Therapeutic strategies to overcome crizotinib resistance
advertisement

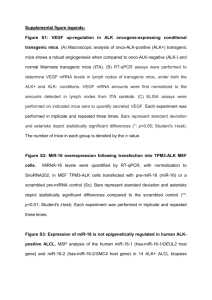
Therapeutic strategies to overcome crizotinib resistance in non-small cell lung cancers harboring the fusion oncogene EML4-ALK The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Katayama, R. et al. “Therapeutic strategies to overcome crizotinib resistance in non-small cell lung cancers harboring the fusion oncogene EML4-ALK.” Proceedings of the National Academy of Sciences 108 (2011): 7535-7540. Web. 2 Dec. 2011. © 2011 New York Academy of Sciences As Published http://dx.doi.org/10.1073/pnas.1019559108 Publisher National Academy of Sciences Version Final published version Accessed Thu May 26 23:33:32 EDT 2016 Citable Link http://hdl.handle.net/1721.1/67357 Terms of Use Article is made available in accordance with the publisher's policy and may be subject to US copyright law. Please refer to the publisher's site for terms of use. Detailed Terms Therapeutic strategies to overcome crizotinib resistance in non-small cell lung cancers harboring the fusion oncogene EML4-ALK Ryohei Katayamaa,b, Tahsin M. Khana,c, Cyril Benesa,b, Eugene Lifshitsa, Hiromichi Ebia,b, Victor M. Riverad, William C. Shakespeared, A. John Iafrateb,e, Jeffrey A. Engelmana,b,1, and Alice T. Shawa,b,c,1 a Massachusetts General Hospital Cancer Center, Boston, MA 02129; bDepartment of Medicine, Harvard Medical School, Boston, MA 02115; cKoch Institute for Integrative Cancer Research, Massachusetts Institute of Technology, Cambridge, MA 02139; dARIAD Pharmaceuticals, Cambridge, MA 02139; and e Department of Pathology, Massachusetts General Hospital, Boston, MA 02114 The echinoderm microtubule-associated protein-like 4 (EML4)anaplastic lymphoma kinase (ALK) fusion oncogene represents a molecular target in a small subset of non-small cell lung cancers (NSCLCs). This fusion leads to constitutive ALK activation with potent transforming activity. In a pivotal phase 1 clinical trial, the ALK tyrosine kinase inhibitor (TKI) crizotinib (PF-02341066) demonstrated impressive antitumor activity in the majority of patients with NSCLC harboring ALK fusions. However, despite these remarkable initial responses, cancers eventually develop resistance to crizotinib, usually within 1 y, thereby limiting the potential clinical benefit. To determine how cancers acquire resistance to ALK inhibitors, we established a model of acquired resistance to crizotinib by exposing a highly sensitive EML4-ALK–positive NSCLC cell line to increasing doses of crizotinib until resistance emerged. We found that cells resistant to intermediate doses of crizotinib developed amplification of the EML4-ALK gene. Cells resistant to higher doses (1 μM) also developed a gatekeeper mutation, L1196M, within the kinase domain, rendering EML4-ALK insensitive to crizotinib. This gatekeeper mutation was readily detected using a unique and highly sensitive allele-specific PCR assay. Although crizotinib was ineffectual against EML4-ALK harboring the gatekeeper mutation, we observed that two structurally different ALK inhibitors, NVPTAE684 and AP26113, were highly active against the resistant cancer cells in vitro and in vivo. Furthermore, these resistant cells remained highly sensitive to the Hsp90 inhibitor 17-AAG. Thus, we have developed a model of acquired resistance to ALK inhibitors and have shown that second-generation ALK TKIs or Hsp90 inhibitors are effective in treating crizotinib-resistant tumors harboring secondary gatekeeper mutations. F irst described in 2007, the oncogenic fusion kinase echinoderm microtubule-associated protein-like 4-anaplastic lymphoma kinase (EML4-ALK) is present in ∼4% of patients with non-small cell lung cancer (NSCLC) (1). Chromosomal translocations involving ALK also occur in other cancers, including anaplastic large cell lymphomas and inflammatory myofibroblastic tumors. In all cases, the fusion partner (e.g., EML4) is believed to mediate ligand-independent oligomerization of ALK, resulting in constitutive ALK kinase activation (2–4). In cell line and genetically engineered mouse models, EML4-ALK serves as a potent oncogenic “driver,” and cancers with this translocation are highly sensitive to ALK kinase inhibition (5, 6). Recently, a tyrosine kinase inhibitor (TKI) targeting ALK, crizotinib (PF-02341066), was examined in a phase 1 trial (7). Among 105 patients with EML4-ALK–positive NSCLC, crizotinib showed remarkable activity, with an objective response rate of 56% and a median progression-free survival of 9.2 mo (7, 8). These results support the notion that lung cancers harboring EML4-ALK are highly susceptible to ALK-targeted therapies and demonstrate the properties of “oncogene addiction” to ALK. Although many patients derive substantial clinical benefit, the development of drug resistance has curbed the impact of crizo- www.pnas.org/cgi/doi/10.1073/pnas.1019559108 tinib in this