Hospitals as Insurers of Last Resort RAND March 16, 2015
advertisement

Hospitals as
Insurers of Last Resort
RAND
March 16, 2015
Craig Garthwaite
Northwestern University
and NBER
Tal Gross
Columbia University
and NBER
Matthew J. Notowidigdo
Northwestern University
and NBER
The Uninsured will still exist after
the ACA is fully implemented
25
20
15
10
5
0
2012
2014
2016
2018
2020
2022
The Uninsured will still exist after
the ACA is fully implemented
25
20
15
25 million newly insured
10
5
0
2012
2014
2016
2018
2020
2022
The Uninsured will still exist after
the ACA is fully implemented
25
20
15
25 million newly insured
10
5
30 million remain uninsured
0
2012
2014
2016
2018
2020
2022
“People have access to health care in
America. After all, you just go to an
emergency room.”
George W. Bush, July 2007.
Hospitals are required to provide the care
to the uninsured
1. Emergency Medical Treatment and Active
Labor Act (EMTALA)
2. Community-benefit standards for nonprofit hospitals
3. Medical ethics
Hospitals provide $54 billion in
uncompensated care each year
For Profit
Not For Profit
Public
0
10,000
20,000
30,000
Uncompensated costs in millions
40,000
The cost of uncompensated care
ought to inform policy decisions
• Typical analysis focuses on cost to the
government of covering the uninsured
• A portion of the cost to the government is
a transfer from private hospitals
This Paper’s Goals:
1. Measure how the size of the
uninsured population affects
uncompensated care.
2. Measure how the number of
providers in a local market affects
uncompensated care.
First Goal: Demand for
uncompensated care
• Estimate the relationship between share
uninsured and uncompensated care per
capita in a state
• Exploit two Medicaid disenrollments in
Tennessee and Missouri
Second Goal: Supply of
uncompensated care
Study how hospital closures affect:
– Uncompensated care costs
– Revenue
– Profits
Summary of Results
• Every additional uninsured person costs
hospitals $900.
• Hospital closures substantially increase
uncompensated care at neighboring
hospitals.
Outline
• Background
• First Goal: The uninsured and
uncompensated care
• Second Goal: Hospital closures and
uncompensated care
Outline
• Background
• First Goal: The uninsured and
uncompensated care
• Second Goal: Hospital closures and
uncompensated care
What do we already know about
uncompensated care?
• Correlates and trends in uncompensated care
(Mann et al., 1997; Cunningham and Tu, 1997)
• A few case studies (Blewett et al., 2003; APS
Healthcare, 2006)
• Two papers study the effect of Medicaid
eligibility and other variables on hospital
uncompensated care (Davidoff et al., 2000;
LoSasso and Seamster, 2007)
Related literature:
non-profits as “for-profits in disguise”
• A large literature examining differences
between for-profits and non-profits
(Weisbrod 1988; Sloan and Vraciu 1983;
Duggan 2001; Dranove, Garthwaite, and
Ody 2014).
• Our finding that non-profits react differently
than for-profits to changes in share uninsured
suggests that non-profits are not simply “forprofits in disguise.”
Related literature:
Crowdout of private charity
• Recent work examines how government
spending affects private charity
(Hungerman 2004; Gruber and
Hungerman 2005).
• Our results suggest a potentially large
amount of crowdout of private charity by
public health insurance programs.
Related literature:
Third parties in social insurance
• Recent work on third parties in social
insurance:
– IRS tax prep (Kopczuk and Pop-Eleches 2007)
– WIC and grocery stores (Meckel 2014)
• Our work emphasizes the role of hospitals
in providing social insurance in their role as
“insurers of last resort.”
