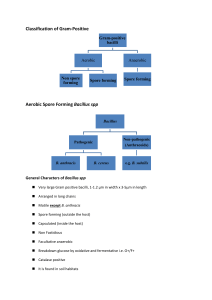
BACILLUS SPECIES
advertisement

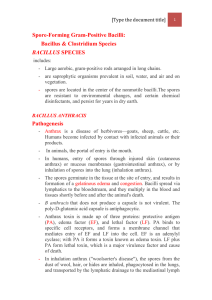
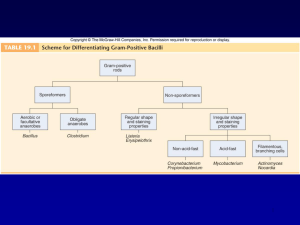
Spore-Forming Gram-Positive Bacilli: Bacillus & Clostridium Species 1 BACILLUS SPECIES Large aerobic, gram-positive rods arranged in long chains. Bacillus is saprophytic organisms prevalent in soil, water, and air and on vegetation. The spores are resistant to environmental changes, and certain chemical disinfectants, and persist for years in dry earth. Bacillus anthracis Pathogenesis: - Anthrax is a disease of herbivores—goats, sheep, cattle, etc. Humans become infected by contact with infected animals or their products. - In humans, entry of spores through injured skin (cutaneous anthrax) or mucous membranes (gastrointestinal anthrax), or by inhalation of spores into the lung (inhalation anthrax). - The spores germinate in the tissue at the site of entry, and results in formation of a gelatinous edema and congestion. Bacilli spread via lymphatics to the bloodstream, and they multiply in the blood and tissues shortly before and after the animal's death. - In inhalation anthrax ("woolsorter's disease"), the spores from the dust of wool, hair, or hides are inhaled, phagocytosed in the lungs, and transported by the lymphatic drainage to the mediastinal lymph nodes, where germination occurs. This is followed by toxin production and the development of hemorrhagic mediastinitis and sepsis, which are fatal. Clinical Findings - In humans, 95% of cases are cutaneous anthrax and 5% are inhalation. Gastrointestinal anthrax is rare. - Cutaneous anthrax occurs on arms or hands, face and neck. A pruritic papule Spore-Forming Gram-Positive Bacilli: Bacillus & Clostridium Species 2 develops 1–7 days after entry of the organisms or spores. The papule changes into a vesicle, and a necrotic ulcer develops. The lesions have a characteristic central black eschar. Lymphangitis and lymphadenopathy and systemic signs and symptoms of edema, fever, malaise, and headache also occur. After 7– 10 days the eschar is dries, and separates; healing is by granulation and leaves a scar. In 20% of patients, cutaneous anthrax leads to sepsis, meningitis and death. -The incubation period in inhalation anthrax 6 weeks. Clinical manifestations are hemorrhagic necrosis and edema of the mediastinum. Substernal pain. Hemorrhagic pleural; cough is secondary to the effects on the trachea. Sepsis occurs, and there may be bowel ulceration, or hemorrhagic meningitis. The fatality rate is high. Diagnostic Laboratory Tests - Specimens are fluid or pus from a local lesion, blood, and sputum. Stained smears from dead animals often show chains of large gram-positive rods. - Immunofluorescence staining techniques. - When grown on blood agar plates, the organisms produce nonhemolytic gray to white colonies with a rough texture and a ground-glass appearance. Comma-shaped outgrowths (Medusa head) may project from the colony. - An enzyme-linked immunoassay (ELISA) has been developed to measure antibodies against edema and lethal toxins. Spore-Forming Gram-Positive Bacilli: Bacillus & Clostridium Species 3 Treatment - In humans, treatment must be started early. Ciprofloxacin is recommended; penicillin G, along with gentamicin or streptomycin, has previously been used to treat anthrax. - In the setting of potential exposure to B anthracis , prophylaxis with ciprofloxacin or doxycycline should be continued for 4-8 weeks. - Some other gram-positive bacilli, such as B cereus, are resistant to penicillin. Doxycycline, erythromycin, or ciprofloxacin may be effective alternatives to penicillin. Epidemiology, Prevention, & Control - Soil is contaminated with anthrax spores from dead animals. These spores remain viable for decades. Contact with infected animals or with their hides, hair, and bristles is the source of infection in humans. Control measures include:(1) Disposal of animal carcasses by burning or by deep burial in lime pits, (2) Decontamination by autoclaving of animal products (3) Protective clothing and gloves for handling potentially infected materials Spore-Forming Gram-Positive Bacilli: Bacillus & Clostridium Species 4 BACILLUS CEREUS 1. Food poisoning caused by Bacillus cereus has two forms: The emetic type, associated with fried rice, is manifested by nausea, vomiting, abdominal cramps, and diarrhea and is self-limiting, with recovery occurring within 24 hours. It begins 1–5 hours after ingestion of rice and pasta dishes. When large amounts of rice are cooked and allowed to cool slowly, the B cereus spores germinate and the vegetative cells produce the toxin. The diarrheal type, associated with meat dishes and sauces. Has an incubation period of 1–24 hours and is manifested by: diarrhea with abdominal pain and cramps. The enterotoxin may be performed in the food or produced in the intestine. 2. eye infections, severe keratitis, endophthalmitis, and panophthalmitis. The organisms are introduced into the eye by foreign bodies associated with trauma. 3. B cereus has also been associated with localized infections and with systemic infections, including endocarditis, meningitis, osteomyelitis, and pneumonia; the presence of a medical device or intravenous drug use predisposes to these infections.