Urinary tract infection
advertisement
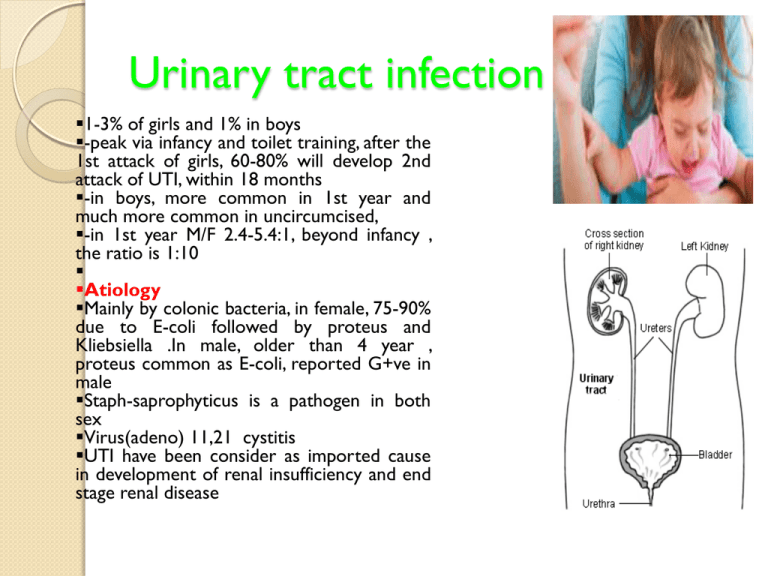
Urinary tract infection 1-3% of girls and 1% in boys -peak via infancy and toilet training, after the 1st attack of girls, 60-80% will develop 2nd attack of UTI, within 18 months -in boys, more common in 1st year and much more common in uncircumcised, -in 1st year M/F 2.4-5.4:1, beyond infancy , the ratio is 1:10 Atiology Mainly by colonic bacteria, in female, 75-90% due to E-coli followed by proteus and Kliebsiella .In male, older than 4 year , proteus common as E-coli, reported G+ve in male Staph-saprophyticus is a pathogen in both sex Virus(adeno) 11,21 cystitis UTI have been consider as imported cause in development of renal insufficiency and end stage renal disease pathogensis Nearly all UTI are secondary from bacteria arise from fecal flora , colonized the perineum and enter the bladder via urethra, or from bacteria beneath the prepuse in uncircumcised boy , it may lead to pyelonephritis. Rarly hematogeneusa Risk Factors of UTI Female, uncircumcised boy, vesicouretric reflux(VUR), toilet training, obstructive uropathy, urethral insterumentation, wiping from back to front, bubble bathing, tight clothes, pin worm infestation, constipation, neuropathic bladder , Sexual activity, Pregnancy. The incidence of UTI in breast fed babies is less than formula fed. C/F and Classification 1- Pyelonephritis is characterized by any or all of the following Abd pain(flank), fever(may be the only manifestation), malaise, nausea, vomiting, and accocianly diarrhea, in newborn and infant, nonspecific (irritability, jaundice, poor feeding, weight loss). Pyelonephritis is the most common serious bacterial infection in infants <24 mo of age who have fever without an obvious focus Renal damage, if no called pyelitis 2- Cystitis Baldder involvement, dysurea, frequency, urgency, malodorous urine, no renal damage, no fever 3- Asymptomatic bacterurea +ve urine culture but no manifestation, benign condition , no treatment require except in pregnancy Diagnosis Suspected from symptoms and or finding of urine analysis or both. +culture for confirmation and appropriate treatment the DX of UTI, depend on proper sampling of urine(4 ways) 1- Midstream urine = in child having toilet training +ve if the colony count more than 100,000 colony –forming units(CFU)of single MO or child is symptomatic, and 10,000 CFU is consider UTI, In uncircumcised boy , the prepuce should be retracted. 2- Adhesive , sealed , sterile collecting urine bag= in infant, after disinfection of skin of genitalia. false-positive rate too high to be suitable for diagnosing UTI; however, a negative culture is strong evidence that UTI is absent. +ve if the colony count more than 100,000 CFU of single MO and child is symptomatic, and +ve urine analysis, however if any of this criteria are not met , we may need next way Continue….Diagnosis. 3Catheterized sample= proper skin preparation , gentle technique of catheter is important, feeding tube polythene nu 5 or nu 8 with lubricant in older child to decrease risk of trauma, +ve if more than 10000 CFU of single MO 4- Suprapubic puncture = +ve if any MO best method NOTE Prompt plating of urine sample is important (stay in room temp for 60 min, lead to over growth of minor contamination the may suggest UTI), put it in refrigerator. Others indicators of UTI A- pyurea (pus cell in urine) suggest UTI, confirmatory than diagnostic. Conversely, pyuria can be present without UTI.,so its absence does not exclude UTI(sterile pyurea) Sterile pyuria (positive leukocytes, negative culture) occurs