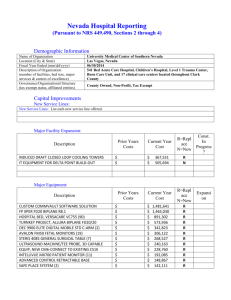
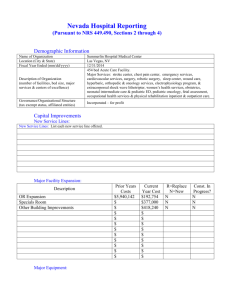
Primary data set in this paper
• Data-use agreement with AHA to use
previously confidential hospital-level
financial data from 1984–2011
• We combine this data with rich financial
and non-financial data available in the
public-use AHA data set (e.g., revenue,
expenditures, admissions, beds, etc.)
Uncompensated care represents
roughly five percent of hospital
Figure 1. Uncompensated
Care Cost Shares, 1984–2011
expenditures
A. All Hospitals
.07
.06
Uncompensated
costs as share
of expenditures
.05
.04
.03
1984
1988
1992
1996
Year
2000
2004
2008
2012
.03
For government hospitals, 7
percent
1984
1988
1992
1996
Year
2000
2004
2008
2012
B. By Hospital Type
.1
Government
hospitals
.08
Uncompensated
costs as share
of expenditures
Not-for-profit
hospitals
.06
.04
For-profit
hospitals
.02
1984
1988
1992
1996
Year
2000
2004
2008
2012
Non-profit hospitals provide a
disproportionate amount of this care
For Profit
Government
Not For Profit
Cost Share
Hospital Share
Cost Share
Hospital Share
Cost Share
Hospital Share
0
.2
.4
Uncompensated costs in millions
.6
Additional Data
1. March Current Population Survey to measure
uninsured population (for state-year panel
analysis) and other state-level demographic
information.
2. For Tennessee, we have compiled Joint
Annual Reports (JAR) data for each hospital in
the state for several years.
Correlation between uncompensated care
in AHA data and JAR data
Measuring uncompensated care
• Uncompensated care comes in two
forms:
1. Bad debt
2. Charity care
• We adjust uncompensated care charges
using a hospital-level cost-to-charge
ratio
Outline
• Background
• First Goal: The uninsured and
uncompensated care
• Second Goal: Hospital closures and
uncompensated care
We take several approaches to isolate
the causal effect of the uninsured on
uncompensated care
1. Simple cross-sectional relationship
2. State-by-year panel regression analysis
3. Missouri case study
4. Tennessee case study
Uncompensated
care
per
capita,
Figure 2. Share Uninsured and Uncompensated Care Costs
2000 cross-section
A. 2000 Cross Section
800
DC
700
600
500
Uncompensated
care per capita
TX
FL LA
NJ
400
ALAR
MS
SC OK
GA
NV
IL NC
NYWV
MA
KY
TN
CO
OH
MO
KS
VA
WY
IN
PA
ME
MI
RI CT NH
AK
ND
MD
MT
DEHI
UT
IA
ID
NE VT
MN
WA
WI
SD
OR
300
200
100
NM
CA
AZ
0
.04
.08
.12
.16
.2
Share uninsured
.24
.28
.32
0
.04
.08
.12
.16
.2
Share uninsured
.24
.28
Uncompensated care per capital,
2000–2005 first
differences
B. 2000–2005
Changes
NJ
400
350
NV
TX
FL
300
Change in
uncompensated
care per capita
.32
CO
SC
250
MS
200
AKAL
KY
NH
OHVA
MA
NM
150
DC
CA
100
AZ
NY
MECT
50
HI
0
-.04
-.02
0
OR IN
RI
TN
LA
AR
GA
WA WV
NC
NE
MO
PA
MT
ILSD
WY
IA
WI
DE
UTMN
ID MI VT
KS
OK
MD
ND
.02
.04
Change in share uninsured
.06
.08
.1
Dependent Variable: Per-Capita Uncompensated Care Costs
Share of Population
Insured
R2
Share of Population
Insured
R2
Share of Population
Insured
(1)
(2)
(3)
1990
cross-section
1995
cross-section
2000
cross-section
A. All Hospitals
-$456.05
-$555.13
(107.28)
(224.50)
[0.000]
[0.016]
-$558.83
(154.99)
[0.001]
0.27
0.11
B. Hospitals with an ER
-$439.99
-$411.54
(102.21)
(215.53)
[0.000]
[0.022]
0.27
0.10
C. Hospitals without an ER
-$14.61
-$41.96
(9.86)
(13.06)
[0.145]
[0.002]
0.21
-$511.78
(151.63)
[0.001]
0.19
-$47.06
(19.06)
[0.017]
0.04
0.18
0.11
R2
Notes: N = 51. Robust standard errors in parentheses; associated p-values
in brackets.
