Document 12300097
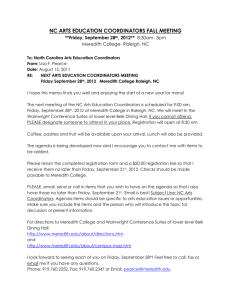
advertisement
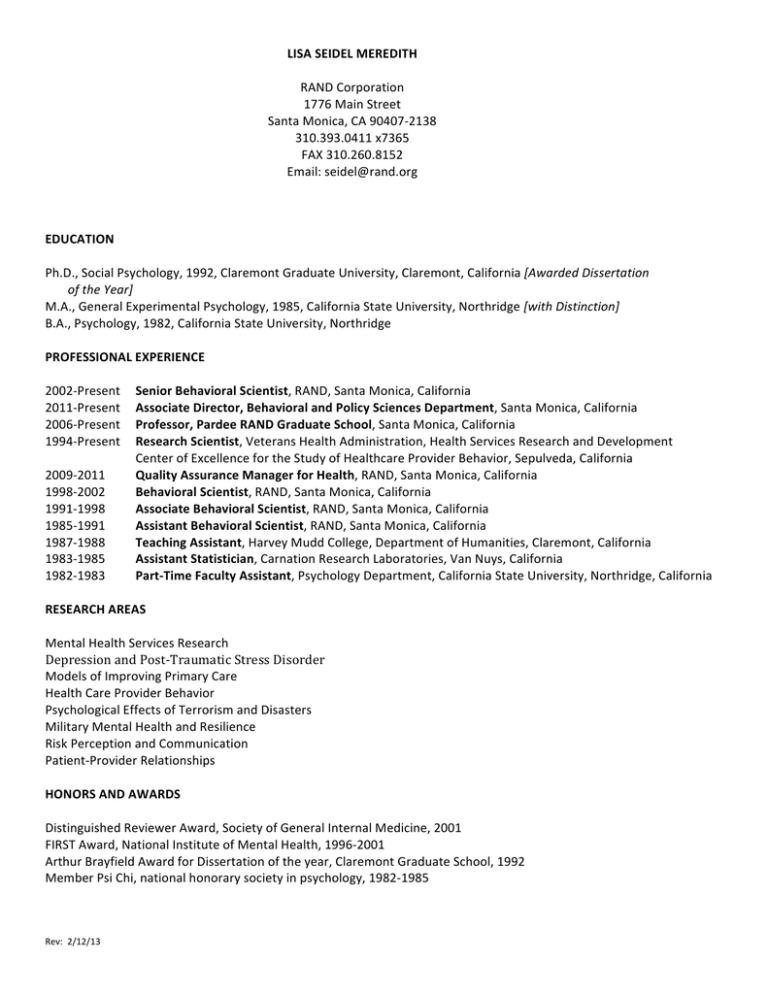
LISA SEIDEL MEREDITH RAND Corporation 1776 Main Street Santa Monica, CA 90407-­‐2138 310.393.0411 x7365 FAX 310.260.8152 Email: seidel@rand.org EDUCATION Ph.D., Social Psychology, 1992, Claremont Graduate University, Claremont, California [Awarded Dissertation of the Year] M.A., General Experimental Psychology, 1985, California State University, Northridge [with Distinction] B.A., Psychology, 1982, California State University, Northridge PROFESSIONAL EXPERIENCE 2002-­‐Present Senior Behavioral Scientist, RAND, Santa Monica, California 2011-­‐Present Associate Director, Behavioral and Policy Sciences Department, Santa Monica, California 2006-­‐Present Professor, Pardee RAND Graduate School, Santa Monica, California 1994-­‐Present Research Scientist, Veterans Health Administration, Health Services Research and Development Center of Excellence for the Study of Healthcare Provider Behavior, Sepulveda, California 2009-­‐2011 Quality Assurance Manager for Health, RAND, Santa Monica, California 1998-­‐2002 Behavioral Scientist, RAND, Santa Monica, California 1991-­‐1998 Associate Behavioral Scientist, RAND, Santa Monica, California 1985-­‐1991 Assistant Behavioral Scientist, RAND, Santa Monica, California 1987-­‐1988 Teaching Assistant, Harvey Mudd College, Department of Humanities, Claremont, California 1983-­‐1985 Assistant Statistician, Carnation Research Laboratories, Van Nuys, California 1982-­‐1983 Part-­‐Time Faculty Assistant, Psychology Department, California State University, Northridge, California RESEARCH AREAS Mental Health Services Research Depression and Post-­‐Traumatic Stress Disorder Models of Improving Primary Care Health Care Provider Behavior Psychological Effects of Terrorism and Disasters Military Mental Health and Resilience Risk Perception and Communication Patient-­‐Provider Relationships HONORS AND AWARDS Distinguished Reviewer Award, Society of General Internal Medicine, 2001 FIRST Award, National Institute of Mental Health, 1996-­‐2001 Arthur Brayfield Award for Dissertation of the year, Claremont Graduate School, 1992 Member Psi Chi, national honorary society in psychology, 1982-­‐1985 Rev: 2/12/13 MEREDITH GRANTS AND CONTRACTS Current: Principal Investigator, Improving PTSD Management in Primary Care, National Institute of Mental Health (R01MH082768), 2009-­‐2014 (Main Study) Administrative Supplements to: 1. Validate the brief 6-­‐item PTSD screener against the CAPS diagnostic interview in a sample of underserved patients (R01MH082768-­‐02S1), 2011-­‐2014 2. Broaden cost analyses by estimating the potential net cost savings of the PCM from both payer and patient perspectives (R01MH082768-­‐04S1), 2012-­‐2014 Principal Investigator, Consultancy to Help Develop the National university of Singapore Health Services Research, National University of Singapore (Contract No. NUS-­‐01.23.11), 2011-­‐2013 Co-­‐Investigator, Task Leader for Provider Surveys, Patient Centered Medical Home (PCMH) Demonstration Lab, Veterans Health Administration HSR&D (Contract No. 691-­‐D90051, Rubenstein, PI), 2010-­‐2015 Co-­‐Investigator, Task Leader for Provider Surveys, Accelerating Implementation of Comprehensive Women’s Health Care for the VA, Veterans Health Administration HSR&D (Contract No. 691-­‐D25041, Rubenstein, PI), 2013-­‐2016 Senior Advisor, Alcohol Screening in an Ethnically Diverse Sample of Adolescents in Primary Care, National Institute of Alcohol Abuse and Alcoholism (R01AA021786, D’Amico PI), 2012-­‐2017 Senior Advisor, Family Resilience in the Military, Office of the Assistant Secretary of Defense (Contract No. W91WAW-­‐ RC-­‐0030), 2012-­‐2014 Senior Advisor, The Recognition and Referral of Mental Disorders within Religious Congregations, National Institute of Mental Health (R34MH091313, Wong, PI), 2011-­‐2013 Completed: Principal Investigator, Review of Literature and Best Practices for Promoting Resilience, Department of Defense, Health Affairs (PD # 08-­‐542 & PD # 09-­‐512), 2007-­‐2010. Co-­‐Principal Investigator, Evaluation of Service Member and Family Education Needs about Traumatic Brain Injury (TBI), Department of Defense, Health Affairs (PD # 07-­‐538 & PD # 09-­‐508), 2007-­‐20011. Principal Investigator, Enhancing Emergency Preparedness, Response, and Recovery Management for Vulnerable Populations, Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation (Grant No. HHS-­‐100-­‐03-­‐0010), 2007-­‐2008. Principal Investigator, Preparing Hospitals and Clinics for the Psychological Consequences of a Terrorist Incident or Other Public Health Emergency, Los Angeles County Department of Public Health (H-­‐702133), 2006-­‐2007 Principal Investigator, Understanding the Mental Health Needs Resulting from Terrorist Incidents Involving Biological, Chemical, or Radiological Agents Bioterrorism, Hospital Preparedness Program, Los Angeles County Department of Health Services (LACOUNTY_4-­‐1-­‐05), 2005-­‐2006 Principal Investigator, Understanding Primary Care for PTSD and Symptoms, National Institute of Mental Health (R34MH070683), 2005-­‐2007 Principal Investigator, Watchful Waiting for Subthreshold Depression by Primary Care Providers, Robert Wood Johnson Foundation (Grant No. 048121), 2003-­‐2004 Principal Investigator, Evaluation of the DoD Mental Health Counselors Demonstration, Department of Defense, Health Affairs (PD # 02-­‐643), 2002-­‐2004 Principal Investigator, Using Behavioral Science to Explain PCP Depression Care, National Institute of Mental Health (R01MH62062), 2001-­‐2003 Principal Investigator, Patient-­‐Provider Managed Care Relationships, Robert Wood Johnson Foundation (PPRI 034894), 1998-­‐2000 Principal Investigator, Understanding the Content of Depression Counseling, First Independent Research Scientist Training Award, National Institute of Mental Health (R29MH55223), 1996-­‐2001 2 MEREDITH GRANTS AND CONTRACTS Completed (continued): Principal Investigator, UCLA/VA/RAND MEDTEP Center for Asians and Pacific Islanders, pilot project, Agency for Health Care Policy and Research, 1994; subproject: Cultural Adaptation of Self-­‐Report Health Measures, 1995-­‐1997 Principal Investigator, pre-­‐doctoral dissertation research award, Agency for Healthcare Research and Quality, 1991-­‐1992 