U W Warwickshire Infant Mental Health Pathway: January 2014
advertisement

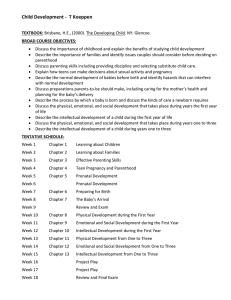
UNIVERSITY OF WARWICK Warwickshire Infant Mental Health Pathway: January 2014 Introduction Why Perinatal and Infant Mental health? Marmot (2010)1 identified that in order to reduce future social and health inequalities we need to give every child the best start in life, and this reflects the view that the origins of much adult disease lie in the ‘developmental and biological disruptions occurring during the early years of life’ and more specifically to ‘the biological embedding of adversities during sensitive developmental periods’.2 Both perinatal and infant mental health are therefore major public health issues, and perinatal and infant mental health services are aimed at giving every child the best start in life by promoting the wellbeing of parents and their babies across the perinatal period, in addition to the early identification and treatment of problems that complicate pregnancy and the post-partum year. For many families, standard perinatal services will help steer them through the life-changing transition to parenthood, while for others the path maybe more complicated and require a greater intensity of specialised services and support. Whatever the level of need, the economic case for providing effective services throughout this period is compelling, 3 and the commissioning of services to achieve these ends is supported by a range of policy documents (see below) emphasising the importance of early intervention, and highlighting the opportunities afforded by the perinatal period. The perinatal and infant mental health pathway described is both evidence-based in that it is underpinned by research about ‘what works’ during this period, and also includes a focus on primary prevention. This goes beyond the traditional focus on the immediate perinatal period to include preconception services that are aimed at building early resilience and self-respect in young people, and developing the foundations for healthy and respectful relationships that form the basis for later perinatal wellbeing. The pathway continues through pregnancy and the postnatal period until the infant is one year. The goals of promotion, prevention and treatment during this important period require the commissioning of a diverse range of services, alongside high standards of service delivery and care. This perinatal and infant mental health pathway has been developed to support the work of both practitioners working directly with infants and their parents, and managers and commissioners who have the remit of ensuring that the health, social care and public health services necessary to give every child the best start in life, are in place. Policy context The policy context for this perinatal and infant mental health pathway is the Healthy Child Programme (HCP),4 which was revised in 2009 to take account of recent changes in evidence about the importance of the perinatal period, and which sets the overall standard in terms of the delivery and commissioning of services from pregnancy to age 5. The Health Visitor Implementation Plan5 describes the government’s strategy for expanding health visiting services, to ensure that families have a positive start, through the delivery of the Healthy Child Programme. A number of government reports3,6 have concluded that strategies to promote infant and child welfare should include a commitment to prevention, and a focus on promoting wellbeing that begins during pregnancy and continues throughout the early years. This has also been reflected in the review of child protection in England, which emphasises the importance and effectiveness of prevention and early intervention. A final endorsement is provided by the cross party government strategy for mental health, which employs ‘starting and developing well’ as one of its key objectives. The need for early prevention and intervention was also highlighted by the Munro Review of child protection services in England, and the cross-party government strategy for mental health – No Health without Mental Health,7 which highlights ‘starting and developing well’ as one of its key objectives. Another significant part of the policy context is the NICE guidance ‘Ante and Postnatal Mental Health’ currently being updated, which will hopefully include a greater focus on the infant. Infrastructure Requirements This perinatal and infant mental health pathway relies on the dedication and commitment of a large number of frontline practitioners such as midwives, health visitors and children’s centre workers. A number of infrastructure requirements are necessary including the following: o A fundamental aspect of the provision of good quality and efficient services are the knowledge and skills of the frontline staff involved in their delivery, alongside the adequate staffing of services. A range of innovative ways of working to support the wellbeing of parents and infants have been developed over the past decade, and staff need to be provided with opportunities for continuing professional development (CPD) in order to acquire the necessary skills to deliver these new ways of working. 2 o The research points to the importance of practitioners having access to appropriate supervision and support, and evidence about the value of supervision has now been provided for practitioners such as health visitors in terms of increasing compassion and job satisfaction, as well as reducing burn-out and stress.8 o Other necessary infrastructure requirements include the type of integrated working practices between, for example, midwives and health visitors, and adult mental health practitioners and children’s social service workers, which have been identified as being necessary to both effective information sharing and patient care, in the perinatal period.9 o The full commissioning of the Healthy Child Programme is necessary to enable staff to work towards achieving the best start in life for every child. An Infant Mental Health Pathway The pathway is divided into three time periods: 1. Pre-conception 2. Antenatal 3. Postnatal (up to one year) Within each of the three colour-coded sections, and in keeping with the Health Visitor Implementation