in 1- partially treated bacterial UTIs, 2-viral infections, 3-renal tuberculosis, 4- renal abscess, 5- UTI in the presence of urinary obstruction, 6- urethritis due to a sexually transmitted infection 7-inflammation near the (appendicitis, Crohn disease), 8- interstitial nephritis (eosinophils) ureter or bladder Continue…Others indicators. B- Nitrate and leukocytestrase +ve in urine If a child asymptomatic, GUA normal, it is unlikely UTI, however, if child symptomatic, and GUA normal, possible UTI. C- Blood (neutrophilia, increase ESR, CRP, in renal abscess, WBC 20,000-25,000, blood culture is indicated sp in infant(sepsis) E-Renal Scannig with Techneutiaiumlabeled DMSA(DiMarcoptoSuccinic Acid) Is the most sensitive and accurate way to detect the renal scaring. F- Urogram less sensitive than DMSA in detecting the renal scaring, and need 1-2 year to detect the pathology , risk of radiation G- CT of abdomin to detect the scaring in some time. Treatment 1-Cystitis should be treated to prevent pyelonephritis A- if symptomatic (sever), urine culture should be obtained, treatment 3-5 days of TrimetheprimSulphmethaxasol(5-10mg/kg), Nitrofurantuin 5-7mg/kg in 3-4 divided doses(Kliebsiella), Amoxil 50mg/kg is effective. B- if symptomatic (less sever ),treatment started till result of urine culture. 2- Pyelonephritis= 14 days course of broad spectrum of AB (Ampicillin 100mg/kg+Gentamycin 3-5mg/kg ) cefotaxime (100 mg/kg/24 hr), or Ceftriaxone 50-75mg/kg not exceed 2 gram)is preferable (less ototoxicity and nephrrotoxicity), serum cr and level of Gentamycin should be obtained before and during treatment if prolonged. Alkinization of urine is valuble in treatment of proteus with Gentamycin. Oral 3rd generation cephalosporin(Cefixim) is effective in G-ve ather than Pseudomonus 4 quinolol drevative is effective(contraindicated below age of 17years, effect the growing cartlige ) Some outhers suggest loading dose of Ceftriaxone then oral 3rd generation cephalosporin(cefixim). In absecce percuatenus drange +parental AB Urine culture should be obtained 1week after complete the treatment(should be sterile) Indications for hospitalization A- dehydration B- unable to drink C-possiple sepsis D-age less than 1month Recurrent UTI , two or more episodes of UTI with acute pyelonephritis/upper urinary tract infection, or • one episode of UTI with acute pyelonephritis/upper urinary tract infection plus one or more episode of UTI with cystitis/lower urinary tract infection, or • three or more episodes of UTI with cystitis/lower urinary tract infection. periodic urine culture every 3months for 2 years (if child asymptomatic) is indicated. In recurrent UTI , identify the risk factor and treat it and give AB prophylactic(1/3 of therapeutic dose) , Trimetheprime, Nitrofurantuine , Nalidixic acid., indicated in 1- neurogenic bladder 2- stasis due to obustruction Atypical UTI UTI associated with sepsis or bacteraemia Concern regarding obstructive uropathy Failure to respond to antibiotics within 48 hours Associated impaired renal function Infection with a non E. coli organism Imaging Study In children with their 1-1st episode of clinical pyelonephritis 2-Those with a febrile UTI 3- In infants, those with systemic illness 4-A positive urine culture, irrespective of temperature, a sonogram of kidneys and bladder should be performed to assess 1- kidney size 2-detect hydronephrosis 3- ureteral dilation, 4- identify the duplicated urinary tract 5- and evaluate bladder anatomy. Next, a DMSA scan is performed to identify whether the child has acute pyelonephritis. If the DMSA scan