Co-­‐Principal Investigator, Brief Youth Substance Use Intervention for Primary Care, National Institute for Drug Abuse (R21DA018854), 2004-­‐2006. Co-­‐Principal Investigator, Treatment of Adolescent Mood and Anxiety Disorders in Primary Care, Pfizer Inc. (Grant No. PFIZER_10/1/3003), 2003-­‐2007. Co-­‐Principal Investigator, Identifying Effective Clinician Incentives to Improve Depression Care, National Institute of Mental Health, 2004-­‐2008. Co-­‐Principal Investigator, Improving Care for Depression, National Institute of Mental Health, 1995-­‐2002 Co-­‐Principal Investigator, Improving Cost-­‐Effectiveness for Depression, Agency for Health Care Policy and Research, 1995-­‐2000 Co-­‐Principal Investigator, Inpatient Practices of Hospitalists vs. Traditional PCPs, Agency for Healthcare Research and Quality, 2000-­‐2001. PROFESSIONAL ORGANIZATIONS AcademyHealth American Psychological Association American Public Health Association International Society for Traumatic Stress Studies Society for the Psychological Study of Social Issues Western Psychological Association APPOINTMENTS, COMMITTEES AND PANELS Admissions Committee, Pardee RAND Graduate School, 2009-­‐2011 Dissertation Chair, Pardee RAND Graduate Student, John Langley, “Occupational Burnout among Air Force Distributed Common Ground System (DCGS) Personnel,” 2010-­‐2011 Dissertation Chair, Pardee RAND Graduate Student, Sarah Gaillot, “Disentangling Racial-­‐Ethnic and Gender Disparities in Trauma and Mental Health Service Use,” 2009-­‐2010 Panel Member, AHRQ Standing Review Group, Health Care Quality and Effectiveness Research (HCQER), 2008-­‐2011. Reviewer, AHRQ Special Emphasis Panel (10 Council ZHS1 HSR-­‐W 02 2), 2007 Committee Chair, AcademyHealth General Poster Review, 2007 Reviewer, AcademyHealth General Poster Review, 2006 Ad Hoc Representative, NIMH Special Emphasis Panel (ZMH1-­‐CRB-­‐1-­‐07), 2004 Ad Hoc Representative, NIMH Special Emphasis Panel (ZMH1-­‐NRB-­‐G-­‐07), 2002 Deputy Editor, Medical Care, 2002-­‐2007 RAND Psychology Speaker Series Co-­‐Coordinator, Recruit expert psychologists from outside the organization to speak at monthly brownbag lectures, 2001-­‐2007. Scientific Advisory Board Member, Minority Services Research Group, USC Keck School of Medicine, Department of Psychiatry (Isabel Lagomosino, MD/Megan Dwight, MD, PIs), 2005-­‐present. Expert Panel Member, Price Indexes for Major Depression, National Institute of Mental Health (conducted at Harvard Medical School, department of Health Care Policy, Richard Frank, PhD, PI), Summer 2002 Scientific Advisory Panel, Social Influences on Practice Study, National Institute of Mental Health (conducted at UC Davis Center for Health Services Research in Primary Care, Richard Kravitz, MD, PI), 2002-­‐2005 3 MEREDITH APPOINTMENTS, COMMITTEES AND PANELS (continued) Expert Panel Member, Problems in Managing Depression in Primary Care, Veterans’ Health and Well-­‐Being Study, VA Center for the Study of Healthcare Provider Behavior/Pfizer Health Solutions (Scott Sherman, MD, MPH, PI), September 2001 Steering Committee, Clinical Services Core of the UCLA/RAND Research Center on Managed Care for Psychiatric Disorders, 1995-­‐2003 Steering Committee, Quality Improvement for Depression, National Institute of Mental Health (Kathryn Rost, PhD, Dan Ford, MD, Lisa Rubenstein, MD, MSPH, PIs), 1997-­‐2004 Invited participant, Media Workshop, Robert Wood Johnson Foundation, May 2001 Ad Hoc Reviewer, RWJF Strengthening the Patient-­‐Provider Relationship in a Changing Health Care Environment program initiative, 1998 Guest Lecturer, UCLA Neuropsychiatric Institute Faculty Scholars Seminar, Models of Health Behavior from Social Psychology, 1999-­‐present Guest Lecturer, UCLA School of Public Health, Qualitative Methods, 2000 Consultant, UCLA/VA/RAND Medical Effectiveness Treatment Program (MEDTEP) Center for the Study of Asians and Pacific Islanders, 1998-­‐1999 Expert Panel Member, Veteran Identity Program, VA Health Services Research and Development (HSR&D), 1999-­‐2002 Consultant and Lecturer, UCLA Clinical Scholars Program, ongoing Volunteer Behavioral Scientist, Science-­‐by-­‐Mail Pen-­‐Pal Program: mentored children in grades 4-­‐9 to encourage and advise on classroom science projects, 1997-­‐2000 Dissertation Committee Member, UCLA Clinical Scholar, Rita Mangione-­‐Smith, M.D., “The Impact of Parental Expectations on Pediatrician Antimicrobial Prescribing Behavior,” 1996 EDITORIAL EXPERIENCE Archives of General Psychiatry BMC Family Practice (Editorial Board) Depression and Anxiety General Hospital Psychiatry Health Services Research International Journal of Psychiatry in Medicine International Journal of Quality in Health Care Journal of the American Medical Association Journal of General Internal Medicine Journal of Health Economics Journal of Managed Care Journal of Psychosomatic Research Journal of Social and Clinical Psychology Medical Care (formerly Deputy Editor) Mental Health Services Research Psychiatric Services Women & Health Women’s Health: Research on Gender, Behavior, and Policy Women’s Health Issues 4 MEREDITH PUBLICATIONS Journal Articles Ettner, S., Azocar, F., Branstrom, R., Meredith, L.S., Zhang, L. & Ong, M. (2010). Association of general medical and psychiatric comorbidities with receipt of guideline-­‐concordant care for depression. Psychiatric Services, 61, 1255-­‐ 1259. Zubkoff, L., Lorenz, K. A., Lanto, A. B., Sherbourne, C. D., Goebel, J. R., Glassman, Pl A., Shugarman, L., Meredith, L. S., Asch, S. M. (2010). Does screening for pain correspond to high quality care for veterans? Journal of General Internal Medicine, 25, 900-­‐905. Meredith, L. S., Branstrom, R. B., Azocar, F., Fikes, R., & Ettner, S. L. (2011). A collaborative approach to identifying effective incentives for mental health clinicians to improve depression care in a large managed behavioral healthcare organization. Psychiatric Services, 192-­‐202. Meredith L. S., Zazzali, J.L., Shields, S., Eisenman, D. P., Alsabagh, H. (2010) Psychological effects of patient surge in large-­‐ scale emergencies: a quality improvement tool for hospital and clinic capacity planning and response. Prehospital and Disaster Medicine. Prehospital and Disaster Medicine, 25, 