disease. The paradigm of acquired TKI resistance has been seen with other targeted therapy successes, including epidermal growth factor receptor (EGFR) mutant lung cancers and v-raf murine sarcoma viral oncogene homolog B1 (BRAF) mutant melanomas (9–16). Similar to the experience with crizotinib, sensitive cancers ultimately develop resistance, usually within 1 y. For example, most patients with EGFR-mutant NSCLC will have disease progression after 9–12 mo of EGFR TKI monotherapy. In about one-half of cases, resistance arises due to the acquisition of a secondary gatekeeper mutation (T790M) within the EGFR (13, 15, 16). This mutation leads to substitution of a threonine in the ATP-binding pocket with a bulky methionine residue, which hinders drug binding. In about 10–20% of cases, resistance arises as a result of focal amplification of the MET proto-oncogene (9, 16, 17). Importantly, preclinical modeling of acquired resistance to EGFR TKIs has proven invaluable, not only for accurately predicting the resistance mechanisms that emerge in the clinic, but also for assessing new therapeutic strategies to overcome resistance (12, 16–22). Recently, one NSCLC patient with acquired resistance to crizotinib was described (23). In this patient who relapsed after 5 mo of treatment, molecular analyses revealed that the resistant tumor cells harbored two secondary mutations within the kinase domain of EML4-ALK, C1156Y, and the gatekeeper mutation L1196M. These mutations occurred independently in distinct subclones of the resistant tumor. Studies of Ba/F3 cells engineered to express EML4-ALK harboring either mutation suggested that these mutants were resistant to crizotinib as well as resistant to a more potent ALK TKI, termed 2,4-pyrimidinediamine derivative (PDD). Thus, strategies to overcome this type of resistance have not yet been established. In addition, because there are no laboratory models of acquired resistance via this mechanism, it remains unknown if cancers that develop these resistance mutations remain addicted to ALK kinase activity and will be highly sensitive to other therapeutics targeting ALK. In this study, we have explored resistance to crizotinib by generating and characterizing a unique cell line model of acquired resistance. In this model of acquired resistance, EML4-ALK is amplified and harbors the L1196M gatekeeper mutation. We show that cells expressing the L1196M mutant form of EML4ALK are resistant to crizotinib, remain addicted to ALK signaling, Author contributions: R.K., J.A.E., and A.T.S. designed research; R.K., T.M.K., E.L., H.E., V.M.R., W.C.S., and A.J.I. performed research; R.K., C.B., V.M.R., W.C.S., and A.J.I. contributed new reagents/analytic tools; R.K., T.M.K., C.B., A.J.I., J.A.E., and A.T.S. analyzed data; and R.K., J.A.E., and A.T.S. wrote the paper. The authors declare no conflict of interest. This article is a PNAS Direct Submission. 1 To whom correspondence may be addressed. E-mail: jengelman@partners.org or ashaw1@partners.org. This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10. 1073/pnas.1019559108/-/DCSupplemental. PNAS | May 3, 2011 | vol. 108 | no. 18 | 7535–7540 MEDICAL SCIENCES Edited by Peter K. Vogt, The Scripps Research Institute, La Jolla, CA, and approved March 23, 2011 (received for review December 27, 2010) cells, we detected a C → A substitution at nucleotide 3586 of EML4-ALK variant 1 (Fig. 2B) that was not detected in the parental cells. This 3586C → A substitution results in a leucine → methionine change within the ALK TK domain, corresponding to the L1196M gatekeeper mutation previously reported in a patient with acquired resistance to crizotinib (23). We did not detect any other TK mutations including the C1156Y substitution, which was also reported in the same patient (23). Consistent with the notion that this L1196M mutation confers resistance to crizotinib, Ba/F3 cells engineered to express this mutant were also resistant to crizotinib, whereas cells expressing wild-type EML4-ALK were sensitive (SI Appendix, Fig. S2). Notably, in the DNA sequence tracings, the peak corresponding to the mutation is approximately one-half to one-third as high as the wild-type peak (Fig. 2B). This suggests that only a fraction of the amplified EML4-ALK fusion genes acquire the secondary resistance mutation. These resistant models were developed by stepwise increases in drug concentration until fully resistant cells emerged. Because both amplification and mutation were identified in H3122 CR cells, we sought to investigate the temporal relationship between gene amplification and secondary mutation in acquired crizotinib resistance. Thus, we analyzed H3122 CR0.6 cells, the intermediate, partially resistant predecessors of H3122 CR cells that were resistant to 600 nM crizotinib. By Western blotting analysis, ALK protein level and p-ALK were up-regulated in H3122 CR0.6 cells (SI Appendix, Fig. S3). FISH analysis