Plan (DH 2011), Universal, Universal Plus and Universal Partnership plus services are identified. Each section starts with an overview of the aims and objectives for each of the time periods and then presents examples of evidence-based or promising initiatives that should be provided and references to the relevant evidence. Example programmes from Warwickshire have been utilised in this programme, but other similar programmes should where appropriate be used. 3 Context of service delivery: The circle represents the local context - the community. The Universal; Universal Partnership and Universal Partnership Plus programmes and services that can be provided as part of this infant mental health pathway will be influenced by and should take account of, the wider community context. Universal Partnership Plus - on-going support for families Universal Plus Support when you need it Universal Services contact at key stages- offered to all local issues important to you , important to you 4 Table 1: Prevalence of Perinatal Mental Health Problems: Warwickshire Registered births 2012 Suffering depression in the postnatal period (10%) Mental disorder requiring referral for psychological therapies (80 per 1,000 deliveries) Mental disorder requiring referral to a specialist perinatal mental health service (40 per 1,000 deliveries) Psychotic episode requiring in-patient admission (0.2%) Non-psychotic depression Requiring in-patient admission (0.2%) Pre-existing serious mental illness complicating and affecting birth (0.2%) Warwickshire North Rugby South Warwickshire Warwickshire 2286 1261 2758 6305 229 126 276 631 183 101 221 504 91 50 110 252 5 3 6 13 5 3 6 13 5 3 6 13 Source: Office for National Statistics – Vital Statistics Tables - Live births (2012) 5 Table 2: Births in Warwickshire England Warwickshire North Rugby South Births 694.241 6,305 2,286 1,261 2,758 Crude birth rate /1,000 population 13.0 11.5 12.2 12.5 10.6 Source: Office for National Statistics – Vital Statistics Tables 2012 Table 3: Numbers of 0-5 year olds (inclusive) Warwickshire North Rugby South 37,853 13,517 7,691 16,645 Source: Mid 2012 population estimates, ONS Table 4: Children subject to a Child Protection Plan as at 31 December 2013 aged 5 or under North Rugby South Warwickshire TOTAL Unborn 3 1 1 5 Under 1 27 6 17 50 1 yr 23 6 14 43 2 yr 27 3 17 47 3 yr 22 2 9 33 4 yr 22 4 12 38 5 yr 13 4 5 22 Warwickshire TOTAL 137 26 75 238 6 Table 5: Family Nurse Partnership Uptake and Referrals - Jan 2013 to Jan 2014 Total No. Notifications No. Declined Not able to Contact Not Eligible* Miscarried Not Recruited Total Enrolled South 36 3 3 3 1 10 16 Rugby 24 1 0 5 1 12 5 North 89 4 1 19 6 48 11 Please note, *those ‘not eligible’ were mostly due to gestation rather than their age. Those ‘not recruited’ were due to lack of capacity The figures are dependent on midwives sending their booking forms and not all forms from the South are sent Table 6: Number of fixed term and permanent exclusions from Warwickshire schools - Autumn and Spring Terms only 2012/13 Note: Data represents the number of exclusions NOT the number of pupils excluded as some pupils will have more than 1 fixed term exclusion during the year Permanent North (North Warwickshire and Nuneaton and Bedworth Districts) 5 South (Warwick and Stratford on Avon Districts) 4 Rugby (Rugby District) 1 Fixed Period North Warwickshire 130 Fixed Period Nuneaton and Bedworth 388 Fixed Period Rugby 373 Fixed Period Stratford on Avon 349 Fixed Period Warwick 303 Permanent North Warwickshire 2 Permanent Nuneaton and Bedworth 3 Permanent Rugby 1 Permanent Stratford on Avon 2 Permanent Warwick 2 7 Table 7: Referrals to CAMHS 2013 - 2014 CAHMS SERVICE - No Of Referrals Number of referrals from Primary Health Care Number of referrals from Child Health Number of referrals from Social Services Number of referrals from Education Number of referrals from YOS Number of referrals from Learning Disability Service Number of referrals from Adult Mental Health Number of referrals from voluntary/ Independent sector Number of self-referrals Number of other Trust Referrals Total Number of Referrals Number of inappropriate Referrals Gender Male Female Area North Rugby South Coventry Out of Area Age Aged 0 - 4 Aged 4 - 9 Aged 9 - 14 Aged 14 -16 Aged 16 -18 April /May /June 513 61 20 109 0 0 0 0 0 100 803 164 July/Aug/Sept 485 64 0 66 0 0 0 0 30 111 756 265 154 146 140 110 144 43 98 10 5 76 45 100 19 10 5 73 110 89 23 1 67 77 75 30 8 Overview of the Infant Mental Health Pathway: Pre-Conception Aims 1. 2. 3. 4. Promote respectful, safe and enjoyable relationships Preparation for future parenthood Reduce teenage conception Promote the planning of pregnancies Promote safe and enjoyable relationships Objectives Preparation for future parenthood SECTION Build self-esteem and awareness of rights and responsibilities Increase knowledge about the importance of respectful, safe, and enjoyable relationships Develop skills for healthy relationships Promote knowledge about healthy intimate relationships and sexual activity Develop knowledge about parenting responsibilities and skills Raise awareness about the importance of parenting Develop parenting skills Reduce teenage conception Improve knowledge about sexual intimacy and relationships Infant Provide Mental access toHealth appropriate support services inside education and other settings ONE: Pathway: Pre-Conception Promote planned pregnancy in adults Raise awareness and understanding about the importance of planning pregnancy Provide access to Long Acting Reversible Contraception to would-be parents who face additional challenges 9 Infant Mental Health Pathway: Pre-Conception 1. Promote respectful safe and enjoyable relationships Build self-esteem and awareness of rights and responsibilities Increase knowledge about the importance of respectful, safe, and enjoyable relationships Develop skills for healthy relationships Promote knowledge and skills to enable children to develop healthy, intimate relationships Intervention Personal Social Health and Economic Education (PHSE) School-based planned programme of learning through which children and young people acquire the knowledge, understanding and skills they need to manage their lives now and in the