6 om as a public service of the RAND Corporation.
advertisement

THE ARTS
CHILD POLICY
This PDF document was made available from www.rand.org as a public
service of the RAND Corporation.
CIVIL JUSTICE
EDUCATION
ENERGY AND ENVIRONMENT
Jump down to document6
HEALTH AND HEALTH CARE
INTERNATIONAL AFFAIRS
NATIONAL SECURITY
POPULATION AND AGING
PUBLIC SAFETY
SCIENCE AND TECHNOLOGY
SUBSTANCE ABUSE
The RAND Corporation is a nonprofit research
organization providing objective analysis and effective
solutions that address the challenges facing the public
and private sectors around the world.
TERRORISM AND
HOMELAND SECURITY
TRANSPORTATION AND
INFRASTRUCTURE
WORKFORCE AND WORKPLACE
Support RAND
Browse Books & Publications
Make a charitable contribution
For More Information
Visit RAND at www.rand.org
Explore RAND Health
View document details
This product is part of the RAND Corporation reprint series. RAND
reprints reproduce previously published journal articles and book
chapters with the permission of the publisher. RAND reprints have
been formally reviewed in accordance with the publisher’s editorial
policy.
EVIDENCE REPORT AND
EVIDENCE-BASED
RECOMMENDATIONS
Chronic Disease Self
Management for Diabetes,
Osteoarthritis, Post-Myocardial
Infarction Care, and
Hypertension
Southern California
EvidenceEvidence-Based
Practice
Center
Santa
Santa Monica
Monica
Los
Los Angeles
Angeles
San
San Diego
Diego
PREPARED FOR:
U.S. Department of Health and Human Services
Centers for Medicare and Medicaid Services
7500 Security Blvd.
Baltimore, MD 21244-1850
PREPARED BY:
RAND
CONTRACT NUMBER:
500-98-0281
CONTRACT PERIOD:
September 30, 1998 to September 29, 2003
Project Staff
Principal Investigator
Paul Shekelle, MD, PhD
Project Manager
Margaret Maglione, MPP
Article Screening/Review
Josh Chodosh, MD, MSHS
Walter Mojica, MD, MPH
Senior Statistician
Sally C Morton, PhD
Senior Quantitative Analyst
Marika J Suttorp, MS
Senior Programmer/Analyst
Elizabeth A Roth, MA
Programmer
Lara Jungvig, BA
Staff Assistant/ Database Manager
Cost Analyst
Principal Investigator
Healthy Aging Project
Shannon Rhodes, MFA
Eileen McKinnon, BA
Shin-Yi Wu, PhD
Laurence Rubenstein, MD, MPH
CMS Project Officer
Pauline Lapin, MHS
i
TABLE OF CONTENTS
EXECUTIVE SUMMARY ..................................................................................... V
INTRODUCTION ...............................................................................................1
METHODS ......................................................................................................5
Conceptual Model ...................................................................................................... 5
Identification of Literature Sources .......................................................................... 9
Evaluation of Potential Evidence ............................................................................ 17
Extraction of Study-Level Variables and Results .................................................. 19
Statistical Methods................................................................................................... 28
Cost Effectiveness ................................................................................................... 36
Expert Review Process and Post-Hoc Analyses ................................................... 36
RESULTS .....................................................................................................42
Identification of Evidence........................................................................................ 42
Selection of Studies for the Meta-Analysis............................................................ 44
Results of the Meta-Analyses ................................................................................. 56
LIMITATIONS...............................................................................................115
CONCLUSIONS ............................................................................................117
RECOMMENDATIONS ...................................................................................119
REFERENCES CITED ...................................................................................120
APPENDIX A. EXPERT PANELIST ..................................................................155
APPENDIX B. ACCEPTED ARTICLES .............................................................156
APPENDIX C. REJECTED ARTICLES ..............................................................162
EVIDENCE TABLES......................................................................................186
ii
Figures and Tables
Figure 1. Conceptual Model ...................................................................................................................... 7
Figure 2. Screening Form........................................................................................................................ 18
Figure 3. Quality Review Form ............................................................................................................... 20
Figure 4. Flow of Evidence...................................................................................................................... 43
Figure 5. Article Flow of References from Boston Group .................................................................... 46
Figure 6. Forest Plot of Diabetes Studies: Hemoglobin A1c ............................................................... 58
Figure 7. Funnel Plot of Diabetes Studies: Hemoglobin A1c .............................................................. 58
Figure 8. Forest Plot of Diabetes Studies: Weight ............................................................................... 59
Figure 9. Funnel Plot of Diabetes Studies: Weight............................................................................... 59
Figure 10. Forest Plot of Diabetes Studies: Fasting Blood Glucose .................................................. 60
Figure 11. Funnel Plot of Diabetes Studies: Fasting Blood Glucose ................................................. 60
Figure 12. Forest Plot of Osteoarthritis Studies: Pain ......................................................................... 63
Figure 13. Funnel Plot of Osteoarthritis Studies: Pain ........................................................................ 63
Figure 14. Forest Plot of Osteoarthritis Studies: Functioning ............................................................ 64
Figure 15. Funnel Plot of Osteoarthritis Studies: Functioning ........................................................... 64
Figure 16. Forest Plot of Post-Myocardial Infarction Care Studies: Mortality ................................... 67
Figure 17. Funnel Plot of Post-Myocardial Infarction Care Studies: Mortality .................................. 67
Figure 18. Forest Plot of Post-Myocardial Infarction Care Studies: Return to Work........................ 68
Figure 19. Funnel Plot of Post-Myocardial Infarction Care Studies: Return to Work ....................... 68
Figure 20. Forest Plot of Hypertension Studies: Systolic Blood Pressure........................................ 71
Figure 21. Funnel Plot of Hypertension Studies: Systolic Blood Pressure ....................................... 71
Figure 22. Forest Plot of Hypertension Studies: Diastolic Blood Pressure....................................... 72
Figure 23. Funnel Plot of Hypertension Studies: Diastolic Blood Pressure...................................... 72
Figure 24. Forest Plot of Pooled Studies............................................................................................... 74
Figure 25. Funnel Plot of Pooled Studies .............................................................................................. 75
Figure 26. Regression of Intermediate 2 on Intermediate 1................................................................. 91
Figure 27. Regression of Outcome on Intermediate 2 ......................................................................... 92
iii
Table 1. Review Articles .......................................................................................................................... 12
Table 2. Articles Rejected from Meta-analysis...................................................................................... 47
Table 3. Diabetes articles Contributing to Meta-analysis .................................................................... 53
Table 4. Osteoarthritis Articles Contributing to Meta-analysis ........................................................... 54
Table 5. Post-Myocardial Infarction Care Articles Contributing to Meta-analysis ............................ 54
Table 6. Hypertension Articles Contributing to Meta-analysis............................................................ 55
Table 7. Publication Bias for Diabetes Studies..................................................................................... 61
Table 8. Publication Bias for Osteoarthritis Studies ............................................................................ 65
Table 9. Publication Bias for Post-Myocardial Infarction Care Studies ............................................. 69
Table 10. Publication Bias for Hypertension Studies...........................................................................73
Table 11. Meta-Analysis Results for Diabetes ...................................................................................... 76
Table 12. Meta-Analysis Results for Osteoarthritis.............................................................................. 77
Table 13. Meta-Analysis Results for Post-Myocardial Infarction Care ............................................... 78
Table 14. Meta-Analysis Results for Hypertension .............................................................................. 79
Table 15. Meta-Analysis Results Pooled Across Conditions .............................................................. 80
Table 16. Meta-Analysis Results for Diabetes (RE-AIM Model)............................................................ 82
Table 17. Meta-Analysis Results for Osteoarthritis (RE-AIM Model) ................................................... 83
Table 18. Meta-Analysis Results for Post-Myocardial Infarction Care (RE-AIM Model) .................... 84
Table 19. Meta-Analysis Results for Hypertension (RE-AIM Model).................................................... 85
Table 20. Meta-Analysis Results Pooled Across Conditions (RE-AIM Model) ................................... 86
Table 21. Meta-analysis Results for Diabetes (Severity Model) ........................................................... 88
Table 22. Meta-analysis Results for Osteoarthritis (Severity Model) .................................................. 88
Table 23. Meta-analysis Results Pooled Across Conditions (“Essential Elements” Model) ........... 89
iv
EXECUTIVE SUMMARY
Introduction
Chronic diseases currently affect well over one hundred million Americans. Though
chronic diseases are not immediately life threatening, they pose a significant threat to the health,
economic status and quality of life for individuals, families and communities.1, 2 The greatest
burden of chronic disease is concentrated in the 65-year and older age group. In 1995, 79% of
noninstitutionalized persons who were 70 years and older reported having at least one of seven
of the most common chronic conditions: arthritis, hypertension, heart disease, diabetes,
respiratory diseases, stroke, and cancer.1 Demographic trends portend alarming increases in the
next 20 years.
There is a growing enthusiasm for self-management programs, either as stand alone
program or as integral components of chronic care models, in controlling and preventing chronic
disease complications.3-7 Despite this enthusiasm, there is no agreed definition of what
constitutes a “chronic disease self-management program” nor is there agreement on which
elements of self management programs are most responsible for any beneficial effects.
We therefore sought to use empirical data from the literature to address the following
research questions posed by the Centers for Medicare and Medicaid Services (CMS).
1. Do these programs work?
2. Are there features that are generalizable across all diseases?
3. Does this intervention belong in the medical care system?
4. Define chronic disease self-management and distinguish between it and disease management.
5. What is the role or potential of technology?
v
6. What is the impact of chronic disease self-management programs on quality of life, health
status, health outcomes, satisfaction, pain, independence, and mental health (e.g., depression,
emotional problems)?
7. To what extent does self-management educate a patient on how to care for himself/herself
(e.g., take medications appropriately, consult with a physician when necessary, etc.)?
8. What is the patient’s retention of self-management skills after the intervention? Is a followup intervention needed at some point?
9. How does the approach for self-management differ for people with multiple chronic
diseases?
10. Is a generic self-management approach preferable to a disease-by-disease approach?
11. Should this intervention be targeted to a subset of the population or available to everyone?
Are there particular chronic conditions that should be addressed (e.g., diabetes, arthritis,
stroke, cancer, Parkinson’s, hypertension, dyslipidemia)?
12. What is the role of the physician? Can physicians be used to reinforce learning?
13. Cost effectiveness or cost savings—does the intervention appear to reduce health care costs
by reducing disease, physician office visits, hospitalizations, nursing home admissions, etc.?
14. Delivery mechanism: What do we know about whom (which provider type? trained lay
person?) should deliver this service? Do we know which care settings have proven effective
(e.g., physician’s office, senior center, other community or clinical settings)?
To address these questions, we focused on evaluating the effect of self-management
programs for the four chronic conditions most commonly studied in controlled trials of older
adults: osteoarthritis, diabetes mellitus, hypertension, and post myocardial infarction.
vi
Methods
Conceptual Model
In order to avoid the premature loss of potentially relevant studies, we broadly defined
"chronic disease self-management" as a systematic intervention that is targeted towards patients
with chronic disease to help them to actively participate in either or both of the following
activities: self-monitoring (of symptoms or of physiologic processes) or decision-making
(managing the disease or its impact based on self-monitoring). All interventions included in this
study attempt to modify patient behavior to reach specific goals of chronic disease selfmanagement.
We attempted to understand the characteristics particular to chronic disease selfmanagement programs that may be most responsible for their effectiveness. Based on the
literature and expert opinion, we postulated five hypotheses regarding effectiveness of chronic
disease self-management programs:
1
Patients who receive interventions tailored to their specific needs and circumstances are
likely to derive more benefit than those receiving interventions that are generic. (Tailored)
2
Patients are more likely to benefit from interventions received within a group setting that
includes others affected by the same condition than they are to benefit from an intervention
that was provided by other means. (Group Setting)
3
Patients who are engaged in a cycle of intervention followed by some form of individual
review with the provider of the intervention are more likely to derive benefit than from
interventions where no such review exists. (Feedback)
vii
4
Patients who engage in activities using a psychological intervention are more likely to derive
benefit than from interventions where there is no psychological emphasis. (Psychological)
5
Patients who receive interventions directly from their medical providers are more likely to
derive benefit than those who received interventions from non-medical providers. (Medical
Care)
Outcome measures
For the diabetes studies we used hemoglobin A1c, fasting blood glucose, and weight as
outcomes. For osteoarthritis, we used measures of pain and function. As would be expected, we
used systolic and diastolic blood pressure for hypertension. For post MI care, we used return to
work and mortality. For all conditions, we also collected intermediate outcomes such as
knowledge, feeling of self-efficacy, and health behaviors that are postulated to be related to
clinical outcomes. We separately assessed studies reporting costs.
Databases for Literature Search
To identify existing research and potentially relevant evidence for this report we searched
a variety of sources including the Cochrane Library (containing both a database of systematic
reviews and a controlled-trials register), the Assessment of Self-Care Manuals published by the
Oregon Health Sciences University (March 2000), and An Indexed Bibliography on SelfManagement for People with Chronic Disease 8 published by the Center for Advancement of
Health (CAH). In addition Medline, PsycInfo, and Nursing and Allied Health databases were
search.
Seventy-three other review articles on disease management were obtained; each review
discussed at least one intervention aimed at chronic disease self-management. We retrieved all
relevant documents referenced. We also contacted experts in the field and asked for any studies
viii
that were in press or undergoing review. Finally, we exchanged reference lists (but not analyses
or results) with a leading east coast university also performing a review of chronic disease selfmanagement programs, but not limited to older adults
Article Selection and Data Abstraction
Article selection, quality assessment, and data abstraction were done in standard fashion
by using two trained physician reviewers working independently; disagreements were resolved
by consensus or third-party adjudication.
Statistical Analyses
We answered many of the research questions through meta-analysis. We conducted
separate meta-analyses for each of the four medical conditions. We included all controlled trials
that assessed the effects of an intervention or interventions relative to either a group that received
usual care or a control group. The majority of our outcomes were continuous and we extracted
data to estimate effect sizes for these outcomes. For each pair of arms, an unbiased estimate9 of
Hedges’ g effect size10 and its standard deviation were calculated. A negative effect size
indicates that the intervention is associated with a decrease in the outcome at follow-up as
compared with the control or usual care group.
Because follow-up times across studies can lead to clinical heterogeneity, we excluded
from analysis any studies whose data were not collected within a specified follow-up interval
chosen based on clinical knowledge.
For each condition and outcome, we conducted the same analysis. We first estimated a
pooled random effects estimate11 of the treatment effect and a pooled effect size for continuous
outcomes across all studies and its associated 95% confidence interval. For each of the original
five hypotheses stated above, study arms either met the hypothesis (a “yes”) or did not (a “no”)
ix
and thus, no missing values exist. For each hypothesis, a simple stratified analysis would have
produced a pooled estimate of the treatment effect for all the “yes” study arms together, and a
pooled estimate for all the “no” study arms together. To facilitate testing the difference between
the two pooled estimates, we constructed these estimates using meta-regression in which the only
variables in the regression were a constant, and an indicator variable equal to one if the study
arm met the hypothesis and zero if the study arm did not. For some outcomes and hypotheses,
all study arms were either "yes" or "no." In this case, we could not fit a model.
As an overall test of the hypotheses, we combined the pain outcomes from osteoarthritis
studies, hemoglobin A1c outcomes from diabetes studies, and systolic blood pressure outcomes
from hypertension into one analysis using effect size and fit the five separate regressions as
above. We also fit a sixth regression that had a constant and all five-indicator variables for the
separate regressions included.
Sensitivity Analyses
Within each regression, and especially in the combined analysis, our primary analysis
ignored the fact that individual studies had multiple intervention arms and thus could contribute
more than one treatment effect to the analysis. The correlation between treatment effects within
the same study, due to the fact the each intervention arm was compared to the same control or
usual care arm, was ignored in this analysis. Our sensitivity analyses consisted of refitting the
meta-regression models using a two-level random effects model that contains a random effect at
the study level, as well as one at the arm level. This hierarchical approach controls for the
correlation within arms in the same study. None of these sensitivity analyses results differed
markedly from that of the primary analysis.
x
Post Hoc Analyses
We presented the results of the above analyses to a group of experts in chronic disease
self-management. Based on this presentation, members of this group suggested a series of
additional analyses exploring other possible mechanisms for an effect of self-management
programs. These included classifying the studies according to categories proposed in the REAIM Model,12 classifying the studies according to potential “essential elements” proposed by
this group,13 assessing whether the effectiveness of self-management programs varied by severity
of illness, and assessing whether interventions more likely to improve the “intermediate
variables,” such as knowledge and perception of self-efficacy, were more likely to improve
health outcomes
Results
Question 1. Do these programs work?
Question 2. Are there features that are generalizable across all diseases?
Question 6. What is the impact of chronic disease self-management programs on
quality of life, health status, health outcomes, satisfaction, pain, independence,
mental health (e.g., depression, emotional problems)?
Question 10. Is a generic self-management approach preferable to a disease-bydisease approach?
These questions are all related and were the focus of our meta-analysis. We first present
a disease-by-disease assessment of the evidence for efficacy, then our assessment of
generalizable or generic elements of a self-management program.
xi
Diabetes
There were 14 comparisons from 12 studies that reported hemoglobin A1c outcomes. In
an overall analysis of the effectiveness of chronic disease self-management programs, these
studies reported a statistically and clinically significant pooled effect size of -0.45 in favor of the
intervention (95% CI: (-0.26, -0.63)). The negative effect size indicates a lower hemoglobin A1c
in the treatment group as compared to the usual care or control group. An effect size of –0.45 is
equal to a reduction in hemoglobin A1c of about 1.0. For change in weight, there were 10
comparisons from 8 studies. There was no statistically significant difference between change in
weight in the intervention and control groups (effect size of -0.05; 95% CI:(-0.12, 0.23)). There
were 10 comparisons from 9 studies that reported fasting blood glucose outcomes. The pooled
effect size was -0.41 in favor of the intervention (95% CI: (-0.23, -0.60)). This effect size equates
to a drop in blood glucose of 1 mml/l.
Our assessment of publication bias revealed likely publication bias in studies reporting
hemoglobin A1c outcomes. Therefore, our results regarding efficacy of chronic disease selfmanagement programs for improving hemoglobin A1c must be interpreted with caution.
Osteoarthritis
For both pain and function outcomes there were 10 comparisons from 7 different studies.
The pooled results did not yield any statistically significant differences between intervention and
control groups (pooled effect sizes of -0.04 and -0.01 for pain and function respectively). Our
assessment of publication bias did not yield any evidence of publication bias.
Hypertension
For hypertension there were 23 comparisons from 14 studies that reported systolic and
diastolic blood pressure changes. The overall pooled result of the chronic disease self-
xii
management programs was a statistically and clinically significant reduction in systolic and
diastolic blood pressure (effect size for systolic blood pressure -0.32; 95% CI: (-0.50, -0.15);
effect size for diastolic blood pressure -0.59; 95% CI: (-0.81, -0.38)). An effect size of 0.32 is
equivalent to a change in blood pressure of 3.5 mm of mercury, the corresponding value for an
effect size of 0.59 is 6.5 mm of mercury. In our assessment of publication bias, there was
evidence of publication bias. Therefore our pooled result favoring chronic disease selfmanagement programs for hypertension must be viewed with caution.
Post Myocardial Infarction Care
There were 9 studies that reported mortality outcomes. There was no effect of chronic
disease self management programs on improving mortality (pooled relative risk 1.04; 95% CI:
(0.56, 1.95)). For return to work there were 10 comparisons from 8 studies. The pooled relative
risk did not show any difference between groups (relative risk 1.02; 95% CI: (0.97, 1.08)). Our
assessment of publication bias showed evidence of publication bias for the mortality outcome but
not the return to work outcome.
Tests of hypothesis of elements essential to chronic disease self-management efficacy
Other than an increased effectiveness seen in hypertension studies reporting systolic
blood pressure outcomes that used tailored interventions, there were no statistically significant
differences between interventions with or without the 5 features hypothesized to be related to
effectiveness (tailoring, use of group setting, feedback, psychological component, and medical
care). Indeed, many of the effects seen were inconsistent across outcomes within the same
condition. For example, in hypertension studies, for the hypothesis “use of a group setting,”
there was a greater than 50% increase in the effect size for improvement in systolic blood
xiii
pressure, but only a 5% increase in the effect size for improvement in diastolic blood pressure
(with neither result reaching statistical significance).
Our "across condition" analysis shows effect sizes that, in general, go in the direction of
supporting increased effectiveness associated with the use of these intervention features,
however none of the differences are statistically significant.
Post Hoc Analyses
Our “post hoc” tests of possible “essential elements” of chronic disease self-management
programs was unrevealing. The RE-AIM theory12 suggests that the following components: oneon-one counseling interventions (individual), group sessions (group), telephone calls (telephone),
interactive computer-mediated interventions (computer), mail interventions (mail) and health
system policies (policy 1 and policy 2) led to positive outcomes. With few exceptions, there
were no results that were statistically significant. An exception is the result for the use of oneon-one counseling sessions, which did show a statistically significant increased effect size when
used.
For the “Essential Elements of Self-management Interventions” evaluation, we did not
find as much variation among studies and components as is necessary for optimal power in the
analysis. Most of the studies scored positively for “problem identification and solving,” and did
not score positively for the “ensuring implementation component.” Given these data, we did not
find evidence to support either any one of these three broad “essential elements” as necessary,
nor some threshold (such as two out of three) in terms of efficacy. This was not an optimal test
of these hypotheses due to the lack of variation in the data.
xiv
Our analysis of the effect of self-management intervention on “intermediate variables”
such as knowledge and self-efficacy did not produce consistent results supporting an effect in the
expected direction.
Lastly, it was suggested we stratify by baseline patient severity. Only the assessment of
hemoglobin A1c demonstrated an increased effect size in patients who had higher (worse) value
of hemoglobin A1c at baseline, and this difference did not quite reach statistical significance.
Question 3. Does this intervention belong in the medical care system?
Whether chronic disease self-management belongs in the medical care system or in the
community is a decision that needs to be made by policy makers, based on many factors. One of
the first hypotheses we tested was whether patients who receive interventions directly from their
medical providers are more likely to have better outcomes than those who received interventions
from non-medical providers; no effect was found. Of the controlled studies that made it into our
meta-analysis, no studies of osteoarthritis or hypertension used medical providers in their selfmanagement interventions. Regarding diabetes, one intervention used medical providers; the
results of this intervention were not significantly different than those using lay leaders. One
post-myocardial infarction intervention used medical providers; the effects on mortality and
return to work were not statistically different from those of the other interventions.
Question 4. Define chronic disease self-management and distinguish between it
and disease management.
For purposes of this review, we initially defined chronic disease self-management
broadly as a systematic intervention that is targeted towards patients with chronic disease to help
them to actively participate in either or both of the following activities: self monitoring (of
xv
symptoms or physiologic processes) or decision-making (managing the disease or its impact
based on self-monitoring). Our analytic attempts to “define” chronic disease self-management
by identifying the components most responsible for the success of the program were
unsuccessful.
The draft evidence report was presented to a group of experts in chronic disease selfmanagement at a meeting convened by the Robert Wood Johnson Foundation on December 14,
2001. The panel’s aim was to focus on interventions offered to patients who need a more intense
level and type of self-management support. They agreed that all self-management programs
should address the following three areas.
Disease, medication and health management. While patients need medical information
about their particular disease (diabetes, arthritis, asthma, etc.), the majority of the content in most
successful self-management programs emphasized generic lifestyle issues such as exercise,
nutrition, and coping skills. More disease-specific medication-specific information can be useful,
but such information rarely constitutes more than 20 percent of the content of programs.
Role management. Patients benefit from programs that help them maintain social
support, connection to work and family, and normal functions of daily life.
Emotional management. Programs should encompass managing depression and stress,
adaptation to change, and maintaining interpersonal relationships.
A monograph authored by Dr. Jesse Gruman (Center for the Advancement of Health,
2002) summarized the discussions from this meeting. The experts concluded that the essential
elements of self-management programs should include the following:
xvi
1. Problem-solving training that encourages patients and providers to identify problems,
identify barriers and supports, generate solutions, form an individually tailored action
plan, monitor and assess progress toward goals, and adjust the action plan as needed.
2. Follow-up to maintain contact and continued problem-solving support, to identify
patients who are not doing well and assist them in modifying their plan, and to relate the
plan to the patient’s social/cultural environment.
3. Tracking and ensuring implementation by linking the program to the patient’s regular
source of medical care and by monitoring the effects of the program on the patient’s
health, satisfaction, quality of life, and health system quality measures.
The experts also recommended that any chronic disease self-management program be
composed of two tiers to accommodate the wide variety of patients with chronic conditions. The
first tier would include a low-intensity intervention designed to reach mass audiences and open
to anybody with a particular illness. The second tier would include a high-intensity intervention
targeted to people who require one-on-one support and case management. This program could
be offered to those who have not successfully managed their condition with the minimal support
of tier #1, those who have complicated conditions, and those whose life circumstances or
conditions change significantly.
Question 5. What is the role or potential of technology?
The advent of new technologies makes communication between patients, providers, and
others more convenient than ever. However, none of the randomized controlled studies on
chronic disease self-management for our study conditions in older patients used email or the
Internet. Thus, we were not able to quantitatively assess the impact of these technologies. A
xvii
recently reported study of back pain in middle aged adults reported modest improvements in
outcomes and costs for subjects randomized to a physician-moderated “email discussion group”
and educational material compared to a control group that received a magazine subscription. This
study suggests that incorporating these technologies into future randomized studies would be a
worthwhile endeavor.
Question 7. To what extent does self-management educate a patient on how to
care for himself/herself (e.g., take medications appropriately, consult with a
physician when necessary, etc.)?
Most CDSM studies that assess knowledge and self-efficacy reported beneficial
improvements. Most studies did NOT measure whether medications were taken appropriately or
“necessary” physician visits were made. The two studies that did assess compliance were
hypertension studies. One had a borderline beneficial overall result; the other reported a
significant beneficial result. One study was based on a conceptual model that specifically
considered that changing medication-taking behavior was going to be easier than changing diet
behavior or other such behaviors. This study did not actually measure compliance, but rather
measured “commitment to taking medications” and showed that this differed between
intervention and controls and that it was one of only three variables among those tested to be
associated with significant changes in blood pressure (the other two were “”belief in severity of
the disease” and “beliefs in efficacy of therapy”). Many studies assessed utilization, but none
assessed whether the utilization was necessary.
xviii
Question 8. What is the patient’s retention of self-management skills after the
intervention? Is a follow-up intervention needed at some point?
We were unable to find studies that actually included a “follow-up intervention” which
incorporated refresher skills on self-management. In light of this, we used a meta-regression
model to test whether self-management interventions that provide follow-up support led to better
results than those that did not. We classified interventions that maintained contact with the
patient through contracts, provider feedback, reminders, peer support, material incentives, or
home visits as including “follow-up support.” Of the interventions which could be included in
our meta-analyses, 19 had “follow-up support” while 28 did not. Pooled results were not
statistically different between the two groups.
Question 9. How does the approach for self-management differ for people with
multiple chronic diseases?
We found no evidence on this topic.
Question 11. Should this intervention be targeted to a subset of the population or
available to everyone? Are there particular chronic conditions that should be
addressed (e.g., diabetes, arthritis, stroke, cancer, Parkinson’s, hypertension,
dyslipidemia)?
We were able to quantitatively assess the effects of chronic disease self-management
programs on patients with diabetes, osteoarthritis, and hypertension. In addition, we were able to
pool results for post myocardial infarction programs. There were insufficient studies on stroke,
cancer, Parkinson’s and dyslipedemia to allow pooling.
xix
In an attempt to assess whether chronic disease self-management programs were more
effective for more severe patients, we undertook a post-hoc quantitative analysis. Two clinicians
independently categorized each diabetes and osteoarthritis program as focusing on either more
severe or less severe patients. The clinicians were unable to categorize the hypertension and
post- MI programs in such a fashion, due to the lack of heterogeneity of the patients. In the
diabetes analysis, there was no statistical difference between the effectiveness of programs
targeted to more severe and less severe patients, in terms of change in hemoglobin A1c or
weight. For osteoarthritis studies, there was no statistical difference in change in pain or
functioning.
Question 12. What is the role of the physician? Can physicians be used to
reinforce learning?
Out meta-analysis did not reveal any statistically significant differences supporting the
role of physicians at enhancing the efficacy of chronic disease self-management programs.
Question 13. Cost effectiveness or cost savings—does the intervention appear to
reduce health care costs by reducing disease, physician office visits,
hospitalizations, nursing home admissions, etc.?
A total of 19 clinical trial studies were identified in this review of the economic impact of
Chronic Disease Self-Management (CDSM). These include 9 studies on diabetes, 4 studies on
osteoarthritis, one study on hypertension, two on post-myocardial infarction, and three nondisease-specific programs for chronically ill patients. They represented only a subset of possible
strategies for CDSM. Thus our economic review has limited generalizability beyond the studied
interventions.
xx
Costs of the intervention were rarely reported and health care costs as an outcome of the
intervention were rarely studied. Changes in health care utilization were seldom reported, and in
many cases only studied on a limited scale (not including all types of services). The follow-up
period was short, while many outcomes will not be evident for many years (e.g., rigid metabolic
control may result in delay or prevention of diabetic complications, but only after several years).
Among the four diseases reviewed, the programs to promote self-management with
osteoarthritis patients have the best economic information and most consistently report
reductions in health care utilization and costs, even to the point of cost-savings. Such findings
are compatible with observational studies.14-16 Programs for diabetic patients have mixed results,
and overall are weaker in the economic information they report. There is only one hypertension
program identified that include any economic information, and the information provided does
not allow us to adequately judge cost-effectiveness of the program. The two reviewed MI studies
both lacked a rigorous collection of economic data, but the limited evidence presented suggests
that home-based rehabilitation programs could potentially be a cost-effective alternative to group
rehabilitation or standard care. As for the three general, non-disease-specific programs, two
RCTs and two observational studies reported that low-cost, community-based CDSM programs
may potentially be cost-saving.
Limitations
Despite finding evidence that CDSM programs have a clinically and statistically
significant beneficial effect on some outcomes, we were unable to discern which elements of
CDSM programs are most associated with success. This may have been because we did not test
the right hypotheses regarding CDSM elements, or because key variables describing these
components were either not recorded adequately or not recorded at all in the published articles,
xxi
or that the individual components themselves each have relatively weak effects. We considered
contacting original authors for additional information regarding their interventions, but rejected
this due to time and resource constraints. Furthermore, our experience has been that any study
published more than a few years ago has a much lower likelihood for getting a favorable
response to such a request. In addition, we may have lacked the statistical power, due to the
small number of studies available, to discern the reasons for the relatively small amount of
heterogeneity in the study results. We note that the preceding challenges are common to all
studies of complex, multicomponent interventions, and these challenges did not prevent us from
detecting important differences in the effectiveness of interventions for prevention of falls17 or
increasing the use of cancer screening and immunizations.18
An additional primary limitation of this systematic review, common to all such reviews,
is the quantity and quality of the original studies. We made no attempt to give greater
importance to some studies based on "quality." The only validated assessment of study quality
includes criteria not possible in self-management (double-blinding). As there is a lack of
empirical evidence regarding other study characteristics and their relationship to bias, we did not
attempt to use other criteria.
As previously discussed, we did find evidence of publication bias in hemoglobin A1c,
mortality, and systolic and diastolic blood pressure outcomes in diabetes, post-myocardial
infarction care, and hypertension, respectively. Therefore, the beneficial results that we report in
our pooled analysis need to be considered in light of the possible existence of unpublished
studies reporting no benefit.
xxii
Conclusions
1. Chronic disease self-management programs probably have a beneficial effect on some, but
not all, physiologic outcomes. In particular, we found evidence of a statistically significant
and clinically important benefit on measures of blood glucose control and blood pressure
reduction for chronic disease self management programs for patients with diabetes and
hypertension, respectively. Our conclusions are tempered by our finding of possible
publication bias, favoring beneficial studies, in these two clinical areas. These was no
evidence of a beneficial effect on other physiologic outcomes such as pain, function, weight
loss, and return to work.
2. There is not enough evidence to support any of the proposed elements as being essential to
the efficacy of chronic disease self-management programs. More research is needed to try
and establish the optimum design of a chronic disease self-management program, and
whether or not this differs substantially depending on the particular chronic disease or
characteristics of the patient.
3. While no randomized studies of chronic disease self-management programs for older adults
assessed the use of email or the Internet, one recently reported randomized study of email use
in the self-management of middle aged adults with back pain was sufficiently promising to
warrant testing such interventions for chronic disease self-management in the Medicare
population.
4. There is no evidence to conclusively support or refute the role of physician providers in
chronic disease self-management programs for older adults.
5. The evidence is inconclusive but suggests that chronic disease self-management programs
may reduce health care use.
xxiii
INTRODUCTION
Chronic diseases are conditions that are usually incurable. Although often not
immediately life threatening, they pose significant burdens on the health, economic status, and
quality of life for individuals, families, and communities.1 In 1995, seventy-nine percent of
noninstitutionalized persons who were 70 years or older reported having at least one of seven of
the most common chronic conditions affecting this age group: arthritis, hypertension, heart
disease, diabetes, respiratory diseases, stroke, and cancer.1
Of these seven conditions, arthritis is most prevalent, affecting more than 47 percent of
individuals 65 years and older.19 Hypertension affects 41 percent of this population while 31
percent have some form of heart disease, of which ischemic heart disease and a history of
myocardial infarction are major components. Diabetes affects approximately 10% of persons 65
years and older and increases the risk for other chronic conditions, including ischemic heart
disease, renal disease, and visual impairment.19
Life-altering disability is a frequent consequence of chronic disease. Of the seven
conditions listed above, arthritis is the leading cause of disability.2 In 1995, 11 percent of
noninstitutionalized persons who were 70 years or older reported arthritis as a cause of limitation
in their activities of daily living. Heart disease was reported by four percent, while 1.5 percent
reported diabetes as a cause of functional limitation.2
The proportion of Americans who are 65 years or older is rising steadily. In 1997,
thirteen out of every 100 Americans were 65 years or older. Demographers predict this
proportion will increase to 20 out of 100 by the year 2030, or approximately 70 million people.
1
Within this age-group, 8.5 million people will be over 85 years old, more than double the 1997
estimates.20
Given these demographic projections, the prevalence of chronic disease and its related
costs will also increase dramatically. Therapies for conditions such as osteoarthritis, heart
disease, and diabetes have improved considerably over the past 20 years. For example, evidence
suggests that exercise programs improve symptoms and reduce disability in individuals with
osteoarthritis;21 modest blood pressure control reduces the incidence of myocardial infarction
and stroke;22 and improved control of blood glucose significantly reduces the incidence of
diabetes, complications including neuropathy, renal disease, and blindness.23, 24
There is a growing conviction that self-management will be an important component of
controlling and preventing illness complications. Studies of condition-specific self-management
interventions have been used to evaluate the benefits of particular interventions. However, one
difficulty in drawing conclusions from this literature is that the interventions being evaluated
often consist of more than one component, making it difficult to identify what caused the
intervention as a whole to succeed or fail.
This evidence report was commissioned by the Centers for Medicare and Medicaid
Services (CMS) to examine the evidence regarding the effectiveness of chronic disease selfmanagement programs and to assess which components may be most crucial to success. More
specifically, this report reviews evidence from controlled trials of chronic disease selfmanagement programs for four of the most common conditions of older adults: diabetes,
osteoarthritis; post-myocardial infarction care; and hypertension. Our charge was to report the
evidence regarding the following key questions specified by CMS:
2
1. Do these programs work?
2. Are there features that are generalizable across all diseases?
3. Does this intervention belong in the medical care system?
4. Define chronic disease self-management and distinguish between it and disease
management.
5. What is the role or potential of technology?
6. What is the impact of chronic disease self-management programs on quality of life,
health status, health outcomes, satisfaction, pain, independence, mental health (e.g.,
depression, emotional problems)?
7. To what extent does self-management educate a patient on how to care for
himself/herself (e.g., take medications appropriately, consult with a physician when
necessary, etc.)?
8. What is the patient’s retention of self-management skills after the intervention? Is a
follow-up intervention needed at some point?
9. How does the approach for self-management differ for people with multiple chronic
diseases?
10. Is a generic self-management approach preferable to a disease-by-disease approach?
11. Should this intervention be targeted to a subset of the population or available to
everyone? Are there particular chronic conditions that should be addressed (e.g.,
diabetes, arthritis, stroke, cancer, Parkinson’s, hypertension, dyslipidemia)?
12. What is the role of the physician? Can physicians be used to reinforce learning?
3
13. Cost effectiveness or cost savings—does the intervention appear to reduce health care
costs by reducing disease, physician office visits, hospitalizations, nursing home
admissions, etc.?
14. Delivery mechanism: What do we know about whom (which provider type? trained
lay person?) should deliver this service? Do we know which care settings have
proven effective (e.g., physician’s office, senior center, other community or clinical
settings)?
4
METHODS
We synthesize evidence from the scientific literature on effectiveness of chronic disease
self-management programs, using the evidence review and synthesis methods of the Southern
California Evidence-Based Practice Center, an Agency for Healthcare Research and Quality—a
designated center for the systematic review of literature on the evidence for benefits and harms
of health care interventions. Our literature review process consisted of the following steps:
x Develop a conceptual model (also sometimes called an evidence model or a causal
pathway).
x Identify sources of evidence (in this case, sources of scientific literature).
x Identify potential evidence.
x Evaluate potential evidence for methodological quality and relevance.
x Extract study-level variables and results from studies meeting methodological and
clinical criteria.
x Synthesize the results.
CONCEPTUAL MODEL
These is no standard definition of what constitutes a chronic disease self-management
program. Indeed, the second key question we were assigned seeks to define essential
components empirically. Still, we needed to start with some initial definition in order to target
our literature search. Therefore, for this review, we defined "chronic disease self-management"
broadly as a systematic intervention that is targeted towards patients with chronic disease to help
them actively participate in either or both of the following activities: self monitoring (of
5
symptoms or of physiologic processes) or decision-making (managing the disease or its impact
based on self-monitoring).
Figure 1 represents a simple conceptual model of how self-management influences
patient outcomes. Patient behavior describes all that patients do to self-manage their chronic
diseases. All interventions included in this study attempt to modify patient behavior to reach
specific goals of chronic disease self-management.
Traditional behavior-change intervention components
Education. Educational efforts can be directed toward an individual, group, or entire
community. Pamphlets and posters can raise awareness among older adults or staff members at
senior centers and nursing homes. More intense educational interventions include one-on-one
counseling.
Psychological. Psychological efforts include counseling, cognitive-behavioral therapy,
relaxation training, and emotional support groups.
Feedback & Incentives include clinical reviews with patients, contracts, provider
feedback, reminders, diaries, goal setting instruction, and material/ financial incentives.
Intervention components aimed at particular physiologic targets include:
Physical Activity includes non-physiotherapy activity, for example walking, cycling, and
aerobic movements. P.A. also includes training geared specifically towards balance, strength, or
gait, for example tai chi or tailored physical therapy.
Medical and Related Interventions include interventions such as medication therapy,
blood pressure monitoring, and dietary monitoring.
6
Figure 1. Conceptual Model
7UDGLWLRQDO%HKDYLRU&KDQJH
&RPSRQHQWV
(GXFDWLRQ
3V\FKRORJLFDO
)HHGEDFN,QFHQWLYHV
+\SRWKHVHV5HJDUGLQJ&'60
,QWHUYHQWLRQV
7DLORUHG,QWHUYHQWLRQV
8VHRI*URXS6HWWLQJ
)HHGEDFNWR3DWLHQWV
3V\FKRORJLFDO&RPSRQHQW
0'&DUH
7KHUDSHXWLF,QWHUYHQWLRQ
&RPSRQHQWV
3K\VLFDO$FWLYLW\
0HGLFDODQG5HODWHG,QWHUYHQWLRQV
Intervention
Patient
Characteristics
Patient Behavior
Chronic Disease
Self-Management
Chronic Disease
Clinical Outcomes
7
Clinical Practice
Interventions may be modified to account for specific patient characteristics, which result
in individualized intervention programs. In this way, the relevance of interventions is enhanced
and patients have greater opportunity to be more personally engaged than with generalized
programs. Programs that utilize intervention components such as group programs, feedback, or
psychological approaches may have greater impact than those programs lacking such
components. Programs using approaches more likely to be engaging may therefore enhance the
level of patient commitment and effort. These programs are also likely to provide more
opportunity for emotional support, both formally and informally, which may address a critical
need of patients who struggle with chronic disease conditions. Interventions that work within the
context of a clinical practice or are delivered by physicians who are otherwise engaged in the
study participants’ care may be more relevant and require potentially a greater investment on the
part of patients, resulting in increased likelihood of behavior change.
Hypotheses
Of key importance to both CMS and providers is what the essential elements of chronic
disease self-management programs seem to be. In this analysis, we attempt to understand the
characteristics particular to chronic disease self-management programs that may be most
responsible for their effectiveness. This analysis was undertaken to help answer CMS’s
secondary question, “Are there features that are generalizable across all diseases?” We
developed five hypotheses regarding effectiveness (terms in parentheses relate to terms used in
evidence tables). These five hypotheses operate on the areas indicated in the conceptual model
with the corresponding number.
8
1. Patients who receive interventions tailored to their specific needs and circumstances
are likely to derive more benefit than those receiving interventions that are generic.
(Tailored)
2. Patients are more likely to benefit from interventions received within a group setting
that includes others affected by the same condition than they are to benefit from an
intervention that was provided by other means. (Group Setting)
3. Patients whose intervention is followed by some form of individual review with the
provider of the intervention are more likely to derive benefit than patients whose
interventions involve no such review. (Feedback)
4. Patients are more likely to derive benefit from activities that use a psychological
intervention than from interventions where there is no psychological emphasis.
(Psychological)
5. Patients who receive interventions directly from their medical providers are more
likely to derive benefit than those who received interventions from non-medical
providers. (MD Care)
IDENTIFICATION OF LITERATURE SOURCES
We used the sources described below to identify existing research and potentially
relevant evidence for this report. We searched each source for articles specific to the four
conditions of interest: diabetes, osteoarthritis, myocardial infarction, hypertension. We chose
these conditions because each had a significant quantity of published literature and each is highly
prevalent in older adults. (Because of these criteria we did not search for literature on conditions
9
with an extensive body of chronic disease self-management literature, such as rheumatoid
arthritis or asthma, as both of these are of low frequency in older adults.)
Cochrane Collaboration
The Cochrane Collaboration is an international organization that helps people make wellinformed decisions about health care by preparing, maintaining, and promoting the accessibility
of systematic reviews on the effects of heath-care interventions. The Cochrane Library contains
both a database of systematic reviews and a controlled-trials registry. The library receives
additional material continually to ensure that reviews are maintained and updated through
identification and incorporation of new evidence. The Cochrane Library is available on CDROM by subscription. The Cochrane Library contained 15 reports on chronic disease selfmanagement; we obtained all studies referenced therein.
Oregon Health Sciences University
The Evidence-based Practice Center (EPC) at the Oregon Health Sciences University
published the Assessment of Self-Care Manuals in March 2000. The Oregon EPC systematically
searched the scientific literature for evidence that self-care manuals produce changes in a variety
of outcomes for health care consumers. We scanned the reference list and ordered relevant
articles.
In addition, the Oregon EPC sent a brief description of the preliminary review process for
a projected titled “Diabetes Self-Management Programs: Medical Guidelines and Patient SelfMonitoring.” This document included abstracts on over 20 studies and a list of 13 review articles
on diabetes self-management. We ordered all relevant publications.