demonstrated amplification of the EML4-ALK fusion gene in the H3122 CR0.6 cells (Fig. 2A). However, they did not harbor a secondary ALK resistance mutation (Fig. 2B). To determine whether L1196M is present at a low level in a subpopulation of H3122 CR0.6 cells, we developed a highly sensitive gatekeeper mutation-specific PCR assay that can detect the L1196M mutation when it represents at least 1% of the mutated ALK alleles (SI Appendix, Fig. S4). Using this assay, we detected L1196M in H3122 CR cells and in all 11 clones derived from single H3122 CR cells (SI Appendix, Fig. S5), but not in the H3122 CR0.6 cells, the parental H3122 cells, or the other NSCLC cell lines harboring EML4-ALK (Fig. 2C and SI Appendix, Fig. S5). These results suggest that the L1196M mutation is present in each cell of the resistant H3122 CR cells and that there is a stepwise model of acquired resistance involving amplification of the target, which confers resistance to 600 nM crizotinib, followed by sec- 1000 nM M non 1% 50 H3122 CR crizotinib(6hr) 100 nM H3122 crizotinib (6hr) crizotinib (200nM), n=704 300 nM C B 100 pALK (pY1604) ALK pAKT (pS473) H460 BT474 SKBR3 H3122 CR H522 H1299 A549 panAKT 0 H3122 cell number (% of control) A 30 nM EML4-ALK Gene Is Amplified and Mutated in H3122 CR Cells. To determine whether gene amplification underlies the elevated protein level of EML4-ALK in H3122 CR cells, we performed fluorescence in situ hybridization (FISH) analysis. Relative to parental H3122 cells, H3122 CR cells showed an increase in the number of rearranged EML4-ALK genes per cell (Fig. 2A). Because the phosphorylation of EML4-ALK in H3122 CR cells is not impacted by 1 μM crizotinib (Fig. 1C), we hypothesized that resistant cells might also harbor a mutation within ALK. We prepared cDNA and examined the entire coding sequence of EML4-ALK in H3122 parental and resistant cells. In the resistant 1000 nM M non and is highly sensitive to treatment with crizotinib. To explore mechanisms of crizotinib resistance, we generated resistant H3122 clones by exposing the sensitive parental cells to increasing concentrations of crizotinib for 4 mo. We maintained cells with intermediate crizotinib resistance, referred to as H3122 CR0.6, in 600 nM of crizotinib. The fully resultant cells, H3122 crizotinibresistant (H3122 CR) cells, were maintained in 1 μM of crizotinib. H3122 CR cells were as resistant to crizotinib as other cancer cell lines that did not harbor ALK gene rearrangements (IC50 > 1 μM; Fig. 1A and SI Appendix, Fig. S1A). In addition, we assessed 704 established cancer cell lines derived from a wide variety of tumor types for sensitivity to crizotinib as part of our automated platform to examine drug sensitivity across multiple cell lines (24). Whereas H3122 parental cells segregated with the most sensitive cell lines, the H3122 CR cells segregated with the highly resistant cell lines (Fig. 1B). Unlike the parental H3122 cells, the H3122 CR cells maintained ALK phosphorylation in the presence of crizotinib (Fig. 1C). Accordingly, AKT and ERK phosphorylation were not suppressed by crizotinib in the resistant cells. Notably, H3122 CR cells also contained higher total protein levels of EML4-ALK compared with the parental line (Fig. 1C). 300 nM Generation and Biochemical Characterization of Crizotinib-Resistant Cells. The NSCLC cell line H3122 expresses EML4-ALK variant 1 100 nM Results 30 nM and are highly sensitive to other structurally distinct ALK TKIs as well as to Hsp90 inhibition. On the basis of these results, we propose two therapeutic strategies for overcoming acquired resistance to crizotinib, particularly when mediated by secondary mutations within the ALK TK domain. <0 0.2 2 0.2 - 0.5 0.5 - 0.75 > 0.75 pERK ERK Actin Fig. 1. H3122 CR cells are resistant to crizotinib. (A) Cell lines were seeded in 96-well plates and treated with 1 μM of crizotinib for 72 h. Cell survival was analyzed using the CellTiter-Glo viability assay. In contrast to the parental H3122 cells, which are highly sensitive to crizotinib (red bar), H3122 CR cells (blue bar) are as insensitive to crizotinib as non-ALK rearranged cell lines. (B) Pie chart representation of the sensitivity of H3122 and H3122 CR cells compared with 704 other human cancer cell lines assessed by an automated cell viability assay to 200 nM crizotinib. Viability at 72 h was calculated as a ratio of viable crizotinib-exposed cells to viable DMSO-treated cells. The color scheme corresponds to the relative inhibitory effect of treatment. The chart depicts the most sensitive cell lines in order of decreasing sensitivity (from top to bottom). (C) H3122 parental and H3122 CR cells were treated with crizotinib at the indicated concentration for 6 h. Cell extracts were immunoblotted to detect the indicated proteins. 