Fixed-effects estimates
OLS regression for state-by-year descriptive approach:
yst = ↵s + ↵t +
· Percent Insuredst +
· Xst + "st
ssee across-state approach:
yst = ↵s + ↵t + ↵s · t +
· I{t
2006}st · I{ Tennessee}s + "st
n-Tennessee approach:
rt
= ↵r + ↵t +
2004–2005 change in enrollment
· Post 2005 ·
+"
2004 Population
Dependent Variable: Per-Capita Uncompensated Care Costs
Share of
Population
Insured
R2
Share of
Population
Insured
(1)
(2)
(3)
All Hospitals
Hospitals with an ER
Hospitals with no ER
A. State Fixed Effects and Year Fixed Effects
- 584.00
- 551.00
(174.00)
(158.00)
[0.00]
[0.00]
0.889
0.897
- 33.00
(27.36)
[0.23]
0.255
B. State Fixed Effects, Year Fixed Effects, and Region-by-Year Fixed Effects
- 608.00
- 577.00
- 31.20
(189.00)
(178.00)
(21.28)
[0.00]
[0.00]
[0.15]
R2
0.906
0.914
0.323
N
1,224
1,224
1,200
Notes: The standard errors in parentheses are robust to auto-corrleation between observations from the same
state; associated p-values in brackets.
Dependent Variable: Per-Capita Uncompensated Care Costs
(4)
(5)
(6)
Non-Profit Hospitals
All with an ER
Share of Population
Insured
R2
Share of Population
Insured
- 320.00
(71.01)
[0.00]
0.882
(7)
(8)
(9)
For-Profit Hospitals
All with an ER
No ER
A. State Fixed Effects and Year Fixed Effects
- 329.00
9.52
36.42
53.00
(73.49)
(12.88)
(64.78)
(64.24)
[0.00]
[0.46]
[0.58]
[0.41]
4.24
(4.67)
[0.37]
0.878
No ER
0.585
0.695
0.690
0.361
B. State Fixed Effects, Year Fixed Effects, and Region-by-Year Fixed Effects
- 390.00
- 402.00
15.94
65.63
72.33
3.92
(90.19)
(92.74)
(18.49)
(66.70)
(62.48)
(5.57)
[0.00]
[0.00]
[0.39]
[0.33]
[0.25]
[0.48]
R2
0.904
0.900
0.651
0.806
0.807
0.471
N
1,224
1,224
1,060
1,161
1,050
1,075
Notes: The standard errors in parentheses are robust to auto-corrleation between observations from the
same state; associated p-values in brackets.
One for-profit hospital chain’s policy
towards uncompensated care
“HCA decided not to treat patients who came in
with non-urgent conditions, like a cold or the flu…
unless those patients paid in advance… HCA said
that… about 1.3 percent [of patients], ‘chose to seek
alternative care options.’”
New York Times
August 14, 2012
Summary of fixed-effects panel
estimates
• Strong association between the share of
the population with health insurance and
hospital uncompensated care costs.
• Overall association is primarily accounted
for by non-profit hospitals with an ER.
Case Study #1: Missouri Medicaid
Disenrollment
• Due to budget shortfall, Missouri dropped
150,000 residents from Medicaid and
SCHIP (Zuckerman, Miller, and Pape,
2009)
• Benefit: Sharp change in share uninsured
in the state.
• Drawback: Limited regional variation
within Missouri.