future (http://www.pshe-association.org.uk) including: Bullying Drug and Alcohol Emotional health and Wellbeing Healthy Lifestyles Safety Commissioning of PHSE training from other agencies (e.g. Warwickshire Respect Yourself Campaign (RYC), which launched the Spring Fever’.10 programme in 2013; Warwickshire’s Safeline11 services deliver both antibullying workshops and counselling to schools and individuals) Who / when Trained primary and secondary school staff, school nurses Voluntary sector 10 Schools to achieve National ‘Healthy Schools’ Status12 Work towards government target of all schools achieving National Healthy Schools Status School staff 2. Preparation for future parenthood Develop knowledge about parenting responsibilities and skills Raise awareness about the importance of parenting Develop parenting skills Commissioning and coordination of countywide services Gather evidence, influence, introduce standards, and commission/deliver Relationship and Sexual Education (RSE) training for various agencies delivering RSE to ensure consistent, key messages countywide County council Schools based programmes13 Accessible Relationship and Sexual Health Services (RSE) (Currently non–statutory) good-quality relationships education: teaching about respect, honesty, trust, self-esteem and sexual health, starting in primary school aged children (e.g. Warwickshire Respect Yourself Campaign (RYC) which launched the ‘Spring Fever’14 programme in 2013) Trained primary and secondary school staff, school nurses and voluntary sector provision Classroom-based initiatives (e.g. Roots of Empathy programme15 - see examples) Drop- in clinics: Advice, support and signposting (e.g. emphasis on keeping safe and safeguarding) Anti-bullying policies and programmes: School-based programs to reduce bullying and victimization16 School nurses in secondary schools 11 Warwickshire’s Safeline17 services deliver both anti-bullying workshops and counselling to schools and individuals National and local policies. Programmes delivered by both statutory and voluntary sector Counselling services School nurses skilled in counselling Conflict resolution Voluntary sector Training for practitioners and participants, online and face-to-face (e.g. One Plus One)18 Web-based resources Preparing Tomorrows Parents - http://www.preparetomorrowsparents.org 3. Reduce teenage conception Improve knowledge of sexual intimacy and relationships Provide access to appropriate support services within education and other settings Accessible Relationship and Sexual Health Education (RSE) Services School-based counselling services Primary health care services Local drop-in clinics Online resources (e.g. RYC on line website, a guide to services and Q & A forum; Kooth’ online support for young people age 11- 1819) Other national resources (e.g. National Children’s Bureau: Sex Education Forum) Primary and secondary school years 12 Provision of contraceptive advice and services Local services Community Contraception Service (CCS) provides a specialist contraceptive and sexual health service which responds to individuals of all age groups, and is delivered in a timely and appropriate manner; including dedicated services for young people) Sexual Health Clinics Primary health care Voluntary sector services Counselling services Online counselling resources RYC online website, a guide to services and Q & A forum; ‘Kooth’ online support Online services for young people age 11- 18 20 School-based counselling services School nurses GPs Primary health care services Support for Care Leavers Practice nurses Statutory social care services Voluntary sector services Factors promoting care leavers transition to independent living Stable placements whilst in care Access to and continuity of professional and informal support for young people as they prepare for the transition out of care Support for Parents of adolescents Online resources (e.g. NSPCC ‘Parent line’21) Parenting programmes for parents of adolescents (e.g. Teen seminars offered by Warwickshire family and parenting team) Voluntary sector 13 Other national/local support (e.g. Online resources from the NSPCC, Barnardos or Action for Children) Commissioning and coordination of countywide services Commissioning and coordination of county-wide services Commissioning and introduction of standards for delivery of Relationship and Sexual Education (RSE) training for various agencies delivering RSE to ensure consistent, key messages countywide 4. Promote planned pregnancies in adults Raise awareness and understanding about the importance of planning pregnancy Provide access to Long Acting Reversible Contraception to would-be parents who face additional challenges Intervention Pre-conception counselling Online pre-conception services (e.g. Foresight 22 - see example below) National and local pre-conception counselling services (NHS Family planning Clinics) Conflict resolution skills training for practitioners and participants; online and face-to-face (e.g. One Plus One23) Youth counselling services Provision of contraceptive advice and services Community Contraception Service (CCS) provides a specialist contraceptive Who / when Community perinatal mental health services and voluntary sector Primary care statutory and 14 and sexual health service which responds to individuals of all age groups, including dedicated services for young people voluntary sector providers Sexual Health Clinics Promote use of Long Acting Reversible Contraception (LARC24) where appropriate to increase planned pregnancy Services for drug and alcohol dependency Access to advice about Long Acting and Reversible Contraception (LARC), and specialist treatment (e.g. Compass Warwickshire - specifically for under 18’s; Supporting Drug and Alcohol Recovery Service provided in Warwickshire by The Recovery Partnership) Support for Care Leavers (e.g. Factors enabling care leavers transition to independent living25) Primary care statutory and voluntary sector providers Statutory social care services Voluntary services Stable placements while in care Access to and continuity of professional and informal support for young people as they prepare for transition out of care (e.g. Care leavers be supported by a ‘leaving care worker’ and also a Personal Adviser (PA) from the charity Barnardo’s) Easy and confidential access to sexual health information (e.g. Respect yourself campaign website http://www.respectyourself.info) Services for refugees and asylum seekers 26 English as a second language (ESL) classes available (n.b. MIND language skills as a key factor in preserving mental health) identified Classes provided by various providers. Some arranged through Children’s centres. 