7536 | www.pnas.org/cgi/doi/10.1073/pnas.1019559108 Katayama et al. A H3122 B Forward H3122 CR H3122 CR0.6 Reverse C water H2228 MGH006 M H3122 CR0.6 3122 CR H3 H3122 22 CR0.6 H312 H3122 H3122 CR Leu (CTG) Met (ATG) Katayama et al. B si-ALK A549 si-control si-ALK si-ALK ol si-contro H3122 CR ol si-contro H3122 100 pALK (pY1604) 50 ALK H3122 H3122 CR si-A ALK si-c cntl Actin ALK si-A 0 si-c cntl the gatekeeper L1196M mutation causes resistance by steric interference with crizotinib binding (23). Thus, although resistant to crizotinib, this mutant ALK may be sensitive to structurally distinct ALK kinase inhibitors. To address this hypothesis, we tested the activity of the ALK inhibitor NVP-TAE684, a 5-chloro-2,4diaminophenylpyrimidine, in parental and resistant H3122 cells. As shown in Fig. 4, NVP-TAE684 markedly reduced cell survival in both sensitive H3122 and H3122 CR cells, but had little to no effect on the viability of other, non-ALK–dependent cancer cell lines (Fig.4A and SI Appendixx, Fig. S1B). Within the panel of 704 established cancer cell lines assessed in the automated platform (24), the vast majority were largely insensitive to 200 nM NVPTAE684; however, 1% of lines displayed marked sensitivity to NVP-TAE684. Both the H3122 and the H3122 CR cell lines segregate with the highly sensitive cell lines (Fig. 4B). This is in sharp contrast to the resistance of H3122 CR cells to crizotinib A si-A ALK NVP-TAE684 and AP26113 Overcome Crizotinib Resistance in H3122 CR Cells. Based on the crystal structure of the kinase domain of ALK, cntl si-c H3122 CR Cells Are Addicted to ALK. To determine if H3122 CR cells continue to require EML4-ALK for their viability, we used siRNAs targeting ALK to knock down EML4-ALK. In both H3122 parental and H3122 CR cell lines, ALK-specific siRNA decreased expression of EML4-ALK and potently suppressed cell growth (Fig. 3 A and B). As expected, the ALK siRNA had no effect on the growth of KRAS mutant A549 cells (Fig. 3 A and B). These results demonstrate that resistant H3122 CR cells expressing EML4-ALK L1196M remain addicted to ALK signaling. (Fig. 1B). In contrast to crizotinib, NVP-TAE684 treatment of H3122 CR cells suppressed phosphorylation of ALK, AKT, and ERK and induced marked apoptosis (Fig. 4C and SI Appendix, Fig. S6). Similarly, NVP-TAE684 potently suppressed the survival of Ba/F3 cells expressing the EML4-ALK L1196M mutant (SI Appendix, Fig. S7A). However, in this system, the potency of NVP-TAE684 against mutant EML4-ALK was slightly reduced relative to native EML4-ALK, with IC50 values of 2.7 versus 1.2 nM, respectively. cell number (% of control) ondary gatekeeper mutation that renders cells resistant to 1 μM crizotinib. A549 Fig. 3. Resistant H3122 CR cells are oncogene-addicted. (A) The indicated cell lines were transfected with small interfering RNA (siRNA) against ALK (siALK) or control siRNA, and cell viability was measured after 72 h. (B) Immunoblotting of protein lysates 72 h after knockdown showing reduced levels of phosphorylated ALK and total ALK in siALK-transfected cells. PNAS | May 3, 2011 | vol. 108 | no. 18 | 7537 MEDICAL SCIENCES Fig. 2. EML4-ALK is both amplified and mutated in resistant H3122 CR cells. (A) Dual-color FISH [ALK-N-terminal (green)/ALK-C-terminal (red)] analysis was performed on H3122 parental, H3122 CR0.6, and H3122 CR cells. Arrows indicate the split ALK C-terminal region (EML4-ALK). Both H3122 CR0.6 and H3122 CR cells demonstrate amplification of EML4-ALK. (B) Secondary L1196M (gatekeeper) mutation in resistant H3122 CR cells. Shown are electrophoretograms of EML4-ALK cDNA from H3122 parental, H3122 CR0.6, and H3122 CR cells. The 1903C → A mutation within exon 23 results in a L635M substitution that corresponds to the L1196M gatekeeper mutation of ALK. (C) Detection of the gatekeeper mutation using an L1196M mutation-specific PCR assay. Shown is the amplified 160-bp product in H3122 CR cells after 35 PCR cycles. This product is not detected in parental H3122 or H3122 CR0.6 cells or in other EML4-ALK– positive cell lines (H2228, MGH006). 300 nM 3 nM 10 nM 30 nM 100 nM non 30 nM 100 nM 300 nM 10 nM non 50 pERK BT474 ERK < 0.2 0.2 - 0.5 0.5 - 0.75 > 0.75 E Actin H3122 CR H3122 3 nM 10 nM 30 nM 100 nM 300 nM crizotinib (1uM) non 3 nM 10 nM 30 nM 100 nM 300 nM crizotinib (1uM) H460 H522 SKBR3 H1299 A549 H3122 CR pAKT (pS473) panAKT D non AP26113 (6hr) 100 pALK (pY1604) 50 pAKT (pS473) AP26113 (6hr) ALK BT474 SKBR3 H460 A549 H1299 H522 0 H3122 CR panAKT AKT H3122 cell number (% of control) H3122 CR TAE684 (6hr) pALK (pY1604) ALK H3122 ce ell number (% of c o ontrol) TAE684 (200nM), n=704 100 0 H3122 TAE684 (6hr) C 3 nM B A pERK ERK Actin Fig. 4. Two different ALK kinase inhibitors, NVP-TAE684 and AP26113, overcome crizotinib resistance in H3122 CR cells. (A) Cell lines were seeded in 96-well plates and treated with 100 nM of TAE684 for 72 h. Cell survival was analyzed using the CellTiter-Glo viability assay. Both parental H3122 cells (red bar) and H3122 CR cells (blue bar) show marked