BioMEMS For Treatment Of Glaucoma S.Sibi , Aman Kumar Arora , Amritraj.k
advertisement
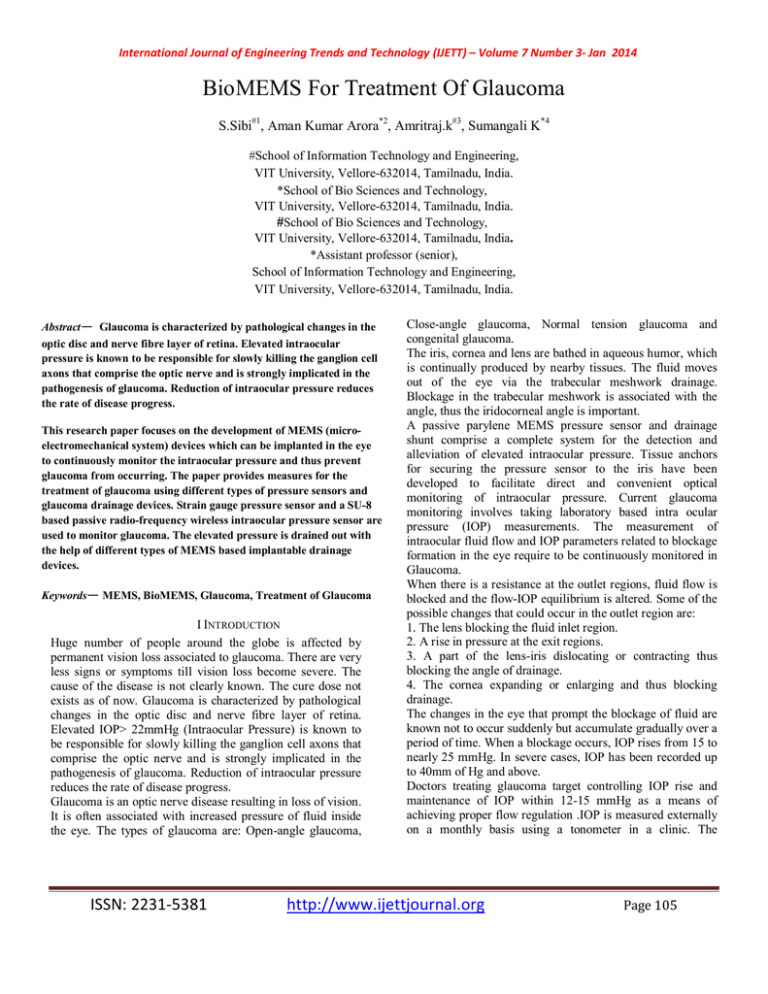
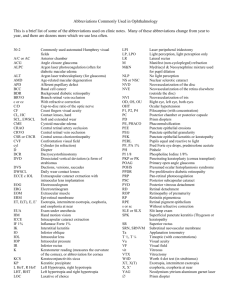
International Journal of Engineering Trends and Technology (IJETT) – Volume 7 Number 3- Jan 2014 BioMEMS For Treatment Of Glaucoma S.Sibi#1, Aman Kumar Arora*2, Amritraj.k#3, Sumangali K*4 #School of Information Technology and Engineering, VIT University, Vellore-632014, Tamilnadu, India. *School of Bio Sciences and Technology, VIT University, Vellore-632014, Tamilnadu, India. #School of Bio Sciences and Technology, VIT University, Vellore-632014, Tamilnadu, India. *Assistant professor (senior), School of Information Technology and Engineering, VIT University, Vellore-632014, Tamilnadu, India. Abstract— Glaucoma is characterized by pathological changes in the optic disc and nerve fibre layer of retina. Elevated intraocular pressure is known to be responsible for slowly killing the ganglion cell axons that comprise the optic nerve and is strongly implicated in the pathogenesis of glaucoma. Reduction of intraocular pressure reduces the rate of disease progress. This research paper focuses on the development of MEMS (microelectromechanical system) devices which can be implanted in the eye to continuously monitor the intraocular pressure and thus prevent glaucoma from occurring. The paper provides measures for the treatment of glaucoma using different types of pressure sensors and glaucoma drainage devices. Strain gauge pressure sensor and a SU-8 based passive radio-frequency wireless intraocular pressure sensor are used to monitor glaucoma. The elevated pressure is drained out with the help of different types of MEMS based implantable drainage devices. Keywords— MEMS, BioMEMS, Glaucoma, Treatment of Glaucoma I INTRODUCTION Huge number of people around the globe is affected by permanent vision loss associated to glaucoma. There are very less signs or symptoms till vision loss become severe. The cause of the disease is not clearly known. The cure dose not exists as of now. Glaucoma is characterized by pathological changes in the optic disc and nerve fibre layer of retina. Elevated IOP> 22mmHg (Intraocular Pressure) is known to be responsible for slowly killing the ganglion cell axons that comprise the optic nerve and is strongly implicated in the pathogenesis of glaucoma. Reduction of intraocular pressure reduces the rate of disease progress. Glaucoma is an optic nerve disease resulting in loss of vision. It is often associated with increased pressure of fluid inside the eye. The types of glaucoma are: Open-angle glaucoma, ISSN: 2231-5381 Close-angle glaucoma, Normal tension glaucoma and congenital glaucoma. The iris, cornea and lens are bathed in aqueous humor, which is continually produced by nearby tissues. The fluid moves out of the eye via the trabecular meshwork drainage. Blockage in the trabecular meshwork is associated with the angle, thus the iridocorneal angle is important. A passive parylene MEMS pressure sensor and drainage shunt comprise a complete system for the detection and alleviation of elevated intraocular pressure. Tissue anchors for securing the pressure sensor to the iris have been developed to facilitate direct and convenient optical monitoring of intraocular pressure. Current glaucoma monitoring involves taking laboratory based intra ocular pressure (IOP) measurements. The measurement of intraocular fluid flow and IOP parameters related to blockage formation in the eye require to be continuously monitored in Glaucoma. When there is a resistance at the outlet regions, fluid flow is blocked and the flow-IOP equilibrium is altered. Some of the possible changes that could occur in the outlet region are: 1. The lens blocking the fluid inlet region. 2. A rise in pressure at the exit regions. 3. A part of the lens-iris dislocating or contracting thus blocking the angle of drainage. 