10
Center for Advancement of Health
The Center for Advancement of Health (CAH) in association with the Group Health
Cooperative of Puget Sound, recently published An Indexed Bibliography on Self-Management
for People with Chronic Disease. The role of the Center is to promote widespread acceptance
and application of an expanded view of health that recognizes psychological and behavioral
factors. The bibliography contained abstracts from over 400 journal articles, from 1980 to the
present, covering 18 chronic diseases and conditions. We ordered all relevant publications.
Library Search
In addition to obtaining references and materials from the above sources we conducted a
library search for all studies published (subsequent to) the CAH bibliography,8 using the search
terms listed below.
Medline, PsycInfo and Nursing and Allied Health databases were the primary sources of
citation information. Searches covered 1980 to 1995, although relevant articles from earlier
dates were included. The major search strategy consisted of keyword searches using a
combination of descriptors to focus the search on pertinent topical areas. Terms representing
each of the chronic diseases included in the bibliography were combined with a set of other
keyword terms that were likely to identify the types of articles that met inclusion criteria. The
following diseases were searched: Arthritis, Chronic Illness, Diabetes, Heart Disease, and
Hypertension. Keywords used in combination with disease names included Anxiety, Behavior,
Compliance, Coping , Depression , Disability, Exercise, Family, Isolation, Modeling, Nutrition,
Patient Education, Patient Satisfaction, Problem-Solving, Relaxation, Self-care ,and Social
Support.
11
Related topics of interest were also searched by keyword, such as interactive video,
computer interventions, telephone intervention, media, practice redesign, case management,
patient provider interaction and illness model. Articles covering a number of different illnesses
or behaviors were sometimes identified by one particular keyword in a database. For instance,
many types of pertinent self-care behaviors would be included within the keyword “compliance,”
but not all articles retrieved under “compliance” would be relevant to chronic illness. Thus of
articles retrieved with such a search were reviewed for the subset of articles pertinent to chronic
illness management.
Previous Systematic Reviews
Sources using the aforementioned, we identified 73 previously completed reviews
relevant to this project (see Table 1). Each review discusses at least one intervention aimed at
chronic disease self-management. We retrieved all relevant documents referenced in these
publications.
Table 1. Review Articles
Review: Self-management education for adults with asthma improves health outcomes. EvidenceBased Medicine. 1999;4:15. Rec #: 740
ACP Journal Club. Review: Several interventions reduce complications in type 2 diabetes mellitus.
ACP J Club. 1998;128:30. Rec #: 2577
Anderson BJ, Auslander WF. Research on diabetes management and the family: A critique. Diabetes
Care. 1980;3:696-702. Rec #: 2220
Assal JP, Muhlauser I, Pernot A, Gfeller R, Jorgens V, Berger M. Patient education as the basis for
diabetes care in clinical practice and research. Diabetologia. 1985;28:602-613. Rec #: 2104
Blumenthal J A, Thyrum E T, Gullette E D, Sherwood A, Waugh R . Do exercise and weight loss
reduce blood pressure in patients with mild hypertension? N C Med J. 1995;56(2):92-5. Rec #:
753
Broderick J E. Mind-body medicine in rheumatological disease. Rheumatic Disease Clinics of North
America. 1999. Rec #: 609
Brown S A . Meta-analysis of diabetes patient education research: variations in intervention effects
across studies. Res Nurs Health. 1992;15(6):409-19. Rec #: 759
Brown S A . Studies of educational interventions and outcomes in diabetic adults: a meta-analysis
revisited. Patient Educ Couns. 1990;16(3):189-215. Rec #: 760
12
Table 1. Review Articles
Brown SA. Effects of educational interventions in diabetes care: a meta-analysis of findings. Nurs Res.
1988;37:223-230. Rec #: 2090
Brownell KD, Kramer FM. Behavioral management of obesity. Medical Clinics of North America.
1989;73:185-201. Rec #: 2642
Cassem NH, Hacket TP. Psychological rehabilitation of myocardial infarction patients in the acute
phase. Heart Lung. 1973;2:382-38. Rec #: 2409
Clark N M . Asthma self-management education. Research and implications for clinical practice.
Chest. 1989;95(5):1110-3. Rec #: 763
Clark N M, Becker M H, Janz N K, Lorig K, Rakowski W, Anderson L. Self-management of chronic
disease by older adults: A review and questions for research. J Aging Health. 1991;3:3-27.
Rec #: 904
Clark NM, Evans D, Zimmerman BJ, Levison MJ, Mellins RB . Patient and family management of
asthma: theory-based techniques for the clinician. J Asthma. 1994;31(6):427-35. Rec #: 764
Clement S . Diabetes self-management education. Diabetes Care. 1995;18(8):1204-14. Rec #: 769
Cox DJ, Gonder-Frederick L. Major developments in behavioral diabetes research. Journal of
Consulting and Clinical Psychology. 1992;60(4):628-638. Rec #: 2441
Dubbert PM, Rappaport NB, Martin JE. Exercise in cardiovascular disease. Behavior Modification.
1987;11:329-347. Rec #: 2643
Dunn S M . Rethinking the models and modes of diabetes education. Patient Educ Couns.
1990;16(3):281-6. Rec #: 778
Epstein LH, Cluss PA. A Behavioral Medicine perspective on adherence to long-term medical
regimens. Journal of Consulting and Clinical Psychology. 1988;6:77-87. Rec #: 2238
Fawzy F I, Fawzy N W, Arndt L A, Pasnau R O . Critical review of psychosocial interventions in cancer
care. Arch Gen Psychiatry. 1995;52(2):100-13. Rec #: 786
Freemantle N, Harvey EL, Wolf F, et al. Printed educational materials to improve the behavior of health
care professionals and patient outcomes. In: Cochrane Database of Systematic Reviews,
Issue 3, 1998. Rec #: 2618
Giloth B E . Promoting patient involvement: educational, organizational, and environmental strategies.
Patient Educ Couns. 1990;15(1):29-38. Rec #: 796
Glanz K. Patient and public education for cholesterol reduction: A review of strategies and issues.
Patient Education and Counseling. 1988;12:235-257. Rec #: 2644
Glasgow R E, Toobert D J, Hampson S E, Wilson W. Behavioral research on diabetes at the Oregon
Research Institute. Ann Behav Med. 1995;17:32-40. Rec #: 905
Glasgow RE, Osteen VL. Evaluating diabetes education: Are we measuring the most important
outcome? Diabetes Care. 1992;15:1423-1432. Rec #: 2177
Goodall T A, Halford W K . Self-management of diabetes mellitus: A critical review [published erratum
appears in Health Psychol 1992;11(1):77]. Health Psychol. 1991;10(1):1-8. Rec #: 802
Griffin S, Kinmonth AL. Diabetes care: the effectiveness of systems for routine surveillance for people
with diabetes (Cochrane Review). In: The Cochrane Library, Issue 4, 1998. Oxford: Update
Software. Rec #: 2620
Hackett TP. The use of groups in the rehabilitation of the postcoronary patient. Adv Cardiol.
1978;24:127-135. Rec #: 2411
Haynes RB, McKibbon KA, Kanani R, et al. Interventions to assist patients to follow prescriptions for
medications (Cochrane Review). In: The Cochrane Library, Issue 4, 1998. Oxford: Update
Software. Rec #: 2621
13
Table 1. Review Articles
Hill D R, Kelleher K, Shumaker S A . Psychosocial interventions in adult patients with coronary heart
disease and cancer. A literature review. Gen Hosp Psychiatry. 1992;14(6 Suppl):28S-42S.
Rec #: 811
Hirano P C, Laurent D D, Lorig K . Arthritis patient education studies, 1987-1991: a review of the
literature [see comments]. Patient Educ Couns. 1994;24(1):9-54. Rec #: 813
Jacob RG, Wing R, Shapiro AP. The behavioral treatment of hypertension: long-term effects. Behav
Therapy. 1987;18:325-352. Rec #: 2471
Jacobson AM, Leibovich JB. Psychological issues in diabetes mellitus. Psychosomatic Illness Review.
1984;25:7-13. Rec #: 2255
Johnston DW. Behavioral treatment in the reduction of coronary risk factors Type A behavior and blood
pressure. Br J Clin Psychol. 1982;21:281-294. Rec #: 2364
Johnston DW. Stress managements in the treatment of mild primary hypertension. Hypertension.
1991;17(Suppl 3):63-68. Rec #: 2470
Kaplan RM, Davis WK. Evaluating costs and benefits of outpatients diabetes education and nutrition
counseling. Diabetes Care. 1986;9:81-86. Rec #: 2379
Kaplan S H, Greenfield S, Ware J E. Assessing the effects of physician-patient interactions on the
outcomes of chronic disease [published erratum appears in Med Care 1989 Jul;27(7):679].
Med Care. 1989;27(3 Suppl):S110-27. Rec #: 820
Keefe F J, Dunsmore J, Burnett R . Behavioral and cognitive-behavioral approaches to chronic pain:
recent advances and future directions. J Consult Clin Psychol. 1992;60(4):528-36. Rec #: 822
Keefe FJ, Gil KM, Rose SC. Behavioral approaches in the multidisciplinary management of chronic
pain: Programs and issues. Clinical Psychology Review. 1986;6:87-113. Rec #: 2292
Keefe FJ, Williams DA. New Directions in pain assessment and treatment. Clinical Psychology
Review. 1989;9:549-568. Rec #: 2293
Kemper D W, Lorig K, Mettler M . The effectiveness of medical self-care interventions: a focus on selfinitiated responses to symptoms. Patient Educ Couns. 1993;21(1-2):29-39. Rec #: 823
Linden W, Chambers L. Clinical effectiveness of non-drug treatment for hypertension: A meta-analysis.
Ann Behav Med. 1994;16:35-45. Rec #: 910
Lorig K. Self-management of chronic illness: A model for the future. Generations. 1993:11-14. Rec #:
911
Lorig K, Holman H . Arthritis self-management studies: a twelve-year review. Health Educ Q.
1993;20(1):17-28. Rec #: 831
Lorig K, Laurin J . Some notions about assumptions underlying health education. Health Educ Q.
1985;12(3):231-43. Rec #: 834
Mazzuca S A . Does patient education in chronic disease have therapeutic value? J Chronic Dis.
1982;35(7):521-9. Rec #: 843
Mazzuca S A . Education and behavioral and social research in rheumatology. Curr Opin Rheumatol.
1994;6(2):147-52. Rec #: 844
Meyer T J, Mark M M . Effects of psychosocial interventions with adult cancer patients: a meta-analysis
of randomized experiments [see comments]. Health Psychol. 1995;14(2):101-8. Rec #: 848
Mullen P D, Laville E A, Biddle A K, Lorig K . Efficacy of psychoeducational interventions on pain,
depression, and disability in people with arthritis: a meta-analysis. J Rheumatol. 1987;14
Suppl 15:33-9. Rec #: 850
Mullen PD, Green LW, Persinger GS. Clinical trials of patient education for chronic conditions: a
comparative meta-analysis of intervention types. Prev Med. 1985;14:753-781. Rec #: 2350
14
Table 1. Review Articles
Mumford E, Schlesinger H J, Glass G V . The effect of psychological intervention on recovery from
surgery and heart attacks: an analysis of the literature. Am J Public Health. 1982;72(2):14151. Rec #: 852
Norris SL, Engelgau MM, Narayan KMV. Effectiveness of self-management training in Type 2
Diabetes. Diabetes Care. 2001;24:561-587.
Nunes E V, Frank K A, Kornfeld D S . Psychologic treatment for the type A behavior pattern and for
coronary heart disease: a meta-analysis of the literature. Psychosom Med. 1987;49(2):15973. Rec #: 854
O'Connor GT, Collins R, Burning JE et al. Rehabilitation with exercise after myocardial infarction.
Circulation. 1989;80(2):234-244. Rec #: 2692
Padgett D, Mumford E, Hynes M, Carter R . Meta-analysis of the effects of educational and
psychosocial interventions on management of diabetes mellitus. J Clin Epidemiol.
1988;41(10):1007-30. Rec #: 857
Razin A M . Psychosocial intervention in coronary artery disease: a review. Psychosom Med.
1982;44(4):363-87. Rec #: 864
Rosenstock IM. Understanding and enhancing patient compliance with diabetic regimens. Diabetes
Care. 1985;8:610-616. Rec #: 2268
Rosenstock J, Raskin P. Diabetes and its complications: Blood glucose control vs. genetic
susceptibility. Diabetes/Metabolism Reviews. 1988;4:417-435. Rec #: 2269
Schlundt DG, McDonel EC, Langford HG. Compliance in dietary management of hypertension.
Comprehensive Therapy. 1985;11:59-66. Rec #: 2645
Sobel D S . Rethinking medicine: improving health outcomes with cost-effective psychosocial
interventions. Psychosom Med. 1995;57(3):234-44. Rec #: 876
Spiegel D . Health caring. Psychosocial support for patients with cancer. Cancer. 1994;74(4
Suppl):1453-7. Rec #: 878
Strecher V J, DeVellis B M, Becker M H, Rosenstock I M . The role of self-efficacy in achieving health
behavior change. Health Educ Q. 1986;13(1):73-92. Rec #: 882
Sunin RM. Intervention with Type A behaviors. J Consult Clin Psychol. 1982;50:933-949. Rec #: 2365
Tattersall RB, McCulloch DK, Aveline M. Group therapy in the treatment of diabetes. Diabetes Care.
1985;8:180-188. Rec #: 2196
Tobin D L, Reynolds R V C, Holroyd K A, Creer T L. Self-management and social learning theory. In:
Holroyd KA, Creer TL. (Eds.) Self-Management of Chronic Disease: Handbook of Clinical
Interventions and Research. Orlando, FL: Academic Press, 1986. Rec #: 914
Toobert DJ and Glasgow RE. Assessing diabetes self-management: The summary of diabetes selfcare activities questionnaire. Berkshire, England: Hardwood Academic. 1994. Rec #: 2446
Turk D, Meichenbaum D. A Cognitive-behavioral approach to pain management. In: Wall P, Melzack
R. Textbook of Paid . London: Churchill Livingstone, 1994. pgs. 1337. Rec #: 2085
Vickery DM. Medical self-care: a review of the concept and program models. Am J Health Promotion.
1986;Summer:23-28. Rec #: 2301
Vijan S Stevens DL Herman et al. Screening, prevention, counseling, and treatment for the
complications of type II diabetes mellitus. Putting evidence into practice. Journal of General
Internal Medicine. 1997;12(9):567. Rec #: 2613
Wagner E H, Austin B T, Von Korff M . Organizing care for patients with chronic illness. Milbank Q.
1996;74(4):511-44. Rec #: 894
Watts FN. Behavioral aspects of the management of diabetes mellitus: Education, self-care and
metabolic control. Behavior Research and Therapy. 1980;18:171-180. Rec #: 2278
15
Table 1. Review Articles
Wing RR. Behavioral strategies for weight reduction in obese Type II diabetic patients. Diabetes Care.
1989;12:139-144. Rec #: 2641
Wing RR, Epstein LH, Nowalk MP, Lamparski D. Behavioral self-regulation in the treatment of patients
with diabetes mellitus. Psychological Bulletin. 1986;99:78-89. Rec #: 2282
Health Care Quality Improvement Projects (HCQIP)
Each U.S. state and territory is associated with a Medicare Peer Review Organization
(PRO) that conducts various research projects. Centers for Medicare and Medicaid Services
(CMS), maintains a database with a narrative description of each research project, called a
Narrative Project Document (NPD). An NPD includes the aims, background, quality indicators,
collaborators, sampling methods, interventions, measurement, and results of a project. Our
search of the NPD database for studies on chronic disease self-management found none.
Experts
We contacted several experts in the field and asked for any studies which were in press or
undergoing review or that we had missed in our published literature.
Other Ongoing Reviews of Chronic Disease Self-management
During our review process we became aware of another group in Boston reviewing the
evidence on chronic disease self-management. While their focus was somewhat different than
ours, both groups were reviewing evidence on some illnesses in common. The two groups
therefore agreed to exchange reference lists (but no analytic strategies or results). The list of
studies included by the other group was provided by Daniel Solomon, MD.
16
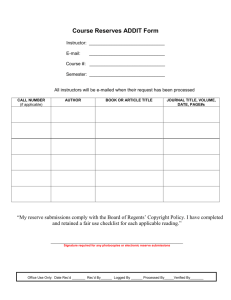
EVALUATION OF POTENTIAL EVIDENCE
We reviewed the articles retrieved from the literature sources against exclusion criteria to
determine whether to include them in the evidence synthesis. A one-page screening review form
that contains a series of yes/no questions was created for this purpose (Figure 2). Two
physicians, each trained in the critical analysis of scientific literature, independently reviewed
each study, abstracted data, and resolved disagreements by consensus. Dr. Shekelle resolved any
disagreements that remained unresolved after discussions between the reviewers. Project staff
entered data from the checklists into an electronic database that was used to track all studies
through the screening process.
While we were searching primarily for data relevant to the Medicare population, we
included studies that contained data on populations under age 65 to avoid loss of potentially
useful data. To be accepted, a study had to be a controlled clinical trial. We further classified
controlled clinical trials as randomized or not, based on the following definitions:
Randomized controlled trial (RCT). A trial in which the participants (or other units) are
definitely assigned prospectively to one of two (or more) alternative forms of health care, using a
process of random allocation (e.g., random number generation, coin flips).
Controlled clinical trial (CCT). A trial in which participants (or other units) are either
(a) definitely assigned prospectively to one of two (or more) alternative forms of health care
using a quasi-random allocation method (e.g., alternation, date of birth, patient identifier), or
(b) possibly assigned prospectively to one of two (or more) alternative forms of health care using
a process of random or quasi-random allocation.
17
Figure 2. Screening Form
1.
Article ID:
2.
First Author:
7.
(Last name of first author)
3.
Reviewer:
4.
Subject of article:
Circle one
Chronic disease self-management................... 1
Other ............................................................... 9 (STOP)
If other, then STOP
5.
6.
Conditions studied: (Check all that apply):
Heart disease
Heart failure
Angina pectoris
Other heart conditions
Back disorders
Osteoarthritis
Rheumatoid arthritis
Other (sp:___________)
Other (sp:___________)
Emphysema
Asthma
COPD
Hypertension
Diabetes
Other (sp:__________)
Unsure
8.Ages of study participants:
Circle one
Excludes over 65............................................. 1
Includes over 65.............................................. 2 (Answer #9)
Unsure............................................................. 9
Do interventions studied satisfy OUR definition of chronic
Check all that apply
disease self-management?
Studies a systematic intervention .................
…targeted towards patients..........................
…with chronic disease.................................
…to help them to actively participate .........
…in the following activities: ........................
self-monitoring (of symptoms or of
illness on quality of life), OR
decision-making (managing disease or
its impacts based on self-monitoring)
If ANY are unchecked, then STOP
9.
If study includes persons 65 and older, are the results
reported separately for this group?
Circle one
Yes .................................................................. 1
No ................................................................... 2
Not applicable ................................................. 8
Unsure............................................................. 9
Notes:
Circle one
Study design:
Descriptive (editorial etc. Do not pull) .......... 0 (STOP)
Review/meta-analysis (pull article)................. 1 (STOP)
Randomized Clinical Trial .............................. 2
Controlled Clinical Trial ................................. 3
Controlled Before and After............................ 4
Interrupted Time Series................................... 5
Simple Pre-Post............................................... 6
Cohort ............................................................. 7
Other ............................................................... 8
Unsure............................................................. 9
If descriptive or review article, then STOP
18
EXTRACTION OF STUDY-LEVEL VARIABLES AND RESULTS
Using a specialized Quality Review Form (QRF - see Figure 3) we abstracted data from
the articles that passed our screening criteria. The form contains questions about the study
design; the number and characteristics of the patients; the setting, location, and target of the
intervention; the intensity of the intervention; the types of outcome measures and the time from
intervention until outcome measurement. We selected the variables for abstraction with input
from the project’s technical experts. Two physicians, working independently, extracted data in
duplicate and resolved disagreements by consensus. A senior physician resolved any
disagreements not resolved by consensus.
To evaluate the quality of the study, we collected information on the study design (with
the hierarchy of internal validity being RCT, CCT, CBA, and ITS), withdrawal/dropout rate,
agreement between the unit of randomization and the unit of analysis, blinding and concealment
of allocation.25
19
Figure 3. Quality Review Form
Article ID:
6.
If reported, was the method of double blinding appropriate? (circle one)
Yes ........................................................................................1
No .........................................................................................2
Double blinding not described ..............................................8
Not applicable (not double blinded)......................................9
7.
If study was randomized, did the method of randomization provide for concealment
of allocation?
(circle one)
Yes ........................................................................................1
No .........................................................................................2
Concealment not described ...................................................8
Not applicable (not randomized)...........................................9
8.
Are numbers and reasons for withdrawals and dropouts described?
Reviewer:
First Author:
(Last Name Only)
Study Number:
of
Date of Publication:
(Enter ‘1of 1’ if only one)
Description (if more than one study):
Study Quality
(circle one)
1. Design:
RCT ......................................................................................1
CCT ......................................................................................2
If not RCT or CCT, then STOP.
2.
Does the study present data on people age 50 and up? (circle one)
Yes........................................................................................1
No .........................................................................................2
If not, reject --STOP.
3.
Is the study described as randomized?
(circle one)
Yes........................................................................................1
No .........................................................................................2
4.
If the study was randomized, was the method of randomization
appropriate?
(circle one)
Yes........................................................................................1
No .........................................................................................2
Method not described............................................................8
Not applicable (not randomized)...........................................9
5.
(circle one)
Is the study described as:
Double blind .........................................................................1
Single blind, patient ..............................................................2
Single blind, outcome assessment ........................................3
Open .....................................................................................4
Blinding not described ..........................................................8
(circle one)
Yes ........................................................................................1
No .........................................................................................2
9.
(circle one)
What is the geographic setting of the study?
Rural .....................................................................................1
Urban/Suburban ....................................................................2
Mixed....................................................................................4
) .......5
Other (specify:
Not specified .........................................................................8
10. What is the setting of study?
(circle one)
Academic ..............................................................................1
Non-academic .......................................................................2
Both academic and non-academic.........................................3
Not specified .........................................................................8
11. In what country was the study conducted?
(circle one)
US .........................................................................................1
Great Britain .........................................................................2
France ...................................................................................3
Germany ...............................................................................4
Other (specify:___________________________)................5
Not specified .........................................................................8
Figure 3. Quality Review Forms (con't)
12. What is the refusal rate?
___ ___ %
DIABETES STUDIES ONLY:
16. Type of diabetes:
(circle one)
Type I DM (IDDM) ............................................................1
Type II DM (NIDDM) ........................................................2
Both types ...........................................................................3
Not specified .......................................................................8
(Enter NR if not reported)
13. Which best describes the reimbursement system in which
the study occurred:
(check all that apply)
FFS ...................................................................................
HMO.................................................................................
MCO (not HMO) .............................................................
Mixed................................................................................
Other (specify:
) .......
Not sure.............................................................................
17. Which baseline diagnostic criteria were used?
(check all that apply)
Fasting blood sugar ...........................................................
Urine glucose ....................................................................
HgbA1c.............................................................................
Other (specify:
) .......
Diagnostic criteria not specified................................... .
14. Are data stratified by any of these groups or does a group
make up t 2/3 of the subjects?
(check all that apply)
85 and older ......................................................................
African-American ............................................................
Hispanic ...........................................................................
Other minority .................................................................
Low income .....................................................................
Nursing home ...................................................................
Veterans ............................................................................
) .......
Other (specify:
None of the above .............................................................
OA/RA STUDIES ONLY:
18. Type of disease:
(circle one)
RA only...............................................................................1
OA only ..............................................................................2
OA and RA .........................................................................3
Arthritis NOS......................................................................4
(check all that apply)
19. Which baseline diagnostic criteria were used?
X-ray .................................................................................
Physical Exam...................................................................
MD diagnosis w/o other detail ..........................................
Other (specify:__________________________)..............
Diagnostic criteria not specified........................................
15. Comorbid conditions
(check all that apply)
Heart disease (not hypertension).......................................
Hypertension.....................................................................
Kidney (renal) disease.......................................................
Chronic respiratory disease...............................................
PVD ..................................................................................
Neuropathy .......................................................................
Obesity..............................................................................
DM....................................................................................
Arthritis.............................................................................
CHF ..................................................................................
Tobacco Abuse .................................................................
Angina ..............................................................................
Other (specify:
) .......
None specified ..................................................................
MI STUDIES ONLY:
(check all that apply)
20. Type of disease:
Uncomplicated ..................................................................
Complicated ......................................................................
First Occurrence................................................................
Recurrence ........................................................................
Angina w/o infarction .......................................................
Angina w/ infarction .........................................................
Unsure/ unspecified ..........................................................
21. Which baseline diagnostic criteria were used?
(check all that apply)
CPK-MB elevation............................................................
Cardiac troponins ..............................................................
ECG ..................................................................................
Diagnostic criteria not specified........................................
Other (specify:__________________________)..............
21
Figure 3. Quality Review Forms (con't)
If study has a control group, then enter data for that group here. Otherwise,
enter data for each group in order of first mention. Complete one page for each arm
Use these abbreviations for interval:
MI
minute WK
week
HR
hour
MO
month
DY
day
YR
year
Arm ____ of ____ Description:
22.
ND not described
NA not applicable
Intervention:
Intervention
component
Target
Content
Delivery
by/during
Provider
type
Setting
Frequency per interval
Duration of session/
units
Total # of
sessions
Total duration / units
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
23. What was the sample size in this intervention arm?
___ ___ ___ , ___ ___ ___
___ ___ ___ , ___ ___ ___
Entering
(Enter 999,999 if not reported.)
26. What was the length of the intervention period?
_________
_________
Number
Completing
Units
Enter MI, HR, DY, WK, MO, YR as defined above
IF “usual care” then SKIP to next page
24. Was there a protocol for the intervention?
(circle one)
Yes......................................................................................1
No .......................................................................................2
Protocol not mentioned .......................................................8
27. Were the intervention providers’ qualifications appropriate? (circle one)
Yes ......................................................................................1
No .......................................................................................2
Qualifications not described................................................8
25. Was the intervention tailored to the individual?
(circle one)
Yes......................................................................................1
No .......................................................................................2
Qualifications not described................................................8
28. Were the providers homogeneous?
(circle one)
Yes ......................................................................................1
No .......................................................................................2
Therapists not described......................................................8
22
Grouped With
Figure 3. Quality Review Forms (con't)
Outcomes, Evaluation, and Statistics
30. When, relative to the start of the intervention, were outcomes measured?
29. Type of outcomes measured:
Enter the code for each outcome measured. Circle at least
one of the letters “P”, “A”, and “L” for each outcome
measured. If rating method is not described, circle ONLY
“ND”.
Patient, assessor, or
laboratory rated?
(ND=not described)
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
P
A
L
Enter the number of weeks in the appropriate box. Enter ‘999’ if not applicable.
use the following
abbreviations for units:
Number
Unit
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
N
D
1st follow-up
2nd follow-up
3rd follow-up
MI
HR
DY
WK
MO
YR
minute
hour
day
week
month
year
4th follow-up
5th follow-up
31. What was the unit of allocation?
(circle one)
Patient .................................................................................1
Provider...............................................................................3
Organization (practice, hospital, HMO, community)..........4
) .....6
Other (specify:
Not reported ........................................................................8
32. What was the unit of analysis?
(circle one)
Patient .................................................................................1
Provider...............................................................................3
Organization (practice, hospital, HMO, community)..........4
Other (specify:
) .....6
Not reported ........................................................................8
33. If the unit of allocation is not the same as the unit of analysis, was any
statistical correction made for clustering?
(circle one)
Yes ......................................................................................1
No .......................................................................................2
Not sure...............................................................................8
Not Applicable....................................................................9
34. Was any cost information provided?
(circle one)
Yes ......................................................................................1
No .......................................................................................2
23
Figure 3. Quality Review Forms (con't)
Hypertension Only Studies
Article ID:
First Author:
Description:
Reviewer:
35. Types of hypertension
(circle one)
Essential ................................................. 1
Secondary............................................... 2
Both........................................................ 3
Not specified .......................................... 8
Not applicable ........................................ 9
37. Types of hypertension
(circle one)
Treated ................................................... 1
Untreated................................................ 2
Both........................................................ 3
Not specified .......................................... 8
Not applicable ........................................ 9
36. Types of hypertension
(circle one)
Systolic................................................... 1
Diastolic ................................................. 2
Both........................................................ 3
Not specified .......................................... 8
Not applicable ........................................ 9
38. Which baseline diagnostic criteria
were used?
(check all that apply)
One blood pressure recording ...............
More than 1 recording...........................
MD diagnosis ........................................
Other (specify:_________________) ...
Diagnostic criteria not specified ...........
39. Medication Treatment?
(circle one)
Yes ......................................................... 1
No........................................................... 2
Other: (specify:_________________) ... 3
Not specified .......................................... 8
Not applicable ........................................ 9
24
Figure 3. Quality Review Forms (con't)
Code Sheet
Intervention components
1. Control
2. Usual Care
3. Advocacy training (how to ask MDs)
4. ASMP (Arthritis self-management)
5. Clinical reviews w/ patient
6. Cognitive-behavioral (including
relaxation training)
7. Consultation with specialists
8. Contracts
9. Counseling/Therapy
10. Dietary monitoring
11. Education
12. Feedback
13. Financial incentives
14. Mass media
15. Nontraditional therapies (massage,
acupuncture, biofeedback, etc.)
16. Practice methods
17. Psychological assessment/care
18. Emotional support
19. Reminders/reinforcement
20. Material incentive
21. Referrals
22. Unstructured group time
23. Exercise program
24. Competition between groups
25. Exercise diary
26. Follow up
27. Social/peer support
28. Cholesterol lowering medication
29. Placebo medication
30. Practice self care skills
31. Goal setting
32.
33.
34.
35.
36.
37.
38.
39.
40.
99.
Exercise testing
Exercise monitoring
Patient directed discussion group
Compensation for participation
Practice diagnostic skills
Blood pressure monitoring
Self monitoring
Medication therapy
Blood pressure lowering medication
Component not specified
Targets, provider types
1. Patients
2. Physicians
3. Psychologists
4. Psychiatrists
5. Nurses
6. Nurse practitioners
7. Other/non-specified medical
professionals
8. Educators
9. Nutritional Expert
10. Office Staff
11. Non-medical personnel not staff
12. Lay leaders
13. Lay (affected) leaders/role models
14. Family members
15. Research assistants
16. Qualified researchers
17. Researchers, qualifications not
specified
18. Physical/Occupational Therapists
19. Health care organizations (e.g.,
HMOs)
25
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
Hospitals
Clinics
Practices
Other organizations, not specified
Group facilitator
Podiatrist
Pharmacist
Exercise leader
Medical student
Exercise therapist
Social worker
Physician assistant
Therapist/counselor
_
_
Psychologists and nurses
Figure 3. Quality Review Forms (con't)
Code Sheet
Specific Content
1. Behavioral assessment/strategies
2. Diet
3. Disease information
4. Exercise
5. Foot care
6. Medication information/compliance
7. Pain coping skills
8. Physical activity
9. Prevention NOS
10. Smoking cessation
11. Stress management
12. Weight management
13. Sleep/fatigue management
14. Symptom management
15. Use of community resources
16. Communication skills
17. Problem solving/decision making
18. Goal setting
19. Empowerment
20. Communicating with professionals
21. Treatment information
22. Adherence/compliance
23. Self-help
24. BG(Blood Glucose) machine use
25. Sexual activity/dysfunction
26. Complementary therapy
27. Cognitive assessments/strategies
28. Self-monitor
29. Blood glucose monitor
30. Joint preservation
31. Relaxation methods
32. Emotional symptoms
33. Urine monitor
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
99.
Metabolic control
Educational methods
Rehabilitation
Blood pressure
Psychotherapy
Exercise capacity
Pain
CPR
Cardiac function
Work
Psychosocial issues
Medication administration
Physical exam
Alcohol
Peer support
Symptoms NOS
Depression
Content not specified
Content Delivered By/During
1. Group meeting
2. Office visit
3.
4. Hospitalization
5. Home visit
6. Telephone
7. Mail (postcards, letters)
8. Detailed reading materials mailed
(pamphlets, newsletters)
9. Detailed reading materials (handouts)
10. Instructional manuals
11. Computer program
12. Email/Internet
26
13.
14.
15.
16.
17.
18.
19.
99.
Video/Audio tapes
Other mechanisms
One on one NOS
Protocols
Detailed reading materials NOS
Self-delivery
Prescription
Mechanism not specified
Settings
1. Hospital
2. Home
3. In office
4.
5. Other setting specified (write in)
6. Nursing home
7. Day center
8. Community Center
99. Setting not specified
Frequency Per Interval
98. Variable frequency
Figure 3. Quality Review Forms (con't)
Code Sheet
Outcomes
DIABETES
1. Diabetic complications
2. Foot care activity
3. Foot lesions
4. FSBG
5. HgbA1c
6. Hypoglycemic episodes
7. Self monitoring frequency (BG)
8. Diabetic symptoms
9. Postpandrial blood glucose
10. C-peptide
11. Urine glucose
12. Self-monitoring accuracy
13. Plasma insulin
14. Creatinine
15. Self-monitoring frequency(UG)
OA
30.
31.
32.
33.
Pain measurement
Physical performance
Mobility
Stiffness
MI
60.
61.
62.
63.
64.
65.
66.
67.
68.
“Rose” questionnaire
Cholesterol
Occurrence/Reoccurrence of MI
Sexual activity (same as 112)
Tobacco use
Hypertension
Angina
Arrhythmia
CABG
69.
70.
71.
72.
73.
74.
75.
Ischemic heart disease
CHF
Cardiac symptoms
Angioplasty (PTCA)
Chest pain
ECG
Exercise tolerant test
(ETT)/Treadmill
OTHER/COMMON
90. MD visits
91. Nurse visits
92. Behavioral measures
93. Blood pressure
94. Coping strategies
95. Depression assessment
96. Dietary measures
97. Disability, physical
98. Disease duration
99. Emotional well-being
100. Exercise frequency
101. Health service utilization NOS
102. Hospitalization
103. Hospitalizations (Days)
104. Interpersonal support
105. Mortality
106. Patient knowledge
107. Patient Satisfaction
108. Provider Satisfaction
109. Psychological measures
110. Quality of life scales
111. Self-efficacy (helplessness)
112. Social assessment
113. Weight control
27
114.
115.
116.
117.
118.
119.
120.
121.
122.
123.
124.
125.
126.
127.
128.
129.
130.
131.
132.
133.
134.
135.
136.
137.
138.
139.
140.
141.
142.
999.
Self rated health
ER visits
Functional status
Medication compliance
Medication use
Work activity
Sexual activity (same as 63)
Physical activity
BMI (Body Mass Index)
Self care
Physician-patient interactions
Cardiac procedures
Compliance/adherence
Marital Adjustment
Aerobic capacity (VO2Max)
Anaerobic threshold
Skin fold thickness
Problem solving
Anxiety
Exercise capacity (METS)
Alcohol use
Heart rate
Symptoms
Catecholamines
Urinary sodium
Physiologic measures
Renin
Cognitive measures
BUN (plasma urea)
Not specified
STATISTICAL METHODS
In the analysis, we sought to answer the questions specified by CMS that can be found at
the beginning of the Methods Section.
Our summary of the evidence is both qualitative and quantitative. We first assessed the
distribution of studies based on the classification of interventions as specified in our data
abstraction form (Figure 3). For many of the fourteen specific questions listed above, the
evidence was too sparse and/or heterogeneous to support statistical pooling. In these cases, our
summary of evidence is qualitative.
To help answer Question 2 posed by CMS, we proposed five overall hypotheses that
encompassed the questions concerning intervention components. These hypotheses were listed
in the introduction. We denote these as the “original” hypotheses to distinguish them from posthoc hypotheses we tested subsequently. We recoded each intervention arm in each study into
“yes” (met hypothesis) or “no” (did not meet hypothesis), and conducted analyses to test these
hypotheses as described below.
Meta-Analysis
We conducted separate meta-analyses for each of the four conditions: diabetes,
osteoarthritis, post-myocardial infarction care, and hypertension. Though separate, these
analyses were sufficiently similar that we will discuss our general analytic approach, inserting
comments about specific outcomes or conditions as needed.
We first identified the most commonly reported clinically relevant outcome or outcomes
for each condition. These outcomes were:
28
x for diabetes
–
fasting blood glucose
–
hemoglobin A1c
–
weight
x osteoarthritis
–
pain
–
functioning
x post-myocardial infarction care
–
mortality
–
return to work
x hypertension
–
systolic blood pressure
–
diastolic blood pressure
We considered only studies that assessed the effects of an intervention or interventions
relative to either a group that received usual care or a control group and that provided outcome
data.
The majority of our outcomes were continuous. For these outcomes we extracted data to
estimate effect sizes. The effect size for the study’s comparison between a particular
intervention arm and usual care or control arm is the difference between the intervention group
and usual care or control group divided by its standard deviation, and is therefore a unitless
29
measure convenient for comparing studies measuring outcomes in the same domain but using
different measures. For the two dichotomous outcomes (mortality and return to work for postmyocardial infarction care), we estimated risk ratios. We will discuss each of these general types
of outcomes in turn.
Because follow-up times across studies can lead to clinical heterogeneity, we excluded
from analysis any studies whose data were not collected within a specified follow-up interval.
These intervals were chosen based on clinical knowledge. For diabetes, studies that had a
follow-up time between three and twelve months were included. Four studies were excluded
because their follow-up time fell outside this interval. For osteoarthritis, all studies retrieved
included a follow-up time between four and six months. One study had multiple follow-up times
between four and six months, and we included the measurement that was closest to six months.
For post-myocardial infarction care, studies that had a follow-up time between six and twelve
months were included, and no studies were excluded due to follow-up time. For hypertension,
all studies were included; a follow-up time between two and six months was used. Four studies
had multiple follow-up times but had only one data point in between two and six months, and we
included this measurement in our analysis.
Some studies had more than one intervention arm of interest. For these “multi-arm”
studies, we estimated one effect size or one risk ratio (depending on the outcome) for each
comparison between an intervention arm and the control or usual care group. The possibility that
a single study might contribute multiple treatment effects to a meta-analysis was addressed via a
sensitivity analysis discussed below.
Data extraction and basic calculations were performed in the statistical package SAS26
and the spreadsheet package Excel.27 The majority of the modeling was performed in the
30
statistical package Stata,28 with some special modeling implemented in StatXact29 for the
mortality outcome, and sensitivity analyses conducted in statistical software package SAS26 as
described below.
Continuous Effect Sizes
For each study, we estimated an effect size for each comparison that was considered
relevant, that is for each intervention arm of interest as compared with the usual care or control
arm. The follow-up mean and standard deviation of each outcome for each relevant arm were
extracted if available. If a study did not report a follow-up mean, or a follow-up mean could not
be calculated from the given data, the study was excluded from the meta-analysis.
For studies that did not report a standard deviation or for which a standard deviation
could not be calculated from the given data, we imputed the standard deviation by using those
studies and arms that did report a standard deviation and weighting all arms equally, or we
assumed that the standard deviation was 0.25 of the theoretical range for the specific measure in
the study. For example, if a study measured pain on a 0-100 scale, we assumed the standard
deviation was 25.
No imputation was required for the diabetes outcomes. For osteoarthritis outcomes, we
used the range approach to impute the standard deviations for pain and functioning for five
studies. For hypertension outcomes, we used five of the studies to impute the standard deviations
for both blood pressure outcomes for the remaining six studies. The post-myocardial infarction
care outcomes were dichotomous and required no imputation, as discussed below.
For each comparison of interest, an unbiased estimate9 of Hedges’ g effect size10 and its
standard deviation were calculated. A negative effect size indicates that the intervention is
31
associated with a decrease in the outcome at follow-up as compared with the control or usual
care group. For example, in the osteoarthritis meta-analysis, the outcome was pain, so a negative
effect size indicated that the intervention was associated with a decrease in pain at follow-up as
compared with the control group.
Risk Ratio Calculations for Dichotomous Outcomes
For the return-to-work outcome for post-myocardial infarction care, we estimated log risk
ratios and standard deviations. We conducted the analysis on the logarithmic scale for variancestabilization reasons.30 We then back-transformed to the risk ratio scale for interpretability.
A risk ratio greater than one indicates that the risk of the outcome in the intervention arm
is larger than that in the control or usual care arm. For example, if the risk ratio is 1.10, then
patients in the intervention group are 1.10 times as likely to return to work as those in the control
or usual care arm.
One study reported that all patients in a particular arm returned to work. For this study,
we performed a continuity correction by adding 0.5 to all cells in the two-by-two table of arm by
outcome. This continuity correction is necessary in order for the risk ratio and its standard
deviation to be estimated.
Mortality was a rare event and the asymptotic method used for the return-to-work
outcome would have required continuity corrections for many studies, not just one as in the
return-to-work situation. We were concerned that many corrections would bias our results.
Thus, we employed exact calculations to estimate the risk ratios using statistical software
package StatXact.29 This approach uses exact nonparametric inference and, in particular, does
not require continuity corrections to be performed for zero cells. For mortality, a risk ratio less
32
than one indicates that the risk of mortality in the intervention arm is smaller than that in the
control or usual care arm.
Analysis
For each condition and outcome except for mortality, we conducted the same analysis.
For this analysis, we first calculated a pooled random effects estimate11 of the treatment effect, a
pooled effect size for continuous outcomes, or a pooled log risk ratio for the dichotomous
outcome of return to work, as appropriate, across all studies and their associated 95% confidence
interval. We then back-transformed to the risk ratio scale for return to work. We used exact
calculations to estimate the pooled risk ratio of mortality directly. We assessed the betweenstudy heterogeneity for each outcome using a chi-squared test of heterogeneity p-value.9
For each of the original five hypotheses, study arms either meet the criteria (a “yes”) or
do not (a “no”), thus no missing values exist. For each hypothesis, a simple stratified analysis
would have produced a pooled estimate of the treatment effect for all the “yes” study arms
together and a pooled estimate for all the “no” study arms together. To facilitate testing the
difference between the two pooled estimates, we constructed these estimates using a metaregression model in which the only variables in the regression were a constant, and an indicator
variable equal to one if the study arm met the hypothesis and zero if the study arm did not. For
some outcomes and hypotheses, all study arms were either "yes" or "no". In this case, we could
not fit a model, and we labeled those situations as “not estimable (NE)” in our Results tables.
A random effects meta-regression31 allows a straightforward statistical test of the
coefficient for the indicator variable, which is equivalent to testing whether the “yes” pooled
treatment effect and the “no” pooled treatment effect are equal, i.e., whether there is evidence
33
against the hypothesis. In addition, we estimated 95% confidence intervals for each treatment
effect ("yes" and "no"). If the confidence interval does not contain the null value of zero (for a
continuous outcome) or one (for a risk ratio outcome), the treatment effect is probably
statistically significant. For each outcome, we fit five separate regressions, corresponding to the
five original hypotheses. We estimated these models in the statistical package Stata28 using the
“metareg” command with the restricted maximum likelihood estimation option.32
For the mortality outcome, we used exact calculations to conduct the stratified analyses
separately and observed whether the resulting confidence intervals overlapped in order to
determine if there was evidence against each hypothesis. For this outcome, we did not allow
multiple intervention arms per study to contribute to a single stratified analysis. To eliminate
this occurrence, we collapsed the data over multiple intervention arms within a single study
within each stratified analysis. By collapsing the data, we mean we aggregated the numbers of
patients and deaths across all intervention arms in a single study into a combined single
intervention arm.
As an overall test of all the hypotheses, we combined the pain outcomes from
osteoarthritis studies, hemoglobin A1c outcomes from diabetes studies, and systolic blood
pressure outcomes from hypertension studies into one analysis and fit the five separate
regressions as above. These outcomes were chosen because we judged them to be the most
clinically relevant continuous outcomes for each condition. We also fit a sixth regression that
had a constant and all five indicator variables for the separate hypotheses included. Postmyocardial infarction care studies did not have a continuous outcome, so we could not include it
in our overall test of the hypotheses.