sensitivity to TAE684. Non-ALK rearranged cell lines (A549, H1299, SKBR3, H522, H460, and BT474 cells) show minimal growth inhibition with TAE684. (B) Pie chart representation of the sensitivity of H3122 and H3122 CR cells compared with 704 other human cancer cell lines assessed by an automated cell viability assay to 200 nM TAE684. Viability at 72 h was calculated as a ratio of viable crizotinib-exposed cells to viable DMSOtreated cells. The chart depicts the most sensitive cell lines in order of decreasing sensitivity (from top to bottom). Both parental H3122 and H3122 CR cells are among the 1% of the most sensitive cell lines to TAE684. (C) Suppression of ALK signaling by TAE684 in resistant H3122 CR cells. H3122 parental and resistant cells were exposed to increasing concentrations of TAE684 for 6 h. Cell lysates were immunoblotted to detect the indicated proteins. (D) Sensitivity of H3122 CR cells to AP26113. Cell lines were seeded in 96-well plates and treated with 300 nM of AP26113 for 72 h. Cell survival was analyzed using the CellTiter-Glo viability assay. Both parental H3122 cells (red bar) and H3122 CR cells (blue bar) show marked sensitivity to AP26113, compared with non-ALK rearranged cell lines. (E) Suppression of ALK signaling by AP26113 in resistant H3122 CR cells. H3122 parental and resistant cells were exposed to increasing concentrations of AP26113 for 6 h. Cell lysates were immunoblotted to detect the indicated proteins. We also tested a second, structurally distinct ALK kinase inhibitor AP26113. A new highly selective small molecule inhibitor of ALK, AP26113 exhibits about fivefold greater potency in vitro compared with crizotinib (SI Appendix, Table S1A). Like NVPTAE684, AP26113 was highly active against both sensitive and resistant H3122 cells, decreasing cell growth (Fig. 4D and SI Appendix, Fig. S1C), suppressing ALK phosphorylation (Fig. 4E), and inducing apoptosis (SI Appendix, Fig. S6). Higher doses of AP26113 were required to completely suppress ALK in the resistant cells because there were greater levels of ALK/p-ALK as a result of gene amplification. AP26113 was also active in Ba/F3 cells expressing either native or mutant EML4-ALK (IC50’s were 10 and 24 nM, respectively) (SI Appendix, Fig. S7B). Consistent with the Ba/F3 data, the potency of AP26113 against mutant EML4-ALK was slightly reduced relative to native EML4-ALK as determined by its capacity to decrease p-ALK in the H3122 and H3122 CR cells, with IC50 values of 7.4 versus 16.8 nM, respectively (SI Appendix, Fig. S8). These results suggest that AP26113 can overcome crizotinib resistance mediated by the gatekeeper L1196M mutation. Indeed, 7538 | www.pnas.org/cgi/doi/10.1073/pnas.1019559108 we observed impressive in vivo activity of both NVP-TAE684 and AP26113, but not of crizotinib, against the H3122 CR cells grown as xenograft tumors in vivo (SI Appendix, Fig. S9). Hsp90 Inhibitor 17-AAG Overcomes Crizotinib Resistance in H3122 CR Cells. In a recent phase 2 study, the Hsp90 inhibitor IPI-504 demonstrated clinical activity in three of three patients with ALKpositive NSCLC and induced rapid degradation of EML4-ALK in vitro (25). Hsp90 inhibitors also induced tumor regression in a genetically engineered mouse model of lung cancer driven by EML4-ALK (5). Therefore,we evaluated the efficacy of the Hsp90 inhibitor 17-AAG in EML4-ALK L1196M-expressing cells. As shown in Fig. 5A, 17-AAG potently suppressed cell growth in both parental H3122 and H3122 CR cells, but not in other non-ALK– dependent lung cancer lines (SI Appendix, Fig. S1D). However, in contrast to NVP-TAE684 and AP26113, 17-AAG also inhibited the viability of SKBR3 and BT474 cell lines, both of which harbor HER2 amplification and are known to be sensitive to Hsp90 inhibition (26, 27). In Ba/F3 cells, 17-AAG was active against both Katayama et al. ALK 50 pAKT (pS473) panAkt H522 H460 A549 H1299 BT474 SKBR3 pERK H3122 0 ERK Actin Fig. 5. The Hsp90 inhibitor 17-AAG can overcome crizotinib resistance in H3122 CR cells. (A) Cell lines were seeded in 96-well plates and treated with 10 nM of 17-AAG for 72 h. Cell survival was analyzed using CellTiter-Glo. Both parental H3122 cells (red bar) and H3122 CR cells (blue bar) show sensitivity to 17-AAG. (B) Suppression of ALK signaling by 17-AAG in resistant H3122 CR cells. H3122 parental and resistant cells were exposed to increasing concentrations of 17-AAG for 6 h. Cell lysates were immunoblotted to detect the indicated proteins. native and mutant EML4-ALK to a similar extent, but showed no activity in parental Ba/F3 cells (SI Appendix, Fig. S7C). 