4. The cornea expanding or enlarging and thus blocking drainage. The changes in the eye that prompt the blockage of fluid are known not to occur suddenly but accumulate gradually over a period of time. When a blockage occurs, IOP rises from 15 to nearly 25 mmHg. In severe cases, IOP has been recorded up to 40mm of Hg and above. Doctors treating glaucoma target controlling IOP rise and maintenance of IOP within 12-15 mmHg as a means of achieving proper flow regulation .IOP is measured externally on a monthly basis using a tonometer in a clinic. The http://www.ijettjournal.org Page 105 International Journal of Engineering Trends and Technology (IJETT) – Volume 7 Number 3- Jan 2014 condition is treated with a pharmacologic known as betablockers or adrenergic agnostics which are used to clear blockages by regulating fluid production, inlet and exit pressures to maintain an optimal IOP level. IOP is prone to fluctuations and has been recorded to vary during different times of the day. When chemicals fail to bring down IOP, treatment is then focused on surgical removal and correction of the structures blocking fluid drainage. Apart from raised IOP, patients with glaucoma have been observed to have an increased resistance to outflow of the aqueous humor which is also expressed as facility of outflow and is an important blockage related parameter denoted by the symbol Cf. Glaucoma management options include medical therapy, laser surgery, incisional surgery and glaucoma drainage devices (GDD). Medical therapy lowers IOP by improving the outflow of aqueous humor (AH) or to reduce its production. Some surgical techniques attempt to stimulate AH outflow, however, the primary surgical strategy is to manage glaucoma by lowering the patient’s IOP through removal of excess AH. Regardless of the technique that is employed, accurate real-time measurements of IOP and the ability to restore normal levels are critical in the treatment of this disease. We now see the various ways of treatment of glaucoma using MEMS. II TREATMENT OF GLAUCOMA The doctors treating glaucoma target controlling IOP rise and maintenance of IOP within 12-15 mmHg as a means of achieving proper flow regulation .IOP is measured externally on a monthly basis using a tonometer in a clinic. The condition is treated with a pharmacologic known as betablockers or adrenergic agnostics which are used to clear blockages by regulating fluid production, inlet and exit pressures to maintain an optimal IOP level. IOP is prone to fluctuations and has been recorded to vary during different times of the day. When chemicals fail to bring down IOP, treatment is then focused on surgical removal and correction of the structures blocking fluid drainage. Apart from raised IOP, patients with glaucoma have been observed to have an increased resistance to outflow of the aqueous humor which is also expressed as facility of outflow and is an important blockage related parameter denoted by the symbol Cf. Glaucoma management options include medical therapy, laser surgery, incisional surgery and glaucoma drainage devices(GDD). Medical therapy lowers IOP by improving the outflow of aqueous humor (AH) or to reduce its production. Some surgical techniques attempt to stimulate AH outflow, however, the primary surgical strategy is to manage glaucoma by lowering the patient’s IOP through removal of excess AH. Regardless of the technique that is employed, accurate real-time measurements of IOP and the ability to restore normal levels are critical in the treatment of this disease. ISSN: 2231-5381 A. Glaucoma Drainage Device (GDD) These are the devices that are surgically inserted into the eye in order to increase the outflow of the aqueous humor. They create an alternate pathway by channeling aqueous from anterior chamber through a long tube to an equatorial plate inserted under the conjunctiva. Fig 1: A glaucoma drainage device implanted in the eye Once the device is surgically implanted, body begins to encapsulate the device with fibrous tissue as it considers the GDD to be a foreign object, forming a bleb. This bleb is extremely important in the operation of the device, because it principal source of resistance to flow of aqueous through device. Aqueous humor flows freely out of anterior chamber, through tube and onto drainage plate, from where it would spread across surface of sclera with minimal resistance. This is a major feature which determines success or failure in an individual. MEMS technology offers several advantages over traditional approaches to glaucoma therapy including highly functional microfluidic systems that can be adapted to drug delivery and IOP management, miniaturized sensors suitable for implantation with precise and accurate readouts; precision and batch fabrication. The purpose of a GDD is to