107-­‐14. Meredith, L. S., Eisenman, D. P., Tanielian, T., Taylor, S. L., Basurto-­‐Davila, R., Zazzali, J., Diamond, D., Engleman, B., & Shields, S. (2010). Prioritizing “psychological” consequences for disaster preparedness and response: A framework for addressing the emotional, behavioral, and cognitive effects of patient surge in large-­‐scale emergencies. Disaster Medicine and Public Health Preparedness. Meredith, L. S., Zazzali, J. L., Shields, S., Eisenman, D., P., & Alsabagh, H. (2010). Psychological effects of patient surge in large-­‐scale emergencies: A quality improvement tool for hospital and clinic capacity planning and response. Disaster Medicine and Public Health Preparedness, 25, 107-­‐114. Shugarman, L. R., Asch, S. M., Meredith, L. S., Sherbourne, C. D., Hagenmeie,r E., Wen, L., Cohen, A., Rubenstein, L. V., Goebel, J., Lanto, A., Lorenz, K. A. Factors Associated with Clinician Intention to Address Diverse Aspects of Pain in Seriously Ill Outpatients, Pain Medicine, [Epub Aug 30 2010], 11, 1365-­‐1372. Shugarman, L. R., Goebel, J. R., Lanto, A., Asch, S. M., Sherbourne, C. D., Lee, M. L., Rubenstein, L. V., Wen, L., Meredith, L. S., Lorenz, K. A. (2010). Nursing Staff, Patient, and Environmental Factors Associated with Accurate Pain Assessment, Journal of Pain Symptom Management, 40, 725-­‐733. Zubkoff L., Lorenz K.A., Lanto A.B., Sherbourne C.D., Goebel J.R., Glassman P.A., Shugarman, L.R., Meredith L.S., Asch S.M. (2010). Does screening for pain correspond to high quality care for veterans? Journal of General Internal Medicine, 25, 889-­‐90. Burnam, M. A., Meredith, L. S., Tanielian, T., & Jaycox, L. H. (2009). Mental health care for Iraq and Afghanistan war veterans: Meeting combat-­‐related mental health needs requires broad services reform that looks beyond the Veterans Health Administration. Health Affairs, 28, 771-­‐782. Chandra, A. Scott, M., Jaycox, L. H., Meredith, L. S., Tanielian, T, Burnam, M. A. (2009). Racial/ethnic differences in teen and parent perspectives towards depression treatment. Journal of Adolescent Heath, 44, 546-­‐553. Goebel, J. R., Sherbourne, C. D., Asch, S. M., Meredith, L. S., Cohen, A. B., Hagemaier, E., Lanto, A. B., Simon, B., Rubenstein, L. V., Shugarman, L. R., Lorenz, K. A. (2009). Addressing patients’ concerns about pain management and addiction risks. Pain Management Nursing, 11, 92-­‐98. Jaycox, L. H., Stein, B. D., Paddock, S., Miles, J., Chandra, A., Meredith, L. S., Tanielian, T., Hickey, S., & Burnam, M. A. (2009). Impact of teen depression on academic, social, and physical functioning, Pediatrics, 124, 1180-­‐1191. Meredith, L. S., Eisenman, D. P., Green, B. L., Basurto-­‐Davila, R., Cassells, A., & Tobin, J. N. (2009). System factors affect the recognition and management of post-­‐traumatic stress disorder by primary care clinicians. Medical Care, 47, 686-­‐ 694. Meredith, L. S., Stein, B. D., Paddock, S. M., Jaycox, L. H., Quinn, V. P., Chandra, A., & Burnam, A. (2009). Perceived barriers to treatment for adolescent depression. Medical Care, 47, 677-­‐685. Meredith, L. S., Stein, B. D., Paddock, S. M., Jaycox, L. H., Quinn, V. P., Chandra, A., & Burnam, A. (2009). Perceived barriers to treatment for adolescent depression. Medical Care 47, 677-­‐685. Tanielian, T., Jaycox, L. H., Paddock, S., Meredith, L. S., Stein, B. D., & Burnam, M. A. (2009). Readiness for Treatment among Teens in Primary Care with Depression, Journal of Adolescent Medicine, 45, 490-­‐498.. 5 MEREDITH Journal Articles (continued) D’Amico, E.J., Miles, J.N.V., Stern, S.A., & Meredith, L.S. (2008). Brief motivational interviewing for teens at risk of substance use consequences: A randomized pilot study in a primary care clinic. Journal of Substance Abuse Treatment, 35, 53-­‐61. Dickinson, L. M., Dickinson, W. P., Rost, K., deGruy, F., Emsermann, C., Froshaug, D., Nutting, P. A., & Meredith, L. S. (2008). Clinician burden and depression treatment: Disentangling patient-­‐ and clinician-­‐level effects of medical comorbidity. Journal of General Internal Medicine, 23, 1763-­‐1769.. Eisenman, D. P., Meredith, L. S., Rhodes, H., Green, B. L., Kaltman, S., Cassells, A., & Tobin, J. N. (2008). PTSD in Latino patients: Illness beliefs, treatment preferences, and implications for care. Journal of General Internal Medicine, 23, 1386-­‐1392. Henke, R. E. M., McGuire, T. G., Zaslavsky, A. M., Ford, D. E., Meredith, L. S., & Arbelaez, J. J. (2008). Clinician and organization level factors in the adoption of evidence-­‐based care for depression in primary care. Health Care Management and Review, 33, 289-­‐299. Mendel, P., Meredith, L. S., Schoenbaum, M., & Sherbourne, C. D. (2008). A framework for community dissemination research: Applying social and behavioral theory to the spread of evidence-­‐based health interventions. Administration and Policy in Mental Health and Mental Health Services Research, 35, 21-­‐37. Bito, S., Matsumura, S., Singer, M. K., Meredith, L. S., Fukuhara, S., Wenger, N. S. (2007). Acculturation and end-­‐of-­‐life decision making: Comparison of Japanese and Japanese-­‐American Focus Groups, Bioethics, 21, 251-­‐262. Hepner, K. A., Rowe, M., Rost, K., Hickey, S. C., Sherbourne, C. D., Ford, D. E., Meredith, L. S., & Rubenstein, L. V. (2007). The effect of adherence to practice guidelines on depression outcomes. Annals of Internal Medicine, 147, 320-­‐329. Meredith, L. S., Cheng, W. J. Y., Hickey, S. C., & Dwight-­‐Johnson, M. (2007). Factors associated with primary care clinician choice of a watchful waiting approach to managing depression. Psychiatric Services, 58, 72-­‐78. Meredith, L. S., Eisenman, D. P., Rhodes, H., Ryan, G., Long, A. (2007). Trust influences response to public health messages during a bioterrorist event. Journal of Health Communication, 12, 217-­‐232. Parker, L. E., Altschuler, A., de Pillis, E., Rubenstein, L. V., Meredith, L. S., Gordon, N. (2007). Balancing participation and expertise: A comparison of locally and centrally managed quality improvement within primary care practices. Qualitative Health Review, 9, 1268-­‐1279. Stern, S. A., Meredith, L. S., Gholson, J., Gore, P., & D’Amico, E. J. (2007). Project CHAT: A brief motivational substance use intervention for teens in primary care. Journal of Substance Abuse Treatment, 32, 153-­‐165. Swanson, K. A., Bastani, R., Rubenstein, Meredith, L. S., & L. V. Ford, D. E. (2007). Effect of mental health