17-AAG treatment decreased both p-ALK level and ALK protein expression with similar potencies in the parental and resistant cells (Fig. 5B). These results suggest that Hsp90 inhibition might represent an alternative therapeutic strategy for overcoming acquired resistance to crizotinib due to acquisition of a resistance mutation. Discussion In tumors dependent on a driver kinase such as BCR-ABL or mutant EGFR, secondary mutation within the kinase domain is a common mechanism of acquired drug resistance. The most frequent resistance mutation involves the gatekeeper residue. Amino acid substitutions at this position hinder drug binding and thereby confer high-level resistance to many tyrosine kinase inhibitors. Other mechanisms of acquired drug resistance involve gene amplification of the kinase target or activation of alternative signaling pathways to bypass the need for kinase activation (10, 28). Identification of the genetic alterations underlying acquired drug resistance has fostered the development of targeted agents for patients with TKI resistance. For example, two secondgeneration TKIs—dasatinib and nilotinib—have efficacy against most of the known imatinib-resistant mutations and are approved for patients with imatinib-resistant chronic myeloid leukemia (CML) (29, 30). However, these drugs are not active against the gatekeeper T315I mutation within ABL (31). Similarly in EGFRmutant lung cancer, second-generation, irreversible EGFR inhibitors are being explored to treat cancers that develop resistance via the gatekeeper T790M mutation (22, 32). EML4-ALK–positive NSCLC represents another tyrosine kinasedriven cancer that is highly responsive to TKI therapy. Recently, two studies have reported the identification of secondary resistance mutations within the ALK TK domain in patients who relapsed on crizotinib (23, 33). One of the mutations identified was the gatekeeper L1196M substitution, analogous to T315I in ABL and T790M in EGFR (23). In this study, we generated a cell line model of acquired crizotinib resistance by exposing sensitive, EML4-ALK–positive H3122 cells to increasing concentrations of crizotinib. The resistant cells harbor both amplification of EML4-ALK and the same L1196M gatekeeper mutation that was identified in a patient with acquired resistance. Notably, we did not identify any other ALK mutations in this cell line, including C1156Y. Because we did not use more sensitive technologies such as deep sequencing, we cannot exclude the possibility that a small fraction of resistant cells harbor distinct secondary mutations such Katayama et al. as C1156Y. However, this seems unlikely because we observed the L1196M mutation and not the C1156Y mutation in all of the clones derived from single cells from the H3122 CR cell line. Although amplification of ALK is a known oncogenic event in pediatric neuroblastoma (34), amplification of ALK fusion oncogenes has not been reported. Analysis of partially resistant H3122 cells (H3122 CR0.6) that harbor EML4-ALK amplification (but no gatekeeper mutation) suggests a step-wise evolution of acquired resistance involving gene amplification followed by point mutation. This model is also supported by the observation that only a fraction of the amplified ALK fusion genes (per cell) harbor L1196M (Fig. 2C). In other TKI-resistant cancers, target amplification preceding acquisition of secondary mutations has not been reported in vitro or in vivo. It remains unknown if this twostep mechanism is unique to EML4-ALK–positive NSCLC or if it is a product of the methodology used to develop resistance in the laboratory. The detection of gatekeeper and other acquired mutations in resistant tumor samples is clinically important, but can be technically challenging. The EGFR T790M resistance mutation, for example, is often difficult to detect on standard sequence tracings and may require more sensitive techniques such as deep sequencing for detection (19, 35, 36). This problem may be due to contamination of the tumor specimen with noncancerous cells (e.g., stromal or inflammatory cells). Alternatively, for some tumors, only a small percentage of the EGFR alleles per cell may harbor the T790M mutation (termed “allelic dilution”), or only a small percentage of resistant cells in the tumor specimen might have T790M-mediated resistance. Notably, the finding of both EML4-ALK amplification and L1196M mutation in the CR cells suggests that allelic dilution also could ultimately contribute to difficulty in detecting resistance mutations in cancers with acquired resistance to crizotinib. In this study, we developed an L1196M-mutation specific PCR assay to detect potentially low levels of the gatekeeper L1196M mutation in partially resistant H3122 CR0.6 cells. This assay is highly sensitive with a detection limit of 1% or less (SI Appendix, Fig. S4) and requires only 30 ng genomic DNA. Thus, this assay might serve as the basis for a clinical diagnostic test for L1196M in biopsy samples from crizotinib-resistant patients. In both CML and EGFR-mutant lung cancer, resistant tumors with gatekeeper mutations have proven refractory to secondgeneration, more potent TKIs. One recent report suggests that the gatekeeper mutation in ALK might behave