control and regulate IOP, however, current GDD’s are lacking in function and in efficacy. GDD is implantable and passive to reduce and regulate IOP by controlling removal of excess aqueous humor from anterior chamber. B Intraocular Pressure Sensor For Glaucoma Management Increased IOP and wide daily IOP variations indicate risk of glaucoma, a widespread condition which leads to irreversible loss of peripheral vision, and detailed information would be invaluable towards the clinical management of glaucoma. Since changes in IOP are correlated to changes in cornea curvature, wearable MEMS strain gauge for the measurement of spherical deformation of the cornea due to intraocular pressure changes promises to provide continuous, minimally invasive monitoring over prolonged periods. The strain gauge developed by Leonardi et al (given in figure) is based on the same flexible polyimide technology with embedded Pt–Ti structures. The polyimide structure is then embedded in a soft contact lens, which can be worn continuously during the course of a day for uninterrupted measurement. http://www.ijettjournal.org Page 106 International Journal of Engineering Trends and Technology (IJETT) – Volume 7 Number 3- Jan 2014 Fig 2: A graph between time and contact lens output voltage Measurements from the sensing contact lens show good sensitivity, revealing pressure changes as low as 1.5–2 mm Hg, and this device shows promise toward the continuous monitoring of IOP. The strain gauge measures the change in pressure on the eye with blinking (eyes are closed but the eyelids are pressed more firmly). Also evident is ocular pulsation due to the heart rate. This pulsation is the smallest signal ever measured in the eye and corresponds to 1.5–2 mm Hg. C Su-8 Based Micro fabricated Implantable Inductively Coupled Passive RF Wireless Intraocular Pressure Sensor An implantable passive wireless pressure sensor uses an inductively coupled wireless sensing technique, particularly designed to monitor IOP of glaucoma patients. The microfabricated IOP sensor consists of a planar spiral gold coil conductor, a two-parallel-gold-plate (metal-insulatormetal) capacitor, and a SU-8 pressure sensitive diaphragm. The IOP is fully encapsulated inside biocompatible SU-8 stacking layers to isolate IOP sensor from biological tissue medium environment. By measuring the impedance phase dip frequency shift from external coil, the IOP signal can be obtained through implanted IOP sensor. The optimised size of manually wound external coil was investigated. The readout distance is upto 6mm from implanted sensor. The microfabricated IOP sensor has relatively high sensitivities7035ppm/mm of Hg in air and 3370 ppm/mm of Hg in saline medium, with pressure resolution lower than 1 mm of Hg, which is adequate for IOP monitoring application. ISSN: 2231-5381 Fig 3: Fabrication process flow of wireless IOP sensor D Implantable Parylene Mems For Glaucoma Therapy Parylene is selected as the structural material for aforementioned components for its desirable properties, both as a biomaterial and a MEMS material. It is a USP Class VI material that is utilized for its biocompatibility, biostability, and low cytotoxicity. Parylene is a proven MEMS material with excellent properties including low process temperature, low defect density, transparency, and chemical inertness. In addition, parylene technology accommodates multi-layer processing to produce highly functional structures and features. While biological environments are extremely corrosive to most MEMS materials, parylene is not affected as it cannot be degraded hydrolytically . The combination of an implantable MEMS sensor and drain will make it possible to closely track a patient’s IOP history and maintain IOP at normal levels. This constitutes a novel and complete diagnostic and therapeutic system for treating glaucoma. GDDs must be designed to incorporate several physiological parameters. Aqueous humor is produced in the eye at 2.4±0.6 µL/min (mean±SD) and changes over the course of a day (morning: 3.0 µL/min; afternoon: 2.4 µL/min; evening: 1.5 µL/min). The resistance of conventional AH drainage tissues is ~3-4 mmHg/µL/min. The minimal system requirements for a MEMS GDD are a shunt and pressure-sensitive valve to remove excess AH such that IOP is maintained between 5-22 mmHg. A parylene shunt has been fabricated