Ways that Missouri Cut Eligibility
1. Income limits for parents went from 75 percent of FPL
to 22 percent of FPL
2. Increased premiums for children in families earning
more than 150 percent of FPL
3. Families ineligible for SCHIP if they earned more than
150 percent of FPL and had access to employerprovided insurance
4. Eliminating the Medicaid Assistance for Workers with
Disabilities program
5. Creating an annual reinvestigation program to ensure
eligibility
Difference-in-Difference regression
LS regression for state-by-year
descriptive approach:
model
yst = ↵s + ↵t +
· Percent Insuredst +
· Xst + "st
across-state approach:
yst = ↵s + ↵t +
· I{t
2006}st · I{Missouri}s + "st
ee across-state approach:
yst = ↵s + ↵t +
· I{t
2006}st · I{Tennessee}s + "st
Tennessee approach:
= ↵r + ↵t +
· Post 2005 ·
2004–2005 change in enrollment
+
Uncompensated Care Costs
Dependent Variable: The logarithm of uncompensated costs in each state and year
Hospitals:
Missouri × Post 2005
Avg. uncompensated costs in
millions in Missouri, 2000–2005
(1)
(2)
(3)
All
Non-Profit
For-Profit
0.171
(0.044)
[0.008]
0.139
(0.059)
[0.056]
0.003
(0.185)
[0.987]
471
335
60.6
N
56
56
Note: The standard errors in parantheses are robust to autocorellation between
observations from the same state; associated p-values in brackets.
24
Assuming 50-percent crowdout:
Assuming 0-percent crowdout:
A Simple Calibration Exercise
• Are our state-level fixed-effects panel
estimates and Missouri case study
estimates similar in magnitude?
• We examine predictions from these two
models for effect of the Affordable Care
Act
Panel regression estimate
$608 × 25 M = $15.2 B decrease
in uncompensated costs
across nation
CBO estimate of newly
insured due to ACA
($533 to $1,066) × 25 M = ($13.3 B to $25.8 B) decrease
in uncompensated costs
across nation
Range of estimates from
Missouri case study
Case Study #2: Tennessee
• In late 2005, the Tennessee government
removed 170,000 people from its
Medicaid program, TennCare
• Those who lost coverage were primarily
relatively high income, childless adults
“Uninsurable”
enrollees required to
undergo
“reverification.”
1994
...
2000
Tennessee
creates
expansion
program for
“uninsured” and
“uninsurable.”
2001
2002
2003
Phil Bredesen
elected governor
of Tennessee on
platform of
reforming
TennCare.
2004
2005
2006
2007
Over last three months of
2005, 170,000 TennCare
enrollees are taken off
program.
Similarities between
TennCare and the ACA
• The ACA primarily targets able-bodied, nonelderly, childless adults: 84% of those newly
eligible for Medicaid under the ACA are
childless adults (Kenney et al. 2012).
• Affects adults with incomes greater than 100%
of FPL.
1,300
Total
TennCare
Enrollment
in thousands
Medicaid
300
1,250
250
1,200
200
Uninsured
and Uninsurable
1,150
150
Uninsured
and
Uninsurable
Program
Enrollment
in thousands
Two Identification Strategies
1,100
Changes in TennCare Enrollment
by Tennessee Counties
100
Basic OLS regression
1,050for state-by-year descriptive approach:
50
1,000
0
2005q1
2006q3
2008q1
2009q3
yst = ↵s2003q3
+ ↵t +Changes
· Percent
Uninsured
in TennCare
Enrollment
st + "st
by Tennessee Counties
Note: This figure presents enrollment numbers reported in TennCare quarterly
reports. Tennessee disenrolled most of those in the Uninsured and Uninsurable
program in the last quarter of 2005.