similarly; compared with control Ba/F3 cells expressing native EML4-ALK, cells expressing mutant EML4-ALK L1196M were markedly less sensitive to a potent PDD (23). In contrast, we have found that crizotinib resistance mediated by the gatekeeper L1196M mutation can be effectively overcome by two different ALK TKIs. Importantly, one of these—AP26113—is under clinical development and is scheduled to begin clinical testing within the year. In H3122 CR cells, the improved cellular activity of AP26113 compared with crizotinib is likely based on both its enhanced potency against ALK and its increased activity against L1196M-mutated ALK. In vitro kinase assays revealed that wild-type and L1196Mmutated ALK showed similar Km values for ATP binding (30.7 and 27.2 μM, respectively). However, crizotinib was about 10-fold less potent against L1196M ALK compared with wild-type ALK (Ki of 8.2 and 0.7 nM, respectively), consistent with its diminished efficacy against the L1196M ALK in cell lines (SI Appendix, Table S1B). In contrast, AP26113 was ∼10-fold more potent against ALK than crizotinib in vitro, and unlike crizotinib, it was similarly potent against the L1196M mutant (Ki of 0.09 and 0.08 nM, respectively). In addition to studying ALK TKIs, we have shown that EML4ALK harboring the gatekeeper mutation is an Hsp90 client protein similar to wild-type EML4-ALK and sensitive to Hsp90 inhibition. Notably, cell lines expressing either native EML4PNAS | May 3, 2011 | vol. 108 | no. 18 | 7539 MEDICAL SCIENCES 300 nM 100 nM 30 nM 10 nM 300 nM non 100 nM 10 nM non H3122 CR 17AAG (24hr) pALK (pY1604) H3122 CR ce ell number (% of control) 100 30 nM H3122 17AAG (24hr) 3 nM B 3 nM A ALK or EML4-ALK L1196M were even more sensitive to 17AAG than two Hsp90-dependent, HER2-amplified breast cancer lines (Fig. 5A). Therefore, patients with crizotinib resistance due to an acquired L1196M mutation may derive benefit from two different ALK-targeted strategies: more potent ALK TKIs such as AP26113 or any of a number of Hsp90 inhibitors already in clinical trials. Notably, although gatekeeper mutations are particularly common in EGFR-mutant lung cancer, the frequency of L1196M in EML4-ALK–positive NSCLC has yet to be established. Because secondary mutations such as the gatekeeper mutation may not represent the predominant mechanism of acquired crizotinib resistance, additional studies are needed to elucidate other mechanisms of resistance. The results of these studies will be critical to selecting the best therapeutic strategies for targeting TKI resistance in the clinic. Materials and Methods See SI Appendix for the description of the cell culture conditions, generation of H3122 CR cells, survival assays, fluorescence in situ hybridization, immunoblotting, apoptosis assay retroviral infection, quantitative RT-PCR (qPCR), siRNA transfection, xenograft study, and statistical analyses. 1. Soda M, et al. (2007) Identification of the transforming EML4-ALK fusion gene in nonsmall-cell lung cancer. Nature 448:561–566. 2. Mano H (2008) Non-solid oncogenes in solid tumors: EML4-ALK fusion genes in lung cancer. Cancer Sci 99:2349–2355. 3. Shinmura K, et al. (2008) EML4-ALK fusion transcripts, but no NPM-, TPM3-, CLTC-, ATIC-, or TFG-ALK fusion transcripts, in non-small cell lung carcinomas. Lung Cancer 61:163–169. 4. Takeuchi K, et al. (2009) KIF5B-ALK, a novel fusion oncokinase identified by an immunohistochemistry-based diagnostic system for ALK-positive lung cancer. Clin Cancer Res 15:3143–3149. 5. Chen Z, et al. (2010) Inhibition of ALK, PI3K/MEK, and HSP90 in murine lung adenocarcinoma induced by EML4-ALK fusion oncogene. Cancer Res 70:9827–9836. 6. Soda M, et al. (2008) A mouse model for EML4-ALK-positive lung cancer. Proc Natl Acad Sci USA 105:19893–19897. 7. Kwak EL, et al. (2010) Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med 363:1693–1703. 8. Camidge DR, et al. (2010) Clinical activity of crizotinib (PF-02341066), in ALK-positive patients with advanced non-small cell lung cancer. Ann Oncol 21(Suppl 8):viii123, mdq518. 9. Bean J, et al. (2007) MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib. Proc Natl Acad Sci USA 104:20932–20937. 10. Engelman JA, Jänne PA (2008) Mechanisms of acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in non-small cell lung cancer. Clin Cancer Res 14:2895–2899. 11. Flaherty KT, et al. (2010) Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med 363:809–819. 12. Johannessen CM, et al. (2010) COT drives resistance to RAF inhibition through MAP kinase pathway reactivation. Nature 468:968–972. 13. Kobayashi S, et al. (2005) EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N Engl J Med 352:786–792. 14. Mok TS, et al. (2009) Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 361:947–957. 15. Pao W, et al. (2005) Acquired resistance of lung adenocarcinomas to gefitinib or erlotinib is associated with a second mutation in the EGFR kinase domain. PLoS Med 2:e73. 