care and shared decision-­‐making on patient satisfaction in a community sample of patients with depression. Medical Care Research and Review, 64, 416-­‐430. Chan, K. S., Bird, C. E., Weiss, R., Duan, N., Meredith, L. S., & Sherbourne, C. C. (2006). Does patient-­‐provider gender concordance affect mental health care received by primary care patients with major depression? Women’s Health Issues, 16, 122-­‐132. Clever, S. L., Ford, D. E., Rubenstein, L. V., Rost, K. M., Meredith, L. S., Sherbourne, C. D., Wang, N-­‐Y, Arbelaez, J. J., Cooper L. A. (2006). Primary care patients’ involvement in decision-­‐making is associated with improvement in depression. Medical Care, 44, 398-­‐405. Johnson, M., Meredith, L. S., Hickey, S. C., Wells, K. B. (2006). Influence of patient preference and primary care clinician proclivity for watchful waiting on receipt of depression treatment. General Hospital Psychiatry, 28, 379-­‐386. Johnson, M., Meredith, L. S., Hickey, S. C., Wells, K. B. (2006). Influence of patient preference and primary care clinician proclivity for watchful waiting on receipt of depression treatment. General Hospital Psychiatry, 28, 379-­‐386. Kravitz, R. L., Franks, P., Feldman, M., Meredith, L. S., Hinton, L., Franz, C., Duberstein, P., & Epstein, R. M. (2006). What drives referral from primary care physicians to mental health specialists? A randomized trial using actors portraying depressive symptoms. Journal of General Internal Medicine, 21, 584-­‐589. Meredith, L. S., Mendel, P., Pearson, M, Wu, S. Y. Joyce, G., Straus, J. B., Ryan, G., Keeler, E., & Unützer, J. (2006). Implementation and maintenance of quality improvement for treating depression in primary care, Psychiatric Services, 57, 48-­‐55. 6 MEREDITH Rubenstein, L. V., Meredith, L. S., Parker, L. E., Gordon, N. P., Hickey, S. C., Oken, C., & Lee, M. L. (2006). Impacts of evidence-­‐based quality improvement on depression in primary care: A randomized experiment. Journal of General Internal Medicine, 21, 1027-­‐1035. Journal Articles (continued) Srinvasan, M., Franks, P., Meredith, L. S., Fiscella, K., Epstein, R., & Kravitz, R. L. (2006). Connoisseurs of care? Unannounced standardized patients’ ratings of physicians. Medical Care, 44, 1092-­‐1098. Balsa, A. I., McGuire, T. G., Meredith, L. S. (2005). Testing for statistical discrimination in health care, Health Services Research, 40, 227-­‐252. Beach, M. C., Meredith, L. S., Halpern, J., Wells, K. B., Ford, D. E. (2005). Physician conceptions of loyalty to patients and social justice in health care, Annals of Family Medicine, 3, 53-­‐59. Meredith, L. S., Yano, E. M., Hickey, S. C., & Sherman, S. E. (2005). Primary care provider attitudes are associated with smoking cessation counseling and referral, Medical Care, 43. Tarn, D. M., Meredith, L. S., Kagawa-­‐Singer, M., Matsumura, S., Bito, S., Oye, R. K., Liu, H., Kahn, K. L., Fukuhara, S., & Wenger, N. S. (2005). Trust in one’s physician: The role of ethnic match, autonomy, acculturation, and religiosity among Japanese and Japanese Americans. Annals of Family Medicine, 3, 339-­‐347. Wells, K. B., Sherbourne, C., Duan, N., Unutzer, J., Miranda, J., Schoenbaum, M., Ettner, S. L., Meredith, L. S., Rubenstein, L. (2005). Quality improvement for depression in primary care: Do patients with subthreshold depression benefit in the long run? American Journal of Psychiatry, 162, 1149-­‐1157. Meredith, L. S. (2004). Depression: 20 years of progress, Medical Care, 42, 499-­‐501. Cooper, L. A., Gonzales, J. J., Gallo, J. J., Rost, K. M., Meredith, L. S., Rubenstein, L. V., Wang, N-­‐Y., & Ford, D. E. (2003). The acceptability of treatment for depression among African American, Latino, and white primary care patients, Medical Care. 41,479-­‐489, Jaycox, L. H., Miranda, J., Meredith, L. S., Duan, N., Benjamin, B., & Wells, K. (2003). Impact of a primary care quality improvement intervention on use of psychotherapy for depression. Mental Health Services Research, 5, 109-­‐120. Marshall, G. N., Sherbourne, C. D., Meredith, L. S., Camp, P., & Hays, R. D. (2003). The tripartite model of anxiety and depression: Symptom structure in depressive and hypertensive patient groups. Journal of Personality Assessment, 80, 139-­‐153. Van Voorhees, B. W., Cooper, L. A., Rost, K. M., Nutting, P., Rubenstein, L. V., Meredith, L. S., Wang, N., & Ford, D. E. (2003). Primary care patients with depression are less accepting of treatment than those seen by mental specialists. Journal of General Internal Medicine, 18, 991-­‐1000. Gallo, J. J., Meredith, L. S., Gonzales, J., Cooper, L. A., Nutting, P., Ford, D., & Rubenstein, L. V., Rost, K., & Wells, K. B. (2002). Do family physicians and internists differ in knowledge, attitudes and self-­‐reported approaches for depression? International Journal of Psychiatry in Medicine, 32, 1-­‐20. Meredith, L. S., & Griffith-­‐Forge, N. (2002). The road to eliminating disparities in health care. Medical Care, 40, 729-­‐731. Meredith, L. S., Humphrey, N., Orlando, M., Camp. (2002). Knowledge of health care benefits among patients with depression, Medical Care, 40, 338-­‐346. Orlando, M., & Meredith, L. S. (2002). Understanding the causal relationship between patient ratings of care and quality of care for depression, Medical Care, 696-­‐704. Rubenstein, L. V., Parker, L. E., Meredith, L. S., Altschuler, A., de Pillis, E., Hernandez, J., Gordon, N. P. (2002). Understanding team-­‐based quality improvement for depression in primary care, Health Services Research, 37, 1009-­‐ 1029. Meredith L. S., Sturm R., Camp P., & Wells K. B. (2001). Effects of cost containment strategies within managed care on continuity of the relationship between depressed patients and their primary care providers. Medical Care, 39, 1075-­‐ 1085. Meredith, L. S., Carney, M. F., Wells, K. B. (2001). Cost-­‐effectiveness of practice-­‐initiated quality improvement for depression: Results of a randomized controlled trial. Journal of the American Medical Association, 286, 1325-­‐1330. Meredith, L. S., Orlando, M., Humphrey, N., Camp, P., & Sherbourne, C. D. (2001). Are better ratings of the patient-­‐ provider relationship associated with higher quality care for depression? Medical Care, 39, 349-­‐360. 