Tennessee
approach:
1. across-state
Across States
yst = ↵s + ↵t + ↵s · t +
· I{t
2006}st · I{ Tennessee}s + "st
Within-Tennessee approach:
Appendix Figure A2. Changes in TennCare Enrollment by Tennessee Counties
2. Within
Tennessee2004–2005 change in enrollment
Change in TennCare Enrollment
yrt/ 2004
= Population
↵r + ↵t +
· Post 2005 ·
Percent
Change in Enrollment:
TennCare
-9.1 to 6.7
-0.090760
- -0.066990
-6.7 to -4.9
-0.066989
- -0.049500
-4.9 to -3.8
-0.049499
- -0.038090
-3.8 to -2.7
-0.038089
- -0.027750
-2.7 to -1.7
-0.027749
- -0.017190
-0.017189
- -0.006720
-1.7 to -0.7
-0.006719
- 0.025000
-0.7 to 2.5
2004 Population
Spillover analysis:
log(y)ct = ↵c + ↵t + 3 · I{3 years before closure}ct
Note: This+
map indicates
changes
in Medicaid
enrollment closure}
for each county in
years
before
2 · I{2
ct
Tennessee as reported in the 2004–2005 and 2005–2006 annual reports for
TennCare.
+ · · · + · I{2 years before closure} + "
+ "rt
Uncompensated Care Costs
Dependent Variable: The logarithm of uncompensated costs in each state and year
Hospitals
Tennessee × Post 2005
Avg. uncompensated costs in
millions in Tennessee, 2000–2005
(1)
(2)
(3)
All
Non-Profit
For-Profit
0.198
(0.026)
[0.000]
0.177
(0.043)
[0.001]
0.150
(0.092)
[0.123]
549.40
359.63
96.91
R2
0.996
0.993
N
136
136
Note: The standard errors in parentheses are robust to autocorellation between
observations from the same state; associated p-values in brackets.
0.991
136
Dollars vs. Visits
• One concern with AHA data is the financial
data may not represent actual changes in
utilization.
• In the Appendix, we show that our results
are robust to several alternative cost-tocharge ratio adjustments.
• We also supplement AHA data with
hospital encounter data from Joint Annual
Reports.
Note: This figure presents the number of charity-care admissions for patients from
two groups of counties, as recorded in the JAR data. We rank the patients’ counties
by the absolute size of the decrease in TennCare enrollments between 2004 and
2005. This figure compares the top 15 counties to the bottom 15 counties.
Share of Visits Self-Pay in JAR Data
Figure 6. Share of Tennessee Hospital Encounters that are Self-Pay, JAR Data
0.09
0.08
Share
self-pay
0.07
0.06
Linear projection
based on 2002–2005
0.05
2002
2003
2004
2005
2006
Note: This figure presents the share of hospital encounters (inpatient, ED, and
2007
Figure 7. Hospital Encounters in
Total
TennCare
Visits
A. TennCare Encounters
B. Self-
3.20
1.00
3.00
0.90
2.80
0.80
2.60
0.70
2.40
0.60
2002
2003
C. Private Encounters
2004
2005
2006
2007
2002
D. To
Encounters in Tennessee, JAR Data
Self-Pay Visits
B. Self-Pay Encounters
1.00
0.90
0.80
0.70
0.60
2007
2002
2003
D. Total Encounters
2004
2005
2006
2007
2.40
0.60
2002
2003
2004
2005
Private Visits
2006
2007
C. Private Encounters
2002
D. Tota
12.00
4.10
4.00
11.50
3.90
3.80
11.00
3.70
10.50
3.60
2002
2003
2004
2005
2006
2007
2002
Note: This figure presents the number of hospital encounters (ED vis
0.60
2007
2002
2003
D. Total Encounters
All visits
2004
2005
2006
2007
12.00
11.50
11.00
10.50
2007
2002
2003
2004
2005
encounters (ED visits, outpatient visits, and inpatient visits) at
2006
2007
We also study within-Tennessee
variation
Figure 8. Changes in Uncompensated Care Costs within Tennessee,
Before and After TennCare Disenrollment
1
.9
.8
Change
in uncompensated .7
care costs from
2004 and 2005 to .6
2006 and 2007
.5
.4
.3
.2
-.04
-.03
-.02
-.01
0
2004-2005 Change in TennCare enrollment divided by 2004 population
Note: This figure presents uncompensated care costs for the 14 health department
regions in Tennessee, as recorded in the AHA survey. See text for details.