15 Services for individuals with learning disabilities Specialist pregnancy services (e.g. The Charity FPA offer Specialist sexual health services for people with learning disabilities - http://www.fpa.org.uk) Staff involved in the care of vulnerable, young people Medication planning in pregnancy (e.g. Severe Mental Illness) Medication planning prior to pregnancy and commenced as soon as pregnancy confirmed27 Primary care statutory and voluntary sector providers in conjunction with specialist services such as perinatal psychiatry Examples 16 Roots of Empathy •Canadian developed, school-based programme where a mother and baby visit a class weekly, outcomes include an increasing social and emotional knowledge, decreasing aggression and increasing prosocial behaviour e.g. sharing, helping and including. 14 Current RCT by Queens University Belfast (Sept11Dec15) Kooth.com Warwickshire website •Warwickshire website: offers online counselling, support and advice to children and young people on a variety of issues Childline •Free 24hr counselling service, support with issues which cause distress or concern to children and young people including child abuse, bullying, depression, substance misuse, parental separation and pregnancy Spring Fever •Lessons on relationships and sexuality in primary schools has been found to promote knowledge and enhance pupil assertiveness 9 17 Overview of the Infant Mental Health Pathway: Antenatal Aims 1. Promote and prepare men and women for a healthy emotional transition to parenthood 2. Support parents to understand the emotional and developing needs of their infant 3. Promote parental mental health 4. Identify and support parents with additional needs (Universal Plus and Universal Partnership Plus services) Objectives Promote and prepare men and women for a healthy emotional transition to parenthood Support emotional preparation for parenthood Support development of new roles Increase knowledge about the parent-infant relationship and early development of foetus and baby Develop communication and conflict resolution skills Support parents to understand the emotional and developing needs of their infant Promote bonding by increasing reflective function Promote parental mental health Prevent anxiety and depression Support healthy couple relationships Support development of social networks Identify and support parents with additional needs Identify parents with Universal Plus level needs (e.g. anxiety/depression, unwanted pregnancy, learning or physical disability, lack of social support, care leavers etc.) Identify parents with Partnership Plus needs (e.g. unresolved loss, substance dependence, severe mental illness, domestic abuse) Infant Mental Health Pathway: Antenatal Aims 1. 2. 3. 4. Promote and prepare men and women for a healthy emotional transition to parenthood Support parents to understand the emotional and developing needs of their infant Promote parental mental health Identify and support parents with additional needs (Universal Plus and Universal Partnership Plus services) 1. Promote and prepare men and women for a healthy emotional transition to parenthood Support development of new roles Support emotional preparation for parenthood Increase knowledge about the parent-infant relationship and early development of the foetus and baby Develop communication and conflict resolution skills Interventions Who /When Routine Antenatal Care (e.g. Health and social care assessment of needs, risk and choices) Support mothers (and fathers where possible) in the transition to parenthood and in the promotion of bonding and attachment.28 Encourage mothers and fathers to reflect on their developing baby and what their unborn baby may be like Midwives, health visitors medical staff, allied health professionals, children’s centre staff Promote parental wellbeing (e.g. Encourage ‘mindfulness’,29 promote relaxation, address anxiety and depression, support healthy couple relationships, support the development of social networks 19 Support the role of fathers - engage and promote the role of the father30,31 Signposting to information and services as appropriate Resources: Maternal Emotional Wellbeing and Infant Development: A Good Practice Guide for Midwives32 Healthy habits for baby and you33 Apps (e.g. Getting to Know your Baby34, Best Beginnings35 Bump to Breastfeeding NCT online information and resources ) Antenatal Clinics Midwifery clinics in children’s centre Antenatal Promotional Guide 36 (28 weeks) to identify women with additional needs (e.g. anxiety/depression; domestic abuse; substance dependency) Midwives to inform heath visitors of pregnancy (follow-up with information as necessary i.e. change of pregnancy status) and health visitor to conduct interview using the Promotional Guide and inform midwives of named health visitor team Midwives, health visitors, children’s centre Staff Health visitor Antenatal Preparation for Parenthood Programmes Offered to all parents, but particularly first time parents.37 Programmes should include the ‘transition to parenthood’, getting to know your unborn baby and negotiating new roles in addition to physical aspects of pregnancy. For example: Universal programmes: Pregnancy, Birth and Beyond: Resource pack for all providers of antenatal education38 Solihull Approach antenatal course39 National Childbirth Trust (NCT) 40 Midwives/health visitors, children’s centre Staff 20 Mellow Bumps41 Voluntary sector Targeted programmes: Baby Steps (NSPCC)42 Nurturing Parents Programme (PEEP)43 Voluntary sector Practitioner training in supporting couple relationships One Plus One – Relationship Support (Brief Encounters)Training44 Solihull Approach45 Infant Mental Health (IMH) Champions Practitioner with ‘Perinatal and Infant Mental Health’ training to provide an advisory service to