34
Sensitivity Analyses
Within each regression, and especially in the combined analysis, our primary analyses
ignored the fact that some studies had multiple intervention arms and thus could contribute more
than one treatment effect to the analysis. The correlation between treatment effects within the
same study, due to the fact the each intervention arm was compared to the same control or usual
care arm, was ignored in this analysis. Among diabetes studies, two studies had two intervention
arms each; among osteoarthritis studies, three studies had two intervention arms; and among
hypertension studies, four studies had two intervention arms, and two studies had three
intervention arms. In post-myocardial infarction care, we collapsed across intervention arms in
the same study as done in the primary mortality analysis. For this outcome, two studies had two
intervention arms and one study had five intervention arms.
Our sensitivity analyses consisted of refitting the meta-regression models using a twolevel random effects model that contains a random effect at the study level, as well as one at the
arm level. This hierarchical approach controls for the potential correlation within arms in the
same study. We estimated these models in the statistical software package SAS26 using PROC
MIXED.
For the mortality outcome, no sensitivity analysis of the possible effect of multiple
intervention arms was needed as we collapsed prior to analysis as described above. None of these
sensitivity analyses results differed markedly from that of the primary analysis we present in this
report.
35
Assessment of publication bias
We assessed the possibility of publication bias by evaluating funnel plots of effect sizes
or log risk ratios for asymmetry, which results from the non-publication of small, negative
studies. Because graphical evaluation can be subjective, we also conducted an adjusted rank
correlation test33 and a regression asymmetry test34 as formal statistical tests for publication bias.
We conducted these tests at the intervention arm level, and also at the study level by choosing
only the most statistically significant treatment effect for multi-arm studies as a sensitivity
analysis. We conducted all analyses and constructed all graphs using the statistical package
Stata.28
COST EFFECTIVENESS
To assess the cost-effectiveness of the interventions, we first determined whether the
studies included cost data. We chose to summarize these studies qualitatively because of
heterogeneity.
EXPERT REVIEW PROCESS AND POST-HOC ANALYSES
The draft evidence report was presented to a group of experts in chronic disease selfmanagement at a meeting convened by the Robert Wood Johnson Foundation and held in Seattle
on December 14, 2001. The list of experts attending is present in Appendix A. At this meeting,
the draft evidence report, which had been mailed to each panelist several weeks in advance, was
presented and discussed. As a result of this discussion several additional hypotheses and
analyses were proposed, which we term “post-hoc” hypotheses and analyses since they were
generated after seeing the results of the original five hypotheses analyses. These “post-hoc”
hypotheses and analyses were:
36
x Assessing the effectiveness of intervention components as defined by the RE-AIM
model of Glasgow.
x Assessing the effectiveness of CDSM programs stratified by severity of illness at
baseline.
x Assessing the effectiveness of CDSM program components as classified by the
“Essential Elements of Self-management Interventions,” which was the result of the
group discussion at the Seattle meeting.
x Assessing the effectiveness of CDSM program that assessed and demonstrated
improvement in “intermediate” variables according to the following conceptual
model:
InterventionÆ
knowledge, self-efficacy, Æ dietary measures Æ
attitudes
physical activity
behavior
hemoglobin A1c
pain
blood pressure
With regard to the first suggested analysis, components of CDSM were classified in REAIM as including:12
x one-on-one counseling interventions,
x group sessions,
x interactive computer-mediated interventions,
x telephone calls,
x mail interventions, and
x health system policies.
37
We coded each of our included articles as having each component present or not, and
then conducted meta-analysis and meta-regression analyses for each hypothesis using the method
described previously for our original hypotheses. “Health system policies” was particularly
difficult to define, so we developed both a “strict” and a “broad” definitions, and tested each.
With regard to stratifying by severity at presentation, we assessed those studies that
presented baseline information on blood pressure, hemoglobin A1c, weight, glucose control,
pain, and function, and stratified these into two categories: “more severe” and “less severe.” We
were not able to stratify the hypertension studies or diabetes studies reporting fasting blood
glucose outcomes as the distributions of baseline values in these studies did not support a
“threshold” value. We were able to stratify by severity for hemoglobin A1c, weight, pain, and
functioning. Effect sizes were then compared between studies of “more severe” and “less
severe” patients at baseline.
With regard to the “Essential Elements of Self-management Interventions,” these were
defined by the Seattle Expert Panel to be:13
1. problem-solving training that encourages patients and providers
identify problems
identify barriers and supports
general solutions
form an individually tailored action plan, including:
à long and short-term goals
à goals that are measurable and achievable
38
monitor and assess progress toward goals, including feedback
adjust the action plan as needed, reinforcing positive outcomes
à repeat problem-solving process, enhancing the person’s
–
confidence or self-efficacy (“I can do it.”)
–
skill mastery (“Here’s how.”)
–
modeling (“I am not alone.”)
–
Social persuasion (“I can be a role model for others.”)
–
Ability to re-interpret symptoms (“I know what different symptoms
mean.”)
2. follow-up
maintain contact and continued problem-solving support via one of many
available modalities (e.g., telephone, e-mail, mail, etc)
identify patients who are not doing well and assist them in modifying their plan
and actions to ensure optimal outcomes
relate plan to patient’s social/ cultural environment
à teach patients how to connect with resources and support in their own
community because the need for these links changes over time
3. tracking and ensuring implementation
programs should be linked to the individual’s regular source of medical care
39
à communication among the patient, the self-management delivery staff, and the
patient’s usual provider of medical care is likely to improve results
programs should monitor their effects on patients’ health, satisfaction, quality of
life, and the health-system quality measures in order to help make improvements
over time and to help decision-makers evaluate the benefits
For our purposes, the studies available were not characterized in detail sufficient to
perform an analysis except at the coarsest level of aggregation:
x problem-solving training
x follow-up
x tracking and ensuring implementation
Each of our included studies was characterized as having these features as present or
absent, and then we performed meta-analysis and meta-regression analyses for each hypothesis
using the method previously described. We ran a meta-regression controlling for each of the
three components separately. We then ran a meta-regression controlling for all three components
simultaneously and calculated an adjusted effect size for each component.
Lastly, to assess the effectiveness of CDSM programs according to their effect on
intermediate variables, we identified those studies that assessed intermediate variables and with
the help of Russ Glasgow, MD, we classified these into the previously presented model. We
then assessed the effectiveness of the CDSM programs by regressing the effect size of
“intermediate 2 variables” (such as dietary measures, physical activity, behavioral measures) on
“intermediate 1 variables” (such as self-efficacy, patient knowledge, psychological measures)
and regressing the effect size of “outcome variables” (such as hemoglobin A1c, pain, systolic
40
blood pressure) on “intermediate 2 variables.” The conceptual model for these analyses is that
studies with interventions that promote improvements in self-efficacy, patient knowledge, and
psychosocial measures should be more likely to result in improvements in dietary measures,
physical activity, and behavioral measures, which in turn should lead to improvements in
outcomes measures such as hemoglobin A1c, pain, and blood pressure. Therefore, studies that
measured these “intermediate variables” can be assessed to see if their evidence support this
conceptual model.
41
RESULTS
IDENTIFICATION OF EVIDENCE
Figure 4 describes the flow of evidence from the original sources to final acceptance for
our review. The Cochrane Database provided 15 relevant citations. From the Center for
Advancement of Health publication, An Indexed Bibliography on Self-management for People
with Chronic Disease, we ordered 168 articles based on a review of included abstracts. 549
additional articles were ordered upon review of the reference lists from these articles. A library
search yielded an additional seven articles and four additional articles not previously noted were
obtained from experts. From the Boston group, we received a reference list of 62 articles
included in their analysis that were not in our dataset. Of these, however, only nineteen were
considered for screening after title review. Articles were rejected at title review because their
focus was on conditions not included in our analysis (such as studies of asthma, rheumatoid
arthritis, or fibromyalgia), or concerned children or young adults (Figure 5). In total, the above
sources yielded 762 articles. We were unable to obtain 23 of these. This left 739 articles for the
screening process.
42
Figure 4. Flow of Evidence
Cochrane
Review
(n = 15)
Center for
Advancement
of Health
(n = 168)
Reference
Lists
(n = 549)
Library
Search
(n = 7)
Identified
by Expert
(n = 4)
Boston
Group
(n = 19)
n=4
n = 19
762 Articles Requested
n = 15
n = 168
n = 526
n=7
23 Not Found
739 Articles Screened
n=0
n = 26
n = 80
n=2
n=3
n = 10
121 Articles Passed on to Quality Review
79 Articles Passed on to Consideration for Meta-Analysis
44 Articles Contribute Data to Meta-Analysis
9 Myocardial Infarction
14 Diabetes
14 Hypertension
7 Osteoarthritis
43
618
79
13
77
319
122
8
Rejected
Subject
Age
CDSM Definition
Study Design
Condition
Duplicate Article
42 Rejected:
14 not RCT study design
28 no usual care or comparable control group
35
20
5
6
4
Rejected:
insufficient statistics
follow-up time outside 3-12 months
no relevant outcomes
duplicate data or study population
Of the 739 articles screened, 79 did not assess chronic disease self-management. Three
hundred nineteen were rejected because they were not randomized controlled trials (RCTs) or
controlled clinical trials (CCTs), 13 because they did not satisfy the age criteria (not adults), and
122 did not discuss one the conditions of interest (osteoarthritis, diabetes, hypertension, or postmyocardial infarction care). Another 8 articles were duplicates of articles already on file.
Seventy-seven others did not meet our chronic disease self-management definition. This left 121
articles for further review.
SELECTION OF STUDIES FOR THE META-ANALYSIS
Studies that met the inclusion criteria listed above were reviewed in more detail for
potential inclusion in the meta-analysis. At the first stage of this review, a study needed to be an
RCT and compare a chronic disease self-management program to a control or usual care group.
Of the 121 studies accepted for quality review, 79 went on to be considered for meta-analysis
because they were randomized controlled trials with a usual care or comparable control group.
These studies were then reviewed in more detail regarding their reported outcomes and followup times. Based on the distribution of these outcomes and follow-up times, and using our
clinical judgment, we accepted into the next stage diabetes studies that reported any of the
following outcomes: hemoglobin A1c, weight, and/or fasting blood glucose, with a follow-up
time between 3 - 12 months. If there was more than one follow-up time, the time closest to 12
months was selected for inclusion in the final analysis. For osteoarthritis, we accepted studies
that reported a pain outcome or a function outcome. For post-myocardial infarction care, we
used studies with return to work and mortality outcomes. For hypertension, studies that reported
mean systolic and diastolic blood pressure outcomes, with follow-up time of between 8 weeks to
44
6 months were selected for inclusion. If more than one follow-up time was reported, the time
closest to 6 months was selected.
Of the 79 studies considered for meta-analysis, 35 studies were excluded because of
insufficient statistics and/or follow-up times, no relevant outcomes, duplicate data (data
presented in another included study), or duplicate study populations. From the 19 articles
received from the Boston group only two meet the eligibility criteria for our meta-analysis, the
remainder being rejected due to not being a controlled trial, not having a usual care or
comparable control group, or not having sufficient statistical data for meta-analysis (Figure 5).
Therefore, forty-four studies contributed data to the meta-analysis (14 diabetes studies, 7
osteoarthritis studies, 9 post-myocardial infarction care studies, and 14 hypertension studies; see
Tables 2-5).
45
Figure 5. Article Flow of References from Boston Group
Boston List (n = 70)
8 Rejected: Duplicate of article in database
43 Rejected at title review
19 Passed Title Review
on to Article Screening
5 Rejected: Not condition of interest
4 Rejected: Study design not RCT or CCT
10 Articles Accepted after Screening
on to QRF
3 Rejected: No usual care or comparable control group
1 Rejected: Age
6 Articles Accepted after QRF
on to Data Extraction
4 Rejected: Insufficient statistics
2 Articles Accepted into meta-analysis
46
Table 2. Articles Rejected from Meta-analysis
Reason for Exclusion
Diabetes Articles
Integrated care for diabetes: clinical, psychosocial, and economic evaluation.
Diabetes Integrated Care Evaluation Team. BMJ. 1994;308(6938):12081212. Rec #: 2614
no usual care or comparable
control group
Allen BT, DeLong ER, Feussner JR. Impact of glucose self-monitoring on noninsulin-treated patients with type II diabetes mellitus. Diabetes Care.
1990;13:1044-1050. Rec #: 2201
no usual care or comparable
control group
Anderson R M, Funnell M M, Butler P M, Arnold M S, Fitzgerald J T, Feste C C .
Patient empowerment. Results of a randomized controlled trial. Diabetes
Care. 1995;18(7):943-9. Rec #: 747
not RCT
Arseneau D L, Mason A C, Wood O B, Schwab E, Green D . A comparison of
learning activity packages and classroom instruction for diet management of
patients with non-insulin-dependent diabetes mellitus. Diabetes Educ.
1994;20(6):509-14. Rec #: 749
no usual care or comparable
control group
Aubert RE Herman WH Waters J et al. Nurse case management to improve
glycemic control in diabetic patients in a health maintenance organization.
A randomized, control trial (see comments). Annals of Internal Medicine.
1998;129(8):605. Rec #: 2581
no usual care or comparable
control group
Bethea DC, Stallings SF, Wolman PG, Ingram RC. Comparison of conventional
and videotaped diabetic exchange lists instruction. Journal of the American
Dietetic Association. 1989;89:405-406. Rec #: 2105
not RCT
Bloomgarden ZT, Karmally W, Metzger J, Borhters M, Nechemias C, Bookman
J, et al. Randomized, controlled trial of diabetic education: improved
knowledge without improved metabolic status. Diabetes Care.
1987;10:263-272. Rec #: 2172
follow-up time not 3-12 months
Boehm S, Schlenk E A, Raleigh E, Ronis D . Behavioral analysis and
behavioral strategies to improve self- management of type II diabetes. Clin
Nurs Res. 1993;2(3):327-44. Rec #: 754
insufficient statistics
Campbell EM Redman S Moffitt PS et al. The relative effectiveness of
educational and behavioral instruction programs for patients with NIDDM: a
randomized trial. Diabetes Educator. 1996;22(4):379. Rec #: 2586
insufficient statistics
de Bont AJ, Baker IA, St Leger AS, Sweetman PM, Wragg KG, Stephens SM, et
al. A randomized controlled trial of the effect of low fat diet advice on
dietary response in insulin independent diabetic women. Diabetologia.
1981;21(6):529. Rec #: 2210
no usual care or comparable
control group
Emori KH. The Use of a Programmed Textbook in Diabetic Patient Education.
Loma Linda, CA: Loma Linda University; 1964. [Dissertation]. Rec #: 2118
follow-up time not 3-12 months
Glasgow RE/Toobert DJ, Mitchell DL, Donnely JE, Calder D. Nutrition
education and social learning interventions for type II diabetes . Diabetes
Care. 1989;12:150-152. Rec #: 2209
insufficient statistics
Glasgow R E, Toobert D J, Hampson S E . Effects of a brief office-based
intervention to facilitate diabetes dietary self-management. Diabetes Care.
1996;19(8):835-42. Rec #: 799
insufficient statistics
Glasgow RE, La Chance PA, Toobert DJ, Brown J, Hampson SE, Riddle MC.
Long-term effects and costs of brief behavioural dietary intervention for
patients with diabetes delivered from the medical office. Patient Educ Couns
1997;32(3):175-84. Rec #: 3433
insufficient statistics
47
Table 2. Articles Rejected from Meta-analysis
Reason for Exclusion
Hanefield M Fischer S Schmechel H et al. Diabetes Intervention Study. Multiintervention trial in newly diagnosed NIDDM. Diabetes Care.
1991;14(4):308. Rec #: 2595
no usual care or comparable
control group
Hassell J, Medved E. Group/audiovisual instruction for patients with diabetes.
Journal of the American Dietetic Association. 1975;5:465-470. Rec #: 2121
no glucose or weight outcomes
reported
Hoskins PL Fowler PM Constantino M et al. Sharing the care of diabetic
patients between hospital and general practitioners: does it work? Diabetic
Medicine. 1993;10(1):81. Rec #: 2597
no usual care or comparable
control group
Kaplan, Wilson, Hartwell/Merino, Wallace. Prospective evaluation of HDL
changes after diet and physical conditioning programs for patients with Type
II diabetes mellitus. Diabetes Care. 1985;8:343-48. Rec #: 2817
insufficient statistics
Kaplan RM, Hartwell SL, Wilson KD, Wallace JP. Effects of diet and exercise
interventions on control and quality of life in non-insulin dependent diabetes
mellitus. J Gen Intern Med. 1987;2:220-227. Rec #: 2175
insufficient statistics
Kendall PA, Jansen GR. Educating patients with diabetes: comparison of
nutrient-based and exchanged group methods. J Am Diet Assoc.
1990;90:238-243. Rec #: 2207
no usual care or comparable
control group
Kinmonth AL Woodcock A Griffin S et al. Randomised controlled trial of patient
centred care of diabetes in general practice: impact on current wellbeing
and future disease risk. The Diabetes Care From Diagnosis Research
Team. British Medical Journal. 1998;317(7167):1202. Rec #: 2599
no usual care or comparable
control group
Kumana CR/Ma JT, Kung A, Kou M, Lauder I. An assessment of drug
information sheets for diabetic patients: Only active involvement by patients
is helpful. Diabetes Research and Clinical Practice. 1988;5:225-231. Rec
#: 2130
no glucose or weight outcomes
reported
Litzelman D K, Slemenda C W, Langefeld C D, Hays L M, Welch M A, Bild D E,
et al. Reduction of lower extremity clinical abnormalities in patients with
non-insulin-dependent diabetes mellitus. A randomized, controlled trial.
Ann Intern Med. 1993;119(1):36-41. Rec #: 828
no glucose or weight outcomes
reported
Mazzuca SA, Moorman NH, Wheeler ML, Norton JA, Fineberg NS, Vinicor F, et
al. The diabetes education study: A controlled trial of the effects of
diabetes patient education. Diabetes Care. 1986;9:1-10. Rec #: 2132
duplicate data (Vinicor, 1987)
Mulrow C, Bailey S, Sonksen PH, Slavin B. Evaluation of an audiovisual
diabetes education program: Negative results of a randomized trial of
patients with non-insulin dependent diabetes mellitus. Journal of General
Medicine. 1987;2:215-219. Rec #: 2266
no usual care or comparable
control group
Pratt C, Wilson W, Leklem J, Kingsley L. Peer support and nutrition education
for older adults with diabetes. Journal of Nutrition for the Elderly.
1987;6:37-43. Rec #: 2139
follow-up time not 3-12 months
Rabkin SW, Boyko E, Wilson A, Sreja DA. A randomized clinical trial comparing
behavior modification and individual counseling in the nutritional therapy of
non-insulin-dependent diabetes mellitus: comparison of the effect on blood
sugar, body weight, and serum lipids. Diabetes Care. 1983;6:50-56. Rec #:
2195
no usual care or comparable
control group
Rainwater N, Ayllon T, Frederiksen LW, Moore EJ, Bonar JR. Teaching selfmanagement skills to increase diet compliance in diabetics. In: Stewart RB
(Ed.). Adherence, Compliance and Generalization in Behavioral Medicine.
New York: Brunner/Mazel, 1982. pgs. 304-328. Rec #: 2140
no usual care or comparable
control group
48
Table 2. Articles Rejected from Meta-analysis
Reason for Exclusion
Rettig BA, Shrauger DG, Recker RP, Gallagher TF, Wiltse H. A randomised
study of the effects of a home diabetes education program. Diabetes Care.
1986;9:173-178. Rec #: 2270
no glucose or weight outcomes
reported
Sadur C N, Moline N, Costa M, Michalik D, Mendlowitz D, Roller S, et al.
Diabetes management in a health maintenance organization. Efficacy of
care management using cluster visits [In Process Citation]. Diabetes Care.
1999;22(12):2011-7. Rec #: 1668
not RCT
Stevens J, Burgess MB, Kaiser Dl, Sheppa CM. Outpatient management of
diabetes mellitus with patient education to increase carbohydrate and fiber.
Diabetes Care. 1985;8:359-366. Rec #: 2208
no usual care or comparable
control group
Vinicor F, Cohen S J, Mazzuca S A, Moorman N, Wheeler M, Kuebler T, et al.
DIABETES: a randomized trial of the effects of physician and/or patient
education on diabetes patient outcomes. J Chronic Dis. 1987;40(4):34556. Rec #: 892
follow-up time not 3-12 months
Ward WK, Haas LB, Beard JC. A randomized, controlled comparison of
instruction by a diabetes educator versus self-instruction in self-monitoring
of blood glucose. Diabetes Care. 1985;8:284-286. Rec #: 2152
no usual care or comparable
control group
Werdier JD, Jesdinsky HJ, Helmich P. A randomized controlled study on the
effect of diabetes counseling in the offices on 12 general practitioners. Rev
Epidemiol Med Sante Publique . 1984;32:225-229. Rec #: 2401
not RCT
Wheeler LA, Wheeler ML, Ours P, Swider C. Evaluation of computer-based diet
education in persons with diabetes mellitus and limited educational
background. Diabetes Care 1985;8(6):537-44. Rec #: 3442
follow-up time not 3-12 months
Wilson W, Pratt C . The impact of diabetes education and peer support upon
weight and glycemic control of elderly persons with non-insulin dependent
diabetes mellitus (NIDDM). Am J Public Health. 1987;77(5):634-5. Rec #:
900
duplicate data (Pratt, 1987)
Wing RR, Epstein LH, Nowalk MP, Koeske R, Hagg S. Behavior change,
weight loss and physiological improvements in Type II diabetic patients.
Journal of Consulting and Clinical Psychology. 1985;53:11-122. Rec #:
2156
no usual care or comparable
control group
Wing RR, Epstein LH, Nowalk MP, Scott N, Koeske R, Hagg S. Does selfmonitoring of blood glucose levels improve dietary compliance for obese
patients with Type II diabetes? the American Journal of Medicine.
1986;81:830-836. Rec #: 2158
no usual care or comparable
control group
Wing RR, Epstein LH, Nowalk MP, Scott N, Koeski R. Self-regulation in the
treatment of Type II diabetes. Behavior Therapy. 1988;19:11-23. Rec #:
2283
no usual care or comparable
control group
Wise PH, Dowlatshahi DC, Farrant S, Fromson SS/Meadows KA. Effect of
computer-based learning on diabetes knowledge and control. Diabetes
Care. 1986;9:504-508. Rec #: 2205
not RCT
Wood ER. Evaluation of a hospital-based education program for patients with
diabetes. Journal of the American Dietetic Association. 1989;89:354-358.
Rec #: 2159
not RCT
Worth R, Home PD, Johston DG, Anderson J, Ashworth L, Burrin JM, et al.
Intensive attention improves glycemic control in insulin-dependent diabetes
without further advantage from home glucose monitoring: results of a
controlled trial. BMJ. 1982;285:1233-1240. Rec #: 2198
no usual care or comparable
control group
49
Table 2. Articles Rejected from Meta-analysis
Reason for Exclusion
Osteoarthritis
Cohen J L, Sauter S V, deVellis R F, deVellis B M . Evaluation of arthritis selfmanagement courses led by laypersons and by professionals. Arthritis
Rheum. 1986;29(3):388-93. Rec #: 770
insufficient statistics
Doyle TH, Granada JL. Influence of two management approaches on the health
status of women with osteoarthritis. Arthritis and Rheumatism.
1982;25:S56. Rec #: 2427
no usual care or comparable
control group
Keefe F, Caldwell D, Baucom D, et al. Spouse-assisted coping skills training in
the management of osteoarthritis knee pain. Arthritis Care and Research.
1996;9:279. Rec #: 2082
no usual care or comparable
control group
Keefe F J, Caldwell D S, Williams D A, Gil K M, et al. Pain coping skills training
in the management of osteoarthritic knee pain: A comparative study.
Behavior Therapy. 1990b;21:49-62. Rec #: 908
duplicate populations (Keefe,
1990a)
Laborde JM, Powers MJ. Evaluation of education interventions for
osteoarthritics. Multiple Linear Reg Viewpoints. 1983;12:12-37. Rec #:
2355
insufficient statistics
Weinberger M, Tierney W M, Booher P, Katz B P . Can the provision of
information to patients with osteoarthritis improve functional status? A
randomized, controlled trial. Arthritis Rheum. 1989;32(12):1577-83. Rec #:
430
duplicate data (Weinberger,
1991)
Weinberger M, Tierney W M, Booher P, Katz B P . The impact of increased
contact on psychosocial outcomes in patients with osteoarthritis: a
randomized, controlled trial. J Rheumatol. 1991;18(6):849-54. Rec #: 898
insufficient statistics
50
Table 2. Articles Rejected from Meta-analysis
Reason for Exclusion
Post-Myocardial Infarction Care Articles
DeBusk RF, Miller NH, Superko HR, Dennis CA, Thomas RJ, Lew HT, et al. A
case-management system for coronary risk factor modification after acute
myocardial infarction [see comments]. Ann Intern Med. 1994;120(9):721-9.
Rec #: 775
no usual care or comparable
control group
Frasure-Smith N, Prince R . The ischemic heart disease life stress monitoring
program: impact on mortality. Psychosom Med. 1985;47(5):431-45. Rec #:
790
not RCT
Frasure-Smith N, Prince R. Long-term follow-up of the ischemic heart disease
life stress monitoring program. Psychosom Med. 1989;51:485-513. Rec #:
2218
not RCT
Friedman M, Thoresen C, Gill JJ, Ulmer DK. Feasibility of altering Type A
behavior pattern after myocardial infarction: Recurrent coronary prevention
project study: Methods, baseline results and preliminary findings.
Circulation. 1982;66:83-92. Rec #: 2367
not RCT
Friedman M, Thoresen CE, Gill JJ, et al. Alteration of Type A behavior and
reduction in cardiac recurrences in postmyocardial infarction patients. Am
Heart J. 1984;108:237-248. Rec #: 2362
no usual care or comparable
control group
Gruen W. Effects of brief psychotherapy during the hospitalization period on the
recovery process in heart attacks. J Consulting Clinical Psychology.
1975;43:223-232. Rec #: 2360
not RCT
Lewin B, Robertson I H, Cay E L, Irving J B, Campbell M . Effects of self-help
post-myocardial-infarction rehabilitation on psychological adjustment and
use of health services. Lancet. 1992;339(8800):1036-40. Rec #: 827
insufficient statistics
Miller NH, Haskell WL, Berra K et al. Home versus group exercise training for
increasing functional capacity after myocardial infarction. Circulation.
1984;4:645-649. Rec #: 2670
insufficient statistics
Oldenburg B, Allan R, Fastier G. The role of behavioral and educational
interventions in the secondary prevention of coronary heart disease. In P.F.
Lovibond & P.H. Wilson (Eds), Clinical and Abnormal Psychology
Proceedings of the XXIV International Congress of Psychology of the
International Union of Psychological Science. 1989:429-438. Rec #: 2698
insufficient statistics
Oldenburg B, Perkins RJ, Andrews G. Controlled trial of psychological
intervention in myocardial infarction. Journal of Consulting and Clinical
Psychology. 1985;53:852-859. Rec #: 2699
not RCT
Ott CR, Sivarajan ES, Newton KM et al. A controlled randomized study of early
cardiac rehabilitation: the Sickness Impact Profile as an assessment tool.
Heart Lung. 1983;12:162-170. Rec #: 2657
insufficient statistics
Payne T J, Johnson C A, Penzien D B, Porzelius J, Eldridge G, Parisi S, et al.
Chest pain self-management training for patients with coronary artery
disease. J Psychosom Res. 1994;38(5):409-18. Rec #: 859
not RCT
Powell LH, Friedman M, Thoresen CE, Gill JJ, Ulmer DK. Can the Type A
behavior pattern be altered after myocardial infarction? A second year
report from the Recurrent Coronary Prevention Project. Psychosom Med.
1984;46(4):293-313. Rec #: 2361
no usual care or comparable
control group
Schulte MB, Pluym B, Van Schendel G. Reintegration with duos: A self-care
program following myocardial infarction. Patients Education and
Counseling. 1986;8:233-244. Rec #: 2438
not RCT
51
Table 2. Articles Rejected from Meta-analysis
Reason for Exclusion
Sivarajan ES, Bruce RA, Lindskog BD, et al. Treadmill test responses to an
early exercise program after myocardial infarction: a randomized study.
Circulation. 1982;65:1420. Rec #: 3248
duplicate population (Froelicher,
1994)
Sivarajan ES, Newton KM, Almes MJ, et al. Limited effects of outpatient
teaching and counseling after myocardial infarction: A controlled study.
Heart and Lung. 1983;12:65-73. Rec #: 2439
insufficient statistics
Turner L, Linden W, van der Wal R, Schamberger W . Stress management for
patients with heart disease: a pilot study. Heart Lung. 1995;24(2):145-53.
Rec #: 887
no mortality or return to work
outcomes reported
Hypertension Articles
Irvine MJ, Johnson DW, Jenner DA, et al. Relaxation and stress management
in the treatment of essential hypertension. J of Psychosomatic Res.
1986;30:437-450. Rec #: 2458
no usual care or comparable
control group
Leveille SG, Wagner EH, Davis C, Grothaus L, Wallace J, LoGerfo M, et al.
Preventing disability and managing chronic illness in frail older adults: A
randomized trial of a community-based partnership with primary care.
JAGS. 1998;46(10):1-9. Rec #: 1175
insufficient statistics
Levine DM, Green LW, Deeds SG, Chwalow J, Russell RP, Finlay J. Health
education for hypertensive patients. JAMA 1979;241:1700-1703. Rec #:
3453
insufficient statistics
Martinez-Amenos A, Ferre LF, Vidal CM, Rocasalbas JA. Evaluation of two
educative models in a primary care hypertension programme. Journal of
Human Hypertension 1990;4:362-4. Rec #: 3457
insufficient statistics
Morisky DE, Levine DM, Green LW, Russell RP, Smith C, Benson P, et al. The
relative impact of health education for low- and high-risk patients with
hypertension. Prev Med 1980;9(4):550-8. Rec #: 3461
insufficient statistics
Morisky DE, Levine DM, Green LW, et al. Five-year blood pressure control and
mortality following health education for hypertensive patients. Am J Public
Health. 1983;73(2):153-162. Rec #: 2304
insufficient statistics
52
Hemoglobin
A1c
Blood
Glucose
D'Eramo-Melkus GA, Wylie-Rosett J, Hagan JA. Metabolic impact of education in NIDDM .
Diabetes Care. 1992;18:864-869. Rec #: 2202
Weight
Table 3. Diabetes articles Contributing to Meta-analysis
X
X
X
Falkenberg MG, Elwing BE, Goransson AM, Hellstrand BE, Riis UM. Problem oriented
participatory education in the guidance of adults with non-insulin-treated type II diabetes
mellitus. Scand J Prim Health Care. 1986;4:157-164. Rec #: 2190
X
Frost G, Wilding J, Beecham J . Dietary advice based on the glycemic index improves
dietary profile and metabolic control in type 2 diabetic patients. Diabet Med.
1994;11(4):397-401. Rec #: 791
X
Glasgow RE, Toobert DJ, Hampson SE, Brown JE, Lewinsohn PM, Donnelly J. Improving
self-care among older patients with type II diabetes: the "sixty something...." study.
Patient Educ Couns. 1992;19:61-74. Rec #: 2212
X
X
X
Greenfield S, Kaplan S H, Ware J E, Yano E M, Frank H J . Patients' participation in medical
care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med.
1988;3(5):448-57. Rec #: 803
X
Jaber LA Halapy H Fernet M et al. Evaluation of a pharmaceutical care model on diabetes
management. Annals of Pharmacotherapy. 1996;30(3):238. Rec #: 2598
X
Jennings PE, Morgan HC, Barnett AH. Improved diabetes control and knowledge during a
diabetic self-help group. The Diabetes Educator. 1987;13:390-393. Rec #: 2126
X
Korhonen T, Huttnen JK, Aro A, Hentinen M, Ihalainen O, Majander H, et al. A controlled trial
of the effects of patient education in the treatment of insulin dependent diabetes.
Diabetes Care. 1983;6:256-261. Rec #: 2259
X
X
Laitinen JH, Ahola IE, Sarkkinen ES, Winberg RL, Harmaakorpi-Ilvonen PA, Usitupa MI.
Impact of intensified dietary therapy on energy and nutrient intakes and fatty acid
composition of serum lipids in patients with recently diagnosed non-insulin-dependent
diabetes mellitus. J Am Diet Assoc. 1993;93:276-283. Rec #: 2176
X
X
McCulloch DK, Mitchell RD, Ambler J, Tattersall RB. Influence of imaginative teaching of diet
on compliance and metabolic control in insulin dependent diabetes. British Medical
Journal. 1983;28:1858-1861. Rec #: 2264
X
X
Raz I, Soskolne V, Stein P. Influence of small-group education sessions on glucose
homeostasis in NIDDM. Diabetes Care. 1988;11:67-71. Rec #: 2141
X
X
X
Vanninen E, Uuspitupa M, Siitonen O, Laitinen J, Lansimies E. Habitual physical activity,
aerobic capacity and metabolic control in patients with newly-diagnosed type 2 (noninsulin-dependent) diabetes mellitus: effect of 1-year diet and exercise intervention.
Diabetologia. 1992;35:340-346. Rec #: 2174
X
X
X
X
X
X
X
X
8
12
9
Weinberger M, Kirkman M S, Samsa G P, Shortliffe E A, Landsman P B, Cowper P A, et al.
A nurse-coordinated intervention for primary care patients with non- insulin-dependent
diabetes mellitus: impact on glycemic control and health-related quality of life [see
comments]. J Gen Intern Med. 1995;10(2):59-66. Rec #: 896
White N, Carnahan J, Nugent CA, Iwaoka T, Dodsono MA. Management of obese patients
with diabetes mellitus: comparison of advice education with group management.
Diabetes Care. 1986;9:490-496. Rec #: 2154
Total number of studies
53
X
Table 4. Osteoarthritis Articles Contributing to Meta-analysis
Barlow JH, Turner AP, Wright CC. A randomized controlled study of the Arthritis Self-Management Programme in
the UK. Health Educ Res. 2000;15(6):665-80. Rec #: 3274
Goeppinger J, Arthur M W, Baglioni A J, Brunk S E, Brunner C M . A reexamination of the effectiveness of self-care
education for persons with arthritis. Arthritis Rheum. 1989;32(6):706-16. Rec #: 801
Keefe F J, Caldwell D S, Williams D A, Gil K M, et al. Pain coping skills training in the management of osteoarthritic
knee pain-II: Follow-up results. Behavior Therapy. 1990a;21:435-447. Rec #: 907
Lorig K, Feigenbaum P, Regan C, Ung E, Chastain R L, Holman H R . A comparison of lay-taught and
professional-taught arthritis self- management courses. J Rheumatol. 1986;13(4):763-7. Rec #: 830
Lorig K, Lubeck D, Kraines R G, Seleznick M, Holman H R . Outcomes of self-help education for patients with
arthritis. Arthritis Rheum. 1985;28(6):680-5. Rec #: 835
Lorig K, Seleznick M, Lubeck D, Ung E, Chastain R L, Holman H R . The beneficial outcomes of the arthritis selfmanagement course are not adequately explained by behavior change. Arthritis Rheum. 1989;32(1):91-5. Rec
#: 837
Lorig K R, Sobel D S, Stewart A L, Brown Jr B W, Bandura A, Ritter P, et al. Evidence suggesting that a chronic
disease self-management program can improve health status while reducing hospitalization: A randomized trial.
Medical Care. 1999;37(1):5-14. Rec #: 608
Death
Return to
Work
All articles contributed both pain and function outcomes.
Burgess AW, Lerner DJ D'Agostino RB, Vokonas PS, Hartman CR, Gaccione P. A randomized
control trial of cardiac rehabilitation. Soc Sci Med. 1987;24:359-370. Rec #: 2652
X
X
DeBusk F, Haskell WL, Miller NN et al. Medically directed at-home rehabilitation soon after clinically
uncomplicated acute myocardial infarction: a new mode for patient care. Am J Cardio.
1985;85:251-257. (in MA for mortality only) Rec #: 2669
X
Dennis C, Houston-Miller N, Schwartz RG et al. Early return to work after uncomplicated myocardial
infarction. JAMA. 1988;260:214-220. Rec #: 2656
X
X
Froelicher E S, Kee L L, Newton K M, Lindskog B, Livingston M . Return to work, sexual activity,
and other activities after acute myocardial infarction. Heart Lung. 1994;23(5):423-35. Rec #:
792
X
X
Heller R F, Knapp J C, Valenti L A, Dobson A J . Secondary prevention after acute myocardial
infarction. Am J Cardiol. 1993;72(11):759-62. Rec #: 809
X
X
Horlick L, Cameron R, Firor W, et al . The effects of education and group discussion in the
postmyocardial infarction patient. J Psychosom Res. 1984;28:485-492. Rec #: 2219
X
X
Oldridge N, Guyatt G, Jones N. Effects of quality of life with comprehensive rehabilitation after
acute myocardial infarction. Am J Cardiol. 1991;67:1084-1089. Rec #: 2653
X
X
Rahe RM, Ward HW, Hayes V. Brief group therapy in myocardial infarction rehabilitation: Three to
four year follow-up of a controlled trial . Psychosom Med. 1979;41:229-242. Rec #: 2406
X
X
Stern MJ, Gorman PA, Kaslow . The group counseling vs. exercise therapy study: A controlled
intervention with subjects following myocardial infarction. Arch Intern Med. 1983;143:17191725. Rec #: 2377
X
X
9
8
Table 5. Post-Myocardial Infarction Care Articles Contributing to
Meta-analysis
Total number of studies
54
Table 6. Hypertension Articles Contributing to Meta-analysis
Blumenthal JA, Siegel WC, Appelbaum M . Failure of exercise to reduce blood pressure in patients with mild
hypertension. Results of a randomized controlled trial [see comments]. JAMA. 1991;266(15):2098-104. Rec
#: 752
Given C, Given B, Coyle B. The effects of patient characteristics and beliefs on responses to behavioral
interventions for control of chronic diseases. Pat Ed Counsel. 1984;6(3):131-140. Rec #: 2309
Goldstein IB, Shapiro D, et al. Comparison of drug and behavioral treatments of essential hypertension. Health
Psychology. 1982;1:7-26. Rec #: 2466
Gonzalez-Fernandez RA, Rivera M, Torres D, Quiles J, Jackson A. Usefulness of a systemic hypertension inhospital program. The American Journal of Cardiology 1990;65:1384-1386. Rec #: 3451
Hafner RJ. Psychological treatment of essential hypertension: A controlled comparison of meditation and
medication plus biofeedback. Biofeedback and Self-Regulation. 1982;7:305-315. Rec #: 2467
Hoelscher TJ, Lichstein KL, Fischer S, et al. Home relaxation practice in hypertension treatment: Objective
assessment and compliance induction. J of Consulting and Clinical Psychology. 1986;54:217-221. Rec #:
2457
Jacob RG, Fortmann SP, Kraemer HC, et al. Combining behavioral treatments to reduce blood pressure: A
controlled outcome study. Behavior Modification. 1985;9:32-45. Rec #: 2459
Jorgensen RS, Houston BK, Zurawski RM. Anxiety management training in the treatment of essential hypertension.
Behavior Research and Therapy. 1981;19:467-474. Rec #: 2452
Kostis JB, Rosen RC, Brondolo E, et al. Superiority of nonpharmacologic therapy compared to propranolol and
placebo in men with mild hypertension: A randomised prospective trial. American Heart Journal.
1992;123:466-474. Rec #: 2472
Lagrone R, Jeffrey TB, Ferguson CL. Effects of education and relaxation training with essential hypertension
patients. J of Clinical Psychology. 1988;44:271-276. Rec #: 2460
Muhlhauser I, Sawicki PT, Didjurgeit U, Jorgens V, Trampisch HJ, Berger M. Evaluation of a structured treatment
and teaching programme on hypertension in general practice. Clin Exp Hypertens 1993;15(1):125-42. Rec #:
3467
Southam MA, Agras WS, Taylor CB, et al. Relaxation training: Blood pressure lowering during the working day.
Archives of General Psychiatry. 1982;39:715-717. Rec #: 2453
Taylor CB, Farquhar JW, Nelson E, et al. Relaxation therapy and high blood pressure. Arch General Psychiatry.
1977;34:339-342. Rec #: 2464
Watkins CJ, Papacosta AO, Chinn S, Martin J. A randomized controlled trial of an information booklet for
hypertensive patients in general practice. J R Coll Gen Pract 1987;37(305):548-50. Rec #: 3469
All studies contributed to both systolic and diastolic blood pressure analyses.
55
RESULTS OF THE META-ANALYSES
Of the 14 questions posed by CMS, the following four could be most directly addressed
via meta-analyses. Theses four questions are related and their results are presented together.
Question 1. Do these programs work?
Question 2. Are there features that are generalizable across all diseases?
Question 6. What is the impact of chronic disease self-management programs on
quality of life, health status, health outcomes, satisfaction, pain, independence,
mental health (e.g., depression, emotional problems)?
Question 10. Is a generic self-management approach preferable to a disease-bydisease approach?
The responses to these questions are presented in this section, by condition, (Diabetes,
Osteoarthritis, Post-Myocardial Infarction Care and Hypertension). We then by report the results
as they address our five hypotheses, both within condition and across conditions.
Diabetes
There were 14 comparisons from 12 studies that reported hemoglobin A1c outcomes. In
an overall analysis of the effectiveness of chronic disease self-management programs, these
studies reported a statistically and clinically significant pooled effect size of -0.45 in favor of the
intervention (95% CI: (-0.26, -0.63); see Figure 6). The negative effect size indicates a lower
hemoglobin A1c in the treatment group as compared to the usual care or control group. An
effect size of –0.45 is equal to a reduction in hemoglobin A1c of about 1.0. For change in
weight, there were 10 comparisons from 8 studies. There was no statistically significant
56
difference between change in weight in the intervention and control groups (effect size of -0.05;
95% CI:(-0.12, 0.23); see Figure 8). There were 10 comparisons from 9 studies that reported
fasting blood glucose outcomes. The pooled effect size was -0.41 in favor of the intervention
(95% CI: (-0.23, -0.60); see Figure 10). This effect size equates to a drop in blood glucose of
1 mml/l.
Our assessment of publication bias (graphically depicted in funnel plots in Figures 7, 9,
and 11 and also presented in Table 7) revealed likely publication bias in studies reporting
hemoglobin A1c outcomes. Therefore, our results regarding efficacy of chronic disease selfmanagement programs for improving hemoglobin A1c must be interpreted with caution.