Note: This figure presents uncompensated care costs for the 14 health department
regions in Tennessee, as recorded in the AHA survey. See text for details.
Figure 9. Changes in Uncompensated Care Costs within Tennessee, Before and After 2002
.3
.2
.1
Change
in uncompensated
care costs from
2000 and 2001 to
2002 and 2003
0
-.1
-.2
-.3
-.4
-.5
-.04
-.03
-.02
-.01
0
2004-2005 Change in TennCare enrollment divided by 2004 population
Note: This figure presents uncompensated care costs for the 14 health department
regions in Tennessee, as recorded in the AHA survey. See text for details.
Figure 6. Charity-Care Visits by Patients’ County of Residence
50,000
40,000
Number of
charity-care
admissions
Counties with
largest TennCare
enrollment cuts
30,000
20,000
Counties with
smallest TennCare
enrollment cuts
10,000
0
2002
2003
2004
2005
2006
Note: This figure presents the number of charity-care admissions for patients from
two groups of counties, as recorded in the JAR data. We rank the patients’ counties
by the absolute size of the decrease in TennCare enrollments between 2004 and
2005. This figure compares the top 15 counties to the bottom 15 counties.
Dependent Variable: The logarithm of uncompensated costs in each region and year
Hospitals
2004–2005 disenrollment in region
/ 2004 population × Post 2005
Estimates scaled by statewide
disenrollees per capita
(1)
(2)
All
Private
A. Within-Tennesse Estimates
- 6.713
(2.270)
[0.011]
0.175
- 6.787
(3.063)
[0.045]
0.177
0.981
R2
0.979
Note: Standard errors in parentheses are robust to autocorellation between observations from
the same region; associated p-values in brackets.
Dependent Variable: The logarithm of uncompensated costs in each region and year
Hospitals
2004–2005 de-enrollment in region
/ 2004 population × Post 2005
Estimates scaled by statewide
disenrollees per capita
(1)
(2)
All
Private
B. Within-Tennesse Estimates with Linear Trends
- 10.400
- 9.528
(4.954)
(6.200)
[0.056]
[0.148]
0.271
0.248
R2
0.984
0.986
Note: Standard errors in parentheses are robust to autocorellation between observations from
the same region; associated p-values in brackets.
Dependent Variable: The logarithm of uncompensated costs in each region and year
2004–2005 disenrollment in region
/ 2004 population × Post 2001
Estimates scaled by statewide
disenrollees per capita
(1)
(2)
C. Placebo Estimates Within-Tennesse (1997–2004)
1.103
0.442
(4.816)
(6.100)
[0.822]
[0.943]
-0.029
-0.012
R2
0.965
0.970
N
112
112
Note: Standard errors in parentheses are robust to autocorellation between observations from
the same region; associated p-values in brackets.
Summary of Results from
Tennessee
• The disenrollment led to an approximately
20 percent increase in uncompensated costs.
• The increase was concentrated in non-profit
hospitals.
• Increase in uncompensated care
concentrated in Tennessee regions most
exposed to the disenrollment.
How much does each TennCare
disenrollee cost hospitals?
Back-of-the-envelope calculation for Tennessee:
Regression
estimates
Pre-existing uncompensated
care costs in Tennessee
0.21 × $549 M
Increase in
uninsured
population
80,000
= $1,441 increase
in uncompensated costs
per uninsured person
What number should we take to
the ACA?
• Estimates we have:
– OLS: $608
– Missouri: $533 – $1,066
– Tennessee: $1,441
• Kenney et al. (2013) predict that 82% of
newly covered under ACA are in good
health.
• Midpoint of Missouri estimate × 0.82 +
Tennessee estimate × 0.18 ≈ $900
Outline
• Background
• First Goal: The uninsured and
uncompensated care
• Second Goal: Hospital closures and
uncompensated care
The supply of uncompensated care
• If the uninsured demand a minimum level
of care, and hospitals are “insurers of last
resort,” then a hospital’s uncompensated
care costs should be a function of the
number of firms in a market.