colleagues; liaise with specialist mental health services; cascade training to others and provide on-going support and motivation Health professionals and children’s centre practitioners Midwives, health visitors, children’s centre staff Unicef Baby Friendly Accreditation46 47 Breast feeding coordinators in post, promotion of breastfeeding advice and support Breastfeeding buddies48 Midwives, health visitors, medical staff, allied health professionals, children’s centre staff 2. Support parents to understand the emotional and developing needs of their infant Promote bonding by increasing parental reflective function: Getting to Know Your Baby app and website34 58 Bookstart - reading to bump 36 Antenatal Promotional Guide Midwives, health visitors, children’s centre staff 21 3. Promote parental mental health Prevent anxiety and depression Support healthy couple relationships Support development of social networks Practitioner training in supporting couple relationships – see above Antenatal Promotional Guide - see above Group-based Programmes Mindfulness-based Stress-Based Reduction Programmes in Pregnancy Health visitors 49 31 Trained midwife, health visitor, voluntary sector staff Antenatal Preparation for Parenthood Programme - see above 4. Identify and support parents with additional needs Identify parents with Universal Plus level needs (e.g. anxiety/depression, unwanted pregnancy, learning or physical disability, lack of social support, care leavers etc.) Identify parents with Partnership Plus needs (e.g. unresolved loss, substance dependence, severe mental illness, domestic abuse) Identification of women in need of additional support Midwifery screening at booking-in Health visitor Antenatal Promotional Guide - see above Midwife, health visitor Referral pathways for women with additional needs Universal Plus Additional visits by health visitor/midwives As appropriate via midwives, health visitors, GP 22 Group-based support (see above) Family Nurse Partnership50 51 Universal Partnership Plus Domestic abuse support worker Substance/alcohol misuse worker; Parents Under Pressure Programme52 Perinatal psychiatrist/psychologist/CPN/crisis team IAPT (Improving Access to Psychological Therapies) Specialist practitioners in NHS and voluntary sector 1. Identify and support parents with additional needs 23 Examples of good practice: Solihull Approach • Solihull Approach Antenatal course: antenatal parenting group consisting of five-session course for mothers, fathers, partners, birth partners and grandparents National Childbirth Trust (NCT) • Voluntary sector service providing comprehensive antenatal education and support. Available nationally PEEP (Parents Early Education Partnership) • Nurturing Parents programme. A targeted programme for first time parents based based on the concept of Reflective Function. Pilot study currently underway Pregnancy , Birth and Beyond • Online framework for the delivery of antenatal education. Consists of a resource pack for leaders of community groups and activities.It covers the physiological aspects of pregnancy and birth, but also addresses the emotional transition to parenthood in greater depth and recognises the need to include fathers and other partners in groups and activities stic abuse) Overview of the Infant Mental Health Pathway: Postnatal to 1 Year Aims 1. Support parents to provide an environment that fosters the infant’s emotional, behavioural, social and cognitive development 2. Promote continued healthy social and emotional transition to parenthood 3. Promote parental mental health 4. Identify parents in need of additional support (Universal Plus and Partnership Plus services) Objectives Support parents to provide an environment that fosters the infant’s emotional, behavioural, social and cognitive development Promote continued healthy social and emotional transition to parenthood Support the development of new roles Prepare men and women for the social changes and emotional challenges of the transition to parenthood Development of communication and conflict resolution skills Promote parental mental health Promote parent-infant interaction that is sensitive/attuned and high in reflective function Promote secure attachment Encourage mental wellbeing Support healthy couple relationships Support the development of social networks Identify mental health problems early and create a culture where parents are confident to seek help Identify parents in need of additional support Identify parents with Universal Plus level needs (e.g. anxiety/depression, unwanted pregnancy, learning or physical disability, lack of social support, care leavers etc) Identify parents with Partnership Plus needs (e.g. unresolved loss, substance dependence, severe mental illness, domestic abuse) Infant Mental Health Pathway: Postnatal to 1 year Aims 1. Support parents to provide an environment that fosters the infant’s emotional, behavioural, social and cognitive development 2. Promote continued healthy social and emotional transition to parenthood 3. Promote parental mental health 4. Identify parents in need of additional support (Universal Plus and Partnership Plus services) 1. Support parents to provide an environment which fosters the infant’s emotional, behavioural, social and cognitive development Promote parent-infant interaction that is sensitive/attuned and high in reflective function Promote secure attachment Interventions Who Unicef Baby-Friendly hospital Baby to breast following delivery Skin-to-skin care post delivery Midwives in delivery suite Promotion of parent-infant interaction Skin-to-skin contact 53 Infant carriers54 Breastfeeding support55 Cues-based infant massage programmes56 57 Midwives, health visitors, children’s centre practitioners, GPs References Introduce the social baby using media-based resources Getting to know your Baby’ app34 for parents and website for professionals. Social baby book and DVD58 Zero to Three ‘Healthy Minds’ resources 59 Baby Express newsletter57 Standardized tools to teach parents about the social baby (e.g. Brazleton Neonatal Behavioural Assessment Scale60 and Newborn Behavioral Observations (NBO) system61 Promoting early learning and home learning environment Health visitors, children’s centre practitioners, early