7 MEREDITH Journal Articles (continued) Rost, K. M., Duan, N., Ruben, L. V., Ford, D. E., Sherbourne, C. D., Meredith, L. S., Wells, K. B. (2001). The Quality Improvement for Depression collaboration: General analytic strategies for a coordinated study of quality improvement for depression care. General Hospital Psychiatry, 23, 239-­‐253. Borowsky, S., Rubenstein, L. V., Meredith, L. S., Camp, P., Jackson-­‐Triche, M., & Wells, K. B. (2000). Who is at risk for non-­‐detection of mental health problems in primary care? Journal of General Internal Medicine, 15, 381-­‐388. Harada, N., Meredith, L. S., Liu, H., Stewart, A., Makinodan, T., Kahn, K. (2000). Does acculturation influence physical activity in Japanese American Older Adults? Asian American and Pacific Islander Journal of Health, 8,130-­‐137. Meredith L. S. & Mazel R. M. (2000) Counseling for depression by primary care providers. International Journal of Psychiatry in Medicine, 30, 343-­‐365. Meredith, L. S., Jackson-­‐Triche, M., Duan, N., Rubenstein, L. V., Camp, P., & Wells, K. B. (2000). Quality improvement for depression enhances long-­‐term treatment knowledge for primary care providers. Journal of General Internal Medicine, 15, 859-­‐867. Sherbourne, C. D., Wells, K. B., Duan, N., Miranda, J., Unützer, J., Jaycox, L., Schoenbaum, M., Meredith, L. S., & Rubenstein, L. V. (2000) Long-­‐term effectiveness of disseminating quality improvement for depression in primary care, Archives of General Psychiatry, 58, 696-­‐703. Wells, K. B., Sherbourne, C., Schoenbaum, M., Duan, N., Meredith, L. S., Unützer, J., Miranda, J., Carney, M.F., & Rubenstein, L.V. (2000). Impact of disseminating quality improvement programs for depression to managed primary care: A randomized, controlled trial. Journal of American Medical Association, 282, 212-­‐220. Lee, P. P., Meredith, L. S., Whitcup, S. M., Spritzer, K., & Hays, R. D. (1999). A comparison of the self-­‐reported utilization of ophthalmic care for diabetes in managed care versus fee-­‐for-­‐service. Retina, 18, 356-­‐369. Meredith, L. S., Rubenstein, L. V., Rost, K. M., Ford, D. E., Gordon, N., Nutting, P., Camp, P. & Wells, K.B. (1999). Treating depression in staff-­‐model vs. network-­‐model managed care organizations. Journal of General Internal Medicine, 14, 39-­‐48. Meredith, L. S., Rubenstein, L. V., Rost, K. M., Ford, D. E., Gordon, N., Nutting, P., Camp, P. & Wells, K.B. (1999). Treating depression in staff-­‐model vs. network-­‐model managed care organizations. Journal of General Internal Medicine, 14, 39-­‐48. Meredith, L. S., Wenger, N., Harada, N., Liu, Honghu, L., & Kahn, K. (1999). Development of a brief scale to measure acculturation among Japanese Americans. Journal of Community Psychology, 28, 103-­‐113. Meredith, L. S., Sherbourne, C. D., Jackson, C. A., Camp, P., & Wells, K. B. (1997). Treatment typically provided for comorbid anxiety disorder. Archives of Family Medicine, 6, 231-­‐237. Meredith, L. S., Wells, K. B., Kaplan, S., & Mazel, R. M. (1996). Counseling typically provided for depression: Role of clinician specialty and payment system. Archives of General Psychiatry, 53, 905-­‐912. Sherbourne, C. D., Jackson, C. A., Meredith, L. S., Camp, P. & Wells, K. B. (1996). Prevalence of comorbid anxiety disorders in general medical and mental health specialty outpatients. Archives of Family Medicine, 5, 27-­‐34. Sherbourne, C. D., Wells, K. B., Meredith, L. S., Jackson, C. A., & Camp, P. (1996). Comorbid anxiety disorder and the functioning and well-­‐being of chronically ill patients of general medical providers. Archives of General Psychiatry, 53, 889-­‐895. Sturm, R., Meredith, L. S., & Wells, K. B. (1996). Provider choice and continuity for the treatment of depression. Medical Care, 34, 723-­‐734. Meredith, L. S., & Siu, A. L. (1995). Variation and quality of self-­‐report health data: Asians and Pacific Islanders compared to other ethnic groups. Medical Care, 33, 1120-­‐1131 Sturm, R., Jackson, C., Meredith, L. S., Yip, W., Manning, W. G., Rogers, W. H., & Wells, K. B. (1995). Mental health care utilization in prepaid and fee-­‐for-­‐service plans among depressed patients in the Medical Outcomes Study. Health Services Res, 30, 319-­‐340 Meredith, L. S., Wells, K. B., & Camp, P. (1994). Clinician specialty and treatment style for depressed outpatients in primary care with and without medical comorbidities. Archives of Family Medicine, 3, 1065-­‐1072. Sturm, R., McGlynn, E., Meredith, L. S., Wells, K. B., Manning, W. G., & Rogers, W. H. (1994). Health plan and provider switching among depressed patients in the Medical Outcomes Study. Medical Care, 32, 917-­‐929. 8 MEREDITH Journal Articles (continued) Rogers, W. H., Wells, K. B., Meredith, L. S., Sturm, R., & Burnam, M. A. (1993). Outcomes for adult outpatients with depression under prepaid or fee-­‐for-­‐service financing. Archives of General Psychiatry, 50, 517-­‐525. Sherbourne, C. D., Hays, R. D., Meredith, L. S., & Mazel, R. M. (1993). Life events as benchmarks for quality of life changes in the MOS SF-­‐36. Quality of Life Res, 3, 55-­‐65. Schoenbaum, M., Unützer, J., Sherbourne, C., Duan, N., 009, L. V., Miranda, J., Sherbourne, C. D., & Meredith, L. S. (1992). Quality of self-­‐report data: A comparison of older and younger chronically ill patients. Journals of Gerontology, 47(4), S204-­‐S211. Meredith, L. S., & Wilsoncroft, W. E. (1989). Time perception: Effects of sensory modality, ambient illumination and intervals. Perceptual and Motor Skills, 68, 373-­‐374. Books and Book Chapters Meredith, L. S., Sturm, R., & Wells, K. B. (1999). A naturalistic study of psychotherapy: The Medical Outcomes Study approach. In N. E. Miller & K. M. Magruder (Eds.), Cost-­‐effectiveness of psychotherapy: A guide for practitioners, researchers, and policymakers (pp. 52-­‐62). New York: Oxford University Press. Wells, K. B., Sturm, R., Sherbourne, C. D., & Meredith, L. S. (1996). Caring for Depression. Cambridge, MS: Harvard University Press. Meredith, L. S., Sherbourne, C. D, Gaillot, S., Hansell, L., Ritschard, H. V., Parker, A. M., Wrenn, G. (2011). Promoting Psychological Resilience in the U.S. Military. Santa Monica, CA: RAND Corporation, MG-­‐996-­‐OSD. Chandra, A., Acosta, J., Meredith, L.S., Sanches, K., Stern, S., Uscher-­‐Pines, L., Williams, M., Yeung, D. (2010). Understanding Community Resilience in the Context of National Health Security a Literature Review, RAND