16. Turke AB, et al. (2010) Preexistence and clonal selection of MET amplification in EGFR mutant NSCLC. Cancer Cell 17:77–88. 17. Engelman JA, et al. (2007) MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 316:1039–1043. 18. Corcoran RB, et al. (2010) BRAF gene amplification can promote acquired resistance to MEK inhibitors in cancer cells harboring the BRAF V600E mutation. Sci Signal 3: ra84. 7540 | www.pnas.org/cgi/doi/10.1073/pnas.1019559108 Reagents. Crizotinib and NVP-TAE684 were purchased from ChemieTek and 17-AAG was purchased from Selleck. AP26113 was provided by ARIAD Pharmaceuticals that makes AP26113 available to qualified academic laboratories free of charge for verification and reproduction of the results reported in this paper. Each compound was dissolved in DMSO for cell culture experiments. Control or ALK siRNA was from Invitrogen, and HiPerfect reagent was from Qiagen. Isolation of Genomic DNA Preparation and L1196M Mutation-Specific PCR. Genomic DNA was isolated from cell pellets with a DNeasy kit (QIAGEN) according to the manufacturer’s protocol. Exon 23 of ALK was PCR-amplified from genomic DNA using Pfu Ultra II (Agilent Technologies) and sequenced bidirectionally by Sanger dideoxynucleotide sequencing with the primers described in SI Appendix. ALK-Exon23 or L1196M mutation-specific qPCR was performed by a LightCycler 480 (Roche Diagnostics) with CYBR Green Master Mix (Roche). Primer sequences are provided in SI Appendix. ACKNOWLEDGMENTS. This study was supported in part by a V Foundation for Cancer Research Translational Grant (to J.A.E. and A.T.S.), by the Charles W. and Jennifer C. Johnson Koch Institute Clinical Investigator Award (to A.T.S.), by National Institutes of Health K08 Grant CA120060-01 (to J.A.E.), by the Sig Adler Lung Cancer Research Fund, by the Massachusetts General Hospital Thoracic Oncology Fund, and by a Japan Society for the Promotion of Science Postdoctoral Fellowship for Research Abroad from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (to R.K.). 19. Engelman JA, et al. (2006) Allelic dilution obscures detection of a biologically significant resistance mutation in EGFR-amplified lung cancer. J Clin Invest 116: 2695–2706. 20. Faber AC, et al. (2009) Differential induction of apoptosis in HER2 and EGFR addicted cancers following PI3K inhibition. Proc Natl Acad Sci USA 106:19503–19508. 21. Guix M, et al. (2008) Acquired resistance to EGFR tyrosine kinase inhibitors in cancer cells is mediated by loss of IGF-binding proteins. J Clin Invest 118:2609–2619. 22. Zhou W, et al. (2009) Novel mutant-selective EGFR kinase inhibitors against EGFR T790M. Nature 462:1070–1074. 23. Choi YL, et al.; ALK Lung Cancer Study Group (2010) EML4-ALK mutations in lung cancer that confer resistance to ALK inhibitors. N Engl J Med 363:1734–1739. 24. McDermott U, et al. (2008) Genomic alterations of anaplastic lymphoma kinase may sensitize tumors to anaplastic lymphoma kinase inhibitors. Cancer Res 68:3389–3395. 25. Sequist LV, et al. (2010) Activity of IPI-504, a novel heat-shock protein 90 inhibitor, in patients with molecularly defined non-small-cell lung cancer. J Clin Oncol 28:4953–4960. 26. Chandarlapaty S, et al. (2010) Inhibitors of HSP90 block p95-HER2 signaling in Trastuzumab-resistant tumors and suppress their growth. Oncogene 29:325–334. 27. Zheng FF, et al. (2000) Identification of a geldanamycin dimer that induces the selective degradation of HER-family tyrosine kinases. Cancer Res 60:2090–2094. 28. Engelman JA, Settleman J (2008) Acquired resistance to tyrosine kinase inhibitors during cancer therapy. Curr Opin Genet Dev 18:73–79. 29. Kantarjian H, et al. (2010) Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 362:2260–2270. 30. Saglio G, et al.; ENESTnd Investigators (2010) Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med 362:2251–2259. 31. O’Hare T, et al. (2005) In vitro activity of Bcr-Abl inhibitors AMN107 and BMS-354825 against clinically relevant imatinib-resistant Abl kinase domain mutants. Cancer Res 65:4500–4505. 32. Yap TA, et al. (2010) Phase I trial of the irreversible EGFR and HER2 kinase inhibitor BIBW 2992 in patients with advanced solid tumors. J Clin Oncol 28:3965–3972. 33. Sasaki T, et al. (2010) The neuroblastoma associated F1174L ALK mutation causes resistance to an ALK kinase inhibitor in ALK translocated cancers. Cancer Res 70: 10038–10043. 34. Chiarle R, Voena C, Ambrogio C, Piva R, Inghirami G (2008) The anaplastic lymphoma kinase in the pathogenesis of cancer. Nat Rev Cancer 8:11–23. 35. Kosaka T, et al. (2006) Analysis of epidermal growth factor receptor gene mutation in patients with non-small cell lung cancer and acquired resistance to gefitinib. Clin Cancer Res 12:5764–5769. 36. Kwak EL, et al. (2005) Irreversible inhibitors of the EGF receptor may circumvent acquired resistance to gefitinib. Proc Natl Acad Sci USA 102:7665–7670. Katayama et al.