years librarians PEEP62 Baby express63 Bookstart64 Temperament-based anticipatory guidance65 Midwives and health visitors, at every postnatal contact Bath and bedtime routines Inform parents about available resources 66 NHS Information Service for Parents Netmums67 online support group for parents Family Information Service, Local services (i.e. Warwickshire County Council)68 Midwives, health visitors, children’s centre practitioners, GPs Promote secure infant attachment Promote parental reflective function Train practitioners to ‘model’ reflective parenting (Universal) Provided jointly by NHS, Department of Health and Department for Education Voluntary sector Primary care, children’s centre and voluntary sector staff who have been 27 References Minding the Baby Programme (e.g. NSPCC)69 (Targeted) Nurturing Parents Programme (e.g. PEEP)43 (Targeted) trained to deliver these methods of working Promote ‘Secure Base’ parenting Train practitioners to ‘model’ secure base behaviour (Universal) Circle of Security programme70 (Targeted) Specialist intervention for parent-infant relationship difficulties Video-interaction guidance71 72 (Targeted) Parent-infant psychotherapy (i.e. Watch, Wait and Wonder73) 2. Promote continued healthy social and emotional transition to parenthood Support the development of new roles Prepare men and women for the social changes and emotional challenges of the transition to parenthood Development of communication and conflict resolution skills Promote continued attendance of antenatal/ postnatal transition to parenthood classes (see above) Support fathers Dads groups Infant massage groups for dads Support for couple relationships One Plus One – Brief Encounters44 Support development of social networks Invitation to attend infant massage group Children’s centre activities Midwives, health visitors, children’s centre practitioners, GPs 28 References 3. Promote parental mental health Support mental wellbeing Support healthy couple relationships Support the development of social networks Identify mental health problems early and create a culture where parents are confident to seek help Support mental wellbeing Teach ‘mindfulness’ skills or invite to stress reduction groups Encourage parent ‘special time’ for self Encourage the use of relaxation techniques Midwives, health visitors, children’s centre practitioners, GPs Support for healthy couple relationships Voluntary sector 44 One Plus One - Brief Encounters Support development of social networks Invite to attend infant massage group Encourage to attend children’s centre activities Midwives, health visitors, children’s centre practitioners, GPs 4. Identify parents in need of additional support (Universal Plus and Partnership Plus services) Identify parents with Universal Plus level needs (e.g. anxiety/depression, unwanted pregnancy, learning or physical disability, lack of social support, care leavers etc.) Identify parents with Partnership Plus needs (e.g. unresolved loss; substance dependence; severe mental illness; domestic abuse) Postnatal Interview using the Promotional Guide36 (includes Whooley questions) Screen parent-infant interaction Health visitor at 8 weeks 29 References Parent-Infant Interaction Observation Scale (PIIOS)74 Ages and Stages Questionnaire75 Support mental wellbeing Health visitors, children’s centre practitioners, GPs Teach ‘mindfulness’ skills or invite to stress reduction groups Encourage parent ‘special time’ for self Encourage the use of relaxation techniques Support for healthy couple relationships One Plus One44 Support development of social networks Invite to attend infant massage group Encourage to attend children’s centre activities Use of local voluntary sector services to support families (i.e. the national charity Home-Start76) Voluntary sector Health visitors, children’s centre practitioners Voluntary sector services 4. Identify parents in need of additional support Identify parents with Universal Plus level needs (e.g. anxiety/depression; unwanted pregnancy; learning or physical disability, lack of social support, Care leavers, etc.) Identify parents with Partnership Plus needs (e.g. unresolved loss; substance dependence; severe mental illness; domestic abuse) Identification of strategies as above Referral pathways for women with additional needs Universal Plus Additional visits by health visitor/midwives Health visitors and midwives refer through GPs to specialist perinatal 30 References Group-based support (see above) Family Nurse Partnership49,50 Universal Partnership Plus Domestic abuse support worker Substance/alcohol dependency worker; Parents Under Pressure IAPT (Improving Access to Psychological Therapies) National counselling service for parents with Anxiety and Depression Access to a specialist perinatal and infant mental health services (e.g. Mother and Baby In-Patient and Day Units; parent-infant psychotherapy; Perinatal psychologist. mental health services Referrals may be made directly to IAPT services. Women may also self-refer to IAPT services Specialist mental health practitioners (e.g. psychologist; psychiatrists etc.). 31 References Examples: The Neonatal Behavioural Assessment Scale (NBAS) •The NBAS is is a neuro-behavioural assessment of the newborn, designed to document the newborn's contribution to the parentinfant system, the competencies and individual differences of the newborn, as well as any difficulties. The main feature of the NBAS is that it is an interactive assessment, which gives a clear profile of the baby's behaviour, and how it must feel to parent the infant. •Britt GC and Myers BJ (1994) The effects of Brazelton intervention: a review. Infant Mental Health Journal, 15, 278-292 Newborn Behavioural Observations Systems Training (NBO) •Use of the Newborn Behavioural Observations Systems Training (NBO) The NBO is a relationship-building tool between practitioner and parent, that supports the developing parent-infant relationship, and provides an introduction to their infant’s behaviour. 