Obstetrics بطلا ةيلك ⁄
advertisement

المرحلة الرابعة
جامعة بابل⁄ كلية الطب
نسرين مالك-د
Obstetrics
Abnormal labour:-The labour becomes abnormal when there is poor progress(
a delay in cervical
dilatation or descent of the presenting part), and⁄or the fetus shows signs of compromise. Also it is
considered abnormal if there is malpresentation, malposition, a uterine scar or if labour has been induced.
Prolonged labour(dystocia) or called dysfunctional labour:- Dystocia of labour is defined as
difficult labor or abnormally slow progress of labour.
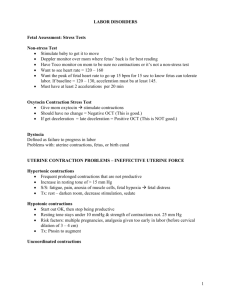
Poor progress of labour occur either in first or second stage of labour:Progress of labour is depend on three variables (3 P):1-The powers, i.e.the efficiency of uterine contractions.
2-The passages,i.e, the uterus, cervix, and the bony pelvis.
3--The passenger, i.e.,the fetus( with particular respect to the size , presentation, and position ).
The patient and the provider may be other dependant factors.
Abnormalities in one or more of these factors can slow the normal progress of labour .
1-The powers(inefficient uterine action):This is the most common cause of poor progress in labour. It is more common in primigravidae and
perhaps in older women and is characterized by weak and infrequent contractions.
The assessment of uterine contractions is most commonly carried out by clinical examination and by using
external uterine tocography. However, this can only provide information about the frequency and duration
of contractions. Intrauterine pressure catheters are available and these do give an accurate measurement of
the pressure being generated by the contractions , but they are rarely necessary. A frequency of 4 to 5
contractions per 10 minutes is usually considered efficient.
Treatment of inefficient uterine contractions is by maternal rehydration, artificial rupture of
membarane(ARM),and intravenous oxytocin(syntocinon).
Uterine contractions may also be extremely irregular and may occur close together in twos and threes,
followed by longer periods of inertia .Syntocinon is also effective in correcting this
inco-ordinate uterine activity and usually succeeds in spacing the contractions out more evenly.
1
2-The passages,i.e, the uterus, cervix, and the bony pelvis:The genital tract abnormalities(soft tissue ,or the bony pelvis abnormalities ):1-Small pelvis:-There are 4 types of the pelvis gynecoid, android, anthropoid, and platypelloid, the
gynecoid pelvis is most optimal for normal delivery, while the others cause obstructed labour. Abnormal
shape of the pelvis due to diseases like rickets, osteomalacia or tuberculosis, tumors of the bones, childhood
poliomyelitis affecting the shape of the hips, previous accidents , congenital dislocation of the hips or
congenital deformity of the sacrum or coccyx. Kyphosis and Scoliosis,also affect the shape of the pelvis.
Pelvimetry is clinical estimation of the adequacy of the pelvis.
Clinical indices that increase the suspicion of disproportion during labor:1- Pelvic sidewalls are convergent.
4- Subpubic arch angle is <90 degrees
2- Ischial spines are prominent.
5-Sacrum is flat.
3- Diagonal conjugate is <11.5 cm
6- No descent of vertex with Valsalva or
fundal pressure (Müller-Hillis maneuver)
2-Problems with the genital tract:-Soft tissue abnormalities in the pelvis occasionally can result in
dystocia. Uterine myomas are the most common pelvic masses associated with dystocia. They may obstruct
the birth canal or cause malpresentation of the fetus. Other possible causes of upper genital tract dystocia
include ovarian tumors, bladder distention, pelvic kidney, excess adipose tissue, uterine malposition, and
cervical stenosis or neoplasm(like cervical cancer,cervical fibroids obstructing the birth passage), congenital
rigidity of the cervix, scarring of the cervix due to previous operations( like cone biopsy). Lower genital
tract dystocia can be caused by partial vaginal or vulvar atresia, vaginal septum, severe edema or
inflammation, Bartholin’s or Gartner’s duct cysts, , hematomas, and neoplasms.
2
3-The passenger, i.e.,the fetus:Cephalo-pelvic disproportion:-The term 'cephalopelvic disproportion' implies anatomical disproportion
between the head of the baby ('cephalus') and the mother's pelvis. Complications can occur if the fetal
head is too large to pass through the mother's pelvis or birth canal, this can be because of a small pelvis
and an average sized fetus, or a large baby with an average sized pelvis (this is termed absolute cephalopelvic disproportion) , women of short stature(less than 1.60 meter) with a large baby in their first
pregnancy are likely candidates to develop this problem.
Other cause of CPD is malposition of the fetal head which lead to large presenting head diameters(this is
termed relative cephalo-pelvic disproportion).
Causes of absolutec ephalo-pelvic disproportion (CPD): ■ A- Fetal causes
■ B-Maternal causes:-
■ A- Fetal causes:1-Increased fetal weight: Very large baby whose weight is estimated to be above 5 Kgs (10 pounds) due to
hereditary reasons , post mature baby (when the pregnancy goes above 42 weeks), diabetic women, babies
of mothers who have had a number of children( each succeeding baby tends to be larger and heavier).