57
Figure 6. Forest Plot of Diabetes Studies: Hemoglobin A1c
D'Eramo-Melk(2202)
D'Eramo-Melk(2202)
Falkenberg(2190)
Glasgow(2212)
Greenfield(803)
Jaber(2598)
Jennings(2126)
Laitinen(2176)
McCulloch(2264)
McCulloch(2264)
Raz(2141)
Vanninen(2174)
Weinberger(896)
White(2154)
Combined
-2
-0.45
0
1
Effect Size
Favors Treatment
Favors Control
Figure 7. Funnel Plot of Diabetes Studies: Hemoglobin A1c
0.5
Effect Size
0
-0.5
-1
-1.5
0.00
0.20
Standard Error of Effect Size
58
0.40
Figure 8. Forest Plot of Diabetes Studies: Weight
D'Eramo-Melk(2202)
D'Eramo-Melk(2202)
Frost(791)
Glasgow(2212)
Laitinen(2176)
McCulloch(2264)
McCulloch(2264)
Raz(2141)
Vanninen(2174)
White(2154)
Combined
-1
- 0.05
1
Effect Size
Favors Treatment
Favors Control
Figure 9. Funnel Plot of Diabetes Studies: Weight
1
Effect Size
0.5
0
-0.5
-1
0.00
0.10
0.20
Standard Error of Effect Size
59
0.30
0.40
Figure 10. Forest Plot of Diabetes Studies: Fasting Blood Glucose
D'Eramo-Melk(2202)
D'Eramo-Melk(2202)
Frost(791)
Jaber(2598)
Korhonen(2259)
Laitinen(2176)
Raz(2141)
Vanninen(2174)
Weinberger(896)
White(2154)
Combined
-1.5
-0.41
0
0.5
Effect Size
Favors Treatment
Favors Control
Figure 11. Funnel Plot of Diabetes Studies: Fasting Blood Glucose
0.5
Effect Size
0
-0.5
-1
0.00
0.10
0.20
Standard Error of Effect Size
60
0.30
0.40
Table 7. Publication Bias for Diabetes Studies
# arms
Correlation
Test
(p-value)
# studies
Correlation
Test
(p-value)
Hemoglobin
14
0.016
0.006
12
0.011
0.008
Weight
10
0.210
0.079
8
0.108
0.090
Blood Glucose
10
0.210
0.136
9
0.118
0.177
Condition/
Outcome
Asymmetry
Test
(p-value)
61
Asymmetry
Test
(p-value)
Osteoarthritis
For both pain and function outcomes there were 10 comparisons from 7 different studies.
The pooled results of these chronic disease self-management programs did not yield any
statistically significant differences between intervention and control groups (pooled effect sizes
of -0.04 and -0.01 for pain and function respectively; see Figures 12 and 14).
Our assessment of publication bias depicted graphically in Figures 13 and 15 and Table 8
did not yield any evidence of publication bias.
62
Figure 12. Forest Plot of Osteoarthritis Studies: Pain
Barlow(3274)
Goeppinger(801)
Goeppinger(801)
Keefe(907)
Keefe(907)
Lorig(608)
Lorig(830)
Lorig(830)
Lorig(835)
Lorig(837)
Combined
-1
-0.04
1
Effect Size
Favors Treatment
Favors Control
Figure 13. Funnel Plot of Osteoarthritis Studies: Pain
Effect Size
0.5
0
-0.5
-1
0.00
0.10
0.20
Standard Error of Effect Size
63
0.30
Figure 14. Forest Plot of Osteoarthritis Studies: Functioning
Barlow(3274)
Goeppinger(801)
Goeppinger(801)
Keefe(907)
Keefe(907)
Lorig(608)
Lorig(830)
Lorig(830)
Lorig(835)
Lorig(837)
Combined
-1
-.01
1
Effect Size
Favors Treatment
Favors Control
Figure 15. Funnel Plot of Osteoarthritis Studies: Functioning
Effect Size
0.5
0
-0.5
0.00
0.10
0.20
Standard Error of Effect Size
64
0.30
Table 8. Publication Bias for Osteoarthritis Studies
Condition/
Outcome
Pain
Functioning
# arms
Correlation
Test
(p-value)
Asymmetry
Test
(p-value)
10
10
0.592
0.788
0.724
0.230
65
# studies
Correlation
Test
(p-value)
Asymmetry
Test
(p-value)
7
7
0.548
0.764
0.831
0.337
Post Myocardial Infarction Care
There were 9 studies that reported mortality outcomes. There was no effect of chronic
disease self-management programs on improving mortality (pooled relative risk 1.04; 95% CI:
(0.56, 1.95); see Figure 16). For return to work there were 10 comparisons from 8 studies. The
pooled relative risk did not show any difference between groups (relative risk 1.02; 95% CI:
(0.97, 1.08); see Figure 18).
Our assessment of publication bias (Funnel Plots 17 and 19, and Table 9) showed
evidence of publication bias for the mortality outcome but not the return to work outcome.
66
Figure 16. Forest Plot of Post-Myocardial Infarction Care Studies: Mortality
Burgess {2652}
Debusk {2669}
Dennis {2656}
Heller {809}
Horlick {2219}
Oldridge {2653}
Rahe {2406}
Sivarajan-Fr {792}
Stern {2377}
Combined
0.01
1.04
Risk Ratio - log scale
21
Figure 17. Funnel Plot of Post-Myocardial Infarction Care Studies: Mortality
4
Effect Size
2
0
-2
-4
0.0
0.5
1.0
Standard Error of Effect Size
67
1.5
Figure 18. Forest Plot of Post-Myocardial Infarction Care Studies: Return to Work
Burgess {2652}
Dennis {2656}
Heller {809}
Horlick {2219}
Oldridge {2653}
Rahe {2406}
Sivarajan-Fr {792}
Sivarajan-Fr {792}
Stern {2377}
Stern {2377}
Combined
0.01
1.02
100
Risk Ratio - log scale
Figure 19. Funnel Plot of Post-Myocardial Infarction Care Studies: Return to
Work
4
log Risk Ratio
Ri k R ti
2
0
-2
-4
0
0.5
1
Standard Error of log Risk Ratio
68
1.5
Table 9. Publication Bias for Post-Myocardial Infarction Care Studies
Condition/
Outcome
Mortality
Return to Work
# arms
Correlation
Test
(p-value)
Asymmetry
Test
(p-value)
15
0.012
0.005
10
1.000
0.450
69
# studies
Correlation
Test
(p-value)
Asymmetry
Test
(p-value)
9
0.076
0.087
8
0.902
0.641
Hypertension
For hypertension there were 23 comparisons from 14 studies that reported systolic and
diastolic blood pressure changes. The overall pooled result of the chronic disease selfmanagement programs was a statistically and clinically significant reduction in systolic and
diastolic blood pressure (effect size for systolic blood pressure -0.32; 95% CI: (-0.50, -0.15);
effect size for diastolic blood pressure -0.59; 95% CI: (-0.81, -0.38); see Figures 20 and 22). An
effect size of 0.32 is equivalent to a change in blood pressure of 3.5 mm of mercury, the
corresponding value for an effect size of 0.59 is 6.5 mm of mercury.
In our assessment of publication bias, (presented in Funnel Plots 21 and 23 and
Table 10), there was evidence of publication bias. Therefore our pooled result favoring chronic
disease self-management programs for hypertension must be viewed with caution.
70
Figure 20. Forest Plot of Hypertension Studies: Systolic Blood Pressure
Blumenthal {752}
Blumenthal {752}
Given {2309}
Goldstein {2466}
Goldstein {2466}
Goldstein {2466}
Gonzalez-Fer {3451}
Hafner {2467}
Hafner {2467}
Hoelscher {2457}
Hoelscher {2457}
Hoelscher {2457}
Jacob {2459}
Jorgensen {2452}
Kostis {2472}
Kostis {2472}
Lagrone {2460}
Lagrone {2460}
Muhlhauser {3467}
Southam {2453}
Taylor {2464}
Taylor {2464}
Watkins {3469}
Combined
-3.5
-0.32
0
1.5
Effect Size
Figure 21. Funnel Plot of Hypertension Studies: Systolic Blood Pressure
1
Effect Size
0
-1
-2
0.00
0.20
0.40
Standard Error of Effect Size
71
0.60
0.80
Figure 22. Forest Plot of Hypertension Studies: Diastolic Blood Pressure
Blumenthal {752}
Blumenthal {752}
Given {2309}
Goldstein {2466}
Goldstein {2466}
Goldstein {2466}
Gonzalez-Fer {3451}
Hafner {2467}
Hafner {2467}
Hoelscher {2457}
Hoelscher {2457}
Hoelscher {2457}
Jacob {2459}
Jorgensen {2452}
Kostis {2472}
Kostis {2472}
Lagrone {2460}
Lagrone {2460}
Muhlhauser {3467}
Southam {2453}
Taylor {2464}
Taylor {2464}
Watkins {3469}
Combined
-3.5
-0.59
0
1.5
Effect Size
Figure 23. Funnel Plot of Hypertension Studies: Diastolic Blood Pressure
1
Effect Size
0
-1
-2
0.00
0.20
0.40
Standard Error of Effect Size
72
0.60
0.80
Table 10. Publication Bias for Hypertension Studies
# arms
Correlation
Test
(p-value)
# studies
Correlation
Test
(p-value)
Systolic BP
20
0.074
0.077
11
0.008
0.021
Diastolic BP
20
0.074
0.045
11
0.043
0.017
Condition/
Outcome
Asymmetry
Test
(p-value)
73
Asymmetry
Test
(p-value)
Overall Analysis
For the three conditions that reported continuous outcomes (diabetes, osteoarthritis and
hypertension) we chose the one outcome from each study that we judged most clinically relevant
(hemoglobin A1c, pain, and systolic blood pressure, respectively) and used this to perform an
overall analysis of the efficacy of chronic disease self-management programs across conditions.
This analysis is shown in Figure 24, which contains 47 comparisons from 33 studies. The
overall pooled result is a statistically and clinically significant effect size favoring chronic
disease self-management programs of -0.26; 95% CI: (-0.36, -0.15).
Figure 24. Forest Plot of Pooled Studies
Barlow {3274}
Blumenthal {752}
Blumenthal {752}
D'Eramo-Melk {2202}
D'Eramo-Melk {2202}
Falkenberg {2190}
Given {2309}
Glasgow {2212}
Goeppinger {801}
Goeppinger {801}
Goldstein {2466}
Goldstein {2466}
Goldstein {2466}
Gonzalez-Fer {3451}
Greenfield {803}
Hafner {2467}
Hafner {2467}
Hoelscher {2457}
Hoelscher {2457}
Hoelscher {2457}
Jaber {2598}
Jacob {2459}
Jennings {2126}
Jorgensen {2452}
Keefe {907}
Keefe {907}
Kostis {2472}
Kostis {2472}
Lagrone {2460}
Lagrone {2460}
Laitinen {2176}
Lorig {608}
Lorig {830}
Lorig {830}
Lorig {835}
Lorig {837}
McCulloch {2264}
McCulloch {2264}
Muhlhauser {3467}
Raz {2141}
Southam {2453}
Taylor {2464}
Taylor {2464}
Vanninen {2174}
Watkins {3469}
Weinberger {896}
White {2154}
Combined
-3.5
-0.26
Effect Size
74
0
1.5
Figure 25. Funnel Plot of Pooled Studies
Effect Size
1
0
-1
-2
0.00
0.20
0.40
0.60
Standard Error of Effect Size
0.80
Tests of hypothesis of elements essential to chronic disease self-management efficacy
Tables 11 through 14 present the results of our analysis looking at the five hypotheses
regarding the elements contributing to the effectiveness of chronic disease self-management
programs. Other than the increased effectiveness seen in hypertension studies reporting systolic
blood pressure outcomes that used tailored interventions, there were no statistically significant
differences between interventions with or without the 5 features hypothesized to be related to
effectiveness (tailoring, use of group setting, feedback, psychological component, and MD care).
Indeed, many of the effects seen are inconsistent across outcomes within the same condition.
For example, in hypertension studies, for hypothesis 2 (use of a group setting), there is a greater
than 50% increase in the effect size for improvement in systolic blood pressure, but only a 5%
increase in the effect size for improvement in diastolic blood pressure (note that neither result is
75
statistically significant). In other situations, the effect actually goes the opposite way (for
example, hypothesis 4, the use of a psychological component, shows opposite effects in studies
of diabetes depending on whether hemoglobin A1c or fasting blood glucose is used as the
outcome).
Our "across condition" analysis, presented in Table 15 shows effect sizes that, in general,
go in the direction of supporting increased effectiveness associated with the use of these
intervention features, however none of the differences are statistically significant.
Table 11. Meta-Analysis Results for Diabetes
Outcome
Overall
Tailored
No
Yes
Group Setting
No
Yes
Feedback
No
Yes
Psychological
No
Yes
MD Care
No
Yes
Hemoglobin A1c
Weight
Fasting blood glucose
(N = 12)
(N = 8)
(N = 9)
effect size
effect size
effect size
# comparisons
(95% CI)
# comparisons
(95% CI)
# comparisons
(95% CI)
14
-0.45
10
-0.05
10
-0.41
(-0.63, -0.26)
(-0.23, 0.12)
(-0.60, -0.23)
1
-0.32
1
0.0
1
-0.81
(-1.05, 0.41)
(-0.56, 0.56)
(-1.42, -0.20)
13
-0.46
9
-0.06
9
-0.37
(-0.66, -0.26)
(-0.24, 0.12)
(-0.55, -0.19)
4
-0.50
2
-0.05
4
-0.38
(-0.83, -0.18)
(-0.39, 0.30)
(-0.68, -0.09)
10
-0.42
8
-0.05
6
-0.46
(-0.66, -0.18)
(-0.25, 0.15)
(-0.74, -0.18)
4
-0.26
3
0.10
2
-0.42
(-0.58, 0.07)
(-0.18, 0.38)
(-0.90, 0.06)
10
-0.52
7
-0.15
8
-0.42
(-0.73, -0.30)
(-0.38, 0.07)
(-0.65, -0.20)
8
-0.48
5
-0.09
5
-0.37
(-0.74, -0.22)
(-0.36, 0.18)
(-0.63, -0.11)
6
-0.42
5
-0.02
5
-0.49
(-0.71, -0.12)
(-0.25, 0.20)
(-0.80, -0.18)
13
-0.45
9
-0.04
8
-0.48
(-0.66, -0.25)
(-0.22, 0.15)
(-0.70, -0.27)
1
-0.43
1
-0.14
2
-0.20
(-1.08, 0.21)
(-0.59, 0.30)
(-0.58, 0.18)
Overall Chi-squared p-value
0.081
0.942
N = number of studies contributing data; CI = confidence interval; NE = not estimable
76
0.195
Table 12. Meta-Analysis Results for Osteoarthritis
Pain
(N = 7)
Outcome
# comparisons
Overall
Tailored
Group Setting
Feedback
Psychological
MD Care
10
No
0
Yes
10
No
1
Yes
9
No
4
Yes
6
No
3
Yes
7
No
Yes
effect size
(95% CI)
-0.04
(-0.11, 0.04)
NE
Functioning
(N = 7)
effect size
# comparisons
(95% CI)
10
0
-0.01
(-0.09, 0.07)
NE
10
10
NE
0.10
(-0.14, 0.34)
-0.05
(-0.13, 0.02)
-0.04
(-0.17, 0.10)
-0.04
( -0.12, 0.05)
0.04
(-0.13, 0.20)
-0.05
( -0.14, 0.03)
NE
10
NE
0.17
(-0.06, 0.41)
-0.03
(-0.11, 0.04)
0.01
(-0.13, 0.16)
-0.01
( -0.11, 0.08)
0.10
(-0.07, 0.26)
-0.04
(-0.12, 0.04)
NE
0
NE
0
NE
1
9
4
6
3
7
Overall Chi-squared p-value
0.243
0.532
N = number of studies contributing data; CI = confidence interval; NE = not estimable
77
Table 13. Meta-Analysis Results for Post-Myocardial Infarction Care
Mortality
(N = 9)
Outcome
# comparisons
Overall
9
Tailored
No
Yes
9
Group Setting
No
5
Yes
6
No
4
Yes
6
No
4
Yes
7
No
8
Yes
1
Feedback
Psychological
MD Care
0
risk ratio
(95% CI)
Return to Work
(N = 8)
risk ratio
# comparisons
(95% CI)
1.04
(0.56, 1.95)
NE
10
NE
1.22
(0.54, 2.79)
0.81
(0.32, 2.05)
1.01
(0.34, 3.20)
1.03
(0.48, 2.23)
1.81
(0.68, 5.35)
0.69
(0.31, 1.54)
1.09
(0.57, 2.10)
0.52
(0.01, 9.90)
10
Overall Chi-squared p-value
0
4
6
4
6
4
6
9
1
1.02
(0.97, 1.08)
NE
NE
1.02
(0.95, 1.11)
1.01
(0.92, 1.11)
0.91
(0.81, 1.02)
1.05*
(1.00, 1.11)
0.97
(0.88, 1.07)
1.05
(0.98, 1.13)
1.01
(0.95, 1.08)
1.07
(0.94, 1.22)
0.30
0.035
N = number of studies contributing data; CI = confidence interval; NE = not estimable
* "yes" is statistically significant as compared to "no" (p<0.05)
78
Table 14. Meta-Analysis Results for Hypertension
Systolic BP
(N = 14)
effect size
# comparisons
(95% CI)
Outcome
Overall
Tailored
23
Yes
15
No
23
-0.32
(-0.50, -0.15)
-0.08
(-0.33, 0.16)
-0.41*
(-0.59, -0.22)
-0.20
(-0.46, 0.06)
-0.41
(-0.65, -0.18)
-0.26
(-0.49, -0.02)
-0.40
(-0.67, -0.14)
-0.25
(-0.50, 0.00)
-0.38
(-0.62, -0.14)
NE
Yes
0
NE
No
6
Yes
17
Group Setting No
Feedback
Yes
13
No
13
Yes
10
Psychological No
MD Care
10
8
Diastolic BP
(N = 14)
effect size
# comparisons
(95% CI)
23
23
-0.59
(-0.81, -0.38)
-0.41
(-0.78, -0.03)
-0.67
(-0.92, -0.42)
-0.54
(-0.87, -0.21)
-0.64
(-0.94, -0.35)
-0.56
(-0.85, -0.26)
-0.65
(-0.98, -0.32)
-0.44
(-0.76, -0.12)
-0.70
(-0.98, -0.42)
NE
0
NE
6
17
10
13
13
10
8
15
Overall Chi-squared p-value
0.008
0.000
N = number of studies contributing data; CI = confidence interval; NE = not estimable
* "yes" is statistically significant as compared to "no" (p<0.05)
79
Table 15. Meta-Analysis Results Pooled Across Conditions
Pain, Hemoglobin A1c, Systolic
(N = 30)
effect size
# comparisons
(95% CI)
Outcome
Overall
Tailored
Group Setting
Feedback
Psychological
MD Care
47
No
7
Yes
40
No
15
Yes
32
No
21
Yes
26
No
19
Yes
28
No
46
Yes
1
-0.26
(-0.36, -0.15)
-0.14
(-0.42, 0.13)
-0.28
(-0.39, -0.16)
-0.26
(-0.46, -0.07)
-0.26
(-0.38, -0.13)
-0.16
(-0.32, 0.00)
-0.32
(-0.46, -0.18)
-0.27
(-0.43, -0.11)
-0.25
(-0.39, -0.11)
-0.25
(-0.36, -0.15)
-0.43
(-1.09, 0.22)
Adjusted
effect size
(95% CI)
NA
NA
-0.21
(-0.53, 0.12)
NA
-0.16
(-0.45, 0.14)
NA
-0.27
(-0.69, 0.15)
NA
-0.08
(-0.51, 0.34)
NA
-0.23
(-0.99, 0.54)
Overall Chi-squared p-value
0.000
NA
N = number of studies contributing data; CI = confidence interval; NE = not estimable
Adjusted effect size is adjusted for all components simultaneously
80
Post Hoc Analyses
Components of CDSM according to RE-AIM
The components of CDSM can be classified using RE-AIM as:
x one-on-one counseling interventions (individual)
x group sessions (group)
x telephone calls (telephone)
x interactive computer-mediated interventions (computer)
x mail interventions (mail)
x health system policies (policy 1 and policy 2)
The results of the meta-regression analyses are presented in Tables 16-20. With few
exceptions, there were no results that were statistically significant. An exception is the result for
the use of one-on-one counseling sessions, which did show a statistically significant increased
effect size when used. “Policy 1” is the variable we constructed using a strict definition of health
system policies, while “Policy 2” uses a broad definition of health system policies.
81
Table 16. Meta-Analysis Results for Diabetes (RE-AIM Model)
Outcome
Overall
Individual
No
Yes
Group
No
Yes
Telephone
No
Yes
Hemoglobin
Weight
(N = 12)
(N = 8)
effect size
effect size
# comparisons
(95% CI) # comparisons (95% CI)
-0.45
-0.05
14
10
(-0.63, -0.26)
(-0.23, 0.12)
-0.23
0.0
6
3
(-0.44, -0.02)
(-0.29, 0.29)
-0.60*
-0.08
8
7
(-0.83, -0.38)
(-0.30, 0.13)
-0.54
-0.05
6
3
(-0.82, -0.27)
(-0.36, 0.27)
-0.36
-0.05
8
7
(-0.62, -0.10)
(-0.26, 0.15)
-0.48
13
10
NE
(-0.68, -0.28)
-0.23
1
0
NE
(-0.74, 0.29)
14
NE
10
NE
Blood Glucose
(N = 9)
effect size
# comparisons
(95% CI)
-0.41
10
(-0.60, -0.23)
-0.55
3
(-0.89, -0.20)
-0.36
7
(-0.60, -0.11)
-0.38
4
(-0.68, -0.09)
-0.46
6
(-0.74, -0.18)
-0.44
9
(-0.67, -0.22)
-0.32
1
(-0.78, 0.13)
10
NE
Computer
No
Yes
0
NE
0
NE
0
NE
Mail
No
14
NE
10
NE
10
NE
Yes
0
0
NE
0
No
13
10
NE
9
Yes
1
0
NE
1
No
13
10
NE
9
Yes
1
NE
-0.48
(-0.68, -0.28)
-0.23
(-0.74, 0.29)
-0.48
(-0.68, -0.28)
-0.23
(-0.74, 0.29)
0
NE
1
NE
-0.44
(-0.67, -0.22)
-0.32
(-0.78, 0.13)
-0.44
(-0.67, -0.22)
-0.32
(-0.78, 0.13)
Policy 1
Policy 2
0.081
0.942
N = number of studies contributing data; CI = confidence interval; NE = not estimable
* "yes" is statistically significant as compared to "no" (p<0.05)
82
0.195
Table 17. Meta-Analysis Results for Osteoarthritis (RE-AIM Model)
Pain
(N = 7)
Outcome
# comparisons
Overall
Individual
Group
Telephone
Computer
Mail
Policy 1
Policy 2
10
No
10
Yes
0
No
1
Yes
9
No
8
Yes
2
No
10
Yes
0
No
9
Yes
1
No
9
Yes
1
No
9
Yes
1
effect size
(95% CI)
-0.04
(-0.11, 0.04)
NE
NE
-0.67
(-1.20, -0.14)
-0.02*
( -0.10, 0.05)
-0.03
(-0.10, 0.05)
-0.32
( -0.68, 0.05)
NE
NE
-0.05
(-0.13, 0.02)
0.10
( -0.14, 0.34)
-0.03
(-0.12, 0.06)
-0.06
( -0.19, 0.07)
-0.03
(-0.12, 0.06)
-0.06
( -0.19, 0.07)
Functioning
(N = 7)
effect size
# comparisons
(95% CI)
-0.01
10
(-0.09, 0.07)
10
NE
0
1
9
8
2
10
0
9
1
9
1
9
1
NE
0.06
(-0.46, 0.59)
-0.01
(-0.09, 0.08)
-0.01
(-0.10, 0.07)
0.17
( -0.20, 0.53)
NE
NE
-0.03
(-0.11, 0.04)
0.17
(-0.06, 0.41)
0.03
(-0.05, 0.12)
-0.12*
(-0.25, 0.01)
0.03
(-0.05, 0.12)
-0.12*
(-0.25, 0.01)
Chi-squared p-value
0.243
0.532
N = number of studies contributing data; CI = confidence interval; NE = not estimable
* "yes" is statistically significant as compared to "no" (p<0.05)
83
Table 18. Meta-Analysis Results for Post-Myocardial Infarction Care
(RE-AIM Model)
Outcome
Overall
Individual
No
Yes
Group
No
Yes
Telephone
No
Yes
Computer
Mail
Policy 1
Policy 2
No
Return to Work
(N = 8)
risk ratio
# comparisons
(95% CI)
1.02
10
(0.97, 1.08)
0.97
5
(0.89, 1.06)
1.05
5
(1.00, 1.11)
1.03
5
(0.95, 1.11)
1.01
5
(0.92, 1.11)
1.00
9
(0.95, 1.08)
1.07
1
(0.94, 1.22)
10
NE
Yes
0
No
7
Yes
3
No
10
NE
1.03
(0.95, 1.11)
1.01
(0.92, 1.11)
NE
Yes
0
NE
No
10
NE
Yes
0
NE
Chi-squared p-value
0.035
N = number of studies contributing data; CI = confidence interval; NE = not estimable
NA = not applicable
Note: it was not possible to perform this analysis for the outcome “mortality”.
84
Table 19. Meta-Analysis Results for Hypertension (RE-AIM Model)
Outcome
Overall
Individual
No
Yes
Group
No
Yes
Telephone
No
Yes
Systolic BP
(N = 14)
effect size
# comparisons
(95% CI)
-0.32
23
(-0.50, -0.15)
-0.32
17
(-0.53, -0.12)
-0.33
6
(-0.70, 0.05)
-0.21
15
(-0.42, -0.01)
-0.48
8
(-0.76, -0.21)
-0.32
22
(-0.50, -0.14)
-0.42
1
(-1.39, 0.54)
23
NE
Diastolic BP
(N = 14)
effect size
# comparisons
(95% CI)
-0.59
23
(-0.81, -0.38)
-0.64
17
(-0.79, -0.30)
-0.75
6
(-1.19, -0.31)
-0.51
15
(-0.78, -0.24)
-0.75
8
(-1.12, -0.38)
-0.57
22
(-0.79, -0.35)
-1.24
1
(-2.38, -0.10)
23
NE
Computer
No
Yes
0
NE
0
NE
Mail
No
23
NE
23
NE
Yes
0
0
No
20
Yes
3
No
20
Yes
3
NE
-0.40
(-0.55, -0.17)
-0.06
(-0.57, 0.46)
-0.40
(-0.55, -0.17)
-0.06
(-0.57, 0.46)
NE
-0.63
(-0.86, -0.39)
-0.38
(-0.99, 0.24)
-0.63
(-0.86, -0.39)
-0.38
(-0.99, 0.24)
Policy 1
Policy 2
20
3
20
3
Chi-squared p-value
0.008
0.006
N = number of studies contributing data; CI = confidence interval; NE = not estimable
85
Table 20. Meta-Analysis Results Pooled Across Conditions (RE-AIM Model)
Outcome
Overall
Individual
No
Yes
Group
No
Yes
Telephone
No
Yes
Computer
Mail
Policy 1
Policy 2
No
Pain, Hemoglobin A1c, Systolic
(N = 30)
# comparisons
effect size
-0.26
47
(-0.36, -0.15)
-0.14
33
(-0.23, -0.05)
-0.51*
14
(-0.70, -0.32)
-0.35
22
(-0.51, -0.19)
-0.18
25
(-0.31, -0.05)
-0.25
43
(-0.37, -0.14)
-0.30
4
(-0.65, 0.04)
47
NE
Yes
0
No
46
Yes
1
No
42
Yes
5
No
42
Yes
5
NE
-0.27
(-0.37, -0.16)
0.10
(-0.41, 0.61)
-0.28
(-0.39, -0.17)
-0.10
(-0.40, 0.20)
-0.28
(-0.39, -0.17)
-0.10
(-0.40, 0.20)
Adjusted
effect size
NE
NE
-0.54*
(-0.75, -0.34)
NE
-0.15
(-0.26, -0.03)
NE
-0.34
(-0.65, -0.04)
NE
NE
NE
0.03
(-0.39, 0.45)
NE
-0.07
(-0.35, 0.20)
excluded from
model
Chi-squared p-value
0.000
N = number of studies contributing data; CI = confidence interval; NE = not estimable
* "yes" is statistically significant as compared to "no" (p<0.05)
Adjusted effect size is adjusted for all components simultaneously
86
Effectiveness of CDSM According to Baseline Severity
We were able to perform the meta-analysis according to baseline severity for
hemoglobin A1c and weight outcomes in diabetes, and pain and function for osteoarthritis. For
hemoglobin A1c, a study’s sample was considered more severe if the mean baseline hemoglobin
value was greater than or equal to 10%. Seven out of the 12 studies were considered more
severe, which provided 9 comparisons. For weight, severity was assigned to studies with a mean
baseline weight of greater than 185 lbs or 84.1 kgs, or BMI greater than 30 kg/m2. Six of the 8
weight studies were categorized as “more severe” which provided seven comparisons. For the
pain outcome, a study had a more severe patient sample if the mean baseline pain value was
greater than 5 on a 0-10 or 0-15 Visual Analogue Scale or on the AIMs pain scale. Four of the
six pain studies were rated as “more severe” which provided 6 comparisons. A sample was
considered more severe for the functioning outcome if the baseline mean was greater than one on
the HAQ (0-3). One of the six studies was considered “more severe” which provided one
comparison. Effect sizes were then compared between studies of “more severe” and “less
severe” patients at baseline. Only the assessment of hemoglobin A1c demonstrated an increased
effect size in patients who were more severely effected, and this difference did not quite reach
conventional levels of statistical significance.
87
Table 21. Meta-analysis Results for Diabetes (Severity Model)
Hemoglobin A1c
Weight
(N = 12)
(N = 8)
effect size
effect size
Level
# comparisons
(95% CI)
# comparisons
(95% CI)
-0.55
-0.04
More Severe
9
7
(-0.79, -0.31)
(-0.42, 0.35)
-0.29
-0.06
Less Severe
5
3
(-0.57, -0.01)
(-0.25, 0.14)
N = number of studies contributing data; CI = confidence interval; NE = not estimable
Table 22. Meta-analysis Results for Osteoarthritis (Severity Model)
Pain
(N = 6)
Functioning
(N = 6)
effect size
effect size
Level
# comparisons
(95% CI)
# comparisons
(95% CI)
-0.04
-0.02
More Severe
6
1
(-0.14, 0.05)
(-0.11, 0.08)
-0.03
0
Less Severe
4
9
(-0.14, 0.08)
(-0.20, 0.20)
N = number of studies contributing data; CI = confidence interval
88
Effectiveness of CDSM Program Components According to the “Essential Elements of Selfmanagement Interventions”
For the “Essential Elements of Self-management Interventions” evaluation, we did not
find as much variation among studies and components as is necessary for optimal power in the
analysis. Most of the studies scored positively for “problem identification and solving,” and did
not score positively for the “ensuring implementation component.” Given these data, we did not
find evidence to support either any one of these three broad “essential elements” as necessary,
nor some threshold (such as two out of three) in terms of efficacy. This was not an optimal test
of these hypotheses due to the lack of variation in the data.
Table 23. Meta-analysis Results Pooled Across Conditions
(“Essential Elements” Model)
Pain, Hemoglobin A1c, Systolic
(N = 30)
Adjusted
# comparisons
effect size
effect size
-0.24
Problem
No
8
NE
(-0.47, 0)
-0.26
-0.27
Yes
39
(-0.38, -0.14)
(-0.46, -0.09)
-0.27
Support
No
28
NE
(-0.41, -0.13)
-0.24
-0.20
Yes
19
(-0.41, -0.08)
(-0.54, 0.14)
-0.25
Track
No
44
NE
(-0.35, -0.14)
-0.38
-0.35
Yes
3
(-0.76, 0.01)
(-0.84, 0.13)
N = number of studies contributing data; CI = confidence interval; NE = not estimable
Adjusted effect size is adjusted for all three components simultaneously
Outcome
89
Effectiveness According to Intermediate Variables
Figures 26 and 27 present graphical representations of the correlation between
“intermediate” variable 1 and variable 2, and between variable 2 and outcome. Figure 26 shows
that the correlation between intermediate variables 1 and 2 is strongly effected by outliers.
Including two outlier values actually produces a negative correlation, meaning that
improvements in intermediate variable 1 (such as self-efficacy, patient knowledge, and
psychological measures) actually is associated with worsening values for intermediate 2
variables (such as dietary measures, physical activity, and behavioral measures). Ignoring the
two outlier values yields a correlation in the expected direction. Figure 27 shows that the
correlation of intermediate 2 on outcome is weak but in the expected direction.
90
Figure 26. Regression of Intermediate 2 on Intermediate 1
91
Figure 27. Regression of Outcome on Intermediate 2
92
Question 3. Does this intervention belong in the medical care system?
Whether chronic disease self-management belongs in the medical care system or in the
community is a decision that needs to be made by policy makers, based on many factors. That
being said, one of the first hypotheses we tested was whether patients who receive interventions
directly from their medical providers are more likely to have better outcomes than those who
received interventions from non-medical providers. Of the controlled studies that made it into
our meta-analysis, no studies of osteoarthritis or hypertension used medical providers in their
self-management interventions. Regarding diabetes, one intervention used medical providers; the
results of this intervention were not significantly different than those using lay leaders (see
Table 11). One post-myocardial infarction intervention used medical providers; the effects on
mortality and return to work were not statistically different from those of the other interventions.
Question 4. Define chronic disease self-management and distinguish between it
and disease management.
There is no standard definition of chronic disease self-management. For purposes of this
review, we initially defined chronic disease self-management broadly as a systematic
intervention that is targeted towards patients with chronic disease to help them to actively
participate in either or both of the following activities: self monitoring (of symptoms or
physiologic processes) or decision-making (managing the disease or its impact based on selfmonitoring). Our analytic attempts to “define” chronic disease self-management by identifying
the components most responsible for the success of the program were unsuccessful.
The draft evidence report was presented to a group of experts in chronic disease selfmanagement at a meeting convened by the Robert Wood Johnson Foundation and held in Seattle
93
on December 14, 2001. The list of experts attending is present in Appendix A. The panel’s aim
was to focus on interventions offered to patients who need a more intense level and type of selfmanagement support. They agreed that all self-management programs should address the
following three areas.
Disease, medication and health management. While patients need medical information
about their particular disease (diabetes, arthritis, asthmas, etc.), the majority of the content in
most successful self-management programs emphasized generic lifestyle issues such as exercise,
nutrition, and coping skills. More disease-specific medication-specific information can be useful,
but such information rarely constitutes more than 20 percent of the content of programs.
Role management. Patients benefit from programs that help them maintain social
support, connection to work and family, and normal functions of daily life.
Emotional management. Programs should encompass managing depression and stress,
adaptation to change, and maintaining interpersonal relationships.
A monograph authored by Dr. Jesse Gruman (Center for the Advancement of Health,
2002) summarized the discussions from the meeting of December 14, 2001. The experts
concluded that the essential elements of self-management programs should include the
following:
1. Problem-solving training that encourages patients and providers to identify problems,
identify barriers and supports, generate solutions, form an individually tailored action
plan, monitor and assess progress toward goals, and adjust the action plan as needed.
94
2. Follow-up to maintain contact and continued problem-solving support, to identify
patients who are not doing well and assist them in modifying their plan, and to relate
the plan to the patient’s social/ cultural environment.
3. Tracking and ensuring implementation by linking the program to the patient’s regular
source of medical care and by monitoring the effects of the program on the patient’s
health, satisfaction, quality of life, and health system quality measures.
The experts also recommended that any chronic disease self-management program be
composed of two tiers to accommodate the wide variety of patients with chronic conditions. The
first tier would include a low-intensity intervention designed to reach mass audiences and open
to anybody with a particular illness. The second tier would include a high-intensity intervention
targeted to people who require one-on-one support and case management. This program could
be offered to those who have not successfully managed their condition with the minimal support
of tier #1, those who have complicated conditions, and those whose life circumstances or
conditions change significantly.
Question 5. What is the role or potential of technology?
The advent of new technologies makes communication between patients, providers, and
others more convenient than ever. However, none of the randomized controlled studies on
chronic disease self-management used email or the Internet. Thus, we were not able to
quantitatively assess the impact of these technologies. Still, incorporating these technologies into
future randomized studies would be a worthwhile endeavor.
None of the randomized controlled trials of programs for arthritis, hypertension, or postmyocardial infarction involved patient use of computer programs. However, diabetes self-
95
management programs have utilized computer programs since the late 1970s. Randomized
controlled trials are discussed below.
The DIABEDS study, conducted from 1978 to 1982 at University of Indiana, used
computers to generate diet menus and physician reminders.35, 36 Over 500 patients were assigned
to either routine care, patient education, physician education, or both physician and patient
education. At two-year follow-up, the combination of patient plus physician education resulted in
the greatest improvements in fasting plasma glucose, hemoglobin A1C, body weight, and
diastolic blood pressure. A small substudy was conducted at the university on computer-based
techniques for diet education and meal planning.37 Sixteen inner city, low SES patients received
computer-assisted instruction combined with an interactive videodisc system. They also received
face-to-face education from a dietitian. The computer –assisted instruction was operated entirely
by the patient, who answered questions by pressing on of three color-coded keys on the
keyboard. At four-week follow-up the group had lost an average of 4.6 pounds (p<0.005) and
reduced their reported fat intake (p<0.05).
Scientists in the U.K. also designed and evaluated two interactive computer based
diabetes education tools in the early 1980s.38 One was a teaching program with animated
graphics, while the other was a multiple choice knowledge assessment with optional prescriptive
feedback. Each program used questioning after each provision of fact, followed by optional or
compulsory rerun of the fact sequence if inadequate performance was recorded. Patients could
progress through the programs at their own rate. In a controlled trial, the programs led to an
increase in knowledge and a decrease in Hemoglobin A1c levels.
More recently, Glasgow and colleagues developed a single session MD office-based
intervention for diabetics using a brief touchscreen computer assessment that provided
96
individualized feedback to both providers and patients.39 The feedback took the form of a report
on key barriers to dietary self-management, along with goal setting and problem-solving
counseling. At three-month follow-up, intervention patients had lowered mean serum
cholesterol from 216 to 207, while patients in the usual care group actually increased total
cholesterol from 223 to 231 (p<0.001). In addition, intervention patients had larger decreases in
percent of calories from fat (p<0.008). Differences remained significant at twelve months.40
Recently, Lorig and colleagues reported the results of an “email discussion group” for
patients with back pain.41 While not one of our conditions of interest, and also not assessing
older individuals (mean age of study subjects was 45 years), the results are the first we have
found to assess the use of internet technology in patient management of a chronic illness. The
“email discussion group” participants received an educational book and videotape about back
pain, and had access to an email listserve where subjects could post questions or comments about
their illness. The “email discussion group” was moderated by content experts who answered
(non-participant specific) questions about back pain. The authors report that at one year subjects
in the “email discussion group” had, compared to controls that received a magazine subscription,
modest improvements in measures of self-efficacy, self-care orientation, pain interference, and
health related quality of life, and about one less physician visit for back pain over the past year.
This study suggests that email and the Internet may be a promising method for delivering selfcare interventions.
97
Question 7. To what extent does self-management educate a patient on how to
care for himself/herself (e.g., take medications appropriately, consult with a
physician when necessary, etc.)?
Most CDSM studies that assess knowledge and self-efficacy reported beneficial
improvements. Most studies did NOT measure whether medications were taken appropriately or
“necessary” physician visits were made. The two studies that did assess compliance were
hypertension studies. One had a borderline beneficial overall result; the other reported a
significant beneficial result. One study was based on a conceptual model that specifically
considered that changing medication-taking behavior was going to be easier than changing diet
behavior or other such behaviors. This study did not actually measure compliance, but rather
measured “commitment to taking medications” and showed that this differed between
intervention and controls and that it was one of only three variables among those tested to be
associated with significant changes in blood pressure (the other two were “”belief in severity of
the disease” and “beliefs in efficacy of therapy”). Many studies assessed utilization, but none
assessed whether the utilization was necessary.
Question 8. What is the patient’s retention of self-management skills after the
intervention? Is a follow-up intervention needed at some point?
The best way to answer this question would be to review clinical trials where one arm
receives a “follow-up intervention” and another does not. No such studies were found. Failing
this, we could compare the results of studies that included a “follow-up intervention” with
studies that did not. Again, we were unable to find studies that actually included a “follow-up
intervention” which incorporated refresher skills on self-management. In light of this, we used a
meta-regression model to test whether self-management interventions that provide follow-up
98
support led to better results than those that did not. We classified interventions that maintained
contact with the patient through contracts, provider feedback, reminders, peer support, material
incentives, or home visits as including “follow-up support.” Of the interventions which could be
included in our meta-analyses, 19 had “follow-up support” while 28 did not. Pooled results were
not statistically different between the two groups.
Question 9. How does the approach for self-management differ for people with
multiple chronic diseases?
We found no evidence on this topic.
Question 11. Should this intervention be targeted to a subset of the population or
available to everyone? Are there particular chronic conditions that should be
addressed (e.g., diabetes, arthritis, stroke, cancer, Parkinson’s, hypertension,
dyslipidemia)?
We were able to quantitatively assess the effects of chronic disease self-management
programs on patients with diabetes, osteoarthritis, and hypertension. In addition, we were able to
pool results for post myocardial infarction programs. There were insufficient studies on stroke,
cancer, Parkinson’s and dyslipedemia to allow pooling. As reported above, self-management
programs for hypertension had a significant beneficial effect on systolic and diastolic blood
pressure when compared to usual care. Programs for diabetics showed a beneficial effect on
hemoglobin A1c and blood glucose, but not on weight. There was insufficient evidence to
support a beneficial effect on the health outcomes for pain and function for programs targeting
patients with osteoarthritis or the health outcomes of death or return-to-work for heart attack
patients.
99
In an attempt to assess whether chronic disease self-management programs were more
effective for more severe patients, we undertook a post-hoc quantitative analysis. Two clinicians
independently categorized each diabetes and osteoarthritis program as focusing on either more
severe or less severe patients. The clinicians were unable to categorize the hypertension and
post- MI programs in such a fashion, due to the lack of heterogeneity of the patients. In the
diabetes analysis, there was no statistical difference between the effectiveness of programs
targeted to more severe and less severe patients, in terms of change in hemoglobin A1c or
weight. For osteoarthritis studies, there was no statistical difference in change in pain or
functioning.
Question 12. What is the role of the physician? Can physicians be used to
reinforce learning?
Out meta-analysis did not reveal any statistically significant differences supporting the
role of physicians at enhancing the efficacy of chronic disease self-management programs.
Question 13. Cost effectiveness or cost savings—does the intervention appear to
reduce health care costs by reducing disease, physician office visits,
hospitalizations, nursing home admissions, etc.?
A total of 19 clinical trial studies were identified in this review of the economic impact of
Chronic Disease Self-Management (CDSM). These include 9 studies on diabetes, 4 studies on
osteoarthritis, one study on hypertension, two on post-myocardial infarction, and three nondisease-specific programs for chronically ill patients.
The 19 articles were located by four search methods: 1) previously described Quality
Review Form (QRF) with the key words “cost” or “utilization,” 2) references listed in relevant
100
articles or review articles (e.g., Clement,42 Norris,43 Klonoff44), 3) key word “health care
use/costs” search in “An Indexed Bibliography on Self-Management for People with Chronic
Disease,” and 4) a PubMed search with key words “diabetes,” “osteoarthritis,” “hypertension,”
“self-care,” and “cost,” “cost-effectiveness” or “economics.” Then we did title and abstract
screening to choose the literature. Finally, after careful assessment of study quality and relevance
for CDSM and economic analysis, 19 studies representing 19 programs were selected for review
(Evidence Table 5). All studies were randomized clinical trials if not otherwise indicated.
Diabetes
The type of articles included in our economic review of diabetic self-management
programs discuss:
1. Providing patient education programs,45-47
2. Comparing relative effectiveness of various intensity of educational programs,48, 49
3. Providing behavioral-based interventions,50
4. Providing dietary-specific interventions,40 and
5. Providing CDSM education and support as part of changes in the healthcare delivery
system.51, 52
Two of the three educational programs45, 47 failed to demonstrate effectiveness for the
measured outcomes. Thus these interventions cannot be cost-effective. The hospital education
program in de Weerdt47 incurred program costs – direct and indirect – at US $144 (1990 dollars,
101
about $240 in 2002 dollars*) per participant. The home visitation education program in Rettig45
was more expensive with an estimated program cost at $175 per participant (1983 dollars, about
$470 in 2002 dollars). Authors of both studies attribute the ineffectiveness of the interventions
partially to lack of supportive changes in the healthcare delivery system.
