W O R K I N G Assessing Health and
advertisement

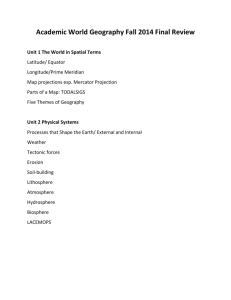
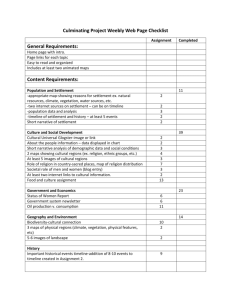
WORKING P A P E R Assessing Health and Health Care in the District of Columbia Phase 2 Report RAND AUTHORS: NICOLE LURIE, CAROLE ROAN GRESENZ, JANICE C. BLANCHARD, ANITA CHANDRA, BARBARA O. WYNN, KRISTY GONZALEZ MORGANTI, TEAGUE RUDER, AND AMBER PRICE This product is part of the RAND Health working paper series. RAND working papers are intended to share researchers’ latest findings and to solicit additional peer review. This paper has been peer reviewed but not edited. Unless otherwise indicated, working papers can be quoted and cited without permission of the author, provided the source is clearly referred to as a working paper. RAND’s publications do not necessarily reflect the opinions of its research clients and sponsors. is a registered trademark. GEORGE WASHINGTON UNIVERSITY AUTHORS: DONNA SICKLER, BONNIE NORTON, JANICE C. BLANCHARD, KAREN JONES, MARSHA REGENSTEIN, AND BRUCE SIEGEL WR-579 June 2008 EXECUTIVE SUMMARY As a result of the recent settlement of tobacco litigation, the District of Columbia has more than $200 million available to invest in the health of the city’s residents. A Health Care Task Force, convened in 2006 by then-Mayor Anthony Williams, considered alternative ways to invest the available funds. The Task Force crafted several options that included investment in additional or improved hospital capacity, ambulatory care, and health care system improvement, but agreed that research was needed before final investment decisions could be made. The District contracted with the RAND Corporation to study health and the health care delivery system in the District. The goals of RAND’s evaluation are to: 1) Conduct a comprehensive health needs assessment for Washington D.C.; 2) Assess the quality and accessibility of the District’s health care delivery system for individuals with urgent or emergent medical needs; and, 3) Use information from those assessments to identify and assess various policy options for improving the health care delivery system. An interim report (http://www.rand.org/pubs/working_papers/WR534/) summarizes findings related to the first two goals. Since the release of the interim report, we conducted additional quantitative and qualitative analyses. Specifically, we: x Conducted focus groups with community residents. x Interviewed and convened focus groups with District health care providers. x Synthesized information describing the health care safety net in the District. x Conducted additional analyses of Medicaid and Alliance managed care claims data, hospital discharge data, and data on Medicaid provider capacity from the Medicaid Assistance Administration (MAA). x Surveyed each of the eight acute care hospitals in the District of Columbia to get additional information about hospital and emergency department patient flow and staffing. x Analyzed data from D.C. Fire and Emergency Medical Services (FEMS), including six years of computer-aided dispatch (CAD) data and data from electronic run sheets for a two-month period in 2006. x Obtained and analyzed information about the times at which patients first present to emergency departments. In addition, we visited six clinics and discussed our findings and with a wide array of stakeholders, including representatives from DCHA, staff at individual hospitals and clinics, representatives from DCPCA, and the RAND Advisory Committee appointed by the Mayor and City Council. Findings are presented in the body of the full report. The majority of the report addresses the third goal. Legislation passed in December 2006 allocated some of the tobacco settlement funds, including $20 million for cancer prevention, $10 iv million for anti-smoking efforts, $10 million for chronic disease treatment, $6 million for establishing a regional health information exchange, and $2 million to buy new ambulances. Legislation passed in 2007 further authorized the use of $79 million for a public/private partnership between the District and Specialty Hospitals of America for the revitalization of Greater Southeast Community Hospital (though some of those funds are in the form of a loan). We provide recommendations for the allocation of the remaining funds, totaling approximately $135 million, which by legislation are limited to capital expenditures. ES.1 Recommendation Based on our analyses, we articulate (1) specific recommendations for the expenditure of tobacco settlement funds; (2) additional policies critical to the success of the capital investments; (3) complementary policies needed to improve ambulatory care; (4) recommendations relating to emergency medical services; and (5) recommendations regarding the allocation levels of capital investments. Recommendations for Investing Tobacco Settlement Funds (1) Use tobacco settlement funds to expand the capacity and improve the physical space of community health centers. 1 (1.1) Target expanding primary care capacity in community health centers (CHCs) by roughly 200,000 visits. (1.2) Invest in CHCs that expand capacity in high-need locations. (1.3) Invest in CHCs that establish and commit to maintaining urgent care capacity (including after-hours and weekend capacity) in at least two high-need locations. (1.4) Prioritize expansions to CHCs that would increase the availability of specialty care through plans for additional exam room space, investments in equipment to allow for specialty care services, and planned personnel arrangements with local hospitals. (1.5) To the extent possible, invest in expansions that leverage funding from other sources. (2) Use tobacco settlement funds to support greater adoption of health information technology. (2.1) Subsidize the adoption of electronic health records by hospitals and by providers who serve a substantial number of individuals who are enrolled in Medicaid or the Alliance or who are uninsured. (2.2) Invest in sustaining the regional health information organization (RHIO). (2.3) Consider investments in other promising health technologies. (3) Use tobacco settlement funds to invest in establishing an information clearinghouse for provider availability. 