'Getting to know your baby’ app and website •APP/website for Health visitors/other practitioners to use with parents who are pregnant or with babies under 6 months to enhance appropriate parent infant interaction. Video Interaction Guidance (VIG) •A Relationship-Based Intervention to help improve communication and interaction, promote empathy and wellbeing.Video interaction guidance is an intervention through which a “guider” aims to enhance communication within relationships. It works by engaging clients actively in a process of change towards realizing their own hopes for a better future in their relationships with others who are important to them. Guiders are themselves guided by the values and beliefs around respect and empowerment. The Tavistock 'Under Fives' infant mental health service •The service is for parents and babies or toddlers who are struggling with the ordinary problems of development. Services are delivered to those who have a worry relating to their baby or young child, whether it is temporary or long standing, major or minor. A variety of talking therapies may be offered. (http://www.tavistockandportman.nhs.uk/underfivesmentalhealthservice) 32 References Examples continued: Mellow Babies •Mellow Babies programme has undergone a randomized waiting list controlled trial. Clinically and statistically significant positive effects on maternal depression and Mother child interaction Parents Under Pressure •Parents with drug or alcohol misuse, who have a child under 2 in their care receive a 20 week programme which aims to support family functioning, develop parenting skills and caring relationships with infants Minding the Baby •NSPCC delivered intensive home visiting programme for vulnerable and at risk first time mothers under 25 and their babies. Delivered by social workers and health staff. Currently being evaluated. Video Interactive Guidance (VIG) •Fukkink, R. G. (2008). Video feedback in widescreen: A meta-analysis of family programs Clinical Psychology Review 28(6): 904-916. 33 References Section 3: References 1 Marmot M. (2010) Fair Society, Healthy Lives: strategic Review of health Inequalities in England Post 2010. London: Marmot Review 2 Shonkoff JP, Boyce WT, McEwen BS. (2009) Neuroscience, Molecular Biology and the Childhood Roots of Health disparities: Building a New Framework for Health promotion and Disease Prevention. JAMA 301; 21: 2252-2259 3 Knapp M, McDaid M and Parsonage M (2011) Mental Health Promotion and Prevention: The Economic Case. Department of Health, London. 4 DH. (2009). Healthy Child Programme: Pregnancy and the first five years of life. London: Department of Health 5 Department of Health. (2011). Health Visitor Implementation Plan - A Call to Action. London: Stationery Office 6 Munro, E. (2011). The Munro Review of Child Protection: Final Report. A child-centred system. London: Department for Education 7 DoH. (2011). No health without mental health. A cross government mental health outcomes strategy for people of all ages. London: Department of Health 8 Wallbank S, Hatton, S. (2011). Reducing burnout and stress: the effectiveness of clinical supervision. Community Practitioner, 84(7), 31- 35 9 Leadsom A, Field F, Burstow, P & Lucas, C (September 2013 ). The 1,001 critical days: the importance of the conception to age two period: a cross party manifesto. London: DH. 10 Evaluation of the Spring Fever programme. Rutgers WPF and CPS. An evaluation of the programme used in upper primary school. Accessed at http://www.rutgerswpf.org 11 Safeline – surviving abuse. http://www.safeline.org.uk/ 12 Healthy schools. Department for Education. (webpage) http://www.education.gov.uk/schools/pupilsupport/pastoralcare/a0075278/healthy-schools: 13 Farrington D, Ttofi M. (2009) Campbell Systematic Reviews. School based programs to reduce bullying and victimization. 14 Evaluation of the Spring Fever programme. Rutgers WPF and CPS. An evaluation of the programme used in upper primary school. Accessed at http://www.rutgerswpf.org 15 Santos R.G., Chartier M.J., Whalen, J.C., Chateau D., Boyd L. Effectiveness of the Roots of Empathy (ROE) Program in Preventing Aggression and Promoting Prosocial Behavior: Results from a Cluster Randomized Controlled Trial in Manitoba. Poster presented at the Banff Conference on Behavioral Sciences, Banff, March 2008. 34 References 16 DfES (2006) Teenage Pregnancy Next Steps: Guidance for Local Authorities and Primary Care Trusts on Effective Delivery of Local Strategies. London 17 Safeline – surviving abuse. http://www.safeline.org.uk/ 18 One Plus One On line support and training. The Couple Connexion. http://thecoupleconnection.net/ 19 Kooth. Online counselling. http://www.Kooth.com 20 Kooth. Online counselling. http://www.Kooth.com 21 NSPCC. Online support for parents http://www.nspcc.org.uk/help-and-advice/for-parents/for-parents-hub_wda96726.html 22 Foresight. http://www.foresight-preconception.org.uk 23 One Plus One On line support and training. The Couple Connexion. http://thecoupleconnection.net/ 24 NICE/SCIE ‘Promoting the quality of life of looked-after children and young people’ accessed online http:// www.nice.org.uk/guidance/PH28 25 Fauth, R., Hart, D., & Payne, L. (2012). Supporting Care Leavers' sucessful transition to independent living. NCB Research Centre, London: National Childrens's Bureau. 26 MIND, A civilised society: Mental health provision for refugees and asylum-seekers in England and Wales, 2009 (Report accessed online at http://www.mind.org.uk/assets/0000/5695/refugee_report_2.pdf) 27 Gregoire, A (2004) Maternal Mortality and Mental Health: Challenges and Solutions. Conference presentation 28 Barlow, J., & Underdown, A. (2007). The transition to parenthood: the role of the health visitor. In M. Bannon & Y. Carter (Eds.), Practical Paediatric Problems in Primary Care. Oxford: Oxford University Press. 29 Vieten, C., & Astin, J. (2008). Effects of a mindfulness- based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Archives of Womens Health 11, 67-74. 30 Magill-Evans, J., Harrison, M. J., Rempel, G., & Slater, L. (2006). Interventions with fathers of young children: systematic literature review. Journal of Advanced Nursing, 55(2), 248-264. 31 Ferguson, H., & Gates, P. (2013). Early intervention and holistic, relationship-based practice with fathers: evidence from the work of the Family Nurse 35 References Partnership. Child & Family Social Work 32 Underdown, A, & Barlow, J. (2012). Maternal Emotional Wellbeing and Infant Development. In RCM (Ed.). London: Royal College Midwives Trust. 