Wood46 reported that hospitalized patients who received an inpatient group education
program, which stressed both knowledge and self-help behaviors, experienced a significantly
lower emergency room (ER) visitation rate over the next four months (p <0.005). Based on selfreport, the 40 control patients reported 20 ER visits, and the 53 intervention patients reported
only two ER visits. Moreover, the control patients reported 18 hospital readmissions, whereas the
intervention patients reported only eight hospital readmissions. Although program cost was not
reported, the dramatic results in healthcare utilization outcomes would likely offset the program
cost and result in cost savings.
Klonoff and Schwartz44 conducted an economic analysis of interventions for diabetes,
including a section on self-management programs. Of the six self-care education programs they
analyzed, two were overlapped with the current review45, 47 and were discussed above. These
were the only two that did not report favorable cost-benefit results. The other four programs
reported in six studies had a benefit-cost ratio ranging from $0.43 to $8.76 for each dollar
spent.53-58 However, all these programs were conducted in or before 1985.
Two studies compared the relative effectiveness of various intensities of educational
programs.48, 49 Arsennau48 compared individualized learning activity packages (LAP) with
*
The inflation to 2002 dollars is derived from the percentage increase from 1990 to 2002 in the Consumer Price Indexes of Total
Medical Care Prices (From Statistical Abstract of United States, 2001). The indexes give 1990 = 162.8 given 1982-1984 = 100.
102
classroom instruction. LAP could provide a cheaper means of education for individuals by
saving $108.50 (1994 dollars, about $140 in 2002 dollars) in instructional fees. However, the
study reported LAP was less effective in lowering blood glucose levels than classroom
education, and thus was likely not to save healthcare costs. Campbell49 compared four programs
ranging from minimal instruction to an intensive educational and behavioral program. They
found that programs that were more intensive in terms of patient time and resources may be more
effective, but became less cost-effective. Their results showed that the four programs of differing
intensity had no difference in results in healthcare utilization and many outcome measures,
except for that the most intensive program (behavioral program) did have greater reduction in
diastolic blood pressure and cholesterol risk ratio along with higher patient satisfaction.
Kaplan and colleagues investigated behavioral-based interventions.50 The authors
reported direct costs for a program combining diet and exercise to be $1,000 (1986 dollars, about
$2190 in 2002 dollars) per participant, and this program could result in 0.092 incremental years
of well-being for each participant. The authors calculated the cost/utility equal to $10,870 (about
$23,800 in 2002 value) per “well-year” by the combined program. A cost/utility ratio less than
$50,000 is often considered cost-effective. Moreover, had the authors subtracted the cost of the
control program (10 weeks of group education) from the cost of the intervention program
($1,000), the cost/utility ratio would have been even more favorable than the one they reported.
Glasgow40 reported on a personalized, medical office-based intervention focused on
behavioral issues related to dietary self-management. This intervention used touchscreen
computer assessments to provide immediate feedback on key issues to patients and providers just
We assume the same rate of increase to estimate the index for 2002 to be 270. This method of inflation to 2002 dollars is applied
to the rest of the cost data in this section of the report.
103
prior to a visit, and provided goal setting and problem-solving assistance to patients following
the visit with a physician. Follow-up components included phone calls and videotape or
interactive video instruction depending on patient self-efficacy level. Incremental costs for the
delivery of this intervention totaled $14,755 (1995 dollars, about $18065 in 2002 dollars), or
$137 ($168 in 2002 dollars) per participant. At 12 month follow-up, this study resulted in $62
($76 in 2002 dollars) per reduction of each percent in dietary fat, $105 ($129 in 2002 dollars) per
percent reduction in saturated fat, and $8 ($10 in 2002 dollars) per mg/dl reduction in serum
cholesterol. The authors reported these costs are quite low compared to other studies of
pharmacological interventions to reduce cholesterol, which can cost from $350 ($430 in 2002
dollars) to $1,400 ($1715 in 2002 dollars) per patient per year. There were also significant
differences favoring the intervention as measured by patient satisfaction (p < 0.02). However,
there were no significant differences between groups to either hemoglobin A1c or on Body Mass
Index.
There are many ways to provide CDSM education and support as part of changes in the
healthcare delivery system. We were only able to review the economic impact of this type of
intervention based on two studies.51, 52 Sadur51 reported that, for patients who had poor diabetic
management, providing intensive multidisciplinary outpatient diabetes care management may be
cost neutral in the short term. This could be achieved by significant improvement in glycemic
control, which led to an early reduction in health care utilization, which would offset costs of the
intervention promptly. However, it is too early to conclude if improved glycemic control really
reduces health care utilization. Moreover, although the study reported the resources in terms of
providers’ time used for the program, the authors did not report the dollar figure that how much
104
the program costs. A cost-effectiveness study and replication of this intervention should be
conducted.
Litzelman52 investigated a multifaceted intervention that included patient education and a
behavioral contract about foot-care, and provided patient reinforcement reminders. Other
components of the intervention involved health care system support of identifiers on patient
folders to prompt providers for foot-care, and giving providers practice guidelines and
informational flow sheets on foot-related risk factors for amputation. This intervention resulted
in improved foot-care outcomes and process measures. The authors reported this intervention
would only cost $5,000 (1993 dollars, about $6700 in 2002 dollars) for study materials if it could
be implemented with the existing staff of a healthcare organization.
Osteoarthritis
The four OA studies include three types of articles:
1. Comparing relative effectiveness of lay-taught and professional-taught educational
programs,59
2. Providing patient education programs,60, 61 and
3. Providing social support and education interventions.62
The study that compared lay-taught and professional-taught self-management courses
reported that lay leaders could teach arthritis courses with results similar to those achieved by
professionals.59 Cost then became an issue of concern to patients and providers. The authors
assumed that lay leaders would either volunteer their time or would be paid a maximum of $100
(1985 dollars, about $245 in 2002 dollars) for leading the course. Thus, the arthritis course that
needed two lay-leaders would cost $0 to $200. On the other hand, a profession-led course would
105
cost $240 to $600. The authors reported, with similar effects, a lay-led course could result in
savings of $40 to $600 per course over the same courses taught by health professionals. This cost
savings, however, did not take into account any costs required for training and support of the lay
leaders (such as a center to answer lay-leaders’ questions). When compared with the no
intervention group at four-month follow-up, we also note that this study failed to show any
benefit in reducing the number of physician visits by either lay- or professional-led selfmanagement courses.
A similar self-help education program for arthritis patients60 was taught solely by lay
persons in a four-month RCT with a 20-month follow-up.† At four months, arthritis patients who
received the self-management course significantly exceeded control patients (who received no
CDSM course) in knowledge, recommended behaviors, and in decreased pain. The number of
visits to physicians was reduced without reaching statistical significance. The 20-month
longitudinal data showed the number of physician visits reduced from baseline to four-month
follow-up, and from four-months to eight-months, and remained about the same from eightmonth to 20-months. However, none of the differences reached statistical significance.
In contrast to the previous two community-based educational programs, a more recent
study,61 a nonrandomized clinical trial, tested the effects of a limited self-care intervention for
patients with knee OA that was delivered by an arthritis nurse specialist as an adjunct to primary
care. This intervention emphasized nonpharmacologic management of joint pain and
preservation of function by problem solving and by practicing behavioral principles of joint
protection. Telephone follow-up at one week and one month after initial instruction was designed
106
as part of the intervention, and a full written report of patient teaching and outcomes as well as
any needs or questions was placed in patient’s clinic record for any action deemed necessary by
the primary care physician. The results showed fewer physician visits by intervention subjects
(median visits five) compared to attention-control subjects (median visits six)(p <0.05) at 1-year
follow-up. Fewer visits translated directly into reduced clinic costs in the intervention group
(median costs at 1996 dollars = $229/patient, about $270/patient in 2002 dollars), compared to
controls (median costs = $305/patient, about $360/patient in 2002 dollars)(p <0.05). However,
the intervention had no significant effects on utilization and costs of outpatient pharmacy,
laboratory, or radiology services at the one-year follow-up. The authors reported 80% of the cost
of delivering the intervention ($58.70 per participant at 1996 dollars, about $70 in 2002 dollars)
was offset within one year by the reduced frequency and costs of primary care visits in this
study.
Groessl and Cronan62 in a recent study demonstrated that the monetary savings of a
community-based social support and education intervention greatly outweighed the cost of
conducting the intervention. In this study, 363 members of a health maintenance organization
(HMO), 60 years of age and older with osteoarthritis were randomly assigned to one of three
intervention groups (social support, education, or a combination of both) or to a control group.
These intervention programs were adapted from existing efficacy programs.61, 63-68 The total
costs to deliver the intervention were $9,450 for social support group (1992 dollars, about
$13,530 in 2002 dollars), $18,675 ($26,740 in 2002 dollars) for education group, and $14,175
($20,300 in 2002 dollars) for combination group, totaling $42,300 ($60,580 in 2002 dollars).
†
The 20-month follow-up after the four months RCT was a longitudinal study design. In other words, only intervention subjects
were followed up to 20 months whereas the control subjects were only followed up to 4 months.
107
After determining that there were no significant differences among the four groups when
analyzed separately, the authors examined a planned comparison of differential changes in health
care costs for the three intervention groups combined, in contrast to the control group. Assessed
by patients’ medical records, the results showed health care costs (all costs except for mental
health services) increased less in the intervention groups than in the control group over the three
year follow-up period. Health care cost savings were $1,156/participant (between $1,550 to
$1,655 per participant in 2002 value) for year one and two, and $1,279/participant
($1,635/particpant in 2002 value) for year three. With 273 patients who remained in the study
and completed the assessment, the one-year cost savings was $315, 588 ($451,955 in 2002
dollars), and resulted in a cost-benefit ratio of $315,588/$42,300 = $7.46:1. After discounting the
savings at a rate of 5% per year, the total three-year cost-benefit ratio was calculated as $315,588
+ $300,560 + $316,705 = $932,853/$42,300 = $22.05:1. The authors conducted sensitivity
analysis and reported the cost-savings were quite robust.
There are three concerns in this study by Groessl and Cronan.62 First is attrition. The
authors found that the mean annual health care costs of participants who dropped out ($4,793 in
1992 dollars, about $6,865 in 2002 dollars) were significantly higher than those of participants
who continued ($1,802 in 1992 dollars, about $2,580 in 2002 dollars). Secondly, health care
costs did not vary as a function of attendance at the meetings. The authors argued that many of
the study participants may have already been well educated about osteoarthritis and selfmanagement principles and/or had strong support networks. This suggests that a shorter
intervention, less than 20 meetings, might be just as effective. The last issue is about
generalizability of the study to minority population; the sample was largely Caucasian (92.3%)
with a mean age of 70 years old at entry into the study.
108
Among the four OA self-management studies reviewed, two of them reported significant
reduction in healthcare utilization and costs.61, 62 Of these two, one was an RCT62 and the other
design was non-randomized attention-control.61 One RCT followed with a longitudinal study60
reported a reduction in number of visits to physician, but did not reach statistical significance at
D = 0.05 level. The other study did not find reduction in number of physician visits, but showed a
cheaper alternative – led by lay leaders – to deliver patient education with same effectiveness as
a professional-led course.
Hypertension
For hypertension self-management, we identified only one study with economic
information.69, 70 This study was intended to investigate methods to enhance patient compliance
with assigned relaxation practice and to understand the impact of accomplished relaxation on
elevated blood pressure. Although all interventions were found to have significant effects on
reducing blood pressure, the authors reported that group relaxation alone was the most costeffective strategy as compared to individual training and group plus contingency contracting.
This is because it achieved higher relaxation practice compliance and greater reductions in blood
pressure while using the least time of the therapist. The authors did not provide the actual costs
for therapist time; nor did they attempt to measure impact on healthcare costs or utilization. Thus
we cannot judge if such a relaxation practice is cost saving.
Post-Myocardial Infarction
We identified two studies of post-myocardial infarction programs containing economic
information.71, 72 Both programs assessed home-based rehabilitation as an alternative to
traditional rehabilitation programs.
109
The study of DeBusk71 compared the medically directed at-home rehabilitation training
with a group rehabilitation and two no-training intervention arms (one with exercise testing but
not subsequent exercise training, and one with neither testing nor training). Their targeted
population was male patients aged 70 or younger with a clinically uncomplicated acute
myocardial infarction (AMI). Compared to group rehabilitation, patients assigned to the
medically directed at-home rehabilitation had about equally high adherence to individually
prescribed exercise, increase in functional capacity, and equally low nonfatal reinfarction and
dropout rates. Compared to the no-training groups, the patients randomized to the two training
groups achieved significantly greater increases in functional capacity, but there was no
difference in cardiac events. The cost for the three months of at-home rehabilitation in this study
was estimated to be approximately $328 per patient (1983 dollars, about $885 in 2002 dollars).
In contrast, the group rehabilitation program was approximately $720 ($1,945 in 2002 dollars).
Thus the authors claimed that, compared to group rehabilitation, medically directed at-home
rehabilitation has the potential to increase the availability and to decrease the cost of
rehabilitating low-risk survivors of AMI.
The study by Lewin72 examined whether a comprehensive home-based program reduced
psychological distress and use of health services. Subjects randomized into the self-help
rehabilitation program were given a heart manual that included education, a home-based exercise
program, and a tape-based relaxation and stress management program. Also included were
specific self-help treatments for commonly experienced psychological problems among post –MI
patients. Spouses were given materials to support and encourage compliance by patients. A
treatment facilitator provided follow-up and feedback to potentiate self-help treatments. In the
control group, subjects received standard care plus a placebo package of information and
110
informal counseling. Besides finding better psychological adjustment in the rehabilitation group
than the control, the authors reported significant differences in the use of health services. The
rehabilitation group made significantly less GP consultations in the one-year follow-up (a mean
of 1.8 less visits than did the control group in the first 6 months, and a mean of 0.9 less visits in
the subsequent 6 months). In addition, significantly more control patients than rehabilitation
group patients were admitted to the hospital in the first 6 months (18 vs. 6) but not significant at
the second 6 months (18 vs. 9).
Costs of the intervention were not assessed rigorously, but the authors estimated it to be
£30 - £50 (roughly $100 to $165 in 2002 dollars). The authors claimed that the modest costs of
the self-help program might well be balanced by the reduction in GP consultations and hospital
admissions. The caveat of this result is that the use of health services was based on patients’
general practitioners self-report, so the reliability and validity is uncertain. In addition, as an
alternative to hospital-based program, the cost-effectiveness of the home-based program should
be compared with that of a hospital-based program.
Non-disease-specific Programs
Three RCTs provided self-management programs to general chronically ill patients were
identified to include economic evaluation.73-75 One intervention setting was within healthcare
organization,74 another was community-based,75 and the other was collaboration between
primary care providers and community center.73 The latter two showed significant reductions in
hospital use (including number of hospitalized patients, number of hospitalizations, and inpatient
hospital days). From a societal perspective, such reduced hospital use may result in the two
CDSM programs being cost-saving interventions (i.e., the savings in hospital utilization offsets
111
the cost to provide interventions). Nevertheless, rigorous cost-benefit or cost-effectiveness
analyses were not done.
The primary care-based intervention, called “Chronic Care Clinics” for frail older adults,
did not find significant differences in healthcare costs or utilization between intervention and
control groups.74 Besides methodological reasons to explain these findings, the authors attributed
these results to a hindrance in implementation of this intervention due to major changes in the
delivery system under study. These changes resulted in a lack of continuity and support of
clinical and administrative staff and thus undoubtedly influenced the ability of the study to
demonstrate more positive effects on patient outcomes and utilizations.
A geriatric nurse-led “care manager” model that involved collaboration between primary
care providers and a community center reported beneficial reductions in hospital use, and should
be further examined.73 The utilization differences were of borderline statistical significance (see
Appendix evidence table). The study did not report beneficial findings on two outcome measures
– physical performance and overall health profile (as measured by SF-36). Additional studies
seeking to replicate or explain these findings are warranted.
The other program, the community-based Chronic Disease Self-Management Program
(CDSMP), was an extensive educational course with skills training, feedback, and group support.
It was designed for people who had lung disease, heart disease, stroke, arthritis, or diabetes. The
program approach did not differ by disease type. This program reported decreases in healthcare
utilization in the randomized clinical trial,75 and in two additional observational studies. One
study used a before-after cohort design,76 and the other study was a longitudinal design intended
to follow-up patients enrolled in the randomized trial.77 According to the authors, all three
studies were likely to be cost-saving from a societal perspective. However, this conclusion is
112
tempered as none of the studies performed a rigorous cost-benefit analysis. In addition, the
studies differed in what aspect of utilization was reduced. The randomized clinical trial75
significantly decreased the number of hospitalizations and length of hospital stays. The beforeafter cohort study found the study participants had fewer visits to the emergency department.76
The longitudinal study reported a reduction in combined ER/outpatient visits.77 Compared to the
other two RCTs,73, 74 the CDSMP was provided to younger populations. The mean age of the
study participants was about 65 years old, while the mean age was about 77 years old in the other
two RCTs.
Critiques and Conclusions
These reviewed interventions from clinical trials represent only a subset of possible
strategies for CDSM. This economic review has limited generalizability beyond the studied
interventions. Critiques about the economic aspect of CDSM literature include:
1. Costs of the intervention are rarely reported and, when reported, was sometimes not
rigorously performed (e.g., by author’s best approximation; perspective of costing
was inconsistent; time costs to patients and providers were not fully accounted);
2. Health care costs as an outcome of the intervention were rarely studied;
3. Changes in health care utilization were seldom studied, and in many cases only
studied on a limited scale (not including all types of services);
4. The follow-up period is short, while many outcomes will not be evident for many
years (e.g., rigid metabolic control may result in a delay or prevention of diabetic
complications, but only after several years).
113
Among the four diseases reviewed, the programs to promote self-management with
osteoarthritis patients have the best economic information and are most consistently reporting
reductions in health care utilization and costs, even to the point of cost-savings. Such findings
are compatible with observational studies.14-16 Programs for diabetic patients have mixed results,
and overall are weaker in the economic information they report. There is only one hypertension
program identified that include any economic information, and the information provided does
not allow us to adequately judge cost-effectiveness of the program. The two reviewed MI studies
both lacked a rigorous collection of economic data, but the limited evidence presented suggests
that home-based rehabilitation programs could potentially be a cost-effective alternative to group
rehabilitation or standard care. As for the three general, non-disease-specific programs, two
RCTs and two observational studies reported that low-cost, community-based CDSM programs
may potentially be cost-saving.
Question 14. Delivery mechanism: What do we know about whom (which
provider type? trained lay person?) should deliver this service? Do we know
which care settings have proven effective (e.g., physician’s office, senior center,
other community or clinical settings)?
Successful CDSM programs have been delivered by both medically-trained providers and
by training lay people, and have been performed in (list the settings that have positive studies).
However, we were unable to find evidence to support generalizing the finding of these individual
studies to policy.
114
LIMITATIONS
Despite finding evidence that CDSM programs have a clinically and statistically
significant beneficial effect on some outcomes, we were unable to discern which elements of
CDSM programs are most associated with success. This may have been because we did not test
the right hypotheses regarding CDSM elements, or because key variables describing these
components were either not recorded adequately or not recorded at all in the published articles,
or that the individual components themselves each have relatively weak effects. We considered
contacting original authors for additional information regarding their interventions, but rejected
this due to time and resource constraints. Furthermore, our experience has been that any study
published more than a few years ago has a much lower likelihood for getting a favorable
response to such a request, and 524 of our studies were published more than 10 years ago. In
addition, we may have lacked the statistical power, due to the small number of studies available,
to discern the reasons for the relatively small amount of heterogeneity in the study results. We
note that the preceding challenges are common to all studies of complex, multicomponent
interventions, and these challenges did not prevent us from detecting important differences in the
effectiveness of interventions for prevention of falls17 or increasing the use of cancer screening
and immunizations.18
An additional primary limitation of this systematic review, common to all such reviews,
is the quantity and quality of the original studies. We made no attempt to give greater
importance to some studies based on "quality." The only validated assessment of study quality
includes criteria not possible in self-management (double-blinding). As there is a lack of
empirical evidence regarding other study characteristics and their relationship to bias, we did not
attempt to use other criteria.
115
As previously discussed, we did find evidence of publication bias in hemoglobin A1c,
mortality, and systolic and diastolic blood pressure outcomes in diabetes, post-myocardial
infarction care, and hypertension, respectively. Therefore, the beneficial results that we report in
our pooled analysis need to be considered in light of the possible existence of unpublished
studies reporting no benefit.
116
CONCLUSIONS
6. Chronic disease self-management programs probably have a beneficial effect on some, but
not all, physiologic outcomes. In particular, we found evidence of a statistically significant
and clinically important benefit on measures of blood glucose control and blood pressure
reduction for chronic disease self management programs for patients with diabetes and
hypertension, respectively. Our conclusions are tempered by our finding of possible
publication bias, favoring beneficial studies, in these two clinical areas. These was no
evidence of a beneficial effect on other physiologic outcomes such as pain, function, weight
loss, and return to work.
7. There is not enough evidence to support any of the proposed elements as being essential to
the efficacy of chronic disease self-management programs. More research is needed to try
and establish the optimum design of a chronic disease self-management program, and
whether or not this differs substantially depending on the particular chronic disease or
characteristics of the patient.
8. While no randomized studies of chronic disease self-management programs for older adults
assessed the use of email or the Internet, one recently reported randomized study of email use
in the self-management of middle aged adults with back pain was sufficiently promising to
warrant testing such interventions for chronic disease self-management in the Medicare
population.
9. There is no evidence to conclusively support or refute the role of physician providers in
chronic disease self-management programs for older adults.
117
10. The evidence is inconclusive but suggests that chronic disease self-management programs
may reduce health care use.
118
RECOMMENDATIONS
1. There is sufficient evidence to warrant a policy initiative promoting chronic disease selfmanagement programs for older adults.
2. However, before implementing such a policy, additional work is needed to optimally define
the essential elements of such programs, and whether they vary by condition or patient
characteristic.
119
REFERENCES CITED
1. Centers for Disease Control and Prevention. Unrealized prevention opportunities: reducing the health and
economic burden of chronic disease. Centers for Disease Control and Prevention, National Center for
Chronic Disease Prevention and Health Promotion. 1997. [Rec#: 8007 ]
2. National Center for Health Statistics. Health, United States, 1999 with Health and Aging Chartbook.
Hyattsville, MD: National Center for Health Statistics; 1999. [Rec#: 5049]
3. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA
2002;288(14):1775-9. [Rec#: 8036]
4. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the
chronic care model, Part 2. JAMA 2002;288(15):1909-14. [Rec#: 8037]
5. Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care:
translating evidence into action. Health Aff (Millwood) 2001;20(6):64-78. [Rec#: 8038]
6. Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary
care. JAMA 2002;288(19):2469-75. [Rec#: 8039]
7. Robert Wood Johnson Foundation. Advancing Diabetes Self-Management Program Announcement. available
at URL: www.rwjf.org/programs/npoDetail.jsp?id=IDC. Accessed 1/29/2003.
8. Center for the Advancement of Health. An Indexed Bibliography on Self-Management for People with
Chronic Disease. Washington, DC: Center for the Advancement of Health. 1996. [Rec#: 8015]
9. Hedges LV, Olkin I. Statistical Methods for Meta-Analysis. San Deigo, CA: Academic Press Inc; 1985.
[Rec#: 5099]
10. Rosenthal R. Meta-Analytic Procedures for Social Research. Newbury Park: Sage Publications; 1991. [Rec#:
5104]
120
References Cited
11. DerSimonian R LN. Meta-analysis in clinical trials. Control Clin Trials 1986;7(3):177-88. [Rec#: 5098]
12. Glasgow RE, McKay HG, Piette JD, Reynolds KD. The RE-AIM framework for evaluating interventions:
what can it tell us about approaches to chronic illness management? Patient Educ Couns 2001;44
(2):119-27. [Rec#: 8034]
13. Gruman J. Essential elements of self-management interventions (monograph). The Center for the
Advancement of Health; Funding provided by The Robert Wood Johnson Foundation 2002. [Rec#:
8035]
14. Lorig K, Holman HR. Long-term outcomes of an arthritis self-management study: effects of reinforcement
efforts. Soc Sci Med 1989;29(2):221-4. [Rec#: 832]
15. Lorig K, Laurin J, Holman HR. Arthritis self-management: a study of the effectiveness of patient education
for the elderly. Gerontologist 1984;24(5):455-7. [Rec#: 833]
16. Lorig KR, Mazonson PD, Holman HR. Evidence suggesting that health education for self-management in
patients with chronic arthritis has sustained health benefits while reducing health care costs. Arthritis
Rheum 1993;36(4):439-46. [Rec#: 836]
17. Shekelle PG, Morton S, Chang JT, Mojica W, Maglione M, Suttorp M, et al. Falls Prevention Interventions in
the Medicare Population. Baltimore, MD: US Department of Health and Human Services, Health Care
Financing Administration. In preparation. [Rec#: 5113]
18. Shekelle PG, Stone EG, Maglione MA, Morton SC, Roth EA, Chao B, et al. Interventions that increase the
utilization of Medicare-funded preventive services for persons age 65 and older. Evidence Report/
Technology Assessment. US Dept. of Health and Human Services. Health Care Financing
Administration, Publication No. HCFA-02151 1999. [Rec#: 5120]
19. Fried L. Epidemiology of aging. Epidemiology Reviews 2000;22(1):95-106. [Rec#: 8008]
20. Hobbs FB, Damon BL. Sixty-Five Years Plus in America. Current Population Reports, Special Studies.
121
References Cited
Washington, DC: US Department of Commerce, Economics, and Statistics Administration Bureau of
Census. 1996. [Rec#: 8010]
21. Ettinger WH, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial
comparing aerobic exercise and resistance exercise with a health education program in older adults
with knee osteoarthritis The Fitness Arthritis and Seniors Trial (FAST) [see comments]. JAMA
1997;277(1):25-31. [Rec#: 1944]
22. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons
with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program
(SHEP). JAMA 1991;265(24):3255-64. [Rec#: 8012]
23. Diabetes Control and Complications Trial Research Group. N Engl J Med 1993;329:977-86. [Rec#: 8013]
24. Ohikubo Y, Kishidkawa H, Araki E, et al. Intensive insulin therapy prevents the progression of diabetic
microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a
randomized prospective 6-year study. Diabetes Res Clin Pract 1995;28 :103-17. [Rec#: 8014]
25. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of
reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17(1):1-12. [Rec#:
5100]
26. SAS/ STAT [computer program]. Version Version 8. Cary, NC: SAS Institute, Inc.; 1999.
27. Microsoft Excel for Windows 2000 [computer program]. Redmond, WA: Microsoft Corporation; 2000.
28. Stata Statistical Software: Release 6.0 [computer program]. College Station TX: Stata Corporation; 1999.
29. StatXact 4 for Windows [computer program]. Version Version 4.0. Cambridge, MA: Cytel Software
Corporation; 2000.
30. Ioannidis JP, Cappelleri JC, Lau J, et al. Early or deferred zidovudine therapy in HIV-infected patients
without an AIDS-defining illness. Ann Intern Med 1995;122(11):856-66. [Rec#: 5105]
122
References Cited
31. Berkey CS, Hoaglin DC, Mosteller F, et al. A random-effects regression model for meta-analysis. Stat Med
1995;14(4):395-411. [Rec#: 5096]
32. Sharp SJ. Meta-analysis regression. STATA Technical Bulletin 1998;42:16-22. [Rec#: 5097]
33. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics
1994;50 (4):1088-101. [Rec#: 5106]
34. Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ
1997;315(7109):629-34. [Rec#: 5107]
35. Windsor RA, Lowe JB. Behavioral impact and cost analysis of a worksite self-help smoking cessation
program. Prog Clin Biol Res 1989;293:231-242. [Rec#: 1058]
36. Mazzuca SA, Moorman NH, Wheeler ML, Norton JA, Fineberg NS, Vinicor F, et al. The diabetes education
study: A controlled trial of the effects of diabetes patient education. Diabetes Care 1986;9:1-10. [Rec#:
2132]
37. Wheeler LA, Wheeler ML, Ours P, Swider C. Evaluation of computer-based diet education in persons with
diabetes mellitus and limited educational background. Diabetes Care 1985;8( 6):537-44. [Rec#: 3442]
38. Wise PH, Dowlatshahi DC, Farrant S, Fromson SS/Meadows KA. Effect of computer-based learning on
diabetes knowledge and control. Diabetes Care 1986;9:504-508. [Rec#: 2205]
39. Glasgow RE, Toobert DJ, Hampson SE. Effects of a brief office-based intervention to facilitate diabetes
dietary self-management. Diabetes Care 1996;19(8):835-42. [Rec#: 799]
40. Glasgow RE, La Chance PA, Toobert DJ, Brown J, Hampson SE, Riddle MC. Long-term effects and costs of
brief behavioural dietary intervention for patients with diabetes delivered from the medical office.
Patient Educ Couns 1997;32(3):175-84. [Rec#: 3433]
41. Lorig KR, Laurent DD, Deyo RA, Marnell ME, Minor MA, Ritter PL. Can a Back Pain E-mail Discussion
Group improve health status and lower health care costs?: A randomized study. Arch Intern Med
123
References Cited
2002;162(7):792-6. [Rec#: 8041]
42. Clement S. Diabetes self-management education. Diabetes Care 1995;18(8):1204-14. [Rec#: 769]
43. Norris SL, Engelgau MM, Narayan KMV. Effectiveness of self-management training in Type 2 Diabetes. A
systematic review of randomized controlled trials. Diabetes Care 2001;24:561-587. [Rec#: 3431]
44. Klonoff DC, Schwartz DM. An economic analysis of interventions for diabetes. Diabetes Care
2000;23(3):390-404. [Rec#: 8019]
45. Rettig BA, Shrauger DG, Recker RP, Gallagher TF, Wiltse H. A randomised study of the effects of a home
diabetes education program. Diabetes Care 1986;9:173-178. [Rec#: 2270]
46. Wood ER. Evaluation of a hospital-based education program for patients with diabetes. Journal of the
American Dietetic Association 1989;89:354-358. [Rec#: 2159]
47. de Weerdt I, Visser AP, Kok GJ, et al. Randomized controlled multicentre evaluation of an education
programme for insulin-treated diabetic patients: effects on metabolic control, quality of life, and costs
of therapy. Diabetic Medicine 1991;8(4):338. [Rec#: 2589]
48. Arseneau DL, Mason AC, Wood OB, Schwab E, Green D. A comparison of learning activity packages and
classroom instruction for diet management of patients with non-insulin-dependent diabetes mellitus.
Diabetes Educ 1994;20(6):509-14. [Rec#: 749]
49. Campbell EM, Redman S, Moffitt PS, et al. The relative effectiveness of educational and behavioral
instruction programs for patients with NIDDM: a randomized trial. Diabetes Educator 1996;22
(4):379. [Rec#: 2586]
50. Kaplan RM, Hartwell SL, Wilson KD, Wallace JP. Effects of diet and exercise interventions on control and
quality of life in non-insulin dependent diabetes mellitus. J Gen Intern Med 1987;2:220-227. [Rec#:
2175]
51. Sadur CN, Moline N, Costa M, Michalik D, Mendlowitz D, Roller S, et al. Diabetes management in a health
124
References Cited
maintenance organization. Efficacy of care management using cluster visits [In Process Citation].
Diabetes Care 1999;22(12):2011-7. [Rec#: 1668]
52. Litzelman DK, Slemenda CW, Langefeld CD, Hays LM, Welch MA, Bild DE, et al. Reduction of lower
extremity clinical abnormalities in patients with non-insulin-dependent diabetes mellitus. A
randomized, controlled trial. Ann Intern Med 1993;119(1):36-41. [Rec#: 828]
53. Laugharne E, Steiner G. Tri-hospital diabetes education centre: a cost effective, cooperative venture. Can
Nurse 1977;73(9):14-9. [Rec#: 8016]
54. Nersesian W, Zaremba M WB. Impact of diabetes outpatient education program: Maine. MMWR 1982;31:
307-314. [Rec#: 8029]
55. Schwartz R, Zaremba M, Ra K. Third-party coverage for diabetes education program. QRB Qual Rev Bull
1985;11(7):213-7. [Rec#: 8017]
56. Zaremba MM, Willhoite B, Ra K. Self-reported data: reliability and role in determining program
effectiveness. Diabetes Care 1985;8(5):486-90. [Rec#: 8018]
57. Whitehouse FW, Whitehouse IJ, Cox MS, Goldman J, Kahkonen DM, Partamian JO, et al. Outpatient
regulation of the insulin-requiring person with diabetes (an alternative to hospitalization). J Chronic Dis
1983;36(6):433-8. [Rec#: 8021]
58. Fishbein HA. Precipitants of hospitalization in insulin-dependent diabetes mellitus (IDDM): a statewide
perspective. Diabetes Care 1985;8 Suppl 1:61-4. [Rec#: 8020]
59. Lorig K, Feigenbaum P, Regan C, Ung E, Chastain RL, Holman HR. A comparison of lay-taught and
professional-taught arthritis self- management courses. J Rheumatol 1986;13(4):763-7. [Rec#: 830]
60. Lorig K, Lubeck D, Kraines RG, Seleznick M, Holman HR. Outcomes of self-help education for patients
with arthritis. Arthritis Rheum 1985;28(6):680-5. [Rec#: 835 ]
61. Fries JF. Arthritis: A comprehensive guide to understanding your arthritis. Reading, MA: Addison-Wesley;
125
References Cited
1990. [Rec#: 8032]
62. Groessl EJ, Cronan TA. A cost analysis of self-management programs for people with chronic illness. Am J
Community Psychol 2000;28(4):455-80. [Rec#: 8022]
63. Cronan AW. Sexually transmitted diseases: a pilot education programme in Queensland. Community Health
Stud 1985;9(3):246-52. [Rec#: 8025]
64. Fries JF. The future of disease and treatment. Changing health conditions, changing behaviors, and new
medical technology. J Prof Nurs 1986;2(1):10-9. [Rec#: 8026]
65. Fries JF. Arthritis: A take care of yourself health guide. Reading, MA: Addison-Wesley; 1995. [Rec#: 8033]
66. Lorig K, Fries JF. The arthritis helpbook. Reading, MA: Addison-Wesley; 1990. [Rec#: 8030]
67. Lorig K, Konkol L, Gonzalez V. Arthritis patient education: a review of the literature. Patient Educ Couns
1987;10 (3):207-52. [Rec#: 8024]
68. Lorig K, Lubeck D, HOlman HR. Nonassociation of new behaviors with favorable outcomes in effective
arthritis health education. Arthritis and Rheumatology 1982;25(Suppl):S148. [Rec#: 8031]
69. Hoelscher TJ, Lichstein KL, Rosenthal TL. Home relaxation practice in hypertension treatment: objective
assessment and compliance induction. J Consult Clin Psychol 1986;54(2):217-21. [Rec#: 8027]
70. Hoelscher TJ, Lichstein KL, Fischer S, et al. Home relaxation practice in hypertension treatment: Objective
assessment and compliance induction. J of Consulting and Clinical Psychology 1986;54 :217-221.
[Rec#: 2457]
71. DeBusk F, Haskell WL, Miller NNet al. Medically directed at-home rehabilitation soon after clinically
uncomplicated acute myocardial infarction: a new mode for patient care. Am J Cardio 1985;85:251257. [Rec#: 2669]
72. Lewin B, Robertson IH, Cay EL, Irving JB, Campbell M. Effects of self-help post-myocardial-infarction
126
References Cited
rehabilitation on psychological adjustment and use of health services. Lancet 1992;339(8800):1036-40.
[Rec#: 827]
73. Leveille SG, Wagner EH, Davis C, Grothaus L, Wallace J, LoGerfo M, et al. Preventing disability and
managing chronic illness in frail older adults: A randomized trial of a community-based partnership
with primary care. JAGS 1998;46(10):1-9. [Rec#: 1175]
74. Coleman EA, Grothaus LC, Sandhu N, Wagner EH. Chronic care clinics: a randomized controlled trial of a
new model of primary care for frail older adults. J Am Geriatr Soc 1999;47(7):775-783. [Rec#: 1510]
75. Lorig KR, Sobel DS, Stewart AL, Brown Jr BW, Bandura A, Ritter P, et al. Evidence suggesting that a
chronic disease self-management program can improve health status while reducing hospitalization: A
randomized trial. Medical Care 1999 ;37(1):5-14. [Rec#: 608]
76. Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with
chronic disease. Eff Clin Pract 2001;4(6):256-62. [Rec#: 3481]
77. Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW Jr, Bandura A, et al. Chronic disease self-management
program: 2-year health status and health care utilization outcomes. Med Care 2001;39(11):1217-23.
[Rec#: 3473]
127
APPENDIX A. EXPERT PANELIST
Terry L. Bazzarre, PhD
The Robert Wood Johnson Foundation
Albert Martin, MD
Consultant
Linda A. Bergthold, PhD
Health Care Consultant and Researcher
Robin Mockenhaupt, PhD
The Robert Wood Johnson Foundation
Noreen Clark, PhD
University of Michigan School of Public
Health
C. Tracy Orleans, PhD
The Robert Wood Johnson Foundation
Suzanne Smith, MD
National Center for Chronic Disease
Prevention and Health Promotion
James Cooper, MD
George Washington University
Medical Center, Geriatrics Division
Paul Tarini
The Robert Wood Johnson Foundation
Fran Ferrara
The Robert Wood Johnson Foundation
Sara Their, MPH
The Robert Wood Johnson Foundation
Russell E. Glasgow, PhD
AMC Caner Research Center
Michael VonKorff, Sc.D
Center for Health Care Studies,
Group Health Cooperative of Puget Sound
Catherine Gordon, RN, MBA
Center for Medicare and Medicaid Services
Ed Wagner, MD, MPH
McCall Institute for Healthcare Innovations
Group Health Cooperative of Puget Sound
Jessie Gruman, PhD
Center for the Advancement of Health
Kate Lorig, RN, DrPH
Stanford University
155
APPENDIX B. ACCEPTED ARTICLES
Allen BT, DeLong ER, Feussner JR. Impact of glucose
self-monitoring on non-insulin-treated patients with
type II diabetes mellitus. Diabetes Care 1990;13:10441050. [Rec#: 2201]
Campbell EM, Redman S, Moffitt PS, et al. The relative
effectiveness of educational and behavioral instruction
programs for patients with NIDDM: a randomized
trial. Diabetes Educator 1996;22(4):379. [Rec#: 2586]
Anderson RM, Funnell MM, Butler PM, Arnold MS,
Fitzgerald JT, Feste CC. Patient empowerment.
Results of a randomized controlled trial. Diabetes Care
1995;18(7):943-9. [Rec#: 747]
Cohen JL, Sauter SV, deVellis RF, deVellis BM.
Evaluation of arthritis self-management courses led by
laypersons and by professionals. Arthritis Rheum
1986; 29(3): 388-93. [Rec#: 770]
Arseneau DL, Mason AC, Wood OB, Schwab E, Green D.
A comparison of learning activity packages and
classroom instruction for diet management of patients
with non-insulin-dependent diabetes mellitus.
Diabetes Educ 1994;20(6):509-14. [Rec#: 749]
D'Eramo-Melkus GA, Wylie-Rosett J, Hagan JA.
Metabolic impact of education in NIDDM . Diabetes
Care 1992;18:864-869. [Rec#: 2202]
de Pont AJ, Baker IA, St Leger AS, Sweetman PM, Wragg
KG, Stephens SM, et al. A randomized controlled trial
of the effect of low fat diet advice on dietary response
in insulin independent diabetic women. Diabetologia
1981;21(6):529. [Rec#: 2210]
Aubert RE, Herman WH, Waters J, et al. Nurse case
management to improve glycemic control in diabetic
patients in a health maintenance organization. A
randomized, control trial (see comments). Annuals of
Internal Medicine 1998;129(8):605. [Rec#: 2581]
DeBusk F, Haskell WL, Miller NNet al. Medically directed
at-home rehabilitation soon after clinically
uncomplicated acute myocardial infarction: a new
mode for patient care. Am J Cardio 1985;85:251-257.
[Rec#: 2669]
Barlow JH, Turner AP, Wright CC. A randomized
controlled study of the Arthritis Self-Management
Program in the UK. Health Educ Res 2000; 15(6):
665-80. [Rec#: 3274]
Bethea DC, Stallings SF, Wolman PG, Ingram RC.
Comparison of conventional and videotaped diabetic
exchange lists instruction. Journal of the American
Dietetic Association 1989;89:405-406. [Rec#: 2105]
DeBusk RF, Miller NH, Superko HR, Dennis CA, Thomas
RJ, Lew HT, et al. A case-management system for
coronary risk factor modification after acute
myocardial infarction. Ann Intern Med
1994;120(9):721-9. [Rec#: 775]
Biermann E, Dietrich W, Standl E. Telecare of diabetic
patients with intensified insulin therapy. A
randomized clinical trial. Stud Health Technol Inform
2000;77:327-32. [Rec#: 3436]
Dennis C, Houston-Miller N, Schwartz RG, et al. Early
return to work after uncomplicated myocardial
infarction. JAMA 1988;260:214-220.
[Rec#:
2656]
Bloomgarden ZT, Karmally W, Metzger J, Borhters M,
Nechemias C, Bookman J, et al. Randomized,
controlled trial of diabetic education: improved
knowledge without improved metabolic status.
Diabetes Care 1987;10 :263-272. [Rec#: 2172]
DICET. Integrated care for diabetes: clinical, psychosocial,
and economic evaluation. Diabetes Integrated Care
Evaluation Team. BMJ 1994;308(6938):1208-1212.
[Rec#: 2614]
Doyle TH, Granada JL. Influence of two management
approaches on the health status of women with
osteoarthritis. Arthritis and Rheumatism 1982;25:S56.
[Rec#: 2427]
Blumenthal JA, Siegel WC, Appelbaum M. Failure of
exercise to reduce blood pressure in patients with mild
hypertension. Results of a randomized controlled trial
[see comments]. JAMA 1991;266(15):2098-104.
[Rec#: 752]
Emori KH. The use of a programmed textbook in diabetic
patient education. Loma Linda, CA: Loma Linda
University. 1964. [Rec #: 2118]
Boehm S, Schlenk EA, Raleigh E, Ronis D. Behavioral
analysis and behavioral strategies to improve selfmanagement of type II diabetes. Clin Nurs Res
1993;2(3):327-44. [Rec#: 754]
Falkenberg MG, Elwing BE, Goransson AM, Hellstrand
BE, Riis UM. Problem oriented participatory
education in the guidance of adults with non-insulintreated type II diabetes mellitus. Scand J Prim Health
Care 1986;4:157-164. [Rec#: 2190]
Burgess AW, Lerner DJD'Agostino RB, Vokonas PS,
Hartman CR, Gaccione P. A randomized control trial
of cardiac rehabilitation. Soc Sci Med 1987;24:359370. [Rec#: 2652]
156
Accepted Articles
Frasure-Smith N, Prince R. The ischemic heart disease life
stress monitoring program: impact on mortality.
Psychosom Med 1985;47 (5):431-45. [Rec#: 790]
Glasgow RE/Toobert DJ, Mitchell DL, Donnely JE, Calder
D. Nutrition education and social learning
interventions for type II diabetes. Diabetes Care
1989;12:150-152. [Rec#: 2209]
Frasure-Smith N, Prince R. Long-term follow-up of the
ischemic heart disease life stress monitoring program.