• Hospital closures should result in a large
shifting of these costs to remaining nearby
hospitals. We directly test for these
spillovers.
We next study spillovers of
uncompensated care across hospitals
• We assembled data from HHS on all
hospital closures from 1988–2000
• Limit to those markets with a single
closure in our data
Hospital Closed
Hospital Didn't Close
For Profit
0.19
0.26
Non-Profit
0.51
0.48
Public
0.30
0.26
Expenditures
$64,091,373
$14,988,942
Uncompensated Care
$4,164,360
$934,870
Revenue
$57,241,372
$14,217,787
-10.69%
-5.14%
0.84
0.96
Patient Margin
Has an ER
Change in number of hospitals in a
county
Uncompensated care in remaining
hospitals in a county
Total uncompensated care in
county
Summary of County Results
• A large reduction in uncompensated care
following a closure.
• Similar results come from an HSAs.
• These market definitions may be to small
to fully capture spillovers across hospitals.
• We next consider commuting zones.
Uncompensated care at remaining
hospitals in commuting zone
Total Uncompensated Care in
Commuting Zone
Uncompensated Care Costs at non-profit
hospitals that remain open
Uncompensated Care Costs at forprofit hospitals that remain open
Distribution of compensated care
(i.e. revenue)
• Costs are not the only spillover from a
closure
• The compensated care from insured
patients also moves to the remaining
hospitals
Revenue at remaining hospitals in a
commuting zone
Total revenue in commuting zone
Summary of Spillover Analysis
• Increase in uncompensated care costs at
surviving non-profit hospitals.
• No change in total uncompensated care
costs.
• A decrease in total revenue.
• This suggests that uncompensated care
represents a market-level fixed cost for the
local hospitals.
Can hospitals make up this lost
revenue?
• Unclear whether hospitals can make up
these costs by extracting revenue from
other sources or by cutting costs.
• We examine the relationship between the
share uninsured and hospital patient profit
margins:
(Net Patient Revenue – Total Expenses) / Net Patient
Revenue
Patient margins at remaining
hospitals
0.02
0.00
-0.02
-0.04
-0.06
-3
-2
-1
0
1
2
3
4
5
Patient margins at remaining nonprofit hospitals
0.01
0.00
-0.01
-0.02
-0.03
-3
-2
-1
0
1
2
3
4
5
Patient margins at remaining forprofit hospitals
0.01
0.01
0.01
0.00
-0.01
-0.01
-3
-2
-1
0
1
2
3
4
5
Conclusions
• Every uninsured person covered by the ACA
appears to have been costing hospitals
roughly $900 in uncompensated care
• Hospitals provide an additional form of social
insurance, acting as “insurers of last resort”
– Optimal social insurance policy should account
for this unique role
– More broadly, policy should account for spillover
effects on firms
Future work: how do hospitals
respond?
• Open question: How do hospitals absorb
increases in uncompensated care costs?
• Hospitals can pay for financial shocks through
different means:
– Raise prices, i.e. cost-shift
– Decreases costs, i.e. lower quality
– Close unprofitable services
• After a certain point, hospitals may have no more
options and close down
– We speculate that uncompensated care may have
played some role in ongoing decline in EDs in areas
with low rates of health insurance
The true cost of the ACA’s Medicaid
expansion
• Under the ACA, health insurance for those
below 138 percent of the poverty line was
supposed to be covered by Medicaid
• A 2012 Supreme Court decision allowed
states to opt out of this expansion
– Many states have taken them up on this option
– “Cost” is an oft-stated rationale
“Virginia simply cannot afford to become
the bank for a federally designed expansion
of Medicaid.”
-Governor Bob McDonnell
Towards an estimate of the
economic cost of not expanding
• Applying our estimates to the states not
expanding, we predict these states will
have $6.7 billion in additional
uncompensated care costs (relative to
expansion counterfactual).