is positive and shows either acute pyelonephritis or renal scarring, . a voiding cystourethrogram (VCUG) is performed . If reflux is identified, treatment is based on the perceived long-term risk of the reflux to the child. One limitation to this approach is that many hospitals caring for children with a febrile UTI might not have facilities for performing a DMSA scan in children. In these cases, a renal sonogram should be performed, and then the clinician needs to decide on whether to send the child to a facility with DMSA capability or instead do a VCUG VCUR Time= 2-6 week after infection 2types 1- Radionucltide less radiation, less anatomical differentiation 2- Contrast more radiation , good differentiation Alternative Recommendations for UTI In 2007 These recommendations divide children into those <6 mo, 6 mo to 3 yr, and >3 yr of age. The clinical categories are separated into those that 1- respond to treatment within 48 hours 2-recurrent UTI 3- and atypical UTI (sepsis, non–E. coli UTI, suprapubic mass, elevated serum creatinine, hypertension). The recommendations include upper tract imaging with a renal sonogram and DMSA scan for 1- all <6 mo with a UTI 2- All children <3 yr with an atypical or recurrent UTI. 3-For children >3 yr, a DMSA scan is recommended only for recurrent UTI. VCUG is recommended only in children <6 mo. VesicoUretric Reflux(VUR) IS retrograde flow of urine from the bladder to the ureter and renal pelvis Normally , ureter is attached to the bladder in oblique direction perforating between the bladder mucosa and detroser muscle , creating a flap-valve mechanisim that prevent reflux. Reflux occur when the tunnel between the mucosa and detroser muscle is short or obliterated. -reflux usually congenital, run in family (1%), 35%of sibling of a child with reflux also have a reflux - reflux in 25% in neuropathic bladder, 50% in boy with posterior urethral valve, 15%inrenal agenasis - 20% of ESRD, gave ahistory of reflux - reflux is important cause of HT in children Reflux pyelonephritis renal scaring renal insufficaincy ESRD Classification According to the finding in VSUG Grade 1 reflux in to nondilated ureter Grade 2 reflux in to upper collecting system without dilatation Grade 3 reflux in to dilated ureter and or blunting of calyceal fornices Grade 4 reflux in to grossely dilated ureter Grade 5 massive reflux with significant uretral dilatation and tortuousity and loss of pappilary impression C/F Usually discovered during evaluation of UTI, 80% in female , average age is 2-3 year Renal insufficiency, HT DIAGNOSIS 1- VCUG, reflux occurring during bladder filling is called (low pressure)or passive and less likely to show spontaneous resolution, high pressure or active more likely to show spontaneous resolution, 2- Renal U/S 3- DMSA 4- Check the Bpr , ht, wt, urine culture Natural History 1- Grade 1 and 2 ,whether uni or bilateral spontenous resolution 2- Grade 3 younger age and unilateral high rate of resolution 3- Grade 4 bilateral less likely to resolve than unilateral 4- Grade 5 rarely resolve The main age of spontaneous resolution is 6 years Treatment The goal are to 1- prevent pyelonephritis 2- renal insufficiency 3- others reflux complication Treatment contain the following 1- AB prophylaxis , urine culture 2-VCUG every 12-18 month 3- Check the Bpr , ht, wt frequently 4- the above medical treatment is successful when no infection, and no scar or reflux resolve 5- Surgical treatment indicated in A- new scar B- breakthrough UTI C- not resolve at the age more than 7 year(failure of medical treatment) D- Grade 4 and 5