Psychosom Med 1989;51:485-513. [Rec#: 2218]
Goeppinger J, Arthur MW, Baglioni AJ= Jr, Brunk SE,
Brunner CM. A re-examination of the effectiveness of
self-care education for persons with arthritis. Arthritis
Rheum 1989;32(6):706-16. [Rec#: 801]
Friedman M, Thoresen C, Gill JJ, Ulmer DK. Feasibility of
altering Type A behavior pattern after myocardial
infarction: Recurrent coronary prevention project
study: Methods, baseline results and preliminary
findings. Circulation 1982;66:83-92. [Rec#: 2367]
Goldstein IB, Shapiro D, et al. Comparison of drug and
behavioral treatments of essential hypertension. Health
Psychology 1982;1:7-26. [Rec#: 2466]
Friedman M, Thoresen CE, Gill JJ, et al. Alteration of Type
A behavior and reduction in cardiac recurrences in
postmyocardial infarction patients. Am Heart J
1984;108:237-248. [Rec#: 2362]
Gonzalez-Fernandez RA, Rivera M, Torres D, Quiles J,
Jackson A. Usefulness of a systemic hypertension inhospital program. The American Journal of
Cardiology 1990;65:1384-1386. [Rec#: 3451]
Froelicher ES, Kee LL, Newton KM, Lindskog B,
Livingston M. Return to work, sexual activity, and
other activities after acute myocardial infarction. Heart
Lung 1994;23(5):423-35. [Rec#: 792]
Greenfield S, Kaplan SH, Ware JE Jr, Yano EM, Frank HJ.
Patients' participation in medical care: effects on blood
sugar control and quality of life in diabetes. J Gen
Intern Med 1988;3(5):448-57. [Rec#: 803]
Frost G, Wilding J, Beecham J. Dietary advice based on the
glycemic index improves dietary profile and metabolic
control in type 2 diabetic patients. Diabet Med
1994;11(4):397-401. [Rec#: 791]
Gruen W. Effects of brief psychotherapy during rhe
hospitalization period on the recovery process in heart
attacks. J Consulting Clinical Psychology
1975;43:223-232. [Rec#: 2360]
Garcia-Vera MP, Labrador FJ, Sanz J. Stress-management
training for essential hypertension: a controlled study.
Applied Pyschophysiology and Biofeedback
1997;22(4):261-283. [Rec#: 3449]
Hafner RJ. Psychological treatment of essential
hypertension: A controlled comparison of meditation
and medication plus biofeedback. Biofeedback and
Self-regulation 1982;7:305-315. [Rec#: 2467]
Gilden JL, Hendryx MS, Clar S, Casia C, Singh SP.
Diabetes support groups improve health care of older
diabetic patients. JAGS 1992;40:147-150. [Rec#:
3450]
Hanefield M, Fischer S, Schmechel H, et al. Diabetes
Intervention Study. Multi-intervention trial in newly
diagnosed NIDDM. Diabetes Care 1991;14(4):308.
[Rec#: 2595]
Given C, Given B, Coyle B. The effects of patient
characteristics and beliefs on responses to behavioral
interventions for control of chronic diseases. Pat Ed
Counsel 1984;6(3):131-140. [Rec#: 2309]
Hassell J, Medved E. Group/audiovisual instruction for
patients with diabetes. Journal of the American
Dietetic Association 1975;5:465-470. [Rec#: 2121]
Heller RF, Knapp JC, Valenti LA, Dobson AJ. Secondary
prevention after acute myocardial infarction. Am J
Cardiol 1993;72(11):759-62. [Rec#: 809]
Glasgow RE, La Chance PA, Toobert DJ, Brown J,
Hampson SE, Riddle MC. Long-term effects and costs
of brief behavioral dietary intervention for patients
with diabetes delivered from the medical office.
Patient Educ Couns 1997;32(3):175-84. [Rec#: 3433]
Hoelscher TJ, Lichstein KL, Fischer S, et al. Home
relaxation practice in hypertension treatment:
Objective assessment and compliance induction. J of
Consulting and Clinical Psychology 1986;54:217-221.
[Rec#: 2457]
Glasgow RE, Toobert DJ, Hampson SE. Effects of a brief
office-based intervention to facilitate diabetes dietary
self-management. Diabetes Care 1996;19(8):835-42.
[Rec#: 799]
Horlick L, Cameron R, Firor W, et al. The effects of
education and group discussion in the postmyocardial
infarction patient. J Psychosom Res 1984;28:485-492.
[Rec#: 2219]
Glasgow RE, Toobert DJ, Hampson SE, Brown JE,
Lewinsohn PM, Donnelly J. Improving self-care
among older patients with type II diabetes: the "sixty
something...." study. Patient Educ Couns 1992;19:6174. [Rec#: 2212]
Hoskins PL, Fowler PM, Constantino M, et al. Sharing the
care of diabetic patients between hospital and general
practitioners: does it work? Diabetic Medicine
1993;10(1):81. [Rec#: 2597]
157
Accepted Articles
Irvine MJ, Johnson DW, Jenner DA, et al. Relaxation and
stress management in the treatment of essential
hypertension. J of Psychosomatic Res 1986;30:437450. [Rec#: 2458]
Kinmonth AL, Woodcock A, Griffin S, et al. Randomised
controlled trial of patient centered care of diabetes in
general practice: impact on current well-being and
future disease risk. The Diabetes Care From
Diagnosis Research Team. British Medical Journal
1998;317(7167):1202. [Rec#: 2599]
Iso H, Shimamoto T, Tokota K, Sankai T, Jacobs Jr DR,
Komachi Y. Community-based education classes for
hypertension control: A 1.5 year randomized
controlled trial. Hypertension 1996;27:968-974.
[Rec#: 3452]
Korhonen T, Huttnen JK, Aro A, Hentinen M, Ihalainen O,
Majander H, et al. A controlled trial of the effects of
patient education in the treatment of insulin dependent
diabetes. Diabetes Care 1983;6:256-261. [Rec#: 2259]
Jaber LA, Halapy H, Fernet M, et al. Evaluation of a
pharmaceutical care model on diabetes management.
Annals of Pharmacotherapy 1996;30(3):238. [Rec#:
2598]
Kostis JB, Rosen RC, Brondolo E, et al. Superiority of
nonpharmacologic therapy compared to propranolol
and placebo in men with mild hypertension: A
randomised prospective trial. American Heart Journal
1992;123:466-474. [Rec#: 2472]
Jacob RG, Fortmann SP, Kraemer HC, et al. Combining
behavioral treatments to reduce blood pressure: A
controlled outcome study. Behavior Modification
1985;9:32-45. [Rec#: 2459]
Kumana CR/Ma JT, Kung A, Kou M, Lauder I. An
assessment of drug information sheets for diabetic
patients: Only active involvement by patients is
helpful. Diabetes Research and Clinical Practice
1988;5:225-231. [Rec#: 2130]
Jennings PE, Morgan HC, Barnett AH. Improved diabetes
control and knowledge during a diabetic self-help
group. The Diabetes Educator 1987;13:390-393.
[Rec#: 2126]
Laborde JM, Powers MJ. Evaluation of education
interventions for osteoarthritics. Multiple Linear Reg
Viewpoints 1983;12:12-37. [Rec#: 2355]
Jorgensen RS, Houston BK, Zurawski RM. Anxiety
management training in the treatment of essential
hypertension. Behavior Research and Therapy
1981;19:467-474. [Rec#: 2452]
Lagrone R, Jeffrey TB, Ferguson CL. Effects of education
and relaxation training with essential hypertension
patients. J of Clinical Psychology 1988;44:271-276.
[Rec#: 2460]
Kaplan, Wilson, Hartwell/Merino, Wallace. Prospective
evaluation of HDL changes after diet and physical
conditioning programs for patients with Type II
diabetes mellitus. Diabetes Care 1985;8: 343-48.
[Rec#: 2817]
Laitinen JH/Ahola IE/Sarkkinen ES/Winberg RL,
Harmaakorpi-Ilvonen PA, Usitupa MI. Impact of
intensified dietary therapy on energy and nutrient
intakes and fatty acid composition of serum lipids in
patients with recently diagnosed non-insulindependent diabetes mellitus. J Am Diet Assoc
1993;93:276-283. [Rec#: 2176]
Kaplan RM, Hartwell SL, Wilson KD, Wallace JP. Effects
of diet and exercise interventions on control and
quality of life in non-insulin dependent diabetes
mellitus. J Gen Intern Med 1987;2:220-227. [Rec#:
2175]
Leveille SG, Wagner EH, Davis C, Grothaus L, Wallace J,
LoGerfo M, et al. Preventing disability and managing
chronic illness in frail older adults: A randomized trial
of a community-based partnership with primary care.
JAGS 1998;46(10):1-9. [Rec#: 1175]
Keefe F, Caldwell D, Baucom D, et al. Spouse-assisted
coping skills training in the management of
osteoarthritis knee pain. Arthritis Care and Research
1996;9:279. [Rec#: 2082]
Levine DM, Green LW, Deeds SG, Chwalow J, Russell
RP, Finlay J. Health education for hypertensive
patients. JAMA 1979;241:1700-1703. [Rec#: 3453]
Keefe FJ, Caldwell DS, Williams DA, Gil KM, et al. Pain
coping skills training in the management of
osteoarthritic knee pain: A comparative study.
Behavior Therapy 1990b;21:49-62. [Rec#: 908]
Lewin B, Robertson IH, Cay EL, Irving JB, Campbell M.
Effects of self-help post-myocardial-infarction
rehabilitation on psychological adjustment and use of
health services. Lancet 1992;339(8800):1036-40.
[Rec#: 827]
Keefe FJ, Caldwell DS, Williams DA, Gil KM, et al. Pain
coping skills training in the management of
osteoarthritic knee pain-II: Follow-up results.
Behavior Therapy 1990a ;21:435-447. [Rec#: 907]
Litzelman DK, Slemenda CW, Langefeld CD, Hays LM,
Welch MA, Bild DE, et al. Reduction of lower
extremity clinical abnormalities in patients with noninsulin-dependent diabetes mellitus. A randomized,
controlled trial. Ann Intern Med 1993;119(1):36-41.
[Rec#: 828]
Kendall PA, Jansen GR. Educating patients with diabetes:
comparison of nutrient-based and exchanged group
methods. J Am Diet Assoc 1990;90:238-243. [Rec#:
2207]
158
Accepted Articles
Lorig K, Feigenbaum P, Regan C, Ung E, Chastain RL,
Holman HR. A comparison of lay-taught and
professional-taught arthritis self-management courses.
J Rheumatol 1986;13(4 ):763-7. [Rec#: 830]
Mulrow C, Bailey S, Sonksen PH, Slavin B. Evaluation of
an audiovisual diabetes education program: Negative
results of a randomized trial of patients with noninsulin dependent diabetes mellitus. Journal of
General Medicine 1987;2:215-219. [Rec#: 2266]
Lorig K, Lubeck D, Kraines RG, Seleznick M, Holman
HR. Outcomes of self-help education for patients with
arthritis. Arthritis Rheum 1985;28(6):680-5. [Rec#:
835]
Oldenburg B, Allan R, Fastier G. The role of behavioral
and educational interventions in the secondary
prevention of coronary heart disease. In P.F. Lovibond
& P.H. Wilson (Eds), Clinical and Abnormal
Psychology Proceedings of the XXIV International
Congress of Psychology of the International Union of
Psychological Science 1989;429-438. [Rec#: 2698]
Lorig K, Seleznick M, Lubeck D, Ung E, Chastain RL,
Holman HR. The beneficial outcomes of the arthritis
self-management course are not adequately explained
by behavior change. Arthritis Rheum 1989;32(1):91-5.
[Rec#: 837]
Oldenburg B, Perkins RJ, andrews G. Controlled trial of
psychological intervention in myocardial infarction.
Journal of Consulting and Clinical Psychology
1985;53:852-859. [Rec#: 2699]
Lorig KR, Sobel DS, Stewart AL, Brown Jr BW, Bandura
A, Ritter P, et al. Evidence suggesting that a chronic
disease self-management program can improve health
status while reducing hospitalization: A randomized
trial. Medical Care 1999;37(1):5-14. [Rec#: 608]
Oldridge N, Guyatt G, Jones N. Effects of quality of life
with comprehensive rehabilitation after acute
myocardial infarction. Am J Cariol 1991;67:10841089. [Rec#: 2653]
Martinez-Amenos A, Ferre LF, Vidal CM, Rocasalbas JA.
Evaluation of two educative models in a primary care
hypertension program. Journal of Human
Hypertension 1990 ;4:362-4. [Rec#: 3457]
Ott CR, Sivarajan ES, Newton Kmet al. A controlled
randomized study of early cardiac rehabilitation: the
Sickness Impact Profile as an assessment tool. Heart
Lung 1983;12:162-170. [Rec#: 2657]
Mazzuca SA, Moorman NH, Wheeler ML, Norton JA,
Fineberg NS, Vinicor F, et al. The diabetes education
study: A controlled trial of the effects of diabetes
patient education. Diabetes Care 1986;9:1-10. [Rec#:
2132]
Payne TJ, Johnson CA, Penzien DB, Porzelius J, Eldridge
G, Parisi S, et al. Chest pain self-management training
for patients with coronary artery disease. J Psychosom
Res 1994;38(5):409-18. [Rec#: 859]
McCulloch DK, Mitchell RD, Ambler J, Tattersall RB.
Influence of imaginative teaching of diet on
compliance and metabolic control in insulin dependent
diabetes . British Medical Journal 1983;28:1858-1861.
[Rec#: 2264]
Powell LH, Friedman M, Thoresen CE, Gill JJ, Ulmer DK.
Can the Type A behavior pattern be altered after
myocardial infarction? A second year report from the
Recurrent Coronary Prevention Project. Psychosom
med 1984;46(4):293-313. [Rec#: 2361]
Miller NH, Haskell WL, Berra Ket al. Home versus group
exercise training for increasing functional capacity
after myocardial infarction. Circulation 1984;4:645649. [Rec#: 2670]
Pratt C, Wilson W, Leklem J, Kingsley L. Peer support and
nutrition education for older adults with diabetes.
Journal of Nutrition for the Elderly 1987; 6:37-43.
[Rec#: 2139]
Morisky DE, Levine DM, Green LW, et al. Five-year blood
pressure control and mortality following health
education for hypertensive patients. Am J Public
Health 1983;73(2):153-162. [Rec#: 2304]
Rabkin SW, Boyko E, Wilson A, Sreja DA. A randomized
clinical trial comparing behavior modification and
individual counseling in the nutritional therapy of noninsulin-dependent diabetes mellitus: comparison of
the effect on blood sugar, body weight, and serum
lipids. Diabetes Care 1983;6:50-56. [Rec#: 2195]
Morisky DE, Levine DM, Green LW, Russell RP, Smith C,
Benson P, et al. The relative impact of health
education for low- and high-risk patients with
hypertension. Prev Med 1980;9(4):550-8. [Rec#:
3461]
Rahe RM, Ward HW, Hayes V. Brief group therapy in
myocardial infarction rehabilitation: Three to four year
follow-up of a controlled trial. Psychosom Med
1979;41:229-242. [Rec#: 2406]
Muhlhauser I, Sawicki PT, Didjurgeit U, Jorgens V,
Trampisch HJ, Berger M. Evaluation of a structured
treatment and teaching program on hypertension in
general practice. Clin Exp Hypertens 1993;15(1):12542. [Rec#: 3467]
Rainwater N, Ayllon T, Frederiksen LW, Moore EJ, Bonar
JR. Teaching self-management skills to increase diet
compliance in diabetics. In: Stewart RB (Ed.).
Adherence, compliance and generalization in
behavioral medicine. New York: Brunner/Mazel;
1982;304-328. [Rec#: 2140]
159
Accepted Articles
Raz I, Soskolne V, Stein P. Influence of small-group
education sessions on glucose homeostasis in
NIDDM. Diabetes Care 1988;11 :67-71. [Rec#: 2141]
Vanninen E, Uuspitupa M, Siitonen O, Laitinen
J/Lansimies E. Habitual physical activity, aerobic
capacity and metabolic control in patients with newlydiagnosed type 2 (non-insulin-dependent) diabetes
mellitus: effect of 1-year diet and exercise
intervention. Diabetologia 1992;35:340-346. [Rec#:
2174]
Rettig BA, Shrauger DG, Recker RP, Gallagher TF, Wiltse
H. A randomised study of the effects of a home
diabetes education program. Diabetes Care
1986;9:173-178. [Rec#: 2270]
Vinicor F, Cohen SJ, Mazzuca SA, Moorman N, Wheeler
M, Kuebler T, et al. DIABETES: a randomized trial of
the effects of physician and/or patient education on
diabetes patient outcomes. J Chronic Dis
1987;40(4):345-56. [Rec#: 892]
Sadur CN, Moline N, Costa M, Michalik D, Mendlowitz D,
Roller S, et al. Diabetes management in a health
maintenance organization. Efficacy of care
management using cluster visits [In Process Citation].
Diabetes Care 1999;22(12):2011-7. [Rec#: 1668]
Ward WK, Haas LB, Beard JC. A randomized, controlled
comparison of instruction by a diabetes educator
versus self-instruction in self-monitoring of blood
glucose. Diabetes Care 1985;8:284-286. [Rec#: 2152]
Schulte MB, Pluym B, Van Schendel G. Reintegration with
duos: A self-care program following myocardial
infarction. Patients Education and Counseling
1986;8:233-244. [Rec#: 2438]
Watkins CJ, Papacosta AO, Chinn S, Martin J. A
randomized controlled trial of an information booklet
for hypertensive patients in general practice. J R Coll
Gen Pract 1987;37(305):548-50. [Rec#: 3469]
Sivarajan ES, Bruce RA, lindskog BD, Almes MJ, Green
B, Belanger L, et al. Treadmill test responses to an
early exercise program after myocardial infarction: a
randomized study. Circulation 1982;65:1420. [Rec#:
3248]
Weinberger M, Kirkman MS, Samsa GP, Shortliffe EA,
Landsman PB, Cowper PA, et al. A nurse-coordinated
intervention for primary care patients with noninsulin-dependent diabetes mellitus: impact on
glycemic control and health-related quality of life [see
comments]. J Gen Intern Med 1995;10 (2):59-66.
[Rec#: 896]
Sivarajan ES, Newton KM, Almes MJ, et al. Limited
effects of outpatient teaching and counseling after
myocardial infarction: A controlled study. Heart and
Lung 1983;12:65-73. [Rec#: 2439]
Southam MA, Agras WS, Taylor CB, et al. Relaxation
training: Blood pressure lowering during the working
day. Archives of General Psychiatry 1982;39:715-717.
[Rec#: 2453]
Weinberger M, Tierney WM, Booher P, Katz BP. Can the
provision of information to patients with osteoarthritis
improve functional status? A randomized, controlled
trial. Arthritis Rheum 1989;32(12):1577-83. [Rec#:
430]
Stahl SM, Kelley CR, Neill PJ, Grim CE, Mamlin J. Effects
of home blood pressure measurement on long-term BP
control. Am J Public Health 1984;74(7):704-9. [Rec#:
3466]
Weinberger M, Tierney WM, Booher P, Katz BP. The
impact of increased contact on psychosocial outcomes
in patients with osteoarthritis: a randomized,
controlled trial. J Rheumatol 1991;18(6):849-54.
[Rec#: 898]
Stern MJ, Gorman PA, Kaslow . The group counseling vs.
exercise therapy study: A controlled intervention with
subjects following myocardial infarction. Arch Intern
Med 1983;143:1719-1725. [Rec#: 2377]
Werdier JD, Jesdinsky HJ, Helmich P. A randomized
controlled study on the effect of diabetes counseling in
the offices on 12 general practitioners. Rev Epidemiol
Med Sante Publique 1984;32:225-229. [Rec#: 2401]
Stevens J, Burgess MB, Kaiser Dl, Sheppa CM. Outpatient
management of diabetes mellitus with patient
education to increase carbohydrate and fiber. Diabetes
Care 1985;8:359-366. [Rec#: 2208]
Wheeler LA, Wheeler ML, Ours P, Swider C. Evaluation
of computer-based diet education in persons with
diabetes mellitus and limited educational background.
Diabetes Care 1985;8(6):537-44. [Rec#: 3442]
Taylor CB, Farquhar JW, Nelson E, et al. Relaxation
therapy and high blood pressure. Arch General
Psychiatry 1977;34:339-342. [Rec#: 2464]
White N, Carnahan J, Nugent CA, iwaoka T, Dodsono MA.
Management of obese patients with diabetes mellitus:
comparison of advice education with group
management. Diabetes Care 1986;9:490-496. [Rec#:
2154]
Turner L, Linden W, van der Wal R, Schamberger W.
Stress management for patients with heart disease: a
pilot study. Heart Lung 1995;24(2):145-53. [Rec#:
887]
160
Accepted Articles
Wilson W, Pratt C. The impact of diabetes education and
peer support upon weight and glycemic control of
elderly persons with non-insulin dependent diabetes
mellitus (NIDDM). Am J Public Health
1987;77(5):634-5. [Rec#: 900]
Wing RR, Epstein LH, Nowalk MP, Scott N, Koeski R.
Self-regulation in the treatment of Type II diabetes.
Behavior Therapy 1988; 19 :11-23. [Rec#: 2283]
Wing RR/Epstein LH, Nowalk MP, Koeske R, Hagg S.
Behavior change, weight loss and physiological
improvements in Type II diabetic patients. Journal of
Consulting and Clinical Psychology 1985;53:11-122.
[Rec#: 2156]
Wing RR/Epstein LH, Nowalk MP, Scott N, Koeske R,
Hagg S. Does self-monitoring of blood glucose levels
improve dietary compliance for obese patients with
Type II diabetes? The American Journal of Medicine
1986;81:830-836. [Rec#: 2158]
Wise PH, Dowlatshahi DC, Farrant S, Fromson
SS/Meadows KA. Effect of computer-based learning
on diabetes knowledge and control. Diabetes Care
1986;9:504-508. [Rec#: 2205]
Wood ER. Evaluation of a hospital-based education
program for patients with diabetes. Journal of the
American Dietetic Association 1989;89:354-358.
[Rec#: 2159]
Worth R, Home PD, Johston DG, Anderson J, Ashworth L,
Burrin JM, et al. Intensive attention improves
glycemic control in insulin-dependent diabetes
without further advantage from home glucose
monitoring: results of a controlled trial. BMJ
1982;285:1233-1240. [Rec#: 2198]
161
APPENDIX C. REJECTED ARTICLES
Coronary heart disease death, nonfatal acute myocardial
infarction and other clinical outcomes in the Multiple
Risk Factor Intervention Trial. Multiple Risk Factor
Intervention Trial Research Group. Am J Cardiol
1986;58(1):1-13. [Rec#: 851]
Task Force to Revise the National Standards: National
standards for diabetes self-management education
programs. Diabetes Care 1998;18:141-143. [Rec#:
2170]
Tight blood pressure control and risk of macrovascular and
microvascular complications in type 2 diabetes:
UKPDS 38. UK Prospective Diabetes Study Group.
BMJ 1998;317(7160):703-13. [Rec#: 3428]
Disease management program improves diabetes outcomes,
curbs hospital costs, utilization. Health Care Cost
Reengineering Report 1998;3(3):42-45. [Rec#: 2615]
Effect of intensive blood-glucose control with metformin
on complications in overweight patients with type 2
diabetes (UKPDS 34). UK Prospective Diabetes Study
(UKPDS) Group. Lancet 1998;352(9131):854-65.
[Rec#: 3426]
ACPJournal Club. Review: Several interventions reduce
complications in type 2 diabetes mellitus. ACP J Club
1998;128:30. [Rec#: 2577]
Adamson TEGullion DS. Assessment of diabetes
continuing medical education. Diabetes Care
1986;9(1):11. [Rec#: 2578]
The effect of intensive treatment of diabetes on the
development and progression of long-term
complications in insulin-dependent diabetes mellitus.
The Diabetes Control and Complications Trial
Research Group. N Engl J Med 1993;329(14):977-86.
[Rec#: 3444]
Adsett CA, Bruhn JG. Short-term group psychotherapy for
post-myocardial infarction patients and their wives.
Can Med Assoc J 1968;99 :577. [Rec#: 2372]
Alaranta H, Rytokoski U, Rissanen A, Talo S, Ronnemaa
T, Puukka P, et al. Intensive physical and psychosocial
training program for patients with chronic low back
pain. A controlled clinical trial. Spine 1994;19
(12):1339-49. [Rec#: 743]
Effectiveness of routine self-monitoring of peak flow in
patients with asthma. Grampian Asthma Study of
Integrated Care (GRASSIC) [see comments]. BMJ
1994;308(6928):564-7. [Rec#: 929]
Albero RAcha JSanza Aet al. Metabolic improvement of
diabetes mellitus through pamphlets on the norms of
self-monitoring control measures. Atencion Primaria
1993;12(8):475. [Rec#: 2579]
The effects of nonpharmacologic interventions on blood
pressure of persons with high normal levels. Results of
the Trials of Hypertension Prevention, Phase I
[published erratum appears in JAMA 1992 May
6;267(17):2330] [see comments]. JAMA
1992;267(9):1213-20. [Rec#: 885]
Ali NS, Khali HZ. Effect of psycho-educational
intervention on anxiety among Egyptian bladder
cancer patients. Cancer Nursing 1989;12 :236-242.
[Rec#: 2311]
Intensive blood-glucose control with sulphonylureas or
insulin compared with conventional treatment and risk
of complications in patients with type 2 diabetes
(UKPDS 33). UK Prospective Diabetes Study
(UKPDS) Group. Lancet 1998;352(9131):837-53.
[Rec#: 3427]
Allen RM, Jones MP, Oldenburg B. Randomised trial of an
asthma self-management program for adults. Thorax
1995;50(7):731-8. [Rec#: 923]
National Standards for Diabetes Self-Management
Education Programs. Task Force to Revise the
National Standards. The American Diabetes
Association. Diabetes Educ 1995;21 (3):189-90, 193.
[Rec#: 3414]
Altmaier EM, Lehmann TR, Russell DW, Weinstein JN,
Kao CF. The effectiveness of psychological
interventions for the rehabilitation of low back pain: a
randomized controlled trial evaluation. Pain
1992;49(3):329-35. [Rec#: 744]
New study confirms benefit of disease management for less
severe cases of diabetes. Healthcare Demand and
Disease Management 1998 ;4(8 ):120-122. [Rec#:
2616]
Altman DG. A framework for evaluating community based
heart disease prevention programs. Soc Sci Med
1986;22:479-487. [Rec#: 2659]
Ambrosiadou BV, Goulis DG, Pappas C. Clinical
evaluation of the DIABETES expert system for
decision support by multiple regimen insulin dose
adjustment. Comput Methods Programs Biomed
1996;49(1):105-15. [Rec#: 3432]
Review: Self-management education for adults with asthma
improves health outcomes. Evidence-Based Medicine
1999;4:15. [Rec#: 740]
162
Rejected Articles
Task Force on Financing Quality Health Care for Persons
with Diabetes. VA: American Diabetes Association,
Inc. [Rec#: 2440]
Arnold MSButler PMAnderosn RMet al. Guidelines for
facilitating a patient empowerment program. Diabetes
Educator 1995;21(4):308. [Rec#: 2580]
American Diabetes Association. Management of
dyslipidemia in adults with diabetes. Diabetes Care
2001;24(Suppl 1):S58-61. [Rec#: 3430]
Assal JP, Muhlauser I, Pernot A, Gfeller R, Jorgens V,
Berger M. Patient education as the basis for diabetes
care in clinical practice and research. Diabetologia
1985 ;28:602-613. [Rec#: 2104]
American Diabetes Association. Nutrition
recommendations and principles for people with
diabetes mellitus. Diabetes Care 2001;24(Suppl
1):S44-7. [Rec#: 3429]
Atkins CJ, Kaplin RM, Timms RM, et al. Behavioral
exercise programs in the management of chronic
obstructive pulmonary disease. J of Consulting and
Clinical Psychology 1984;52:591-603. [Rec#: 2474]
Amorasa-Tupler B, Tapp JT, Cardia RV. Stress
management through relaxation and imagery in the
treatment of angina pectoris. J Cardiopulmon Rehab
1989;9:348-355. [Rec#: 2686]
Ayres JG, Campbell LM. A controlled assessment of an
asthma self-management plan involving a budesonide
dose regimen. OPTIONS Research Group. Eur Respir
J 1996;9(5):886-92. [Rec#: 924]
Anderson BJ, Auslander WF. Research on diabetes
management and the family: A critique. Diabetes Care
1980;3:696-702. [Rec#: 2220]
Baile WF, Engel BT. A behavioral strategy for promoting
treatment compliance following myocardial infarction.
Psychosom Med 1978;40 :413-419. [Rec#: 2410]
Anderson BJ, Miller JP, Auslander Wf, Santiago JV.
Family characteristics of diabetic adolescents:
Relationship to metabolic control. Diabetes Care
1981;4:580-594. [Rec#: 2221]
Bailey WC, Richards JM, Manzella BA, Windsor RA,
Brooks CM, Soong-S-J. Promoting self-management
in adults with asthma: An overview of the UAB
program. Health Educ Q 1987;14(3):345-356. [Rec#:
2165]
Anderson RM. The personal meaning of having diabetes:
implications for patient behavior and education or
kicking the bucket theory. Diabet Med 1986;3(1): 859. [Rec#: 745]
Bailey WC, Richards JM Jr, Brooks CM, Soong SJ,
Windsor RA, Manzella BA. A randomized trial to
improve self-management practices of adults with
asthma. Arch Intern Med 1990;150(8):1664-8. [Rec#:
750]
Anderson RM, Fitzgerald JT, Funnell MM, Barr PA,
Stepien CJ, Hiss RG, et al. Evaluation of an activated
patient diabetes education newsletter. Diabetes Educ
1994;20(1):29-34. [Rec#: 746]
Baker AM, Lafata JE, Ward RE, Whitehouse F, Divine G.
A Web-based diabetes care management support
system. Jt Comm J Qual Improv 2001;27(4):179-90.
[Rec#: 3434]
Anderson RM, Funnell MM, Barr PA, Dendrick RF, Davis
WF. Lerning to empower patients: the results of a
professional education program for diabetes educators.
Diabetes Care 1991;14:584-90. [Rec#: 2636]
Baker SBVallbona CPavlik Vet al. A diabetes control
program in a public health care setting. Public Health
Reports 1993;108(5):595. [Rec#: 2582]
Arathuzik D. Effects of cognitive-behavioral strategies on
pain in cancer patients. Cancer Nurs 1994;17(3):20714. [Rec#: 748]
Bann HF. Evaluation of glycosylated hemoglobin in
diabetic patients. Diabetes 1981;30:613-617. [Rec#:
2222]
Archterberg J, McGraw P, Lawlis GF. Rheumatoid
arthritis: a study of relaxation and temperature
biofeedback training as an adjunctive therapy.
Biofeedback Self-Regul 1981;6:207-223. [Rec#:
2357]
Barlow JH, Barefoot J. Group education for people with
arthritis. Patient Educ Couns 1996;27(3 ):257-67.
[Rec#: 3277]
Archuleta V, Plummer OB, Hopkins KD. Chapter VI and
VII, pp. 63-108. In: A demonstration model for
patient education: A model for the project "Training
Nurses to Improve Patient Education". Boulder,
Project Report: Western State Commission for Higher
Education; 1977. [Rec#: 2359]
Barlow JH, Turner AP, Wright CC. Long-term outcomes of
an arthritis self-management program. Br J Rheumatol
1998;37(12):1315-9. [Rec#: 3275]
Barlow JH, Wright CC. Knowledge in patients with
rheumatoid arthritis: a longer-term follow-up of a
randomized controlled study of patient education
leaflets. Br J Rheumatol 1998;37(4):373-6. [Rec#:
3276]
Argo JK, Singh RH, Ostapchenko G. A competency based
diabetes diet program. The Diabetes Educator
1983;9(1):21. [Rec#: 2103]
163
Rejected Articles
Barnard J, Lattimore L, Holly RG, et al. Response to noninsulin-dependent diabetic patients to an intensive
program or diet and exercise. Diabetes Care
1982;5:370-374. [Rec#: 2382]
Blumenthal JA, Thyrum ET, Gullette ED, Sherwood A,
Waugh R. Do exercise and weight loss reduce blood
pressure in patients with mild hypertension? N C Med
J 1995;56(2):92-5. [Rec#: 753]
Barnard J, Massey MR, Cherny S, O'Brien LT, Pritikin N.
Long-term use of a high-complex carbohydrate, highfiber, low-fat diet and exercise in the treatment of
NIDDM patients. Diabetes Care 1983;(268-273.).
[Rec#: 2381]
Bobrow ES, Avrusking TW, Siller J. Mother-daughter
interaction and adherence to diabetes regimens.
Diabetes Care 1985;8:146-151. [Rec#: 2225]
Bohachick P. Progressive relaxation training in cardiac
rehabilitation: effect on psychological variables. Nurs
Res 1984;33:283-287. [Rec#: 2696]
Bartholomew LK, Parcel GS, Seilheimer DK, Czyzewski
D, Spinelli SH, Congdon B. Development of a health
education program to promote the self- management
of cystic fibrosis. Health Educ Q 1991;18(4):429-43.
[Rec#: 751]
Bolton MB, Tilley BC, Kuder J, Reeves T, Schultz LR. The
cost and effectiveness of an education program for
adults who have asthma. J Gen Intern Med
1991;6(5):401-7. [Rec#: 755]
Basler HD, Rehfisch HP. Follow-up results of a cognitivebehavioral treatment for chronic pain in a primary care
setting. Psychol Health 1990;4:293-304. [Rec#: 903]
Bone RC. The bottom line in asthma management is patient
education. Am J Med 1993;94(6):561-3. [Rec#: 756]
Bowen RG, Rich R, Schlotfeldt RM. Effects of organized
instruction for patients with the diagnosis of diabetes
mellitus. Nursing Research 196;10:151-159. [Rec#:
2106]
Beaser SM. Teaching the diabetic patient. Diabetes
1956;5:146--149. [Rec#: 2707]
Becker MH, Maiman LA. Socio behavioral determinants of
compliance with health and medical care
recommendations. Medical Care 1975;13:10-14.
[Rec#: 2224]
Braden C, McGlone K, Pennington F. Specific
psychosocial and behavioral outcomes from the
systemic lupus erythematosus self-help course. Health
Education Quarterly 1993 ;20:29. [Rec#: 2075]
Beebe C, Fischer B, McCracken S. Lifestyle change: A
new approach to treatment of obese type II diabetes.
Diabetes 1804;33:6A. [Rec#: 2846]
Bradley L, Young L, Anderson Ket al. Effects of cognitivebehavior therapy on rheumatoid arthritis pain
behavior: One-year follow-up. In: Dubner R, Gebhart
G, Bond M. Pain Research and Clinical Management
(Proceedings of the 5th World Congress on Pain).
Amsterdam: Elsevier; 1988; 310. [Rec#: 2076]
Beeney LJ, Dunn SM. Knowledge improvement and
metabolic control in diabetes education: approaching
the limits? Patient Educ Couns 1990;16(3):217. [Rec#:
2089]
Beggan MP, Cregan D, Drury MI. Assessment of the
outcome of an educational program of diabetes selfcare. Diabetologie 1982;23 :246-251. [Rec#: 2664]
Bradley LA, Turner RA, Young LD, et al. Effects of
cognitive behavioral therapy on pain behavior or
rheumatoid arthritis (RA) patients: preliminary
outcomes. Scan J Behav Ther 1985;14:51-64. [Rec#:
2358]
Benson H, Rosner BA, Marzetta BR, et al. Decreased blood
pressure in borderline hypertensive subjects who
practiced meditation. J Chronic Diseases 1974;
27:163-169. [Rec#: 2465]
Bradley LA, Young LD, Anderson KO, et al. Psychological
approaches to the management of arthritis pain. Soc
Sci Med 1984;19:1353-1360. [Rec#: 2351]
Berg J, Dunbar-Jacob J, Sereika SM. An evaluation of a
self-management program for adults with asthma. Clin
Nurs Res 1997;6(3):225-38. [Rec#: 925]
Bradley LA, Young LD, Anderson KO, Turner RA,
Agudelo CA, McDaniel LK, et al. Effects of
psychological therapy on pain behavior of rheumatoid
arthritis patients. Treatment outcome and six-month
follow-up. Arthritis Rheum 1987;30(10):1105-14.
[Rec#: 757]
Berger M. Evaluation of a teaching and treatment program
for type I diabetic patients. Diabetic Educ 1984;(3638.). [Rec#: 2383]
Bernbaum MAlbert SGBrusca SRet al. A model clinical
program for patients with diabetes and vision
impairment. Diabetes Educator 1989;15(4):325.
[Rec#: 2583]
Brewin AM, Hughes JA. Effect of patient education on
asthma management. Br J Nurs 1995;4(2):81-2, 99101. [Rec#: 926]
Bridge LR, Benson P, Pietroni PC, Priest RG. Relaxation
and imagery in the treatment of breast cancer. BMJ
1988;297(6657):1169-72. [Rec#: 758]
Bindemann S, Soukop M, Kaye SB. Randomised controlled
study of relaxation training. European Journal of
Cancer 1991;27:170-174. [Rec#: 2312]
164
Rejected Articles
Brock AM. A study to determine the effectiveness of a
learning activity package for the adult with diabetes
mellitus. Journal of Advanced Nursing 1978;3:265275. [Rec#: 2107]
Brownlee MA, Cerami A. The biochemistry of the
complications of diabetes mellitus. Annual Review of
Biochemistry 1981;50:358-432. [Rec#: 2226]
Brun JG, Philips BU. Measuring social support: A
synthesis of current approaches. Journal of Behavioral
Medicine 1984;7:151-169. [Rec#: 2228]
Broderick JE. Mind-body medicine in rheumatological
disease. Rheumatic Disease Clinics of North America
1999. [Rec#: 609]
Bruno R, Arnold C, Jacobson L, Winick M, Wynder E.
Randomized controlled trial of a nonpharmacologic
cholesterol reduction program at the worksite. Prev
Med 1983;12(4):523-32. [Rec#: 722]
Brough FK, Schmidt CD, Rasmussen T, et al. Comparison
of two teaching methods for self-care training for
patients with chronic obstructive pulmonary disease.
Patient Counseling and Health Education
1982;4(2):111-116. [Rec#: 2424]
Burish TG, Carey MP, Krozely MG, Greco FA.
Conditioned side effects induced by cancer
chemotherapy: Prevention through behavioral
treatment. Journal of Consulting and Clinical
Psychology 1987;55:42-48. [Rec#: 2313]
Brown SA. Effects of educational interventions and
outcomes in diabetic adults: a meta-analysis revisited.
Patient Educ Counseling 1990;16:189-215. [Rec#:
2638]
Burish TG, Jenkins RA. Effectiveness of biofeedback and
relaxation training in reducing the side effects of
cancer chemotherapy. Health Psychology 1992; 11:1723. [Rec#: 2314]
Brown SA. Effects of educational interventions in diabetes
care: a meta-analysis of findings. Nurs Res
1988;37:223-230. [Rec#: 2090]
Brown SA. Effects of educational interventions in diabetes
care: a meta-analysis of findings. Nurs Res
1988;37(4):223-30. [Rec#: 3403]
Burish TG, Lyles JN. Effectiveness of relaxation training in
reducing adverse reactions to cancer chemotherapy.
Journal of Behavioral Medicine 1981;4:65-78. [Rec#:
2315]
Brown SA. Measurement of quality of primary studies for
meta-analysis. Nursing Research 1991;40(6):352.
[Rec#: 2093]
Burish TG, Snyder SL, Jenkins RA. Preparing patients for
cancer chemotherapy: Effect of coping preparation
and relaxation interventions . Journal of Consulting
and Clinical Psychology 1991;59:518-525. [Rec#:
2316]
Brown SA. Meta-analysis of diabetes patient education
research: variations in intervention effects across
studies. Res Nurs Health 1992;15(6):409-19. [Rec#:
759]
Burnett KF, Taylor CB, Agras WS. Computer assisted
management of weight, diet, and exercise in the
treatment of Type II diabetes. Diabetes Educator
1987;13:234-236. [Rec#: 2229]
Brown SA. Studies of educational interventions and
outcomes in diabetic adults: a meta-analysis revised.
Patient Educ Couns 1990;16:189-215. [Rec#: 2086]
Burton WNConnerty CM. Evaluation of a worksite-based
patient education intervention targeted at employees
with diabetes mellitus. Journal of Occupational &
Environmental Medicine 1998;40(8):702. [Rec#:
2585]
Brown SA. Studies of educational interventions and
outcomes in diabetic adults: a meta-analysis revisited.
Patient Educ Couns 1990;16(3):189-215. [Rec#: 760]
Brown SAHanis CL. A community-based, culturally
sensitive education and group-support intervention for
Mexican Americans with NIDDM: a pilot study of
efficacy. Diabetes Educator 1995;21(3):203. [Rec#:
2584]
Bush MA. Compliance, education, and diabetes control. Mt
Sinai J Med 1987;54(3):221-7. [Rec#: 3441]
Buysschaert M, Lepair-Gadiseus N, Weil R, Vandeleene B,
Leonet J, Lambert AE. Effect of an in-patient
education program upon the knowledge, behavior and
glycemic control of insulin-dependent diabetic
patients. Diabete and Metabolism 1987;13:31-36.
[Rec#: 2230]
Brownell KD, Kramer FM. Behavioral management of
obesity. Medical Clinics of North America
1989;73:185-201. [Rec#: 2642]
Brownlee-Duffeck M, Peterson L, Simonds J, Goldstein D,
Kilo C, Hoette S. The role of health beliefs and
regimen adherence and metabolic control of
adolescents and adults with diabetes mellitus. Journal
of Consulting and Clinical Psychology 1987;55:139144. [Rec#: 2227]
Cain EN, Kohorn EI, Quinlan DM, Latimer K, Schwartz
PE. Psychosocial benefits of a cancer support group.
Cancer 57:183-189. [Rec#: 2317]
Cameron K, Gregor F. Chronic illness and compliance. J
Adv Nurs 1987;12(6):671-6. [Rec#: 761 ]
165
Rejected Articles
Campbell LV. Evaluation of the benefits of a diabetes
education program. Diabetes Educ 1984;10:46-47.
[Rec#: 2666]
Charlton I, Charlton G, Broomfield J, Mullee MA.
Evaluation of peak flow and symptoms only selfmanagement plans for control of asthma in general
practice. Br Med J;1990(301):1355-1359. [Rec#:
2167]
Campbell MK, DeVellis BM, Strecher VJ, Ammerman AS,
DeVellis RF, Sandler Rs. Improving dietary behavior:
the effectiveness of tailored messages in primary care
settings. Am J Public Health 1994;84:783-787. [Rec#:
2689]
Christensen NK, Terry RD, Wyatt S, Pichert JW, Lorenz
RW. Quantitive assessment of dietary adherence in
patients with insulin-dependent diabetes mellitus.
Diabetes Care 1983;6:245-250. [Rec#: 2232]
Cannici J, Malcolm R, Peek LA. Treatment of insomnia in
cancer patients using muscle relaxation training.
Journal of Behavior Therapy and Experimental
Psychiatry 1983;14:251-256. [Rec#: 2318]
Clark NM. Asthma self-management education. Research
and implications for clinical practice. Chest 1989;95(
5):1110-3. [Rec#: 763]
Carey MP, Burish TG. Providing relaxation training to
cancer chemotherapy patients: A comparison of three
delivery techniques. Journal of Consulting and
Clinical Psychology 1987;55:732-737. [Rec#: 2319]
Clark NM, Becker MH, Janz NK, Lorig K, Rakowski W,
Anderson L. Self-management of chronic disease by
older adults: A review and questions for research. J
Aging Health 1991;3:3-27. [Rec#: 904]
Carlson A, Rosenquist U. Diabetes Care Organization,
Process, and Patient Outcomes: Effects of a Diabetes
Control Program. Diabetes Education 1991;1:42-8.