• Kaiser estimates that the cost of the
expansion for these states would be $7.1
billion.
The political economy of Medicaid
• “A program for the poor is a poor program.”
• But Medicaid has never disappeared from a
state and only grown in size over time.
• Our paper suggests that Medicaid benefits not
only the citizens it covers but also the hospitals
they visit.
• Since hospitals are an important political force,
factors requiring hospitals to provide
uncompensated care may have unintentionally
assured Medicaid’s long-term stability.
Thank you!
Extra Slides
Hospital patient margins
State Fixed Effects and Year Fixed Effects
Share of
Population
Uninsured
N
All
Hospitals
Hospitals
with an ED
Hospitals without
an ED
-0.107
(0.068)
[0.122]
-0.096
(0.078)
[0.225]
-0.005
(0.048)
[0.924]
1,224
1,224
1,223
Non-Profit Hospital Patient Margins
State Fixed Effects and Year Fixed Effects
Share of
Population
Uninsured
N
All
Hospitals
Hospitals
with an ED
Hospitals without
an ED
-0.079
(0.028)
[0.007]
-0.072
(0.027)
[0.011]
-0.003
(0.004)
[0.465]
1,224
1,224
1,223
For-Profit Hospital Patient Margins
State Fixed Effects and Year Fixed Effects
Share of
Population
Uninsured
N
All
Hospitals
Hospitals
with an ED
Hospitals without
an ED
-0.009
(0.019)
[0.648]
-0.008
(0.016)
[0.607]
-0.001
(0.004)
[0.793]
1,224
1,224
1,223
Do non-profit hospitals absorb all of the cost
increases for changes in the demand for
uncompensated care?
• In 2000, NFP hospitals had a patient profit margin of -4.7 percent
• A 10 pctg. pt. increase in the number of uninsured results in a $6.1
billion in uncompensated care ($390 per uninsured person)
– If these costs were previously revenue, the new profit margin would be
-7.2 percent.
– This is a 2.6 percentage point increase
– Our estimates show a 0.8 percentage point decrease in patient margin
from a 10 pctg. pt. change in the share uninsured
– This suggests that hospitals are able to make up approximately 70
percent of the increased cost
• We next assume that the patients losing insurance were publicly
insured and Medicaid pays only 70% of actual costs
– If this is the case, the new profit margin falls to only -6.4 percent.
– This suggests that hospitals can make up only 45 percent of costs
Patient Margin at Remaining
Hospitals
Large vs. Small closures
Operating vs. Patient Margin
State-by-year operating margins
State Fixed Effects and Year Fixed Effects
Share of
Population
Uninsured
N
All
Hospitals
Hospitals
with an ED
Hospitals without
an ED
-0.087
(0.025)
[0.001]
-0.089
(0.024)
[0.000]
-0.002
(0.003)
[0.536]
1,224
1,224
1,223
Non-patient operating revenue
Non-patient operating revenue at
NFP
Difference between the two
settings?
• What is non-patient operating revenue?
– DSH Payments
– Local transfers
• Following a closure, these funds are reallocated to
remaining hospitals
• However, this is not true following a change in
Medicaid eligibility
• This is also not true in the ACA, where DSH funds
are being cut regardless of state decisions
regarding coverage
Figure 14. Uncompensated Care Costs in a Hospital
Before and After ED Closure
1.6
1.4
1.2
Uncompensated
care costs in
millions
1
.8
.6
.4
-4
-2
0
2
Years since ED closure
Note: This figure presents a re-centered time series with average uncompensated care
costs in the years before and after a hospital closes its ED.
4
“We have to remember what the state went through
seven years ago when it… cut a lot of people from
the TennCare rolls. We have to be very deliberate
about making a decision to add that many and more
back to the rolls… There are hospitals across this
state… that are going to struggle if not close under
the health care law without expansion, and that’s not
something to take lightly.”
- Bill Haslam, Tennessee governor