Medically Important Bacteria – Gram Positive Bacilli
advertisement

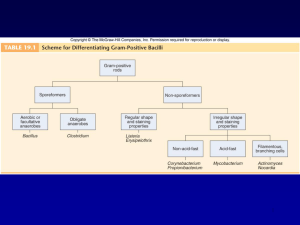
Medically Important Bacteria – Gram Positive Bacilli Learning Objectives Classification of GPBs General properties of GPBs Discuss the role of toxins and other virulence factors in pathogenesis Describe the mechanism of action of various toxins List pathogenicity Medically Important Gram-Positive Bacilli Can be subdivided into two general groups, based on the presence or absence of spores 1. 2. Spore-formers Nonspore-formers Scheme for Differentiating GPBs Spore Forming Gram Positive Bacilli Spore Forming GPBs Spore forming gram +ve bacilli: 2 groups 1. Aerobic – Bacillus: Important species are Bacillus anthracis – Anthrax Bacillus cereus – food poisoning Bacillus stearothermophilus – efficiency testing of an autoclave 2. Anaerobic – Clostridia: Imp species include • • • • Clostridium perfringens – gas gangrene Clostridium tetani – tetanus Clostridium botulinum – botulism (food poisoning) Clostridium difficile – pseudomembranous colitis Bacillus General Characteristics of the Genus Bacillus Aerobic Gram-positive, spore-forming (non bulging spores), bacilli 2 species of medical importance: – Bacillus anthracis – Bacillus cereus B. anthracis - Virulence factors Two virulence factors – Capsular polysaccharide – inhibits phagocytosis Anthrax toxin : made up of 3 fractions 1. 2. 3. Edema factor (EF or Factor I) Protective antigen factor (PA or Factor II) Lethal factor (LF or Factor III) * They are not toxic individually, the whole complex produces local edema & generalised shock. Toxin production is plasmid mediated Anthrax toxin Pathogenicity Anthrax – zoonotic disease of primarily cattle & sheep. Animals get infected by ingestion of spores present in the soil Bacilli are shed in discharges from the mouth, nose & rectum - sporulate in the soil. Human anthrax – contracted from animals, directly or indirectly. Human Anthrax The disease may present as 1. 2. 3. Cutaneous anthrax : ‘Hides Porter’s disease’ – inoculation of spores into the skin Pulmonary anthrax : ‘Wool Sorter’s disease’ – inhalation of spores Intestinal anthrax - ingestion of inadequately cooked meat containing anthrax spores * All types lead to fatal septicemia Human anthrax can be 1. 2. Industrial – in meat packing or wool factories Nonindustrial – frequent association with animals like butchers, veterinarians, farmers Anthrax Bacillus cereus Readily isolated from soil, vegetables and a wide variety of foods including milk, cereals, spices, poultry & meat. Spores survive cooking and reheating Causes foodborne gastroenteritis – 2 patterns of disease (diarrhoeal & emetic); both types are mild & self limited, requiring no specific therapy. Bacillus cereus clinical presentation Gastroenteritis DIARRHOEAL FORM EMETIC FORM Wide range of foods including cooked meat & vegetables Incubation period > 6 hours Diarrhoea & abdominal pain Lasts 20-36 hours Chinese fried rice exclusively Incubation period < 6 hours Severe vomiting Lasts 8-10 hours Clostridium General Characteristics of the Genus Clostridium Gram-positive, spore-forming rods Anaerobic and catalase negative Oval or spherical (bulging) spores produced only under anaerobic conditions Cause wound infections, tissue infections, and food intoxications Cl. perfringens Cl. perfringens: Virulence factors Classified into Five strains, A to E - based on the toxins they produce Produces many toxins: 4 major toxins – alpha, beta, epsilon & iota 1. Alpha toxin – lecithinase C, a phospholipase 2. Damages cell membranes Increase capillary permeability Extravasation & increased tension in affected muscles Lysis of erythrocytes: hemolytic anemia & hemoglobinuria Beta, epsilon & iota – necrosis Enzymes – collagenase, hyaluronidase – spread of infection Cl. perfringens: Pathogenicity Soft tissue infection: Gas gangrene (Type A) Enteric infections: – – – – Food poisoning (some strains of type A) Gangrenous appendicitis (A + D) Necrotising enteritis (C) Biliary tract infections Other diseases: – Brain abscess & meningitis – Thoracic infections Gas Gangrene Clostridium perfringens most frequent clostridia involved in soft tissue and wound infections – myonecrosis Spores found in soil, human skin, intestine, and vagina Predisposing factors – crushing injuries, road accidents, gunshot wounds, surgical incisions, compound fractures, diabetic ulcers, septic abortions, puncture wounds C/F - high fever, brownish pus, gas bubbles under the skin, skin discoloration, and a foul odor Cl. tetani Gram +ve bacilli with terminal, spherical spore Commonly present in soil, GI tracts of animals and inanimate objects like street & hospital dust, cotton wool, bandages, catgut, wall plaster, clothings, etc Causes tetanus or lockjaw, a neuromuscular disease – Most commonly among geriatric patients and IV drug abusers; neonates in developing countries – Death commonly occurs due to paralysis of respiratory muscles Pathogenesis of Tetanus Source of Infection Contaminated soil / dust Mode of transmission Injury, puncture wounds, wound contamination Unhygienic Complication Septic abortion, Cutting umbilical stump Ear boring / circumcision / unsterile injections Virulence factor Tetanospasmin – Neurotoxin Tetanolysin The events in tetanus Spastic Paralysis in Tetanus Ophisthotonus Clostridium botulinum Gram +ve bacilli with subterminal, oval spores Produces toxin – Botulin (botulinum toxin), a neurotoxin Causes Botulism, a paralytic (flaccid paralysis) disease – Ingestion of preformed toxins – In preserved (canned) food