[Rec#: 2417]
Clark NM, Evans D, Zimmerman BJ, Levison MJ, Mellins
RB. Patient and family management of asthma:
theory-based techniques for the clinician. J Asthma
1994;31(6):427-35. [Rec#: 764]
Carlson A, Rosenquist U. Diabetes Control Program
Implementation. On the Importance of Staff
Involvement. Scandinavian J of Primary Health Care
(suppl 1):105-12. [Rec#: 2416]
Clark NM, Janz NK, Becker MH, Schork MA, Wheeler J,
Liang J, et al. Impact of self-management education
on the functional health status of older adults with
heart disease. Gerontologist 1992;32( 4):438-43.
[Rec#: 765]
Carlson A, Rosenqvist U. Locally developed plans for
quality diabetes care. Worker and consumer
participation in the public health care system. Health
Educ Res 1990;5(1):41-51. [Rec#: 3086]
Clark NM, Janz NK, Dodge JA, Garrity CR. Managing
heart disease: a study of the experiences of older
women. J Am Med Women’s Assoc 1994;49(6):2026. [Rec#: 766]
Carney RM, Schechter K, Davis T. Improving adherence to
blood glucose testing in insulin-dependent diabetic
children. Behavior Therapy 1983;24:247-254. [Rec#:
2231]
Clark NM, Janz NK, Dodge JA, Sharpe PA. Self-regulation
of health behavior: the "take PRIDE" program. Health
Educ Q 1992;19(3):341-54. [Rec#: 767]
Carson MA, Hathaway A, Tuohey JP, et al. The effect of a
relaxation technique on coronary risk factors.
Behavioral Medicine 1988;14:71-77. [Rec#: 2450]
Clark NM, Rakowski W, Ostrander L, et al. Development
of self-management education for elderly heart
patients. Gerontologist 1988;28 :491-494. [Rec#:
2425]
Case RB, heller SS, Case NB, Moss AJ, Multicenter PostInfarction Research Group. Type A behavior and
survival after acute myocardial infarction. N Engl J
Med 1985;312:737-741. [Rec#: 2363]
Clark NM, Starr-Schneidkraut NJ. Management of asthma
by patients and families. Am J Respir Crit Care Med
1994;149(2 Pt 2):S54-66; discussion S67-8. [Rec#:
768]
Cassem NH, hacket TP. Psychological rehabilitation of
myocardial infarction patients in the acute phase.
Heart Lung 1973;2:382-38. [Rec#: 2409]
Clement S. Diabetes self-management education. Diabetes
Care 1995;18(8):1204-14. [Rec#: 769]
Clement S. Diabetes self-management education. Diabetes
Care 1995;18(8):1204-14. [Rec#: 3417]
Caudill M, Schnable R, Zuttermeister P, Benson H,
Friedman R. Decreased clinic utilization by chronic
pain patients after behavioral medicine intervention.
Pain 1991;45(3):334-5. [Rec#: 762]
Coehn M, Zimmet P. Self-monitoring of blood glucose
levels in a non-insulin dependent diabetes mellitus.
Med J Aust 1983;2:377-380. [Rec#: 2386]
Chandalia HB, Bragodia J. Effect of nutritional counseling
on the blood glucose and nutritional knowledge of
diabetic subjects. Diabetes Care 1979;2:353-356.
[Rec#: 2385]
Cohen AS, Vance VK, Runyan JWJ, Horwitz D. Diabetic
acidosis: An evaluation of the cause, course and
therapy of 73 cases. Anals of Internal Medicine
1960;52:55-86. [Rec#: 2233]
166
Rejected Articles
Cohen JL, Sauter S, DeVellis RF, DeVellis BM .
Evaluation of arthritis self-management courses led by
laypersons and by professionals. Arthritis Rheum
1986;29:388-393. [Rec#: 2658]
Cox DJ, Gonder-Frederick L, Julian DM, Clarke W. Longterm follow-up evaluation of blood glucose awareness
training. Diabetes Care 1997;17:1-5. [Rec#: 2203]
Cox DJ, Gonder-Frederick L, Polonsky W, Schlundt D,
Kovatchev B, Clarke W. Blood glucose awareness
training (BGAT-2): long-term benefits. Diabetes Care
2001;24(4):637-42. [Rec#: 3406]
Cohen M, Zimmet P. Self-monitoring of blood glucose
levels in non-insulin-dependent diabetes mellitus. Med
J Aust 1983;1983(2):377-380. [Rec#: 2716]
Cohen RY. The evaluation of a community-based group
program for low-income diabetics and hypertensives.
Am J Community Psychol 1982;10:524-539. [Rec#:
2192]
Crowther JH. Stress management training and relaxation
imagery in the treatment of essential hypertension. J of
Behavioral Medicine 1983;6:169-187. [Rec#: 2451]
Cupples ME, McKnight A. Randomised controlled trial of
health promotion in general practice for patients at
high cardiovascular risk. BMJ 1994;309(6960):993-6.
[Rec#: 3459]
Cohen S, Wallis TA. Stress, social support, and the
buffering hypothesis . Psychological Bulletin
1985;98:310-357. [Rec#: 2234]
Collier JH. Developmental and systems perspectives on
chronic illness. Holist Nurs Pract 1990;5(1):1-9.
[Rec#: 771]
D'Souza W, Crane J, Burgess C, Te Karu H, Fox C, Harper
M, et al. Community-based asthma care: trial of a
"credit card" asthma self- management plan. Eur
Respir J 1994 ;7(7 ):1260-5. [Rec#: 777]
Collins RW, Anderson JW. Medication cost savings
associated with weight loss for obese non- insulindependent diabetic men and women. Prev Med
1995;24(4):369-74. [Rec#: 3435]
Dalton JA. Education for pain management: A pilot study.
Patient Education and Counseling 1987;9:155-165.
[Rec#: 2321]
Connelly CE. An empirical study of a model of self-care in
chronic illness. Clin Nurse Spec 1993; 7(5): 247-53.
[Rec#: 772]
Daugherty SA. Hypertension detection and follow-up
program cooperative group: Mortality findings beyond
five years in the hypertension detection and follow-up
program (HDFP). J of Hypertension 1988;6(suppl
4):S597-S601. [Rec#: 2449]
Connelly CE. Self-care and the chronically ill patient. Nurs
Clin North Am 1987;2, 2(3):621-9. [Rec#: 773]
Cotanch PH, Strum S. Progressive muscle relaxation as
antiemic therapy for cancer patients. Oncology
Nursing Forum 1987;14(1):33-37. [Rec#: 2320]
Daughtry SBMagner J. Physician standards of diabetes
care. Results from the North Carolina Diabetes
Control Pilot Project. North Carolina Medical Journal
1994;55(7):281. [Rec#: 2587]
Cote J, Cartier A, Robichaud P, Boutin H, Malo JL,
Rouleau M, et al. Influence on asthma morbidity of
asthma education programs based on self-management
plans following treatment optimization. Am J Respir
Crit Care Med 1997;155(5):1509-14. [Rec#: 927]
Davidson D, Winchester M, Taylor C, Alderman E, Ingels
N. Effects of relaxation therapy and cardiac
performance and sympathetic activity in patients with
organic heart disease. Psychosom Med 1979;41:303309. [Rec#: 2695]
Cott A, Anchel H, Goldberg WM, Fabich M, Parkinson W.
Non-institutional treatment of chronic pain by field
management: an outcome study with comparison
group. Pain 1990;40(2):183-94. [Rec#: 774]
Davis H. Effects of biofeedback and cognitive therapy on
stree in patients with breast cancer. Psychological
Reports 1986;59 :967-974. [Rec#: 2322]
Cowie RL, Revitt SG, Underwood MF, Field SK. The
effect of a peak flow-based action plan in the
prevention of exacerbations of asthma. Chest
1997;112(6):1534-8. [Rec#: 928]
de Sonnaville JJBouma MColly LPet al. Sustained good
glycemic control in NIDDM patients by
implementation of structured care in general practice:
2-year follow-up study. Diabetologia
1997;40(11):1334. [Rec#: 2588]
Cox D, Taylor A, Nowacek G, Holley-Wilcox P, Pohl S.
The relationship between psychological stress and
insulin-dependent diabetic blood glucose control:
Preliminary investigations. Health Psychology 1984;3
:63-75. [Rec#: 2235]
de Weerdt I, Visser A, van der Veen EA. Attitude behavior
theories and diabetes education programs. Patient
Education and Counseling 1989;14:3-19. [Rec#: 3418]
de Weerdt I, Visser AP, Kok GJ, et al. Randomized
controlled multi-centre evaluation of an education
program for insulin-treated diabetic patients: effects
on metabolic control, quality of life, and costs of
therapy. Diabetic Medicine 1991;8(4):338. [Rec#:
2589]
Cox DJ, Gonder-Frederick L. Major developments in
behavioral diabetes research. Journal of Consulting
and Clinical Psychology 1992;60(4):628-638. [Rec#:
2441]
167
Rejected Articles
Decker TW, Cline-Elsen J, Gallagher M. Relaxation
therapy as an adjunct in radiation oncology. Journal of
Clinical Psychology 1992;48:388-393. [Rec#: 2323]
Dubbert PM, Rappaport NB, Martin JE. Exercise in
cardiovascular disease. Behavior Modification
1987;11:329-347. [Rec#: 2643]
DeLawter DE. Diabetes education at a community hospital.
Maryland Medical Journal 1987;36:837-841. [Rec#:
2109]
Dudley JD. The diabetes educator's role in teaching the
diabetic patient. Diabetes Care 1980;3:127-133.
[Rec#: 2709]
Dennis KE, Goldberg AP. Differential effects of body
fatness and body fat distribution on risk factor for
cardiovascular disease in women. Impact of weight
loss. Arterioscler Thromb 1993;13(10):1487-94.
[Rec#: 3478]
Dunn SM. Reactions to educational techniques: coping
strategies for diabetes and learning. Diabet Med
1986;3(5):419-29. [Rec#: 3439]
Dunn SM. Rethinking the models and modes of diabetes
education. Patient Educ Couns 1990;16(3):281-6.
[Rec#: 778]
Denver DR, Vaveault D, Girard F, Lacourciere Y,
Laturlippe L, Grove RN, et al. Behavioral medicine:
biobehavioral effects of short-term thermal
biofeedback and relaxation in rheumatoid arthritic
patients (abstract). Biofeedback Self-Regul
1979;4:245-245. [Rec#: 2683]
Dunn SM, Bryson JM, Hoskins PL, Alford JB,
Handelsman DJ, Turtle JR. Development of the
diabetic knowledge (DKN) scales: Forms KDNA,
DKNB, and DKNC. Diabetes Care 1984;7(1):36.
[Rec#: 2117]
DeVellis BM, Blalock SJ, Hahn PM, et al. Evaluation of a
problem-solving intervention for patients with
arthritis. Patient Education and Counseling
1988;11:29-42. [Rec#: 2426]
Dupuis A. Assessment of the psychological factors and
responses in self-managed patients. Diabetes Care
1980;3:117-120. [Rec#: 2387]
Dupuis A, jones RL, Peterson CM. Psychological effects of
blood glucose self-monitoring in diabetic patients.
Psychosomatics 1980;21:581-591. [Rec#: 2388]
Diehl AK, Bauer RL, Sugarek NJ. Correlates of medication
compliance in non insulin-dependent diabetes
mellitus. Southern Medical Journal 1987;80:332-335.
[Rec#: 2236]
Eardley A. Patients' worries about radiotherapy: Evaluation
of a preparatory booklet. Psychology and Health
1988;2:79-89. [Rec#: 2329]
DiIorio C, Faherty B, Manteuffel B. Epilepsy selfmanagement: partial replication and extension. Res
Nurs Health 1994;17(3):167-74. [Rec#: 776]
Earll L, Johnston M, Mitchell E. Coping with motor neuron
disease--an analysis using self-regulation theory.
Palliat Med 1993;7 (4 Suppl):21-30. [Rec#: 779]
Dixon J. Effect of nursing interventions on nutritional and
performance status in cancer patients. Nursing
Research 1984;33:330-335. [Rec#: 2324]
Dodd MJ. Efficacy of proactive information on self-care in
chemotherapy patients. Patient Education and
Counseling 1988;11:215-225. [Rec#: 2327]
Eastman RC, Siebert CW, Harris M, Gorden P. Clinical
Review 51. Implications of the diabetes control and
complications trial. J Clin Endocrinol & Metab
1993;77:1105-1107. [Rec#: 2189]
Dodd MJ. Efficacy of proactive information on self-care in
radiation therapy patients. Heart and Lung
1987;16:538-544. [Rec#: 2326]
Edgar L, Rosberger Z, Nowlis D. Coping with cancer
during the first year after diagnosis. Assessment and
intervention. Cancer 1992;69(3):817-28. [Rec#: 780]
Dodd MJ. Measuring informational intervention for
chemotherapy knowledge and self-care behavior.
Research in Nursing and Health 1984;7(1):43-50.
[Rec#: 2325]
Edwards PK, Acock AC, Johnston RL. Nutrition behavior
change outcomes of an educational approach. Eval
Rev 1985;9:441-459. [Rec#: 2640]
Elixhauser A. The cost-effectiveness of preventive care for
diabetes mellitus. Diabetes Spectrum 1989;2:349-353.
[Rec#: 3445]
Domar AD, Noe JM, Benson H. The preoperative use of
the relaxation response with ambulatory surgery
patients. Journal of Human Stress 1987;13(3):101107. [Rec#: 2328]
Elliott D. The effects of music and muscle relaxation on
patient anxiety in a coronary care unit. Heart Lung
1994;23(1):27-35. [Rec#: 781]
Dracup K, Moser DK, Marsden C, Taylor SE, Guzy PM.
Effects of a multidimensional cardiopulmonary
rehabilitation program on psychosocial function. Am J
Cardiol 1991;68:31-34. [Rec#: 2654]
Emmelkamp PM, van Oppen P. Cognitive interventions in
behavioral medicine. Psychother Psychosom
1993;59(3-4):116-30. [Rec#: 782]
168
Rejected Articles
Engel GL. The need for a new medical model: a challenge
for biomedicine. Science 1977;196(4286):129-36.
[Rec#: 783]
Flor H, Turk D. Chronic back pain and rheumatoid
arthritis: Predicting pain and disability from cognitive
variables. J Behav Med 1988;11:251. [Rec#: 2078]
Engstrom D. Cognitive behavioral therapy methods in
chronic pain treatment. In: Bonica JJ. (Ed) Advances
in pain research and therapy. New York: Raven Press;
1983 . p. 829-829. [Rec#: 2289]
Flor H, Turk D, Ruidy T. Pain and families. II.
Assessment and treatment. Pain 1987;30:29. [Rec#:
2079]
Fordyce WE, Brockway JA, Berman JA, Spengler D. Acute
back pain: A control-group comparison of behavioral
versus traditional management methods. Journal of
Behavioral Medicine 1986;9:127-140. [Rec#: 2290]
Epstein LH, Cluss PA. A Behavioral Medicine perspective
on adherence to long-term medical regimens. Journal
of consulting and Clinical Psychology 1988;6:77-87.
[Rec#: 2238]
Fordyce WE, Fowler RS, Lehmann JF, DeLateur BJ, Sand
PL, Treischmann RB. Operant conditioning in the
treatment of chronic-pain. Arch Phys Med Rehab
1973;54:399-408. [Rec#: 2694]
Eriksson KF, Lindgarde F. Prevention of type 2 (noninsulin-dependent) diabetes mellitus by diet and
physical exercise. Diabetologia 1991;34:891-898.
[Rec#: 2213]
Forester B, Kornfeld DS, Fleiss JL. Psychotherapy during
radiotherapy: Effects on emotional and physical
distress. American Journal of Psychiatry 1985;
142:22-27. [Rec#: 2331]
Ewart CK, Taylor CB, Reese LB, DeBusk RF. Effects of
early postmyocardial infarction exercise testing on
self- perception and subsequent physical activity. Am
J Cardiol 1983;51(7):1076-80. [Rec#: 784]
Franz MJ, Splett PL, Monk A, Barry B, McClain K,
Weaver T, et al. Cost-effectiveness of medical
nutrition therapy provided by dieticians for persons
with non-insulin-dependent diabetes mellitus. J Am
Diet Assoc 1996; 96(7): 657-8. [Rec#: 3437]
Fawzy FI, Cousins N, Fawzy NW, Kemeny ME, Elashoff
R, Morton D. A structured psychiatric intervention for
cancer patients. I. Changes over time in methods of
coping and affective disturbance. Arch Gen Psychiatry
1990;47(8):720-5. [Rec#: 785]
Frasure-Smith N, Prince R. The ischemic heart disease life
stress-monitoring program: possible therapeutic
mechanism. Psychol Health 1987; 1:273-285. [Rec#:
2217]
Fawzy FI, Fawzy NW. A structured psycho-educational
intervention for cancer patients. Gen Hosp Psychiatry
1994;16(3):149-92. [Rec#: 788]
Fawzy FI, Fawzy NW, Arndt LA, Pasnau RO. Critical
review of psychosocial interventions in cancer care.
Arch Gen Psychiatry 1995;52 (2):100-13. [Rec#: 786]
Frasure-Smith N, Prince R. The ischemic heart disease life
stress-monitoring program: 18-month mortality
results. Can J Public Health 1986; 77(S1)((Suppl)):
46. [Rec#: 2216]
Fawzy FI, Fawzy NW, Hyun CS, Elashoff R, Guthrie D,
Fahey JL, et al. Malignant melanoma. Effects of an
early structured psychiatric intervention, coping, and
affective state on recurrence and survival 6 years later.
Arch Gen Psychiatry 1993;50(9):681-9. [Rec#: 787]
Freemantle N, Harvey EL, Wolf F, et al. Printed
educational materials to improve the behavior of
health care professionals and patient outcomes. In:
Cochrane Database of Systematic Reviews, Issue 3.
1998. [Rec#: 2618]
Fawzy FI, Kemeny ME, Fawzy NW, Elashoff R, Morton
D, Cousins N, et al. A structured psychiatric
intervention for cancer patients. II. Changes over time
in immunological measures. Arch Gen Psychiatry
1990;47(8):729-35. [Rec#: 789]
Freiman JA, Chalmers TC, Smith HJr, Kuebler RR. The
importance of beta, the Type II error and sample size
in the design and interpretation of the randomized
control trial: Survey of 71 "negative" trials. New
England Journal of Medicine 1978; 299:690-694.
[Rec#: 2646]
Fernando DJPerera SD. The work of a diabetes clinic: an
audit. Ceylon Medical Journal 1994;39(3):138. [Rec#:
2590]
Friedman M. The modification of type a behavior in postinfarction patients. Am hert J 1979;97:551-560. [Rec#:
2403]
Fielding R. A note on behavioral treatment in the
rehabilitation of myocardial infarction patients. Br J
Soc Clin Psychol 1980;19 :157-161. [Rec#: 2374]
Friedman M, Rosenman RH. The prudent management of
the coronary-prone individual. Geriatrics 1972;27:7479. [Rec#: 2402]
Flor H, Haag G, Turk DC, et al. Efficacy of EMG
biofeedback, pseudotherapy, and conventional medical
treatment for chronic rheumatic back pain. Pain
1983;17:21. [Rec#: 2077]
Funnell MM, Anderson RM, Arnold MS, Barr PA,
Donnelly M, Johnson PD, et al. Empowerment: an
idea whose time has come in diabetes education.
Diabetes Educ 1991;17(1):37-41. [Rec#: 3415]
169
Rejected Articles
Garrett J, Fenwick JM, Taylor G, Mitchell E, Stewart J,
Rea H. Prospective controlled evaluation of the effect
of a community based asthma education center in a
multiracial working class neighborhood. Thorax 1994;
49(10): 976-83. [Rec#: 793]
Glasgow RE, McCaul KD, Schafer LC. Self-care behaviors
and glycemic control in type I diabetes. J Chronic Dis
1987;40(5):399-412. [Rec#: 798]
Glasgow RE, Osteen VL. Evaluating diabetes education:
Are we measuring the most important outcome?
Diabetes Care 1992;15:1423-1432. [Rec#: 2177]
Gellert GA, Maxwell RM, Siegel BS. Survival of breast
cancer patients receiving adjunctive psychosocial
support therapy: a 10-year follow-up study. J Clin
Oncol 1993 ;11:66-9. [Rec#: 2414]
Glasgow RE, Strycker LA. Preventive care practices for
diabetes management in two primary care samples.
Am J Prev Med 2000;19 (1):9-14. [Rec#: 3419]
Gerber L, Liang M, Stevens MB, et al. Patient education
program to teach energy conservation behaviors to
patients with rheumatoid arthritis: A pilot study. Arch
Phys Med Rehabil 1987;68:442. [Rec#: 2080]
Glasgow RE, Toobert DJ. Social environment and regimen
adherence among type II diabetic patients. Diabetes
Care 1988;11(5):377-86. [Rec#: 800]
Gibson PG, Talbot PI, Toneguzzi RC. Self-management,
autonomy, and quality of life in asthma. Population
Medicine Group 91C. Chest 1995; 107(4): 1003-8.
[Rec#: 794]
Glasgow RE, Toobert DJ, Hampson SE, et al. A brief office
based intervention to facilitate diabetes dietary selfmanagement. Health Education Research
1995;10:467-78. [Rec#: 2418]
Gifford S, Zimmet P. A community approach to diabetes
education in Australia - The Region 8 (Victoria)
Diabetes Education and Control Program. Diabetes
Research and Clinical Practice 1986; 2:105-112.
[Rec#: 2239]
Glasgow RE, Toobert DJ, Hampson SE, Wilson W .
Behavioral research on diabetes at the Oregon
Research Institute. Ann Behav Med 1995;17 :32-40.
[Rec#: 905]
Glasgow RE, Wilson W, McCaul KD. Regimen adherence:
A problematic construct in diabetes research. Diabetes
Care 1985;8(3):300-301. [Rec#: 2241]
Gift AG, Moore T, Soeken K. Relaxation to reduce
dyspnea and anxiety in COPD patients. Nurs Res
1992;41(4):242-6. [Rec#: 795]
Glatthaar C, Welborn TA, Stehnouse NS, Garceia-Webb P.
Diabetes and impaired glucose tolerance: A
prevalence estimate based on the Busselton 1981
survey. Medical Journal of Australia 1985;143:436440. [Rec#: 2242]
Gil KM, Ross SL, Keefe FJ. Behavioral Treatment of
chronic pain: Four pain management protocols. In
R.D. France & K.R>R. Krishman (Eds.). Chronic Pain
1988:3760413. [Rec#: 2705]
Glimelius B, Birgegard G, Hoffman K, Hagnebo C, Kvale
K, Nordin K, et al. A comprehensive cancer care
project to improve the overall situation of patients
receiving intensive chemotherapy. J Psychosoc Oncol
1993;11(1):17-40. [Rec#: 906]
Gilden JL, Hendryx M, Casia C, Singh SP. The
effectiveness of diabetes education programs for older
patients and their spouses. J Am Geriatr Soc 1989;
37:1023-1030. [Rec#: 2211]
Giloth BE. Promoting patient involvement: educational,
organizational, and environmental strategies. Patient
Educ Couns 1990; 15 (1): 29-38. [Rec#: 796]
Goeppinger J, Arthur MW, Brunk Se, Riedesel S. The
impact of participant contracting on the outcomes of
community-based arthritis self-care nursing
intervention. 115th Annual Meeting of the American
Public Health Association. New Orleans 1987. [Rec#:
2660]
Glanz K. Patient and public education for cholesterol
reduction: A review of strategies and issues. Patient
Education and Counseling 1988; 12:235-257. [Rec#:
2644]
Glasgow RE. A practical model of diabetes management
and education. Diabetes Care 1995; 18(1): 117-26.
[Rec#: 797]
Goeppinger J, Brunk SE, Thomas MA . Bone up on
arthritis: Self-care education programs for rural
persons. Meeting of the Arthritis Health Profession
Association. Minneapolis: 1984. [Rec#: 2310]
Glasgow RE, Anderson RM. In diabetes care, moving from
compliance to adherence is not enough. Something
entirely different is needed. Diabetes Care 1999;
22(12): 2090-2. [Rec#: 3404]
Goldberg RJ, Wool MS. Psychotherapy for the spouses of
lung cancer patients: Assessment of an intervention.
Psychotherapy and psychosomatics 1985;43(3):141150. [Rec#: 2332]
Glasgow RE, McCaul KD, Schafer LC. Barriers to regimen
adherence among persons with insulin-dependent
diabetes. Journal of Behavioral Medicine 1986;9:6577. [Rec#: 2240]
Gomez EJdel Pozo FHernando ME. Telemedicine for
diabetes care: the DIABTel approach towards
diabetes telecare. Medical Informatics 1996;21(4):283.
[Rec#: 2591]
170
Rejected Articles
Goodall TA, Halford WK. Self-management of diabetes
mellitus: A critical review [published erratum appears
in Health Psychol 1992;11(1):77]. Health Psychol
1991;10(1):1-8. [Rec#: 802]
Griffin S, Kinmonth AL. Diabetes care: the effectiveness of
systems for routine surveillance for people with
diabetes (Cochrane Review). In: The Cochrane
Library, Issue 4. Oxford: Update Software; 1998.
[Rec#: 2620]
Goodwin JO. Programmed instruction for self-care
following pulmonary surgery. International Journal of
Nursing Studies 1979;16:29-40. [Rec#: 2333]
Gross AM. A behavioral approach to the compliance
problems of young diabetes. Journal of Compliance in
Health Care 1987;2:7-21. [Rec#: 2246]
Gordis L. Conceptual and methodological problems in
measuring patient compliance. In: Haynes RB, Taylor
DW, Sackett DL. Compliance in health care.
Baltimore: Johns Hopkins University Press; 1979. p.
23-43. [Rec#: 2244]
Gross AM, Heimann L, Shapiro R, Schultz RM. Children
with diabetics: Social skills training and hemoglobin
A1c levels. Behavior Modification 1983;7:151-164.
[Rec#: 2247]
Graber AL, Christman BG, Alogna MT, Davidson JK.
Evaluation of diabetes patient-education programs.
Diabetes 26 1977;61-64. [Rec#: 2214]
Gross M, Brandt KD. Educational support groups for
patients with ankylosing spondylitis: a preliminary
report. Patient Counsel Health Ed 1981;3:6-12. [Rec#:
2677]
Graber AL, Wooldridge K, Brown A. Effects of intensified
practitioner-patient communication on control of
diabetes mellitus. Southern Medical Journal
1986;89:1205-1209. [Rec#: 2428]
Gruesser M, Bott U, EllermannP, Kronsbein P, Joergens V.
Evaluation of a structured treatment and teaching
program for non-insulin-treated type II diabetic
outpatients in Germany after the nation-wide
introduction of reimbursement policy for physicians.
Diabetes Care 1993;16:1268-1275. [Rec#: 2187]
Graff WLBensussen-Walls WCody Eet al. Population
management in an HMO: new roles for nursing (see
comments). Public Health Nursing 1995;12(4):213.
[Rec#: 2592]
Gruesser MHartmann PSchlottmann Net al. Structured
treatment and teaching program for type 2 diabetic
patients on conventional insulin treatment: evaluation
of reimbursement policy. Patient Education &
Counseling 1996;29(1):123. [Rec#: 2593]
Grant I, Kyle GG, Teichman A, Mendelsl J. Recent life
events and diabetes in adults. Psychosomatic Medicine
1974;36(2):121. [Rec#: 2245]
Grant M. The effect of nursing consultation anxiety, side
effects, and self-care of patients receiving radiation
therapy. Oncology Nursing Forum 1990;17(3):31-38.
[Rec#: 2348]
Hackett TP. The use of groups in the rehabilitation of the
post-coronary patient. Adv Cardiol 1978;24:127-135.
[Rec#: 2411]
Haisch JBraun SBohm BOet al. Effects of patient education
in type II diabetic patients after clinic admission.
Results of a 3-month catamnesis after new patientcentered education. Psychotherapy, Psychosomatic,
Medizinische, Psychology 1996;46(11):400. [Rec#:
2594]
Greene G. Behavior modification for adult onset diabetes.
Diabetes Educ 1981;7(1):11-5, 27. [Rec#: 3448]
Greenfiel S, Rogers W, Mangotich M, et al. Outcomes of
patients with hypertension and non-insulin dependent
Diabetes Mellitus treated by different systems and
specialties. JAMA 1995;274:1436-44. [Rec#: 2419]
Halford WK, Cuddihy SE, Mortimer RH. Psychological
stress and blood glucose regulation in Type I diabetic
patients. Health Psychology 1990;9:516-528. [Rec#:
2248]
Greenfield SKaplan SHWare JEJr. Expanding patient
involvement in care: the EPIC program. Ann Intern
Med 1985;102:520-528. [Rec#: 2661]
Hampson SE, Glasgow RE, Foster LS. Personal models of
diabetes among older adults: relationship to selfmanagement and other variables. Diabetes Educ
1995;21(4):300-7. [Rec#: 807]
Greenhalgh PM. Shared care for diabetes. A systematic
review. Royal College of General Practitioners
1994;(67):i-viii, 1-35. [Rec#: 2619]
Greer S, Moorey S, Baruch JD, Watson M, Robertson BM,
Mason A, et al. Adjuvant psychological therapy for
patients with cancer: a prospective randomised trial
[see comments]. BMJ 1992;304( 6828):675-80. [Rec#:
804]
Hampson SE, Glasgow RE, Toobert DJ. Personal models
of diabetes and their relations to self-care activities.
Health Psychol 1990;9(5):632-46. [Rec#: 806]
Hampson SE, Glasgow RE, Zeiss A. Personal models of
osteoarthritis and their relation to self-management
activities and quality-of-life. Journal of Behavioral
Medicine 1994;17:143-158. [Rec#: 2448]
Grieco AL, Kopel KF. Self-help and self-care in chronic
illness. South Med J 1983;76(9):1128-30. [Rec#: 805]
171
Rejected Articles
Hanson CL, Henggeler SW, Burghen GA. Model of
associations between psychosocial variables and
health outcome measures of adolescents with IDDM.
Diabetes Care 1987a;10:752-758. [Rec#: 2249]
Hellman CJC, Budd M, Borysenko J, et al. A study of
effectiveness of two group behavioral medicine
interventions for patients with psychosomatic
complaints. Behav Med 1990;(165-173.). [Rec#:
2412]
Hanson CL, Henggeler SW, Burghen GA. Social
competence and parental support as mediators of the
link between stress and metabolic control in
adolescents with insulin-dependent diabetes mellitus.
Journal of Consulting and Clinical Psychology
1987b;55:529-533. [Rec#: 2250]
Heringa P, Lawson L/Reda D. The effect of a structured
education program on knowledge and psychomotor
skills of patients using beclomethasone dipropionate
aerosol for steroid dependent asthma. Health Educ Q
1987;14:309-317. [Rec#: 2163]
Harris MI. Medical care for patients with diabetes.
Epidemiological aspects. Annual of Internal Medicine
1996;124(1, part 2):117. [Rec#: 2596]
Hershman DL, Simonoff PA, Frishman WH, et al . Drug
utilization in the old and how it relates to selfperceived health and all-cause mortality: Results from
the Bronx Aging Study. J Am Geriatr Soc
1995;43:356-360. [Rec#: 2718]
Harris R, Linn MW. Health beliefs, compliance and control
of diabetes mellitus. Southern Medical Journal
1985;78:162-166. [Rec#: 2251]
Hill DR, Kelleher K, Shumaker SA. Psychosocial
interventions in adult patients with coronary heart
disease and cancer. A literature review. Gen Hosp
Psychiatry 1992;14(6 Suppl):28S-42S. [Rec#: 811]
Hartwell SL, Kaplan RM, Wallace JP. Comparison of
behavioral interventions for control of Type II
diabetes mellitus. Behavior Therapy 1986;17:447-461.
[Rec#: 2252]
Hilton S, Sibbald B, Anderson HR, Freeling P . Controlled
evaluation of the effects of patient education on
asthma morbidity in general practice. Lancet
1986;1(8471):26-9. [Rec#: 812]
Haynes RB, mcKibbon KA, Kanani R, et al. Interventions
to assist patients to follow prescriptions for
medications (Cochrane Review). In: The Cochrane
Library, Issue 4. Oxford: Update Software; 1998.
[Rec#: 2621]
Hinkle L, Wolf S. Importance of life stress in course and
management of diabetes mellitus. Journal of the
American Medical Association 1952b;148:513-520.
[Rec#: 2254]
Hays RD, Kravitz RL, Mazel RM, Sherbourne CD,
DiMatteo MR, Rogers WH, et al. The impact of
patient adherence on health outcomes for patients with
chronic disease in the Medical Outcomes Study. J
Behav Med 1994;17 (4):347-60. [Rec#: 808]
Hinkle LE, Wolf S. The effects of stressful life situations
on the concentration of blood glucose in diabetic and
non-diabetic humans. Diabetes 1952a; 1:383-392.
[Rec#: 2253]
Hedback B, Perk J. Five-year results of a comprehensive
rehabilitation program after myocardial infarction. Eur
Heart J 1987;8:234-242. [Rec#: 2655]
Hirano PC, Laurent DD, Lorig K. Arthritis patient
education studies, 1987-1991: a review of the
literature [see comments]. Patient Educ Couns 1994;
24(1):9-54. [Rec#: 813]
Hedback B, Perk J, Perski A. Effect of a post-myocardial
infarction rehabilitation program on mortality,
morbidity, and risk factors. J Cardiopulm Rehab
1985;5:576-583. [Rec#: 2693]
Holman H, Mazonson P, Lorig K. Health education for
self-management has significant early and sustained
benefits in chronic arthritis. Trans Assoc Am
Physicans 1989;102:204-208. [Rec#: 2303]
Heinrich RL, Cohen MJ, Naliboff BD, Collins GA,
Bonbakker AD. Comparing physical and behavior
therapy for chronic low back pain on physical
abilities, psychological distress, and patients'
perceptions. Journal of Behavioral Medicine
1985;8:61-78. [Rec#: 2291]
Horrocks PM, Blackmore R, Wright AD. A long-term
follow-up of dietary advice in maturity onset diabetes:
The experience of one center in the UK prospective
study. Diabetic Medicine 1987;4:241-244. [Rec#:
2122]
Heller RF, Walker RJ, Boyle CA, O'Connell DL,
Rusakaniko S, Dobson AJ. A randomised controlled
trial of a dietary advice program for relatives of heart
attack victims. Med J Aust 1994;161(9):529-31.
[Rec#: 810]
Hoskins P, Alford J, Fowler P, Bolton T, Pech C, Hosking
M, et al. Outpatient stabilization program - An
innovative approach in the management of diabetes.
Diabetes Research 1985;2:85-88. [Rec#: 2123]
Helling DK, Lemke JH, Semla TP, et al. Medication use
characteristics in the elderly: The Iowa 65+ Rural
Health Study. J Am Geriatr Soc 1987;35:4-12. [Rec#:
2717]
Howard M, Barnett C, Chon M, Wolf FM. Retention of
knowledge and self-care skills after an intensive inpatient diabetes education program. Diabetes Research
and Clinical Practice 1986;2:51-57. [Rec#: 2124]
172
Rejected Articles
Ibrahim MA, Feldman JG, Sultz HA, Staiman MG, Young
LJ, Dean D. Management after myocardial infarction:
A controlled trial of the effect of group psychotherapy.
Int J Psychiatry Med 1974;5:253-268. [Rec#: 2368]
Johnson J. The effects of a patient education course on
persons with a chronic illness . Cancer Nursing
1982;5(2):117-123. [Rec#: 2335]
Johnson SB, Silverstein J, RosenbloomA, Carter R,
Cunningham W. Assessing daily management in
childhood diabetes. Health Psychology 1986;5:545564. [Rec#: 2256]
Ignacio-Garcia JM, Gonzalez-Santos P. Asthma selfmanagement education program by home monitoring
of peak expiratory flow. Am J Respir Crit Care Med
1995;151(2 Pt 1):353-9. [Rec#: 814]
Johnston DW. Behavioral treatment in the reduction of
coronary risk factors Type a behavior and blood
pressure. Br J Clin Psychol 1982;21:281-294. [Rec#:
2364]
Irsigler K, Bali-Taubald C. Self monitored blood glucose:
The essential biofeedback signal in the diabetic
patients' effort to achieve normoglycemia. Diabetes
Care 1980;3:163-170. [Rec#: 2389]
Johnston DW. Stress managements in the treatment of mild
primary hypertension. Hypertension 1991;17(Suppl
3):63-68. [Rec#: 2470]
Jacob RG, Wing R, Shapiro AP. The behavioral treatment
of hypertension: long-term effects. Behav Therapy
1987;18:325-352. [Rec#: 2471]
Johnston Dw, Lo CR. The effects of cardiovascular
feedback and relaxation on angina pectoris. Behav
Psychother 1983;11:257-264. [Rec#: 2685]
Jacobs C, Ross RD, Walker IM, Stockdale FE. Behavior of
cancer patients: A randomized study of the effects of
education and peer support groups. American Journal
of Clinical Oncology 1983;6:347-353. [Rec#: 2334]
Jacobson AM, Leibovich JB. Psychological issues in
diabetes mellitus. Psychosomatic Illness Review
1984;25:7-13. [Rec#: 2255 ]
Jones KP, Mullee MA, Middleton M, Chapman E, Holgate
ST. Peak flow based asthma self-management: a
randomised controlled study in general practice.
British Thoracic Society Research Committee. Thorax
1995;50 (8):851-7. [Rec#: 930]
Jacobson JM, O'Rourke PJ, Wolf AE. Impact of a diabetes
teaching program on health care trends in a Air Force
medical center. Mil Med 1983;148:46-47. [Rec#:
2182]
Jones PJ. A self-control behavior techniques course to
increase adherence to the goal for frequency of selfmonitoring blood glucose (Dissertation). University
of Pittsburgh 19989;377. [Rec#: 2668]
Janson-Bjerklie, Shnell S. Effect of peak flow information
on patterns of self-care in adult asthma. Heart and
Lung: The Journal of Critical Care 1988;17:543-549.
[Rec#: 2430]
Jones PM. Use of a course on self-control behavior
techniques to increase adherence to prescribed
frequency for self-monitoring blood glucose. Diabetes
Educ 1990;16(4):296-303. [Rec#: 818]
Jeffrey RW, Thompson PD, Wing RR. Effects on weight
reduction of strong monetary contracts for calorie
restriction or weight loss. Behavior Research and
Therapy 1978;16:363-369. [Rec#: 2647]
Jovanovics L, Peterson CM. A comparison of eight
educational programs. Diabetes Ed 1984;40-42.
[Rec#: 2380]
Jurish JE, Blanchard EB, Andrasik F, et al. Home-versus
clinic-based treatment of vascular headache. J of
Consulting and Clinical Psychology 1983;51:743-751.
[Rec#: 2475]
Jenkins CD. An integrated behavioral medicine approach to
improving care of patients with diabetes mellitus.
Behav Med 1995;21(2):53-65; discussion 66-8. [Rec#:
815]
Kallinke D, Kulick B, Heim P. Behavior analysis and
treatment of essential hypertensive. J of
Psychosomatic Res 1982;26:541-549. [Rec#: 2454]
Jenkinson D, Davison J, Jones S, Hawtin P. Comparison of
effects of a self management booklet and
audiocassette for patients with asthma. BMJ
1988;297(6643):267-70. [Rec#: 816]
Kaplan RM. Behavior as the central outcome in health care.
Am Psychol 1990;45(11):1211-20. [Rec#: 819]
Jenni MA, Wollersheim JP. Cognitive therapy, stress
management training, and the type A behavior pattern.
Cognit Ther Res 1979;3:61-73. [Rec#: 2370]
Kaplan RM, Chadwick MW, Schimmel LE. Social learning
intervention to promote metabolic control in type I
diabetes mellitus: pilot experiment results. Diabetes
Care 1985;8:152-155. [Rec#: 2206]
Jensen MP, Turner JA, Romano JM. Self-efficacy and
outcome expectancies: relationship to chronic pain
coping strategies and adjustment. Pain
1991;44(3):263-9. [Rec#: 817 ]
Kaplan RM, Davis WK. Evaluating costs and benefits of
outpatients’ diabetes education and nutrition
counseling. Diabetes Care 1986;9:81-86. [Rec#: 2379]
173
Rejected Articles
Kaplan RM, Hartwell SL. Differential effects of social
support and social network on physiological and social
outcomes in men and women with Type II diabetes
mellitus . Health Psychology 1987;6:387-398. [Rec#:
2257]
Kennedy L, Walshe K, Hadden DR, et al. The effect of
intensive therapy on serum high density lipoprotein
cholesterol in patients with Type 2 (non-insulindependent) diabetes mellitus: A prospective study.
Diabetologia 1982;23:24-27. [Rec#: 2391]
Kaplan RM, Ries AL, Prewitt LM, Eakin E. Self-efficacy
expectations predict survival for patients with chronic
obstructive pulmonary disease. Health Psychol
1994;13(4):366-8. [Rec#: 821]
Kerns RD, Turk DC, Holzman AD, Rudy TE. Comparison
of cognitive-behavioral and behavioral approaches to
the out-patient treatment of chronic pain. Clinical
Journal of Pain 1986;1:195-203. [Rec#: 2294]
Kaplan S, Kozin F. A controlled study of group counseling
in rheumatoid arthritis. J Rheumatology 1981;8:91-99.
[Rec#: 2352]
Kingery PM, Glasgow RE. Self efficacy and outcome
expectations in the self regulation of non-insulin
dependent diabetes mellitus. Health Education 1989;
20(7):13-19. [Rec#: 2445]
Kaplan SH, Greenfield S, Ware JE= Jr. Assessing the
effects of physician-patient interactions on the
outcomes of chronic disease [published erratum
appears in Med Care 1989 Jul;27(7):679]. Med Care
1989;27(3 Suppl):S110-27. [Rec#: 820]
Kirkley BG, Fisher EB. Relapse as a model of nonadherence to dietary treatment of diabetes. Health
Psychology 1988;7:221-230. [Rec#: 2258]
Kirscht JP. Patient education, blood pressure control, and
the long run. Am J Public Health 1983;73(2):134-135.
[Rec#: 2305]
Karlander S, Kindstedt K. Effects of formalized diabetes
education. Acta Med Scand 1983;213(41-43). [Rec#:
2191]
Kiser DG. Diabetes patient education. Supervisor Nurse
1981;51:32-35. [Rec#: 2179]
Kaye RL, Hammond AH. Understanding rheumatoid
arthritis: evaluation of a patient education program.
JAMA 1978;239:2466-2467. [Rec#: 2649]
Knudson KG, Spiegel TM, Furst DE. Outpatient education
program for rheumatoid arthritis. Patient Counsel
Health Ed 1981;3:77-82. [Rec#: 2679]
Keefe FJ, Caldwell DS, Queen KT, Gil KM, Martinex S,
Crisson JE, et al. Pain coping strategies in
osteoarthritis patients. Journal of Consulting and
Clinical Psychology 1987a;55:208-212. [Rec#: 2703]
Koperski M. How effective is systematic care of Diabetic
patients? A study in one general practice. British J of
General Practice 1992;42:508-11. [Rec#: 2420]
Keefe FJ, Caldwell DS/Queen KT, Gil KM, Martinez S,
Crisson JE, Ogden W, et al. Osteoarthritic knee pain:
A behavioral analysis (1987b). Pain 1987
B.C.;28:309-321. [Rec#: 2704]
Kostis JB, Rosen RC, Cosgrove NM, Shindler DM, Wilson
AC. Nonpharmacologic therapy improves functional
and emotional status in congestive heart failure. Chest
1994;106(4):996-1001. [Rec#: 824]
Keefe FJ, Dunsmore J, Burnett R. Behavioral and
cognitive-behavioral approaches to chronic pain:
recent advances and future directions. J Consult Clin
Psychol 1992;60(4):528-36. [Rec#: 822]
Kotses H, Bernstein IL, Bernstein DI, Reynolds RV,
Korbee L, Wigal JK, et al. A self-management
program for adult asthma. Part I: Development and
evaluation. J Allergy Clin Immunology
1995;95(2):529-40. [Rec#: 825]
Keefe FJ, Gil KM, Rose SC. Behavioral approaches in the
multidisciplinary management of chronic pain:
Programs and issues. Clinical Psychology Review
1986;6:87-113. [Rec#: 2292]
Kotses H, Stout C, McConnaughy K, Winder JA, Creer TL.