WR-­‐737-­‐ DHHS. Santa Monica, CA: RAND Corporation. Burnam, M. A., Meredith, L. S., Helmus, T. C., Burns, R. M., Cox, R. A., D’Amico, E., Martin, L. T., Vaiana, M. E., Williams, K. M., & Yochelson, M. R. (2008). Systems of care: Challenges and opportunities to improve access to high-­‐quality care. In T. Tanielian & L. H. Jaycox (Eds.), Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery, RAND MG-­‐720-­‐CCF. Santa Monica, CA: RAND Corporation. Parker, A. M., Meredith, L. S., Albright, D. L., Burns, R. M., Gaillot, S. J. (in press). Informing Current and Former Service Members and Their Families About Traumatic Brain Injury, RAND TR-­‐1123-­‐OSD. Santa Monica, CA: RAND Corporation. Meredith, L. S., Parker, A. M, Beckjord, E. B., Gaillot, M., Trivedi, M., & Vaiana, M. E. (2008a). Post-­‐Deployment Stress: What You Should Know, What You Can Do. Santa Monica, CA: RAND Corporation, CP-­‐534. Meredith, L. S., Parker, A. M, Beckjord, E. B., Gaillot, M., Trivedi, M., & Vaiana, M. E. (2008b). Post-­‐Deployment Stress: What Families Should Know, What Families Can Do. Santa Monica, CA: RAND Corporation, CP-­‐535. Meredith, L. S., Shugarman, L. R., Chandra, A., Taylor, S. L., Stern, S. A., Beckjord, E. B., Parker, A. M., & Tanielian, T. (2008). Analysis of Risk Communication Strategies and Approaches with At-­‐Risk Populations to Enhance Emergency Preparedness, Response, and Recovery: Final Report. Santa Monica, CA: RAND Corporation, WR-­‐598-­‐HHS. Meredith, L. S., Eisenman, D. P., Tanielian, T., Taylor, S. L., & Basurto, R. (2007). Preparing Hospitals and Clinics for the Psychological Consequences of a Terrorist Incident or Other Public Health Emergency and Preparing Los Angeles County Department of Mental Health Staff to Respond to Hospitals and Clinics Following Large-­‐Scale Emergencies. Santa Monica, CA: RAND Corporation, TR-­‐493-­‐HS. Meredith, L. S., Tanielian, T.L., Greenberg, M. D., Suarez, A. P., & Eiseman, E. Expanding access to mental health counselors: Evaluation of the TRICARE Demonstration. (2005). Publication No. TR-­‐3458-­‐1-­‐OSD, Santa Monica, CA: RAND. Kravitz, R. L., Kahan, J. P., Jacobson, P. D., Meredith, L. S., Coulter, I. D., Tonesk, X., Garber, S., Shekelle, P. & Bozzette, S. (1993). The roles of physicians in the twenty-­‐first century: A research agenda. Publication No. P-­‐7848, Santa Monica, CA: RAND. Burnam, M. A., Meredith, L. S., Sherbourne, C. D., Valdez, R. B., & Vernez, G. (1992). Army families and soldier readiness. Publication No. R-­‐3884-­‐A, Santa Monica, CA: RAND. 9 MEREDITH Other Published Reports and Documents (continued) Kanouse, D. E., Brook, R. H., Winkler, J. D., Kosecoff, J., Berry, S. H., Carter, G. M., Kahan, J. P., McClosky, L., Rogers, W. H., Winslow, C. M., Anderson, G. M., Brodsley, L., Fink, A., & Meredith, L. S. (1989). Changing medical practice through technology assessment: An evaluation of the NIH consensus development program, Publication No. R-­‐3452-­‐ NIH/RC, Santa Monica, CA: RAND. Tanielian, T. L., Jaycox, L. H., Schell, T. Ll., Marshall, G. N., Burnam, M. A., Eibner, C., Karney, B. R., Meredith, L. S., Ringel, J. S., Vaiana, M. E., & the Invisible Wounds Study Team. (2008). Invisible Wounds of War: Summary and Recommendations for Addressing Psychological and Cognitive Injuries. RAND MG-­‐720-­‐CCF: Santa Monica, CA: RAND Corporation. Zellman, G. L., Johansen, A. S., & Meredith, L. S. (1992). Improving the delivery of military child care: An analysis of current operations and new approaches. Publication No. R-­‐4145-­‐FMP, Santa Monica, CA: RAND. Zima, B. T., Meredith, L. S., McClure, J., Kostello, E. C., Knapp, P., Woo, D. F. (2005). Caring for the psychological consequences of terrorism for children: A road map for the development, implementation, and dissemination of a training program for primary care providers. State of California Department of Health, Children Health and Disability Program, Sacramento, CA. Manuscripts Under Review, Under Revision, and In Preparation: Helfrich, C., Dolan, E., Fihn, S., Rodriguez, H. P., Meredith, L. S., Rosland, A-­‐M., Lempa, M., Wakefield, B. J., Joos, S., Stark, R., Schectman, G., & Nelson, K. (under review). Patient centered medical home implementation and burnout at VA clinics, Journal of General Internal Medicine. Meredith, L. S., Eisenman, D. P., Green, B. L., Kaltman, S., Wong, E. C., Han, B., Cassells, A., Tobin, J. N. (under review). Design of the Violence and Stress Assessment (ViStA) Study: Translating Quality Improvement Approaches to Improve PTSD Care in Safety Net Health Centers. General Hospital Psychiatry. Meredith, L. S., Schmidt, N., Darling, J., Rodriguez, H. P., Stockdale, S., Cordasco, K., Yano, B., & Rubenstein, L. V. (in preparation). Capacity and Clinician/Staff Receptivity to Change to the VHA’s Patient-­‐Aligned Care Team (PACT) in Primary Care: Impact on Burnout. Journal of General Internal Medicine (Supplement). Unpublished Manuscripts Bao, Y., Meredith, L. S., Orlando, M., Martino, S. (unpublished). What determines depression treatment in primary care? A joint mode of provider and patient behavior. Bower, T., Meredith, L. S., Garber, S., Geschwind, S. A., Duan, N. (unpublished). Developing methods for studying costs and benefits of Federal environmental regulations for small community Governments. Publication No. DRU-­‐787-­‐EPA, Santa Monica, CA: RAND. Geschwind, S. A., Meredith, L. S., Duan, N. (unpublished). A Breath of Fresh Air: Rethinking National Environmental Policy from Pollutant Source to Exposure. Jackson, C.A., Sherbourne, C. D., Meredith, L. S., Camp, P., Wells, K. B. (unpublished). Impact of comorbid anxiety disorders on the utilization of services by patients with depression and chronic medical illnesses. Martino, S. C., Meredith, L. S., Orlando, M. (unpublished). Applying expectancy-­‐value frameworks to predict primary care provider treatment for depression. Meredith, L. S., Parker, A. M., Beckjord, E. B., Gaillot, S., Trivedi, M. M., & Vaiana, M. E. (under revision). Educating military personnel and their families about post-­‐deployment stress. Military Psychology. Meredith, L. S., Orlando, M., Martino, S. C. (unpublished). Applying behavioral science theory to primary care clinician behavior. Meredith, L. S., Orlando, M., Mazel, R. (unpublished). Reliability and validity of self-­‐reports for assessing depression counseling by primary care providers. Meredith, L. S., Harada, N., Marshall, G., Wenger, N., Kahn, K. (unpublished). Health-­‐related quality of life among Japanese Americans. 