like meat & meat products, fish & canned vegetables Effects of botulinum toxin Phase I/ Module VII Dr Ekta Chourasia Clostridium difficile Normal resident of colon, in low numbers Causes antibiotic-associated colitis (pseudomembranous colitis) – Relatively non-invasive; treatment with broad-spectrum antibiotics kills the other bacteria, allowing C. difficile to overgrow Produces enterotoxins & cytotoxins that damage intestine Major cause of diarrhea in hospitals Non spore Forming Gram Positive Bacilli Gram-Positive Non-Spore-Forming Bacilli Medically important genera: Corynebacterium Listeria Propionibacterium Mycobacterium Actinomyces Nocardia General Features of Corynebacteria Infects nasopharynx or skin Mostly grow aerobically, nonmotile Irregular swellings/clubbedshaped; granules within rod stained with aniline dyes. Corynebacterium diphtheriae Corynebacterium diphtheriae is the pathogen responsible for diphtheria. It colonizes the pharynx, forming a grayish pseudomembrane composed of fibrin, leukocytes, necrotic epithelial cells, and Corynebacterium diphtheriae cells. From this site, the bacteria release a powerful exotoxin into the bloodstream, which specifically damages heart and neural cells by interfering with protein synthesis. Corynebacterium diphtheriae Blood agar+potassium tellurite, tellurite is reduced intracellularly C. diphtheriae - Virulence factor Exotoxin – Diphtheria toxin: – Protein in nature – very powerful toxin – Responsible for all pathogenic effects of the bacilli – Produced by all the virulent strains – Two fragments A & B Toxigenicity can be induced by Lysogenic or phage conversion – corynephages (tox+ phage) or beta phages Diphtheria toxin – Mechanism of action DT - Acts by inhibition of protein synthesis Fragment A – inhibits polypeptide chain elongation by inactivating the Elongation factor EF 2 in the presence of NAD Treatment Tracheostomy in children (to prevent croup) Antitoxin 20000-100000 unit (Intra muscular) Penicillin or erythromycin Prevention Vaccination A combination of diphtheria toxoid, tetanus toxoid, and pertussis. • Given at 2, 4 an 6 months of age, with a booster at 1 and 6 years of age and then each 10 years afterward. (DPT or DT) The toxoid is prepared by treating the exotoxin with 0.3% formaldehyde. Listeria monocytogenes Small/Short, G+,peritrichous flagella, rod. Grow on Mueller-Hinton agar (better in sheep blood-small zone of haemolysis); facultative anaerobe, motile at room temp, catalase + Listeriosis results from ingestion of contaminated food such as cheese and vegie; primarily affects pregnant women, newborns, those with weakened immune system. Able to multiply at low temp, hence accumulate in contaminated food stored in refrigerator. Listeria monocytogenes It is a common cause of meningitis in 2 particular groups: The first group is neonates, who contract this organism from their asymptomatic mothers during delivery. The second group of patients at risk for Listeria meningitis is immunosuppressed patients, such as those with cancer, renal transplants, or AIDS. The mortality rate for meningitis in this second group is extremely high. Steps in the invasion of cells and intracellular spread by L. monocytogenes. The bacterium apparently invades via the intestinal mucosa. It is thought to attach to intestinal cells by means of D-galactose residues on the bacterial surface which adhere to D-galactose receptors on susceptible intestinal cells The bacterium is taken up by induced phagocytosis, which is thought to be mediated by a membrane associated protein called internalin. Once ingested the bacterium produces listeriolysin to escape from the phagosome. The bacterium then multiplies rapidly in the cytoplasm and moves through the cytoplasm to invade adjacent cells by polymerizing actin to form long tails. Treatment When meningitis develops in a patient who is at high risk for Listeria monocytogenes, it is important to treat it empirically with antibiotics that will cover this bacterium. we must add either ampicillin or trimethoprimsulfamethoxazole to the antibiotic regimen. These are 2 antibiotics that cover Listeria monocytogenes. Genus Propionibacterium Propionibacterium acnes most common Aerotolerant or anaerobic Nontoxigenic Common resident of pilosebaceous glands Causes Acne Mycobacteria: Acid-Fast Bacilli Gram-positive irregular bacilli Acid-fast staining Obligate aerobes Possess mycolic acids and a unique type of peptidoglycan Do not form capsules, flagella, or spores Slow growing, 14-15 hrs generation time Mycobacterium Tuberculosis Produces no exotoxins or enzymes that contribute to infectiousness Virulence factors – contain complex waxes and cord factor that prevent destruction by lysosomes or macrophages Mycobacterium Leprae: The Leprosy Bacillus Hansen’s bacillus/Hansen’s Disease First bacterium to be shown to cause disease in humans Humans & Armadillos are the only natural hosts Strict parasite – cannot be cultivated “invitro” , does not grow on artificial media or tissue culture Slowest growing of all species Causes leprosy, a chronic disease that begins in the skin and mucous membranes and progresses into nerves Multiplies within host cells in large packets called globi Actinomycetes: Filamentous Bacilli Genera Actinomyces & Nocardia are nonmotile filamentous bacteria related to mycobacteria May cause chronic infection of skin and soft tissues Actinomyces israelii – responsible for diseases of the oral cavity, thoracic or intestines – actinomycoses “Sun-ray appearnce” Nocardia brasiliensis causes pulmonary disease similar to TB