33 DH. Healthy habits for baby and you (2012) available for health professionals to order online. http://www.nhs.uk/start4life 34 Getting to Know your Baby App and Website: http://www.your-baby.org.uk 35 Best Beginnings. www.bestbeginnings.org.uk/ 36 Purra, K, Davis , H, Mantymaa, M, Tamminen, T, & Roberts, R. (2005). The Outcome of the European Early promotion Project. Mother child interaction The International Journal of Mental Health Promotion, 7(1), 82 - 94. 37 NICE: (2007) Guidelines on Antenatal and Postnatal Mental Health. London: DoH 38 DH (2011) Preparation for Birth and Beyond: resource pack for those providing parenthood groups. London. 39 Solihull Approach www.solihullapproachparenting.com 40 NCT, Online resources http://www.nct.org.uk. 41 Mellow Bumps. Mellow parenting. http://www.mellowparenting.org 42 Baby Steps. National Society Prevention Cruelty to Children. http://www.nspcc.org.uk 43 Nurturing Parents Programme. Peers Early Education Programme (PEEP) http://www.peep.org.uk 44 One Plus One – Supporting couple relationships. http://www.oneplusone.org.uk 45 Solihull Approach http://www.solihullapproachparenting.com 46 Bartington S, Griffiths L, Tate A, Dezateux C and the Millennium Cohort Study Child Health Group.(2006) Are breastfeeding rates higher among mothers delivering in Baby Friendly accredited maternity units in the UK? International Journal of Epidemiology 47 Broadfoot M, Britten J, Tappin DM and MackKenzie JM. The Baby Friendly Initiative and breastfeeding rates in Scotland. (2005) Archives of Disease on Childhood Fetal & Neonatal Edition. 90:114-116 36 References 48 Dyson, L, Renfrew, M, McFadden, A, McCormick, F, Herbert, G, & Thomas, J. (July 2006). Promotion of breastfeeding initiation and duration. Evidence into practice briefing: HDA. 49 Vieten, C., & Astin, J. (2008). Effects of a mindfulness- based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Archives of Womens Health 11, 67-74. 50 Barnes, J et al (2009) Nurse-Family Partnership Programme: Implementation in England – Second Year in 10 Pilot Sites: the infancy period. London DCSF. 51 Barnes, J., Ball, M., Meadows P., Howden, B., Jackson, A., Henderson, J., and Niven, L., (2011) The Family Nurse Partnership Programme in England: Wave 1 Implementation in toddlerhood and a comparison between Waves 1 and 2a implementation in pregnancy and infancy. London, Department of Health 52 Dawe, S., & Harnett, P. (2007). Reducing potential for child abuse among methadone-maintained parents: Results from a randomized controlled trial. Journal of Substance Abuse Treatment, 32(4), 381-390. 53 Puig G, Sguassero Y. Early skin-to-skin contact for mothers and their healthy newborn infants: RHL commentary (last revised: 9 November 2007). The WHO Reproductive Health Library; Geneva: World Health Organization 54 Anisfeld, E., Casper, V., Nozyce, M., & Cunningham, N. (1990). Does Infant Carrying Promote Attachment? An Experimental Study of the Effects of Increased Physical Contact on the Development of Attachment. Child Development, 61(5), 1617-1627 55 Dyson, L., Renfrew, M., McFadden, A., McCormick, F., Herbert, G., & THomas, J. (July 2006). Promotion of breastfeeding initiation and duration. London. National Institute for Health and Clinical Excellence 56 Underdown A, Barlow J, Chung V, & Stewart-Brown S (2006).Massage intervention for promoting mental and physical health in infants aged under six months. Cochrane Database of Systematic Reviews 2007 (4). 57 Underdown A. (2011) Interventions to support early relationships: mechanisms identified within infant massage programmes. Community Practitioner. 2011;84(4):21-6 58 Murray, L., & Andrews, L. (2000). The Social Baby: Understanding Babies Communication from Birth. Richmond, UK: CP Publishing. 59 Zero to Three Healthy Minds resources for parents. Downloadable from http://www.zerotothree.org/ 60 Eiden RD & Reifman A (1996). Effects of Brazelton Demonstrations on Later Parenting: A Meta-Analysis. Journal of Paediatric Psychology 21(6):857-868. 61 The Newborn Behavioral Observations (NBO) System. http://www.brazleton.co.uk 37 References 62 Parents Early Education Partnership (PEEP) http://www.peep.org.uk/ 63 Baby Express. http://www.thechildrensfoundation.co.uk/baby-express.php 64 Bookstart. http://www.bookstart.org.uk 65 Cameron J R & Rice DC (1986). Developing Anticipatory Guidance Programs Based on Early Assessment of Infant Temperament: Two Tests of a Prevention Model. Journal of Paediatric Psychology, 11(2), 221-234. doi: 10.1093/jpepsy/11.2.221 66 NHS Information Service for Parents www.nhs.uk/InformationServiceForParents/pages/home.aspx. 67 Netmums http://www.netmums.com 68 Warwickshire Family Information Service. www.warwickshire.gov.uk/fis 69 Minding the Baby. NSPCC. www.nspcc.org.uk/Inform/resourcesforprofessionals/underones/minding_the_baby_wda85606.html 70 Circle of Security. Early intervention programme for parents and children. http://circleofsecurity.net/ 71 Video Interaction Guidance. NICE public health guidance: Social and emotional wellbeing: early years Issued: October 2012 72 Fukkink, R. G. (2008). Video feedback in widescreen: A meta-analysis of family programs Clinical Psychology Review 28(6): 904-916 73 Cohen, NJ., Muir, E., Lojkasek M., Muir R., Parker CJ., Barwick M., & Brown M. (1999). Watch, wait, and wonder: Testing the effectiveness of a new approach to mother–infant psychotherapy. Infant Mental Health Journal, 20(4), 429-451 74 Svanberg, P. O., Barlow, J., & Tigbe, W. (2013). The Parent–Infant Interaction Observation Scale: reliability and validity of a screening tool. Journal of Reproductive and Infant Psychology, 31(1), 1-10 75 Ages and Stages Questionnaire: Social Emotional. Information available at http://www.brookespublishing.com/resource-center/screening-andassessment/asq/asq-se/. Briggs, Rahil D., Stettler, Erin M., Silver, Ellen Johnson, Schrag, Rebecca D. A., Nayak, Meghna, Chinitz, Susan, & Racine, Andrew D. (2012). SocialEmotional Screening for Infants and Toddlers in Primary Care. Pediatrics. doi: 10.1542/peds.2010-2211 76 Home-start. National charity supporting families with children 0-5years. Further information available http://www.home-start.org.uk/ 38