1 By community health center (CHC) we mean any ambulatory care facility that provides first contact, coordinated, comprehensive, continuous outpatient care for all regardless of their ability to pay. We do not restrict our definition of a CHC to federally qualified health centers or look-alikes. v (4) Use tobacco settlement funds for implementing and evaluating interventions and programs to improve the accessibility and quality of care; for planning and initial implementation of new data collection; and for additional evaluations of health and health care in the District. (5) Use tobacco settlement funds to pay for projects that move ambulatory health care facilities closer to evidence-based design. (6) Invest tobacco settlement funds in diversion reduction strategies including a collaborative and a “dashboard” with real-time information about diversion status and bed availability across hospitals. (7) Delay allocation of a portion of tobacco settlement until an assessment of needs for mental health and dental care is complete, and to pay for ongoing investments in health care service delivery improvement. Additional Policies to Ensure the Success of Capital Investments to Expand Capacity x Modify Medicaid and Alliance reimbursement for primary care and outpatient specialty care providers. x Enhance financial incentives for primary and specialty care providers who serve the underserved. x Ensure the availability and affordability of medical malpractice coverage for specialists serving Medicaid/Alliance enrollees and the uninsured. Complementary Policies for Improving Ambulatory Care x Focus private and public purchasers on purchasing quality health care. x Re-enfranchise District patients in the health care delivery system. x Promote health education and facilitate health care navigation. x Improve coordination of care between hospitals and physicians and between primary care and specialty care physicians. x Improve ongoing data collection and monitoring of health and health care in the District, including data on the health and health care of children. Recommendations for Improving Emergency Services x Develop a robust system to continuously assess the quality of emergency services. vi x Incentivize D.C. hospitals and D.C. FEMS to work together in a concerted effort to reduce hospital diversion and drop times.2 x Develop a system to track diversion and factors related to it. x Create a city-wide diversion policy. x Regionalize services to insure that patients are transported to hospitals that can meet their emergent needs. Recommendations for Funding Allocation Levels Table ES.1 below summarizes the recommended strategy for allocation of tobacco settlement funds. Table ES.1: Summary of Recommended Allocation Strategy Recommendation 1 Expenditure Expansion of primary and urgent care CHC capacity Electronic health record adoption, RHIO, other health information technologies Information clearinghouse Pilots, data collection, and evaluation Evidence-based design for ambulatory care ED collaborative and dashboard Reserve for additional investments, including mental health, oral health Total 2 3 4 5 6 7 Level of Funding (approximate, in millions)* $90 $24 $0.5 $8 $2.5 $2 $7.5 $135 *Figures are upper bounds where a range in the text is specified. ES.2 Gaps in Knowledge Substantial gaps exist in what we know about the health of District residents and their health care. Filling these gaps will better enable the District to determine whether and how to invest in additional components of care for District residents. Our recommendations include the allocation of funds to ongoing evaluation activities. In what follows, we summarize a number of gaps in knowledge that largely reflect gaps in the data available. x Little is known about children’s health status and access to care. 2 Diversion is when a hospital can only accept the sickest “priority 1” patients. Drop time is the amount of time it takes for EMS providers and hospital staff to transfer a patient from pre-hospital to hospital care. vii x Available information about insurance status among adults in the District is inadequate. x Little is known about the quality of emergency medical services in D.C. x Available data on mental health status and mental health and substance abuse service needs and use are extremely limited. x Provider supply could be measured with more precision if reliable data on practice time in the District and population served, by type of insurance, were available. x Differences in data formats and availability of Medicaid and Alliance data from managed care organizations make it less useful than it could be. x The lack of timely analysis of data with which to monitor the health of the District should be addressed. x We need clearer understanding about the role of private office-based providers in the delivery of care to Medicaid and Alliance enrollees and for the uninsured. ES.3 Conclusion The targeted infusion of tobacco settlement funds has the potential to improve considerably the robustness of the District’s health care system; and especially so if these investments are made in conjunction with auxiliary and complementary policies to increase the capacity, quality, and accessibility of health care services in the District, and activities to provide ongoing data and analysis to monitor progress. However, “fixing” the health care delivery system in the District cannot be accomplished with one-time policies or investments. Rather, the District needs to maintain a long-term vision for the future of the health of District residents, and commensurate with that, to devote resources to systematically tracking health and health care outcomes among residents on a consistent basis. That effort must begin with the new investments that will be made with tobacco settlement funds. It also bears repeating that the health of a population is the product of many factors. Our focus in this report on the health care delivery system is not meant to understate the importance of other factors on health outcomes. Systemic factors other than access to health care that give root to poor health outcomes in the city require additional, ongoing, and concentrated attention. These include the social environment (family structure, education, employment, crime), physical environment (air quality, water quality, access to healthy food, safe environments for physical activity), and the prosperity of District residents. viii