ABORTIONS
advertisement

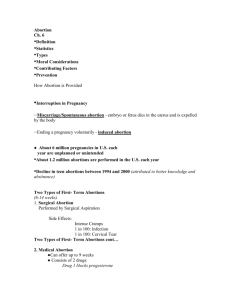
ABORTIONS OBJECTIVES At the end of this session you should be able to: 1. Define various types of abortions. 2. Outline the causes and management approach for various types of abortions. 3. Describe the relation between complications of abortions and maternal mortality DEFINITIONS OF ABORTION 1. Termination of pregnancy before 28/40 2. Delivery of a fetus of weight less than 500 grams STATISTICS OF ABORTIONS • 50 - 60% of all pregnancies end in spontaneous abortion (SAB) since 2-4 wk pregnancies will often go unnoticed. • 15% of all recognized pregnancies 4-20 wks end in SAB. • 30% lost between implantation and the 6th wk. • 70% of first trimester losses are due to chromosomal abnormalities TYPES OF ABORTIONS 1. 2. 3. 4. 5. 6. 7. 8. Induced Threatened Inevitable Incomplete Complete Septic Missed Recurrent 1. INDUCED ABORTION • Intentional medical or surgical termination of a pregnancy • Types – Elective: if performed for a woman’s desires – Therapeutic: if performed for reasons of maintaining health of the mother INDUCED ABORTION – MEDICOLEGAL ASPECTS IN TANZANIA • Only allowed for medical indications – If continuation of pregnancy is risk to life of the woman • At least two medical doctors should reach the decision and sign • Elective abortions – are unlawful INDUCED ABORTIONS - COMPLICATIONS Because most induced abortions are done by less skilled persons they are usually associated with fatal complications including: 1. Perforation of uterus, intestines, etc 2. Severe haemorrhage, 3. Sepsis and its associated complications, 4. Asherman’s syndrome, etc 2. THREATENED ABORTION Refers to a stage in the abortion that suggests potential miscarriage may take place. Symptoms • Minimal or no lower abdominal pain or cramps • Slight abd pain • Minimal draining of liquor Threatened abortion cont Signs • Stable general condition • Fundal height corresponds to GA • Cervix closed Management of threatened abortion 1. Bed rest – Avoid strenuous exercises 2. If GA > 16/40 give - tocolytics 3. INEVITABLE ABORTION Refers to a stage in the abortion when it is not possible for the pregnancy to continue. INEVITABLE ABORTION CONT Symptoms • Moderate to severe vaginal bleeding • Severe abd pain • Significant draining of liquor Signs • Dilatation of cervix with evidence of imminent expulsion of the PoC • Fundal height corresponds to GA • Presence of contractions Management of Inevitable abortion 1. Resuscitation: IV fluids: RL, NS 2. Blood grouping & Cross matching 3. Evacuation • MVA for GA < 12/40 • Augment if the GA > 12/40 Oxytocin If some PoC remain after abortion manage like incomplete abortion. MANUAL VACUUM ASPIRATOR 4. INCOMPLETE ABORTION • Some POC have been expelled from the uterine cavity and other are retained inside. Symptoms – Moderate to severe vaginal bleeding – Cramping/severe abd pain – Partial expulsion of POC Signs – Uterus smaller than dates – Cervix is dilated of cervix Management of Incomplete abortion Resuscitation: IV fluids: RL, NS Blood grouping & Cross matching → BT if indicated Evacuation 1. 2. 3. – – MVA for GA < 12/40 Augment if the GA > 12/40 • Oxytocin • If some PoC remain after abortion manage like incomplete abortion. 4. Antibiotics: ampicilin, metronidazole 5. Analgesics 5. SEPTIC ABORTION An abortion complicated by infection Symptoms – Abdominal pain – Fever – Vaginal discharge (foul smelling) Signs – Sick looking, febrile or jaundiced – Tender uterus – Offensive vaginal discharge or bleeding – Cervix is usu. soft and may be dilated Complications of septic abortions Immediate cpx Late cpx • Haemorrhage • PID • Peritonitis • Pelvic abscess, endometritis, • Septicemia, • Septic/haemorrhagic shock • Pelvic adhesions • 2° Infertility • Chronic LAP Management 1. Resuscitation – 2. IV fluids: RL, NS Insert urethral catheter – Monitor Input/output 3. Blood grouping & Cross matching 4. Antibiotics: • Preferably cephalosporins, if not available ampicilin and metronidazole 5. Evacuation 6. Haematenics 6. RECURRENT PREGNANCY LOSSES • Defined as 3 or more consecutive pregnancy losses Other names: • habitual abortions • habitual miscarriage • recurrent abortions • recurrent miscarriages. Aetiology of RPL Aetiology: Can be established in only 30% • Genetic Factors • Endocrine Factors • Anatomic Causes – Congenital anomalies, in competencies, • Infectious causes • Immunologic problems