Angus McGrouther, and Robert A Brown. A culture force monitor for measurement of contraction forces generated in human dermal fibroblast cultures: evidence for cell-matrix mechanical signalling. Biochimica et Biophysica Acta (BBA)-General Subjects, 1201(2):186–192, 1994. [14] E Hadjipanayi, V Mudera, and RA Brown. Close dependence of fibroblast proliferation on collagen scaffold matrix stiffness. Journal of tissue engineering and regenerative medicine, 3(2):77–84, 2009. [15] Ektoras Hadjipanayi, Vivek Mudera, and Robert A Brown. Guiding cell migration in 3d: a collagen matrix with graded directional stiffness. Cell motility and the cytoskeleton, 66(3):121–128, 2009. [16] S Kasugai, S Suzuki, S Shibata, S Yasui, H Amano, and H Ogura. Measurements of the isometric contractile forces generated by dog periodontal ligament fibroblasts in vitro. Archives of oral biology, 35(8):597–601, 1990. [17] Takahisa Okano and Takehisa Matsuda. Tissue engineered skeletal muscle: preparation of highly dense, highly oriented hybrid muscular tissues. Cell transplantation, 7(1):71–82, 1998. 20 [18] GP Raeber, MP Lutolf, and JA Hubbell. Part ii: Fibroblasts preferentially migrate in the direction of principal strain. Biomechanics and modeling in mechanobiology, 7(3):215–225, 2008. [19] Janet Shansky, Bernard Creswick, Peter Lee, Xiao Wang, and Herman Vandenburgh. Paracrine release of insulin-like growth factor 1 from a bioengineered tissue stimulates skeletal muscle growth in vitro. Tissue engineering, 12(7):1833–1841, 2006. [20] AST Smith, S Passey, L Greensmith, V Mudera, and MP Lewis. Characterization and optimization of a simple, repeatable system for the long term in vitro culture of aligned myotubes in 3d. Journal of cellular biochemistry, 113(3):1044–1053, 2012. [21] Herman H Vandenburgh, Patricia Karlisch, and Lynne Farr. Maintenance of highly contractile tissue-cultured avian skeletal myotubes in collagen gel. In vitro cellular & developmental biology, 24(3):166–174, 1988. [22] Prasad KDV Yarlagadda, Margam Chandrasekharan, and John Yong Ming Shyan. Recent advances and current developments in tissue scaffolding. Bio-medical materials and engineering, 15(3):159–177, 2005. 21