using a sacrificial silicon technology. A shunt mold is etched into a http://www.ijettjournal.org Page 107 International Journal of Engineering Trends and Technology (IJETT) – Volume 7 Number 3- Jan 2014 silicon wafer and parylene is deposited around the mold. Each shunt is removed from the master mold and the silicon is chemically removed. Flow and pressure regulation is achieved by controlling the number of and time at which the punctures are made along the closed end of the shunt. At physiological flow rates, pressure drops are negligible for the size of our shunt. Therefore, the majority of the pressure drop in the system will be concentrated at the valve. In order to promote drainage of AH out of the anterior chamber, the valve must be optimized to drain at a flow rate equal to the production of AH at elevated IOPs. It must open at IOP > 22 mmHg and close when IOP ≤ 22 mmHg to prevent hypo tony. The mechanical pressure sensor is based on the principle of operation of a Bourdon tube and consists of a centrally supported, free-standing parylene spiral-tube formed by a long, thin-walled toroidal channel. An indicator tip is integrated at the end of the channel at the circumference of the spiral as a means for simple optical readout. When a uniform pressure difference is generated across the channel walls, a bending moment is created forcing an in-plane radial and angular deformation of the tube. When the external pressure is lower than the internal pressure in the channel, the spiral structure unwinds. When the external pressure exceeds the internal pressure, the spiral will further coil. This effect can be monitored by visually tracking the movement of the indicator tip. Deformation that results is linearly related to the applied pressure difference and can be correlated to environmental pressure, or in this case, IOP. Implantable devices require mechanical attachment to the biological environment. This is typically achieved by sutures, tacking, or stapling at the expense of increasing overall implant size through the addition of anchoring sites. Given the spatial constraints in the eye and to minimize damage, it is desirable to implant and secure our sensor and GDD without needing sutures. The logical choice for placement of the IOP sensor to facilitate optical readout would be behind the transparent cornea on the iris. E Artificial Nano-Drainage Implant For Glaucoma Treatment (ANDL) This technique involves replacing the functionality of diseased drainage pathway for aqueous humor outflow (i.e., trabecular meshwork). By enhancing aqueous humour outflow, artificial drainage implant will lead to decrease in IOP and a halt in progression of glaucoma. A nano-drainage implant consists of a micro porous membrane connected to an integrated polymeric shaft inserted through sclera into anterior chamber, thereby, allowing a bypass route for aqueous humor outflow. Initial studies of aqueous humor perfusion through such membranes showed protein plugging as a result of hydrophobic interactions. Myocilin, a strong hydrophobic ISSN: 2231-5381 protein was identified as the cause of that obstruction. The nano-filtration implant design could easily and safely be inserted into a glaucomatous eye and could immediately and predictably lower the IOP. Nano pore of 200nm or less in diameter can effectively prevent bacterial penetration. Tiny porous size will contribute to protein absorption and clogging unless a non-fouling biocompatible material is coated on the surfaces. An integrated packaging technique has to be utilized to connect filtration membrane to polymeric shaft for easy implantation procedure. Fig 4: Fabrication process of ANDL F Minimally Invasive Parylene Dual-Valved Flow Drainage Shunt For Glaucoma Implant Enabled by the dual-check valve operation, a paryleneenabled microvalved shunt implant can physically drain extra intraocular fluid and regulate IOP within normal range of 1520mm of Hg. Improved surgical features, in addition to microfluidic components, such as parylene- tube carrier and anchors, are also incorporated in such device to realize minimally invasive suture-less implantation, suitable for practical in-vivo use. With the optimized micromachining and post-fabrication process procedures, developed implant is first check-valved GDD, which is passive, consumes no additional power and functions