10 MEREDITH Unpublished Manuscripts (continued) Meredith, L. S., Valdez, R. B., Andrews, C., Smith, J. (unpublished). Maternal response bias associated with the relationship between ETS exposure and children's health. Miranda, J., Meredith, L. S., & Jaycox, L. (unpublished). A public health perspective on treating mental disorders: Opportunities and challenges for psychologists. Yochelson, M. R., Meredith, L. S., & Karney, B. R. (unpublished). More research and clinical services needed to aid combat wounded servicemembers with TBI. [Optional Editorial] Published Abstracts Stern, S. A., Gholson, J., Meredith, L. S., Gore, P., D’Amico, E. J. (2006). Brief motivational substance use intervention for adolescents in primary care. Poster presented at the annual meeting for the Research Society on Alcoholism, Baltimore, MD. (Abstracted in Alcoholism: Clinical & Experimental Research, 30, p. 100A). Cooper-­‐Patrick L., Gonzales J. J., Rost, K., Meredith L., Rubenstein L., & Ford D.E. (1998). Patient preferences for treatment of depression. Paper presented at the NIMH Effectiveness of Interventions in Primary Care Conference, Baltimore, July, 1998, and has been published in the International Journal of Psychiatry in Medicine, 28, 382. Gallo, J., Meredith, L., Gonzalez, J., Nutting, P., Ford, D., & Rubenstein, L. V. (1998). How do family physicians and internists differ in attitude and approaches to depression in primary care. International Journal of Psychiatry in Medicine, 28, 384. Meredith, L., Miranda, J., Jaycox, L. & Wells, K. (1998). Which medical providers counsel their patients about depression? International Journal of Psychiatry in Medicine, 28, 395. Meredith, L. S., Wells, K. Rost, K., Nutting, P., Ford, D., Gordon, N. & Rubenstein, L. V. (1997). Treating depression in managed care organizations: what do primary care providers think, know, and do about it? International Journal of Psychiatry in Medicine, 27, 313. PRESENTATIONS Provider Perceptions and Experiences from the VAIL Evaluation, CyberSeminar, Veterans Health Administration Health Services Research & Development Center for the Study of Healthcare Provider Behavior, February, 2013. [invited] Facilitating the Nursing Role Transformation in PACTs, CyberSeminar, Veterans Health Administration Health Services Research & Development Center for the Study of Healthcare Provider Behavior, August, 2012. [invited] Addressing PTSD in Underserved Populations, World Congress on Traumatic Stress, Mexico City, Mexico, May 2012. Overcoming Challenges to Implementing Quality Improvement for PTSD in Community Health Centers: The Violence and Stress Assessment (ViStA) Study, International Society for Traumatic Stress Studies, Los Angeles, CA, November 2012. Challenges in Translating Trauma Care Interventions Across Organizations and Cultures (symposium title, Chair) and Challenges in Adapting PTSD Quality Improvement for Underserved Populations in Community Health Centers (symposium presentation), International Society for Traumatic Stress Studies, Montreal, Canada, November 2010. Expanding Access to Mental Health Counselors: Evaluation of the TRICARE Demonstration, Institute of Medicine of the National Academies, April 2009. Teen Depression Awareness Project (TDAP), Panel, AcademyHealth Child Health Services Research Meeting, Washington DC, June, 2008. PTSD Management in Primary Care: System-­‐Level Factors Associated with its Management, International Society for Traumatic Stress Studies, Baltimore, MD, November 2007. System Factors Associated with PTSD Management in Primary Care, National Institute of Mental Health Conference on Mental Heath Services Research, Washington, DC, July 2007. PTSD in Primary Care: System-­‐Level Factors Associated with its Management, Society for General Internal Medicine, Toronto, Ontario, Canada, April 2007. Identifying Effective Clinician Incentives to Improve Depression Care, Academy of Psychosomatic Medicine, Tucson, AZ, November 2006. 11 MEREDITH PRESENTATIONS (continued) Addressing the Psychological Consequences of a Terrorist Incident or Other Public Health Emergency, International Society for Traumatic Stress Studies, Los Angeles, CA, November 2006. Primary Care for PTSD and Trauma-­‐Related Mental Health Symptoms in Community Health Centers, Society of General Internal Medicine, Los Angeles, CA, April 2006. How does trust influence response to public health messages during a bioterrorist event? AcademyHealth, Seattle, WA, June 2006. Continuous Performance Improvement: The Need for Data, Research, and Evaluation for Disaster Readiness and Response, Substance Abuse and Mental Health Services Association National Disaster Behavioral Health Summit, New Orleans, LA, May 2006. [invited] Factors Associated with Primary Care Clinicians’ Decisions to Choose Watchful Waiting for Depression, National Institute of Mental Health Conference on Mental Heath Services Research, Bethesda, MD, July, 2005 Identifying Effective Clinician Incentives to Improve Depression Care: A collaboration between researchers and the managed behavioral healthcare community, AcademyHealth, Boston, MA, June, 2005 Military Family Use of TRICARE Mental Health Services, American Psychological Association, Waikiki, HI, August 2004. The Role of Education in Changing Provider Behavior: Theoretical Basis, South Central Mental Illness Research, Education, and Clinical Center Annual Retreat, Little Rock, AK, March 2004. [invited] Sustainability of Collaborative Depression Management Programs: Lessons from the RAND Evaluation of the Institute for Healthcare Improvement’s Breakthrough Series for Depression, Robert Wood Johnson Foundation, National Advisory Committee and Grantee Annual Meeting, Huntington Beach, CA, November 2004. [invited] Success of Implementation and Maintenance of Quality Improvement for Depression Academy Health, San Diego, CA, June 2004 Understanding and Changing Primary Care Clinician Behavior, Clinical Directors Network Web Cast, October 2003. [invited] Applying Decision Making Theories to Provider Treatment for Depression, Western Psychological Association, Vancouver, British