2- Fetal malformations:- Hydrocephally,anencephaly, conjoined twins.
3- Malpresentations:- Brow presentation ,Face presentation (if mento-posterior), compound
presentation(hand or foot or both presented together with head at the cervix).
■ B-Maternal causes:- The genital tract abnormalities(soft tissue ,or the bony pelvis
abnormalities ):- As mentioned before.
•
.
Causes of relative cephalo-pelvic disproportion:Fetal malposition ( occipito – posterior, or occipito lateral.):Rather than the presentation of the optimal suboccipito-bregmatic diameter(9.5 cm) in a well flexed
occipito-anterior position, the larger occipito-frontal diameter (11.5 cm) in a deflexed occipito-posterior
position or other positions will results in a relative cephalo-pelvic disproportion.
3
Cephalo-pelvic disproportion is suspected in labour if:1-Progress is slow or arrested despite efficient uterine contractions.
2- The fetal head is not engaged.
3-Vaginal examination shows sever moulding and caput formation.
4-The head is poorly applied to the cervix.
Patterns of abnormal progress of labour:Friedman's original research in 1955 defined the following three stages of labor.
1. The first stage starts with uterine contractions leading to complete cervical dilation and is divided
into latent and active phases. In the latent phase, irregular uterine contractions occur with slow and
gradual cervical effacement and dilation till 3-4 cm. The active phase is demonstrated by an
increased rate of cervical dilation and fetal descent. The active phase usually starts at 3-4 cm to full
cervical dilation and is subdivided into the acceleration, maximum slope, and deceleration phases.
2. The second stage of labor is defined as complete dilation of the cervix to the delivery of the infant.
3. The third stage of labor involves delivery of the placenta.
Friedman's partogram
The use of a partogram to plot the progress of labour improves the detection of poor progress. Indeed there
are three pattern of abnormal labour are commonly described on the partogram:-
First stage of labour:1-Prolonged Latent Phase
Latent phase begins with regular contractions that efface and dilate the cervix and ends with the onset of
active labor at 3-4 cm.
Prolonged latent phase is diagnosed after 20 hours in the nullipara or 14 hours in the multipara. This one
approach is to evaluate the patient carefully as 12 hours in latent phase approaches. If there has been
increase cervical effacement and dilation or fetal descent (indicating that the patient is not in false labor).
4
2-Prolonged active phase:-There are 3 types:● Primary dysfunctional labour(Protracted active phase dilatation): Protracted active phase dilatation is
a common dysfunctional labor pattern. It seems to be associated with mild cephalopelvic disproportion
,inefficient uterine contractions, and in malposition of the fetus.
For nulliparas, protracted active phase dilation should be diagnosed when the dilation rate is less than 1
cm/h. For the multipara, the lower limit of normal is 1.5 cm/h. Based on Friedman’s original definition, a
limit for nulliparas of 1.2 cm/h might be used.
● Secondary arrest of dilitation:-This is occur when progress in the active phase is initially good but then
stops , typically after 7 cm dilatation. is diagnosed when there has been no change in cervical dilation for at
least 2 hours. This time criterion is the same for nulliparas and multiparas Secondary arrest usually occur in
association with a significant underlying pathological process like CPD or malpresentation.
● Prolonged deceleration phase:The deceleration phase is the third phase of active labor, after the phase of maximum slope. The onset of
deceleration phase begins at 9 cm for nulliparous and multiparous labor.
Prolonged second stage of labour:Onset of the second stage of labor occurs with full cervical dilation. “Clinical limits” for second-stage
durations at which time the clinician should become concerned and anticipate problems with delivery have
been proposed. For nulliparas, this clinical limit is 2 hours, and for multiparas, it is 1 hour.
■ Protracted Descent
Protracted descent should be diagnosed in nulliparous labor when descent is less than l cm/h, and in
multiparous labor when descent is less than 2 cm/h.
The cause of protracted descent often includes malposition and relatively mild degrees of fetopelvic
disproportion; absolute fetopelvic disproportion is unusual. Slow descent frequently is associated with the
use of epidural anesthesia.
■ Arrest of Descent
The diagnosis of arrest of descent should be made when descent has stopped entirely for at least 2 hour in
the nullipara and 1 hour in the multipara. It frequently is preceded by and has the same causative factors as
protracted descent.
Secondary uterine inertia is common cause the second stage delay , and may be exacerbated by the
epidural analgesia.
5
Having achieved full dilatation , the uterine contractions become weak and ineffectual and this is
sometimes associated with maternal dehydration and ketosis. Delay can also occur because of a persistent
OP position of the fetal head , or because a narrow mid pelvis ( android pelvis ), which prevents internal
rotation of the fetal head this results in the fetal head being arrested at the level of the ischial spine in the
transverse position , a condition called deep transverse arrest.
Deep transverse arrest.
Prolonged third stage of labor :-Is diagnosed when delivery of the placenta is delayed after 30
minutes.