without any circuit involved to pursue it’s medical application. http://www.ijettjournal.org Page 108 International Journal of Engineering Trends and Technology (IJETT) – Volume 7 Number 3- Jan 2014 impanation. The slit between valve and parylene microtube was sealed by epoxy. After epoxy dried, valve tube assembly was inserted into DuPont Teflon FET capillary tube and photoresist was used to seal gap between FET tube and valve tube structure. FET tube was cut into 2 inch segments in advance and integrated valve tube assembly was attached to one end of capillary tube. Whole setup was baked to dry in conventional oven at 100*C. After photoresist dried, each assembly was connected to testing setup. Bench-top testing setup used compressed nitrogen to apply pressure to water. Fig 5: Full GDD System consisting of dual valve micro-flow regulation system The complete implant comprises a dual-valve microflow regulation system in tube with integrated anchors. Dual backto-back microvalves with one normally closed(NC) but open at 20mm Hg and normally open(NO) but closed beyond 50mm Hg are designed. Few holes are designed on strictionbonding parts where epoxy can be used to further ensure bonding strength and to prevent parylene from delamination after repeated operations. To accommodate two microvalves, hollow tubes made of thick parylene are utilized and length is chosen as 6mm long. The fluid can flow from NC valve to NO valve before the pressure reaches limit of NO valve,while opposite direction iis forbidden due to closed NC valve. G Ex-Vivo Implantation Study Of Minimally Invasive GDD The GDD is designed to treat glaucoma patients by draining out their extraneous aqueous humor out of anterior chamber utilizing MEMS micro-fluidic normally closed (NC) check valve. NC check valve is encapsulated in protective tubing made from parylene C, which has been proven to be biocompatible in implantation. A new packaging and benchtop testing procedure is established to characterize integrated GDD prior to it’s implantation into enucleated porcine eyes. Pre-implanted characterization curve demonstrates cracking pressure of 10-20mm Hg of NC check valve. The NC check valve remains closed as long as aye pressure is lower than designed cracking pressure. It restricts eye fluid from leaking out of anterior chamber, which otherwise causes hypotony. Owing to the inherent structure of NC valve, fluid coming from opposite way will be rejected, protecting anterior chamber from any unwanted fluid flowing in. Cracking pressure can be controlled by many parameters such as height of stiction part of parylene, parylene thickness, tether numbers and geometry of tethers. Flow rate is defined by size of opening orifice and opening gap of parylene membrane. The chip with valves was first dipped into acetone water to strip off protective photoresist. Each valve is released from chip by breaking silicon connection part. The NC check valve was then inserted with parylene side facing interior of parylene micro tube in order to prevent damaging parylene membrane during ISSN: 2231-5381 Fig 6: Fabrication process of NC check valves III CONCLUSION Though there are a lot of ways treating glaucoma. The real important question is “is there a cure?” If there is a cure then it would be really be a great medical breakthrough. The most promising method of cure seems possible from the studies of Dr.Drooper of UCLA medical institute. The treatment for glaucoma has increased tremendously over the years but finding the cure is more important. REFERENCES [1] Ellis Meng, Po-Jui Chen, Damien Rodger, Yu-Chong Tai, and Mark Humayun , “Implantable parylene MEMS for glaucoma therapy”. [2] Wen Li, Micro technology Laboratory, Michigan State University, “MEMS for Biomedical applications”. [3] Jeffrey Chun-Hui Lin, Feiqiao Yu, Saloomch Saati, Rohit Varma,Po-Jui , Mark S. Humayun, Yu-Chong Tai,”Ex-vivo implanation study of minimally invasive glaucoma drainage device”. [4] Karen C. Cheung , Philippe Renaud, “BioMEMS for medicine: On-chip cell characterization and implantable microelectrodes”. [5] Jun Cheng, Jiang Liu, Damon Wing Kee Wong, Ngan Meng Tan, Beng Hai Lee,” Focal edge association to glaucoma diagnosis”. [6] Smitha Shankar, SET Portfolio, RMIT University,” Development of a MEMS device to continuously monitor glaucoma”. http://www.ijettjournal.org Page 109