Columbia, May 2003. Primary Care Provider Attitudes Predict Reported Smoking Cessation Behavior, Society for General Internal Medicine, Vancouver, British Columbia, May 2003. Effectiveness of Evidence-­‐Based Quality Improvement Process for Depression: A Randomized Controlled Experiment, Beyond the Clinic Walls: Expanding Mental Health, Drug and Alcohol Services Research Outside the Specialty Care System NIMH, NIDA, NIAAA, Washington DC, March 2003. Partners in Care Study: Improving Care for Depression in Medical Settings. Society for Psychotherapy Research, Santa Barbara, CA, June 2002. Using Social Cognitive Theory to Predict Primary Care Provider Depression Care Practices, National Institute of Mental Health Conference on Mental Heath Services Research, Washington, DC, April 2002. Why don’t we do a provider survey? Tips on conducting surveys of health care providers, Veterans Administration Health Services Research and Development Workshop (co-­‐Presenter), Washington DC, February 2002. Meeting the needs of all Americans: Lessons from Partners in Care (PIC), Campaign for America’s Mental Health Training Conference, National Mental Health Association, January 2002. [invited] Patient-­‐Provider Relationships: Content, Quality, and Continuity, University of Pittsburgh School of Medicine, Center for Continuing Education in the Health Sciences, January 2002. [invited] Understanding and Preparing for the Psychological Effects of Terrorism, Institute of Medicine, Neuroscience and Behavioral Health Board, Irvine, CA, December 2001. [invited] Effects of Cost Containment Strategies within Managed Care on Continuity of the Relationship between Depressed Patients and their Primary Care Providers, Academy for Health Services Research and Health Policy, Atlanta, GA, June 2001. Counseling for Depression in Staff-­‐Model Managed Care Organizations, Society of General Internal Medicine, San Diego, CA, May 2001. Are Better Ratings Of The Patient-­‐Provider Relationship Associated With Higher Quality Of Care For Depression? Association for Health Services Research Conference, Los Angeles, CA, June 2000. 12 MEREDITH PRESENTATIONS (continued) Predictors of Depression Counseling by Primary Care Providers. National Institute of Mental Health Research Conference on Mental Health Problems in the General Health Sector, Washington, DC, July 2000. Effects of Quality Improvement for Depression on Clinicians’ Knowledge and Perceptions of the Care They Provide. Association for Health Services Research Conference, Chicago, IL, June 1999. Understanding the Content of Counseling for Depression. National Institute of Mental Health International Research Conference on Mental Health Problems in the General Health Sector, Washington DC July 1999. Partners in Care: Effectiveness of a Quality Improvement Intervention for Depression in Primary Care. American Association for Behavioral Therapy Annual Meeting, Washington DC, November 1998. [invited] Which Medical Providers Counsel Their Patients About Depression? National Institute of Mental Health International Conference on Mental Health Problems in the General Health Care Sector, Baltimore, MD, September 1998. Treating Depression in VA and other Managed Care Organizations, Veterans Administration Health Services Research and Development Annual Meeting, Washington DC, February 1998. Treating Depression in Managed Care Organizations: What Do Primary Care Providers Think, Know, and Do About It? National Institute of Mental Health International Conference on Mental Health Problems in the General Health Care Sector, Washington DC, September 1997. Cultural Issues Associated with Self-­‐Reported Health Among Japanese Americans, Association for Health Services Research Conference, Chicago, IL, June 1997. A Health Services Research Perspective: The Provider as Subject of Managed Care Research, Panelist in Plenary Session: Conducting Mental Health Research in Primary Care Settings in an Era of Managed Care, National Institute of Mental Health International Conference on Mental Health Problems in the General Health Care Sector, Bethesda, MD, July 1996, [invited] Treatment Typically Provided for Comorbid Anxiety Disorder. National Institute of Mental Health International Conference on Mental Health Problems in the General Health Care Sector, Bethesda, MD, July 1996. Variation in Treatment of Patients in Primary Care Settings: Asians and Pacific Islanders vs. Other Ethnic Groups, Association for Health Services Research Conference, San Diego, CA, June 1994. Variation and Quality of Self-­‐Report Health Data: Asians and Pacific Islanders Compared to Other Ethnic Groups. UCLA Symposium: Health Outcomes Research in A Multicultural Community, Los Angeles, CA, October 1994. Provider and Patient Gender Differences in Psychosocial Treatment Style. American Psychological Association National Multidisciplinary Conference, Psychosocial and Behavioral Factors in Women's Health: Creating an Agenda for the 21st Century, Washington DC, May 1994. Changing Environmental Attitudes Towards Indoor Exposures to Chemicals. American Psychological Association, Los Angeles, California, August 1994. Treatment Style for Depression in Prepaid or Fee-­‐for-­‐Service Care. American Public Health Association, San Francisco, California, October 1993. Maternal Response Biases Associated with the Relationship Between ETS Exposure and Children’s Health. Annual Scientific Conference for the Tobacco-­‐Related Disease Research Program, San Francisco, CA, December 1993. Clinician Specialty and Treatment Style for Depressed Outpatients With and Without Medical Comorbidities. National Institute of Mental Health International Research Conference on Mental Health Problems in the General Health Sector, Washington DC, September 1993. Clinician Style of Care for Depression. Society of Behavioral Medicine, San Francisco, California, June 1993. Psychosocial Factors and Health Care Utilization in Chronically Ill Patients. American Psychological Association, Washington DC, August 1992. Stressful Life Events and Health Outcomes in Older Patients with Chronic Illness. American Psychological Association, San Francisco, California, August 1991. Measuring Life Events by Age in the Chronically Ill. Western Psychological Association, San Francisco, California, April 1991. Rev: 2/18/13 13