Diagnosed criteria for abnormal labour patterns:-
Labour pattern
Nulliparous
Parous
More than 20 h
More than 14 h
Active phase:
Protracted cervical dilation
Less than 1.2 cm⁄h
Less than 1.5 cm⁄h
Arsset of cervical dilation
More than 2 h
More than 2 h
Protracted fetal head descend
Less than 1 cm⁄h
Less than 2 cm⁄h
Arrest of Fetal head descent
More than 2 h
More than 1 h
First stage of labour
Prolonged latent phase
Second stage of labour
Prolonged second stage
Without epidural anesthesia
More than 2 h
More than 1 h
With epidural anesthesia
More than 3 h
More than 2 h
More than 30 min
More than 30 min
Prolonged third stage
6
A-Prolonged latent phase
B-Prolonged active phase
C-Arrest active phase
Management of prolonged labour:1- Management of dystocia in the first stage of labour:□ Prolonged latent phase:-during this period ,women may experience painful contractions and need a
great deal and support. In place of active intervention, careful explanation and the provision of adequate
analgesia may be all that is required before the cervical changes complete and the active phase of labour is
entered. There should be clear maternal or fetal indications to augment labor during the latent phase to
justify the risks associated with oxytocin augmentation such as uterine hyperstimulation, fetal intolerance of
labor and increased rates of operative intervention.
Latent labor may be longer in women undergoing labor induction than in women in spontaneous labor,
and cesarean for dystocia should not be done if women are still in latent labor.
Once a woman is in active labor, amniotomy prior to oxytocin use may be sufficient to augment
slowly-progressing labor.
□ Protracted or arrested active phase labor:- For women with protracted or arrested active phase labor,
the clinician can evaluate the strength and frequency of uterine contractions by abdominal palpation or an
intrauterine pressure catheter (IUPC), which allows calculation of Montevideo units (MVU). 200 or more
MVU in 10 minutes is considered evidence of adequate contractions.
If contractions are inadequate, intravenous oxytocin is administered to increase contraction frequency,
duration, and strength. Low-dose regimens start at 0.5 to 2.0 mU/min and increase by 1 to 2 mU/min
every 15 to 40 minutes to maximum doses of 20 to 40 mU/min.
High-dose regimens have starting doses of 6 mU/min and incremental increases of 1 to 6 mU/min up to
maximums of 40 to 42 mU/min.
7
Great care must be exercised in the use of oxytocin if CPD, malposition or malpresentation is suspected in a
multiparous labours. Augmentation of contractions with oxytocin (syntocinon) should only ever be
commenced if the cardiotochography (CTG),or fetal blood sampling is normal.
If progress fails to occur over the next 4 hours of augmentation with syntocinon, a caesarean section will be
necessary.
2- Management of dystocia in the second stage of labor:- .
Dystocia can also occur in the second stage of labor and is characterized by prolonged duration
or arrest of descent. Such arrest may be due to fetal malposition, inadequate contractions, poor
maternal efforts or true cephalopelvic disproportion.
1- When arrest of descent due to inadequate contractions, it is extremely sensitive to oxytocin
augmentation. Low-dose slow intravenous oxytocin frequently is associated with spontaneous vaginal
delivery. As with the case of augmentation for other labor abnormalities, electronic monitoring is important.
If the patient already is receiving oxytocin augmentation or there is arrest in descent despite efficient
uterine contractions, and there is normal fetal head position (AP), proceeding to cesarean section is probably
the best approach,because the failure of descend is this case is most likely due to absolute CPD.
The situation in which the vertex is below +1 cm, but descent has ceased is not rare. The delivery of such a
deeply engaged fetal head at cesarean section commonly results in lacerations of the cervix and lower
uterus. The possibility of operative vaginal delivery continues to warrant consideration in such cases. Before
undertaking an operative vaginal delivery, it is crucial to evaluate the maternal outlet carefully, particularly
in terms of the angle of the pubic arch and the distance between the ischial tuberosities. Also, the possibility
of macrosomia and shoulder dystocia should be entertained.
2-In case of fetal malposition:- The most common fetal malposition is occiput posterior (OP), where the
fetus lies with its occiput toward the mother’s spine and its face toward the mother’s pubic symphysis. Most
OP fetuses rotate spontaneously to occiput anterior positions prior to delivery, but in 2-7 percent of
nulliparous women, the fetus delivers in direct OP position (face to pubis).
Persistent OP is associated with prolonged second stage labor and increased oxytocin augmentation.
Manual rotation from OP to occiput anterior (OA) position results in a lower cesarean delivery rate. Other
approaches to the care of a woman with persistent OP or asynclitic fetal positions include encouraging a
variety of maternal positions and movements including knee-chest, hands-and-knees, pelvic rocking, sidelying, or asymmetrical sitting or kneeling. In case of persistent OP or asynclitic fetal positions and the
station is below the ischial spines, specially if associated with a non-reassuring fetal heart tracing during
prolonged second stage it may be possible to deliver by forceps or ventouse, but in the case of high station
delivery is accomplished by cesarean section.
8