Evaluation of individualized asthma self-management
programs. J Asthma 1996;33(2):113-8. [Rec#: 931]
Keefe FJ, Williams DA. New Directions in pain assessment
and treatment. Clinical Psychology Review
1989;9:549-568. [Rec#: 2293]
Kronsbein P, Jorgens V, Muhlauser I, Scholz V, Venhaus
A, Berger M. Evaluation of a structured treatment and
teaching program on non-insulin-dependent diabetes.
The Lancet, II 1988;8625:1407-1411. [Rec#: 2129]
Kemp SF, Canfield ME, Kearns FS, et al. The effect of
short-term intervention on long-term diabetes
management. J Arkansas Med Soc 1986;83:241-244.
[Rec#: 2390]
Krosnick A. Self-management, patient compliance, and the
physician. Diabetes Care 1980;3:124-126. [Rec#:
2431]
Kemper DW, Lorig K, Mettler M. The effectiveness of
medical self-care interventions: a focus on selfinitiated responses to symptoms. Patient Educ Couns
1993;21(1-2):29-39. [Rec#: 823]
Kushnir B, Fox KM, Tomlinson W, Aber CP. The effect of
predischarge consultation on the resumption of work,
sexual activity and driving. Scand J. Rehab Med
1976;8:155-159. [Rec#: 2651]
174
Rejected Articles
Laffel LMBrackett JHo Jet al. Changing the process of
diabetes care improves metabolic outcomes and
reduces hospitalizations. Quality Management in
Health Care 1998;6(4):53. [Rec#: 2600]
Lindroth Y, Bauman A, Barnes C, et al . A controlled
evaluation of arthritis education. Br J. Rheumatol
1989;28:7. [Rec#: 2083]
Lindroth Y, Bauman A, Brooks PM, et al. A 5-year followup of a controlled trial of an arthritis education
program. British Journal of Rheumatology
1995;34(7):647-652. [Rec#: 3454]
Lahdensuo A, Haahtela T, Herrala J, Kava T, Kiviranta K,
Kuusisto P, et al. Randomised comparison of guided
self management and traditional treatment of asthma
over one year. BMJ 1996;312(7033):748-52. [Rec#:
932]
Linn MW, Linn BS, Harris R. Effects of counseling for late
stage cancer patients. Cancer 1982;49:1048-1055.
[Rec#: 2336]
Lam KSL, Ma JTC, Chan EYM, et al. Sustained
improvement in diabetic control on long-term selfmonitoring of blood glucose. Diabetes Res Clin Prac
1986;2:165-171. [Rec#: 2393]
Linn MW, Skyler JS, Linn BS, et al. A possible role for
self-management techniques in control of diabetes.
Diabetes Educator 1985;13-16. [Rec#: 2432]
Landis B, Jovanovic L, Landis E, Peterson CM, Groshen S,
Johnson K, et al. Effect of stress reduction on daily
glucose range in previously stabilized insulindependent diabetic patients. Diabetes Care
1985;8(6):624-6. [Rec#: 3440]
Lorig K. Chronic disease self-management: A model for
tertiary prevention. American Behavioral Scientist
1996;39(6):676-683. [Rec#: 939]
Lorig K. Self-management of chronic illness: A model for
the future. Generations 1993;11-14. [Rec#: 911]
Langosch W, Seer P, Brodner G, Kallinke D, Kulick B,
Heim F. Behavior therapy with coronary heart disease
patients: Results of a comparative study. J Psychosom
Res 1982;26:475-484. [Rec#: 2371]
Lorig K, Holman H. Arthritis self-management studies: a
twelve-year review. Health Educ Q 1993;20(1):17-28.
[Rec#: 831]
Larpent N, Canivet J. Bicentric evaluation of a teaching
program for Type I (insulin-dependent diabetic
patients). Diabetologia 1984;27:62. [Rec#: 2667]
Lorig K, Holman HR. Long-term outcomes of an arthritis
self-management study: effects of reinforcement
efforts. Soc Sci Med 1989;29 (2):221-4. [Rec#: 832]
Lawrence PA, Cheely J. Deterioration of diabetic patients'
knowledge and management skills as determined
during outpatient visits. Diabetes Care 1980;3:214218. [Rec#: 2098]
Lorig K, Laurin J. Some notions about assumptions
underlying health education. Health Educ Q
1985;12(3):231-43. [Rec#: 834]
Lorig K, Laurin J, Holman HR. Arthritis self-management:
a study of the effectiveness of patient education for the
elderly. Gerontologist 1984;24(5):455-7. [Rec#: 833]
Lebovitz F, Ellis IIIGJ, Skyler JS. Performance of technical
skills of diabetes management: Increased
independence after a camp experience. Diabetes Care
1978;1(1):23. [Rec#: 2394]
Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW Jr,
Bandura A, et al. Chronic disease self-management
program: 2-year health status and health care
utilization outcomes. Med Care 2001;39(11):1217-23.
[Rec#: 3473]
Lefebvre JP, Houziaux MO, Godart C, Scheen-Lavigne M,
Bartholme M, Luyckz AS. Computer-assisted
instruction for diabetics. Metabolism 1981;7:127-124.
[Rec#: 2204]
Lorig KR, Mazonson PD, Holman HR. Evidence
suggesting that health education for self-management
in patients with chronic arthritis has sustained health
benefits while reducing health care costs. Arthritis
Rheum 1993;36(4):439-46. [Rec#: 836]
Legge JS, Massey VM, Vena CI, Reily BJ. Evaluating
patient education: a case study of a diabetes program .
Health Educ Q 1980;7:148-486. [Rec#: 2181]
Lenker SL, Lorig K, Gallagher D. Reasons for the lack of
association between changes in health behavior and
improved health status: an exploratory study. Patient
Educ Couns 1984;6(2):69-72. [Rec#: 826]
Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M.
Effect of a self-management program on patients with
chronic disease. Eff Clin Pract 2001;4(6):256-62.
[Rec#: 3481]
Leserman J, Stuart EM, Marnish ME, Decro JP, Beckman
RJ, Friedman R, et al. Nonpharmacologic intervention
for hypertension: Long-term follow-up. J
Cardiopulmonary Rehabil 1989;9:316-324. [Rec#:
909]
Lowe JMBowen K. Evaluation of a diabetes education
program in Newcastle, New South Wales. Diabetes
Research & Clinical Practice 1997;38(2):91. [Rec#:
2601]
Linden W, Chambers L. Clinical effectiveness of non-drug
treatment for hypertension: A meta-analysis. Ann
Behav Med 1994;16:35-45. [Rec#: 910]
175
Rejected Articles
Lubeck DP, Brown BW, Holman HR. Chronic disease and
health system performance. Care of osteoarthritis
across three health services. Med Care
1985;23(3):266-77. [Rec#: 838]
Massey MR. Evaluation of a health education program:
compliance of diabetic patients with a dietary regimen.
Dissertation Abstracts International (University
Microfilms International No. 80-20,614) 1980;4:907B. [Rec#: 3446]
Luborsky L, Crits-Christoph P, Brady JP, et al. Behavioral
versus pharmacological treatments for essential
hypertension--A needed comparison. Psychosomatic
Medicine 1982;44:203-213. [Rec#: 2461]
Mayo PH, Richman J, Harris HW. Results of a program to
reduce admissions for adult asthma [see comments].
Ann Intern Med 1990;112(11):864-71. [Rec#: 840]
Lyles JN, Burish TG, Krozely MG, Oldham RK. Efficacy
of relaxation training and guided imagery in reducing
the aversiveness of cancer chemotherapy. Journal of
Consulting and Clinical Psychology 1982;50:509-524.
[Rec#: 2337]
Mazze RS. A systems approach to diabetes care. Diabetes
Care 1994;17 Suppl 1:5-11. [Rec#: 841]
Mazze RS, Etzwiler DD, Strock E, Peterson K, McClave
CR 2nd, Meszaros JF, et al. Staged diabetes
management. Toward an integrated model of diabetes
care. Diabetes Care 1994;17 Suppl 1:56-66. [Rec#:
842 ]
Maggs FM, Jubb RW, Kemm JR. Single-blind randomized
controlled trial of an educational booklet for patients
with chronic arthritis. British Journal of
Rheumatology 1996;35:775-777. [Rec#: 3455]
Mazze RS, Shamoon H, Pasmantier R, Lucido D, Murphy
J, Hartman K, et al. Reliability of blood glucose
monitoring by patients with diabetes mellitus.
American Journal of Medicine 1984;77:211-217.
[Rec#: 2263]
Maguire P, Brooke M, Tait A, Thomas C, Sellwood R. The
effect of counseling on physical disability and social
recovery after mastectomy. Clinical Oncology
1983;9:319-324. [Rec#: 2338]
Mazzuca SA. Does patient education in chronic disease
have therapeutic value? J Chronic Dis 1982;35(7):5219. [Rec#: 843]
Maiman LA, Green LW, Gibson G, Mackenzie EJ.
Education for self-treatment by adult asthmatics.
JAMA 1979;241:1919-1922. [Rec#: 2166]
Mazzuca SA. Education and behavioral and social research
in rheumatology. Curr Opin Rheumatol
1994;6(2):147-52. [Rec#: 844]
Maisiak R, Austin J, Heck L. Health outcomes of two
telephone interventions for patients with rheumatoid
arthritis or osteoarthritis. Arthritis and Rheumatism
1996;39(8):1391-1399. [Rec#: 3456]
Mazzuca SA, Brandt DK, Katz BP, et al. Effects of selfcare education on the health status of inner-city
patients with osteoarthritis of the knee. Arthritis and
Rheumatism 1997;40(8):1466-1474. [Rec#: 3458]
Malik RL, Howitz DL, Smyth-Staruch K. Energy
metabolism in diabetes: Computer-assisted instruction
for persons with diabetes. The Diabetes Educator, 13
(Special Issue) 1987;203-205. [Rec#: 2131]
Mazzuca SA, Clark CM. Persistence of effects of physician
education on diabetes care practices. Diabetes
1983;32S:54A. [Rec#: 2714]
Malone JM, SnyderM, AndersonG, Bernhard VM,
Holloway GA, Blunt TJ. Prevention of amputation by
diabetes education. Am J Surgery 1989;158:520-524.
[Rec#: 2188]
Mazzuca SA, et al . The Diabetes Educational Study: a
controlled trial of the effects of intensive instruction of
internal medicine residents on the management of
diabetes mellitus. J Gen Intern Med 1988;3:1-8.
[Rec#: 2091]
Maras ML, Rinke WJ, Stephens CR, et al. Effect of
meditation on insulin dependent diabetes mellitus.
Diabetes Educ 1984;22-25. [Rec#: 2395]
McCain NL, Lynn MR. Meta-analysis of a narrative
review: Studies evaluating patient teaching. Western
Journal of Nursing Research, 12 1990;347-358. [Rec#:
2099]
Marcus BH, Selby VC, Niaura RS, et al. Self-efficacy and
the stages of exercise behavior change. Res Quart
Exer Sport 1992;63 :60-66. [Rec#: 2473]
McCaul KD, Glasgow RE, Schafer LC. Diabetes regimen
behaviors. Predicting adherence. Med Care
1987;25(9):868-81. [Rec#: 845]
Marrero DG, Fremion AS, Golden MP. Improving
compliance with exercise in adolescents with insulindependent diabetes mellitus: results of a selfmotivated home exercise program. Pediatrics
1988;81:519-525. [Rec#: 2261]
McCulloch DK, Glasgow RE, Hampson SE, Wagner E. A
systematic approach to diabetes management in the
post-DCCT era. Diabetes Care 1994;17(7):765-9.
[Rec#: 846]
Marteau TM, Bloch S, Baum JD. Family life and diabetic
control. Journal of Child Psychology and Psychiatry
1987;28(6):823. [Rec#: 2262]
176
Rejected Articles
McDonald CJ, Hui SL, Smith DM, Tierney WM, Cohen SJ,
Weinberger Met al. Reminders to physicians from an
introspective computer medical record. A two-year
randomized trial. Ann Intern Med 1984;100:130-138.
[Rec#: 2671]
Montgomery EBJ, Lieberman A, Singh G, et al. Patient
education and health promotion can be effective in
Parkinson's Disease: A randomized controlled trial.
PROPATH Advisory Board. Am J Med 1994;97:42935. [Rec#: 2421]
McGrady AV, Turner Jr JW, Fine TH, et al. Effects of
biobehaviorally assisted relaxation training on blood
pressure, plasma renin, cortisol, and aldosterone levels
in borderline essential hypertension. Clinical
Biofeedback and Health 1987;10:16-25. [Rec#: 2456]
Morisky DE, Bowler MH, Finlay JS. An educational and
behavioral approach toward increasing patient
activation in hypertension management. J Community
Health 1982;7(3):171-82. [Rec#: 3462]
Morisky DE, Levine DM, Green LW, Smith CR. Health
education program effects on the management of
hypertension in the elderly. Arch Intern Med
1982;142(10):1835-8. [Rec#: 3460]
McLaughlin J, Zeeberg I. Self-care and multiple sclerosis: a
view from two cultures. Soc Sci Med 1993;37(3):31529. [Rec#: 847]
McNabb WL, Quinn Mt, Rosing L. Weight loss program
for inner-city black women with non-insulindependent diabetes mellitus: pathways. J Am Diet
Assoc 1993;93:75-77. [Rec#: 2194]
Morrow GR, Asbury R, Hammon S, Dobkin P, Caruso L,
Pandya K, et al. Comparing the effectiveness of
behavioral treatment for chemotherapy-induced
nausea and vomiting when administered by
oncologists, oncology nurses, and clinical
psychologists. Health Psychology 1992;11:250-256.
[Rec#: 2339]
Meadows KA, Fromson B, Gillespie C, et al. Development,
validation and application of computer-linked
knowledge questionnaires in diabetes education.
Diabetic Med 1988 ;5:61. [Rec#: 2087]
Morrow GR, Morell C. Behavioral treatments for the
anticipatory nausea and vomiting induced by cancer
chemotherapy. New England Journal of Medicine
1982;307:1476-1480. [Rec#: 2340]
Merritt GJ, Hall NJ, Kobernus CA, Tanenberg RJ.
Outcome analysis of a diabetic education clinic.
Military Medicine 1983;148:545-547. [Rec#: 2133]
Moynihan M. Assessing the educational needs of postmyocardial infarction patients. Nursing Clinics of
North America 1984;19:441-447. [Rec#: 2433]
Meyer TJ, Mark MM. Effects of psychosocial interventions
with adult cancer patients: a meta-analysis of
randomized experiments [see comments]. Health
Psychol 1995;14(2):101-8. [Rec#: 848]
Muhlauser I, Berger M. Diabetes education and insulin
therapy: when will they ever learn? J Intern Med
1993;233(4):321. [Rec#: 2215]
Miller LV, Goldstein J. More efficient care of diabetic
patients in a county-hospital setting. N Engl J Med
1972;286:1388-1391. [Rec#: 2178]
Muhlhauser I, Bruckner I, Berger M, Cheta D, Jorgens V,
Ionescu-Tirgoviste C, et al. Evaluation of an
intensified insulin treatment and teaching program as
routine management of Type 1 (insulin-dependent)
diabetes. Diabetologia 1987;30:681-690. [Rec#: 2134]
Miller LV, Goldsteing J, Nicolaisen G. Evaluation of
patient's knowledge of diabetes self-care. Diabetes
Care 1978;1:275-280. [Rec#: 2168]
Miller ST, Zwagg RV, Joyner MB, Runyan JW. Evaluation
of a decentralized system for chronic disease care:
seven years observation. Am J Public Health
1980;80:401-405. [Rec#: 2184]
Muhlhauser I, Jorgens V, Berger M, Graninger W, Gurtler
W, Hornke L, et al. Biocentric evaluation of a teaching
and treatment program for Type 1 (insulin-dependent)
diabetic patients: Improvement of metabolic control
and other measures of diabetes care for up to 22
months. Diabetolica 1983;25:470-473. [Rec#: 2135]
Minuchin S, Baker L, Rosman BL, Liebman R, Milman L,
Todd TC. A conceptual model of psychosomatic
illness in children: Family organization and family
therapy. Archives of General Psychiatry
1975;32:1031-1038. [Rec#: 2265]
Muhlhauser I, Sawicki P, Didjurgeit U, et al . Uncontrolled
hypertension in type 1 diabetes: assessment of
patients' desires about treatment and improvement of
blood pressure control by a structured treatment and
teaching program. Diabetic Med 1988 ;5:693-698.
[Rec#: 2092]
Montgomery EB= Jr, Lieberman A, Singh G, Fries JF.
Patient education and health promotion can be
effective in Parkinson's disease: a randomized
controlled trial. PROPATH Advisory Board [see
comments]. Am J Med 1994;97(5):429-35. [Rec#:
849]
Mulhauser I, Jorgens V, Berger M, et al. Bicentric
evaluation of a teaching and treatment program for
type I (insulin-dependent) diabetic patients:
Improvement of metabolic control and other measures
of diabetic care for up to 22 months. Diabetologia
1983;25:470-476. [Rec#: 2384]
177
Rejected Articles
Mullen PD. Cutting back after a heart attack: An overview.
Health Education Monographs 1978;6:295-310.
[Rec#: 2434]
Niemi KBabka JCoe Iet al. Integrating clinical and support
process design for effective health services. Managed
Care Quarterly 1997;5(3):1. [Rec#: 2602]
Mullen PD, Green LW, Persinger GS. Clinical trials of
patient education for chronic conditions: a
comparative meta-analysis of intervention types. Prev
Med 1985;14:753-781. [Rec#: 2350]
Norris SL, Engelgau MM, Narayan KMV. Effectiveness of
self-management training in Type 2 Diabetes. A
systematic review of randomized controlled trials.
Diabetes Care 2001;24:561-587. [Rec#: 3431]
Mullen PD, Laville EA, Biddle AK, Lorig K. Efficacy of
psycho educational interventions on pain, depression,
and disability in people with arthritis: a meta-analysis.
J Rheumatol 1987;14 Suppl 15:33-9. [Rec#: 850]
Nunes EV, Frank KA, Kornfeld DS. Psychologic treatment
for the type A behavior pattern and for coronary heart
disease: a meta-analysis of the literature. Psychosom
Med 1987;49(2):159-73. [Rec#: 854]
Mulloy E, Donaghy D, Quigley C, McNicholas WT. A
one-year prospective audit of an asthma education
program in an out- patient setting. Ir Med J
1996;89(6):226-8. [Rec#: 933]
O'Connor GT, Collins R, Burning JEet al. Rehabilitation
with exercise after myocardial infarction. Circulation
1989;80(2):234-244. [Rec#: 2692]
Mumford E, Schlesinger HJ, Glass GV. The effect of
psychological intervention on recovery from surgery
and heart attacks: an analysis of the literature. Am J
Public Health 1982;72(2):141-51. [Rec#: 852]
O'Connor PJCrabtree BFAbourizk NN. Longitudinal study
of a diabetes education and care intervention:
predictors of improved glycemic control. Journal of
the American Board of Family Practice 1992;5(4):381.
[Rec#: 2603]
Nakagawa-Kogan H. Self-management training: potential
for primary care. Nurse Pract Forum 1994;5(2):77-84.
[Rec#: 853]
O'Leary A, Shoor S, Lorig K, Holman HR. A cognitivebehavioral treatment for rheumatoid arthritis. Health
Psychol 1988;7(6):527-44. [Rec#: 855]
Nath C, Rinehart J. Effects of individual and group
relaxation therapy on blood pressure in essential
hypertensive. Res in Nursing and Health 1979;2:119126. [Rec#: 2462]
Oberman A. Does cardiac rehabilitation increase long-term
survival after myocardial infarction? Circulation
1989;80:416-418. [Rec#: 2691]
Oermann MH, Doyle TH, Clark LR, et al. Effectiveness of
self-instruction for arthritis patient education . Patient
Education and Counseling 1986;8:245-254. [Rec#:
2435]
Nathan DM, Singer DE, Hurzthal K, Goodson JD. The
clinical information value of the glycosylated
hemoglobin assay. New Engl J Med 1984;310:341346. [Rec#: 2100]
Nelson EC, McHugo G, Schnurr P, Devito C, Roberts E,
Simmons J, et al. Medical self-care education for
elders: a controlled trial to evaluate impact. Am J
Publ Health 1984;74(12):1357-1362. [Rec#: 2302]
Oldenburg B, Martin A, Greenwood J, Bernstein L, Allan
R. A controlled trial of a behavioral and educational
intervention following coronary artery bypass surgery.
J Cardiopulm Rehabil 1995;15( 1):39-46. [Rec#:
3464]
Neri M, Migliori GB, Spanevello A, Berra D, Nicolin E,
Landoni CV, et al. Economic analysis of two
structured treatment and teaching programs on asthma.
Allergy 1996;51(5):313-9. [Rec#: 934]
Olivarius NF, Beck-Nielsen H, Andreasen AH, Horder M,
Pedersen PA. Randomised controlled trial of
structured personal care of type 2 diabetes mellitus.
BMJ 2001;323(7319):970-5. [Rec#: 3479]
Nersesian W, Zaremba M. Impact of diabetes outpatient
education program - Maine. Morb Mort Wkly Rep
1983;31:307-314. [Rec#: 2186]
Ornish D, Scherwitz LW, Doody RS, et al. Effects of stress
management training and dietary changes in treating
ischemic heart. JAMA 1983;249:54-59. [Rec#: 2378]
Neuberger GB, Smith KV, Black SO, Hassanein R.
Promoting self-care in clients with arthritis. Arthritis
Care Res 1993;6(3):141-8. [Rec#: 3463]
Osman LM, Abdalla MI, Beattie JA, Ross SJ, Russell IT,
Friend JA, et al. Reducing hospital admission through
computer supported education for asthma patients.
Grampian Asthma Study of Integrated Care
(GRASSIC) [see comments]. BMJ
1994;308(6928):568-71. [Rec#: 856]
Nicholas MK, Wilson PH, Goyen J. Comparison of
operant-behavioral and cognitive-behavioral group
treatment, with and without relaxation training, for
chronic low back pain. Behavior Research and
Therapy 1991;29:225-238. [Rec#: 2295]
Ours P, Wheeler M. Diet education and counseling needs
among inner-city patients with diabetes. Diabetes
1804;33:6A. [Rec#: 2713]
178
Rejected Articles
Owens JF, McCann CS, Hutelmyer CM. Cardiac
rehabilitation: A patients education program. Nursing
Research 1978;27:148-150. [Rec#: 2436]
Peyrot M, McMurray J. Psychosocial factors in diabetes
control: Adjustment of insulin-treated adults.
Psychosomatic Medicine 1985;47:542-557. [Rec#:
2267]
Padgett D, Mumford E, Hynes M, Carter R. Meta-analysis
of the effects of educational and psychosocial
interventions on management of diabetes mellitus. J
Clin Epidemiol 1988;41(10):1007-30. [Rec#: 857]
Peyrot M, Rubin RR. Modeling the effect of diabetes
education on glycemic control. Diabetes Educ
1994;20:143-148. [Rec#: 2639]
Page SRTattersall RB. How to achieve optimal diabetic
control in patients with insulin-dependent diabetes.
Postgraduate Medical Journal 1994;70(828):675.
[Rec#: 2604]
Phillips HC. The effects if behavioral treatment on chronic
pain. Behavior Research and Therapy 1987;25:365377. [Rec#: 2296]
Pichert JW, Smeltzer C, Snyder GM, Gregory RP, Smeltzer
R, Kinzer CK. Traditional vs anchored instruction for
diabetes-related nutritional knowledge, skills, and
behavior. Diabetes Educ 1994;20( 1):45-8. [Rec#:
860]
Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX,
et al. Effects of diet and exercise in preventing
NIDDM in people with impaired glucose tolerance.
The Da Qing IGT and Diabetes Study. Diabetes Care
1997;20 (4):537-44. [Rec#: 3421]
Pilowsky I, Barrow CG. A controlled study of
psychotherapy and amitriptyline used individually and
in combination in the treatment of chronic intractabe,
"psychogenic" pain. Pain 1990;40: 3-19. [Rec#: 2297]
Parker J, Singsen B, Hewett J, Walker S, Hazelwood S,
Hall P, et al. Educating patients with rheumatoid
arthritis: a prospective analysis. Arch Phys Med
Rehabil 1984;65:771-774. [Rec#: 2682]
Podrouzkova BKlabusay LBelobradkova Jet al. The effect
of education on metabolic compensation in diabetics.
Vnitrni Lekarstvi 1992;38(10):959. [Rec#: 2605]
Parker JC, Frank RG, Beck NC, Smarr KL, Buescher KL,
Phillips LR, et al. Pain management in rheumatoid
arthritis patients. A cognitive- behavioral approach.
Arthritis Rheum 1988;31(5):593-601. [Rec#: 858]
Pollack AA/Case DB, Weber MA, et al. Limitations of
transcendental meditation in the treatment of essential
hypertension. Lancet 1977;1:71-73. [Rec#: 2468]
Parker JC, Smarr KL, Buckelew SP, et al . Effects of stress
management on clinical outcomes in rheumatoid
arthritis. Arthritis and Rheumatism 1995;38:1807.
[Rec#: 2084]
Potts M, Brandt K. Analysis of education support group for
patients with rheumatoid arthritis. Pat Counsel Health
Educ 1983;4(30):161-166. [Rec#: 2307]
Parker JC, Smarr KL, Buescher KL, Phillips LR, Frank R,
Beck B, et al. Pain control and rational thinking:
Implications for rheumatoid arthritis. Arthritis and
Rheumatism 1989;32:984-990. [Rec#: 2706]
Powell MF, Burkhart Vde P, Lamy PP. Diabetic patient
compliance as a function of patient counseling. Dug
Intelligence and Cliniccal Pharmacy 1979;13:506-511.
[Rec#: 2138]
Patel CH. 12-month follow-up of yoga and biofeedback in
the management of hypertension . Lancet 1975;1:6264. [Rec#: 2463]
Power L. Group approach to diabetes care. Post grad Med
1983;73(2):211. [Rec#: 2396]
Pratt C, Wilson W, Likely J, et al. The effects of nutrition
education, peer support, and patients' beliefs upon
weight and glycemic control among older noninsulindependent diabetic patients. J Nutr Elder 1987;6
(4):31-43. [Rec#: 2397]
Paulozzi LJ, Norman JE, McMahon P, Frederick AC.
Outcomes of a diabetes education program. Public
Health Rep 1984;99:575-579. [Rec#: 2665]
Perri MG, McAllister DA, Gange JJ, Jordan RC, McAdoo
WG, Nezu AM. Effects of four maintenance programs
on the long-term management of obesity. J Consult
Clin Psychol 1988 ;56:529-534. [Rec#: 2687]
Price MJ. An experiential model of learning diabetes selfmanagement. Qual Health Res 1993;3(1):29-54.
[Rec#: 861]
Peters AL, Davidson MB, Ossorio RC. Management of
patients with Diabetes by nurses with support of subspecialists. HMO Practice 1995;9:8-13. [Rec#: 2422]
Prince R, Frasure-Smith N. Comforting the after-coronary
patient. Can Fam Physician 1984;30:1095-99. [Rec#:
3106]
Peterson CM, Jones RL, Dupuis A, Levine BS, Bernstein
R, O'Shea M. Feasibility of improved blood glucose
control in patients with insulin-dependent diabetes
mellitus. Diabetes Care 1979;2:329-335. [Rec#: 2137]
Quevedo SFBlenkiron PLynch K. Diabetes care
management: experience in the staff and IPA model
HMO. HMO Practice 1998;12(1):44. [Rec#: 2606]
179
Rejected Articles
Rabin SW, Boyko E, Wilson A, Streja DA. A randomized
clinical trial comparing behavior modification and
individual counsel in the nutritional therapy in noninsulin dependent diabetes mellitus: Comparison of
the effect on blood sugar, body weight and serum
lipids. Diabetes Care 1983;6:50-56. [Rec#: 2715]
Rimer B, Levy MH, Keintz MK, Fox L, Engstrom PF,
MacElwee N. Enhancing cancer pain control regimens
through patient education. Patient Education and
Counseling 1987;10:267-277. [Rec#: 2341]
Rippey RM, Billl D, Abeles M, et al. Computer-based
patient education for older persons with osteoarthritis.
Arthritis and Rheumatism 1987;30:932-935. [Rec#:
2437]
Rahe RH, O'Neill T, Hagen A, Arthur RJ. Brief group
therapy following myocardial infarction: eighteen
months follow-up of a controlled trial. Int J Psychiatry
Med 1975;6:349-358. [Rec#: 2405]
Roffman RA. Stress inoculation training in the control of
THC toxicities. International Journal of the Addictions
1986;21:883-896. [Rec#: 2342]
Rahe RH, Tuffli CF, Suchor RJ, at el. group therapy in the
out-patient management of post-myocardial infarction
patients. Psychiatry Med 1973;4:77-88. [Rec#: 2404]
Rosenbaum L. Biofeedback-assisted stress management for
insulin-treated diabetes mellitus. Biofeedback Self
Regul 1983;8:519-532. [Rec#: 2398]
Rakowski W, Hickey T, Dengiz AN. Congruence of health
and treatment perceptions among older patients and
providers of primary care. Int J Aging Hum Dev
1987;25(1):63-77. [Rec#: 862]
Rosenqvist U, Carlson A, Luft R. Evaluation of
comprehensive program for Diabetes care at primary
health-care level. Diabetes Care 1988;11:269-74.
[Rec#: 2423]
Randich SR. Evaluation of a pain management program for
rheumatoid arthritis patients (abstract). Arthritis
Rheum 1982;25:S11. [Rec#: 2684]
Rosenstiel AK, Keefe FJ. The use of coping strategies in
low back pain patients: Relationship to patient
characteristics and current adjustment. Pain
1983;17:33-40. [Rec#: 2298]
Rapley P. Adapting to diabetes: metabolic control and
psychosocial variables. Aust J Adv Nurs 19901991;8(2):41-7. [Rec#: 863]
Rosenstock IM. Understanding and enhancing patient
compliance with diabetic regimens. Diabetes Care
1985;8:610-616. [Rec#: 2268]
Rayman KMEllison GC. When management works: an
organizational culture that facilitates learning to selfmanage type 2 diabetes. Diabetes Educator 1998;
24(5):612. [Rec#: 2607]
Rosenstock J, Raskin P. Diabetes and its complications:
Blood glucose control vs. genetic susceptibility.
Diabetes/Metabolism Reviews 1988;4:417-435.
[Rec#: 2269]
Raymond MW. Teaching toward compliance. Diabetes
Educ 1984;10:42-44. [Rec#: 2637]
Razin AM. Psychosocial intervention in coronary artery
disease: a review. Psychosom Med 1982;44(4):36387. [Rec#: 864]
Rosenthal MM, Carlson ARosenqvist U. Beyond CME:
diabetes education field-interactive strategies from
Sweden. Diabetes Educ 1988;14 :212-17. [Rec#:
3087]
Reaven GM. Beneficial effect of moderate weight loss in
older patients with non- insulin-dependent diabetes
mellitus poorly controlled with insulin. J Am Geriatr
Soc 1985;33(2):93-5. [Rec#: 3424]
Rost KM, Flavin KS, Schmidt LE, McGill JB. Self-care
predictors of metabolic control in NIDDM patients.
Diabetes Care 1990;13(11):1111-3. [Rec#: 867]
Redhead JHussain AGedling Pet al. The effectiveness of a
primary-care-based diabetes education service.
Diabetic Medicine 1993;10 (7):672. [Rec#: 2608]
Rotter J, Anderson C, Rimoin D. Genetics of diabetes
mellitus. In: Ellenberg M, Rifkin H. Diabetes
mellitus: Theory and practice. New York: Medical
Examining Publishing; p. 481-503. [Rec#: 2271]
Rene J, Weinberger M, Mazzuca SA, Brandt KD, Katz BP.
Reduction of joint pain in patients with knee
osteoarthritis who have received monthly telephone
calls from lay personnel and whose medical treatment
regimens have remained stable. Arthritis Rheum
1992;35(5):511-5. [Rec#: 865]
Ruberman W. Psychosocial influences on mortality of
patients with coronary heart disease [editorial;
comment]. JAMA 1992;267(4):559-60. [Rec#: 868]
Rubin RR. Evaluation of an intensive education program
incorporating coping skills training. Abstract of the
46th annual meetings of the American Diabetes
Association. Anaheim, CA. 1986 (Abstract) [Rec#:
3438]
Rich MW, Beckham V, Wittenberg C, Leven CL,
Freedland KE, Carney RM. A multidisciplinary
intervention to prevent the readmission of elderly
patients with congestive heart failure [see comments].
N Engl J Med 1995;333(18):1190-5. [Rec#: 866]
180
Rejected Articles
Rubin RR, Peyrot M, Saudek CD. Effect of diabetes
education on self-care, metabolic control, and
emotional well-being [see comments]. Diabetes Care
1989;12(10):673-9. [Rec#: 869]
Schlesinger HJ, Mumford E, Glass GV, Patrick C,
Sharfstein S. Mental health treatment and medical care
utilization in a fee-for- service system: outpatient
mental health treatment following the onset of a
chronic disease. Am J Public Health 1983;73(4):4229. [Rec#: 873]
Rubin RR/Peyrot M, Saudek CD. Differential effect of
diabetes education on self-regulation and life-style
behaviors. Diabetes Care 1997;14:335-338. [Rec#:
2197]
Schlottman NGrusser MHartmann Pet al. Cost
effectiveness and evaluation of a structured therapy
and education program for insulin-treated type II
diabetic patients in Bradenburg. Zeitschift fur
Arztliche Fortbildung (Jena) 1996;90(5):441. [Rec#:
2609]
Ruggiero L, Prochaska JO. Introduction: Readiness for
change: Application of the transtheoretical model to
diabetes. Diabetes Spectrum 1993;6:22-24. [Rec#:
912]
Schlundt DG, McDonel EC, Langford HG. Compliance in
dietary management of hypertension. Comprehensive
Therapy 1985;11:59-66. [Rec#: 2645]
Runyan JW. The Memphis chronic disease program.
JAMA 1975;231:264-267. [Rec#: 2183]
Ruzicki DA. Promoting patient self-management in the
health care system [editorial]. Patient Educ Couns
1990;15(1):1-2. [Rec#: 870]
Schriffrin A, Belmonte M. Multiple daily self-glucose
monitoring: its essential role on long-term glucose
control in insulin-dependent diabetic patients treated
with pump and multiple subcutaneous injections.
Diabetes Care 1982;5:479-484. [Rec#: 2199]
Salonen JT, Pusha P. A community program for
rehabilitation and secondary prevention for patients
with acute myocardial infarction as part of a
comprehensive community program for control of
cardiovascular diseases (North Karelia Project).
1980;12 :33-42. [Rec#: 2375]
Schulman BA. Active patient orientation and outcomes in
hypertensive treatment. Med Care 1979;17:267-280.
[Rec#: 2663]
Schwartz LH, Marcus RR, Condon R. Multidisciplinary
group therapy for rheumatoid arthritis.
Psychosomatics 1978;19:289-293. [Rec#: 2681]
Sassi-Dambron DE, Eakin EG, Ries AL, Kaplan RM.
Treatment of dyspnea in COPD. A controlled clinical
trial of dyspnea management strategies [see
comments]. Chest 1995;107(3):724-9. [Rec#: 871]
Scott RS, Beaven DW, Stafford JM. The effectiveness of
diabetes education for non-insulin-dependent diabetic
persons. Diabetes Educ 1984;10:36-39. [Rec#: 2193]
Satterfield S, Cutler JA, Langford HG, Applegate WB,
Borhani NO, Brittain E, et al. Trials of hypertension
prevention: phase I design. An Epidemiol 1991;1:455174. [Rec#: 3273]
Sharpe PA, Clark NM, Janz NK. Differences in the impact
and management of heart disease between older
women and men. Women Health 1991;17(2):25-43.
[Rec#: 874]
Savitski P. Evaluation of the effects of community-based
diabetic education, in-patient diabetic education and
social support on diabetic management behaviors and
knowledge related to diabetes. Madison: University of
Wisconsin. 1982. [Rec #: 2143]
Shartner CD, Burish TG, Carey MP. Effectiveness of
biofeedback with progressive muscle relaxation
training in reducing the aversiveness of cancer
chemotherapy: A preliminary report. Japanese Journal
of Biofeedback Research 1985;12:33-40. [Rec#: 2343]
Sawicki PT, Muhlhauser I, Didjurgeit U, Baumgartner A,
Bender R, Berger M. Intensified antihypertensive
therapy is associated with improved survival in type 1
diabetic patients with nephropathy. J Hypertens
1995;13(8):933-8. [Rec#: 3468]
Shearn MA, Fireman BH. Stress management and mutual
support groups in rheumatoid arthritis. Am J Med
1985;78:771-775. [Rec#: 2353]
Schafer LC, Glasgow RE, McCaul KD. Increasing the
adherence of diabetic adolescents. Journal of
Behavioral Medicine 1982;5:353-363. [Rec#: 2273]
Simeoni E, Bauman A, Stenmark J, O'Brien J. Evaluation
of a community arthritis program in Australia:
dissemination of a developed program. Arthritis Care
Res 1995;8(2):102-7. [Rec#: 3465]
Schafer LC, Glasgow RE, McCaul KD, et al. Adhgerence
to IDDM regimens: Relationship to psychosocial
variables and metabolic control. Diabetes Care 1983;
6(5):493-498. [Rec#: 2444]
Skyler JS, Lasky IA, Skyler DL, Robertson Eg, Mintz DH.
Home blood glucose monitoring as an aid in diabetic
management. Diabetes Care 1978;1:150-157. [Rec#:
2712]
Schafer LC, McCaul KD, Glasgow RE. Supportive and
non-supportive family behaviors: relationships to
adherence and metabolic control in persons with type I
diabetes. Diabetes Care 1986;9(2):179-85. [Rec#: 872]
181
Rejected Articles
Smith CJ, Abrahmson MJ, Henshilwood PA, Bonnici F.
The effect of an intensive education program on the
glycemic control of type 1 diabetic patients. south
African Medical Journal 1987;71:164-166. [Rec#:
2145]
Starostina EG, Antsiferov M, Galstyan GR, Trautner C,
Jorgens V, Bott U, et al. Effectiveness and cost-benefit
analysis of intensive treatment and teaching programs
for type 1 (insulin-dependent) diabetes mellitus in
Moscow--blood glucose versus urine glucose selfmonitoring. Diabetologia 1994;37(2):170-6. [Rec#:
3470]
Smith JM, et al. Survey of computer programs for diabetes
management and education. Diabetes Educ
1988;14:412-415. [Rec#: 2088]
Starostina EGAntsiferov MBGalstian GRet al.
Effectiveness of an intensive treatment and training
program for patients with type I diabetes mellitus.
Problemy Endokrinologii 1994;40(3):15. [Rec#: 2611]
Smith JMGohdes D. The impact of diabetes care process on
long-term blood sugar control . AHSR & FHSR
Annual Meeting Abstract Book 1996;13:18. [Rec#:
2610]
Stearns SC, Bernard SL, Fasick SB, Schwartz R, Konrad R,
Ory MG, et al. The economic implications of selfcare: the effect of lifestyle, functional adaptations, and
medical self-care among a national sample of
Medicare beneficiaries. Am J Public Health
2000;90:1608-1612. [Rec#: 3093]
Snyder SE, Winder JA, Creer TJ. Development and
evaluation of an adult asthma self-management
program: Wheezers Anonymous. J Asthma
1987;24(3):153-8. [Rec#: 875]
Sobel DS. Rethinking medicine: improving health
outcomes with cost-effective psychosocial
interventions. Psychosom Med 1995;57(3):234-44.
[Rec#: 876]
Stenstrom CH. Home exercise in rheumatoid arthritis
functional class II: goal setting versus pain attention. J
Rheumatol 1994;21(4):627-34. [Rec#: 879]
Stewart AL, Hays RD, Wells KB, Rogers WH, Spritzer
KL, Greenfield S. Long-term functioning and wellbeing outcomes associated with physical activity and
exercise in patients with chronic conditions in the
Medical Outcomes Study. J Clin Epidemiol
1994;47(7):719-30. [Rec#: 880]
Solowiejczyk JN, Baker L. Physician-patient
communication in chronic illness. Diabetes Care
1981;4(3):427-9. [Rec#: 877]
Sommaruga M, Spanevello A, Migliori GB, Neri M,
Callegari S, Majani G. The effects of a cognitive
behavioral intervention in asthmatic patients. Monaldi
Arch Chest Dis 1995;50(5):398-402. [Rec#: 935]
Stone AA, Porter LS. Psychological coping: Its importance
for treating medical problems. Mind Body Medicine
1995;1(1):46-54. [Rec#: 913]
Sonsken PH, Judd LS, Lowy C. Home monitoring of blood
glucose. Method for improving diabetic control.
Lancet 1978;i:732-735. [Rec#: 2710]
Stone RA, DeLeo J. Psychotherapeutic control of
hypertension . NEJM 1976;294:80-84. [Rec#: 2469]
Spiegel D. Health caring. Psychosocial support for patients
with cancer. Cancer 1994;74(4 Suppl):1453-7. [Rec#:
878]
Stratton R, Wilson DP, Endres RK, Goldstein DE.
Improved glycemic control after supervised 8-week
exercise program in insulin-dependent diabetic
adolescents. Diabetes Care 1987;10:589-593. [Rec#:
2274]
Spiegel D. Mind matters:effects of group support therapy
on cancer patients. Journal of NIH Research
1991;3:61-3. [Rec#: 2415]
Strauss GD, Spiegel JS, Daniels M, Spiegel T, Landsverk J,
Roy-Byrne P, et al. Group therapies for rheumatoid
arthritis. A controlled study of two approaches.
Arthritis Rheum 1986;29(10):1203-9. [Rec#: 881]
Spiegel D, Bloom JR. Group therapy and hypnosis reduce
metastatic breast carcinoma pain. Psychosomatic
Medicine 1983;45:333-339. [Rec#: 2344]
Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM.
The role of self-efficacy in achieving health behavior
change. Health Educ Q 1986;13(1):73-92. [Rec#: 882]
Spiegel JS, Spiegel TM, Ward NB, et al. Rehabilitation for
rheumatoid arthritis patients: a controlled trial.
Arhtritis Rheum 1986;29(5):628. [Rec#: 2354]
Street RL, Piziak VK, Carpentier WS, Herzog J, Hejl J,
Skinner G, et al. Provider-patient communication and
metabolic control. Diabetes Care 1993;16(5):714-21.
[Rec#: 3443]
Sprafka JM, Kurth D, Crozier M, Whipple D, Bishops D.
Response of diabetic patients to a community-based
education program. The Diabetes Educator
1988;14:148-151. [Rec#: 2146]
Streja D, Boyko F, Rabkin SW. Nutrition therapy in noninsulin dependent diabetes mellitus. Diabetes Care
1981;4:81-84. [Rec#: 2400]
182
Rejected Articles
Stunkard AJ, Craighead LW, O'Brien R. Controlled trial of
behavior therapy, pharmacotherapy, and their
combination in the treatment of obesity. Lancet
1980;2:1045-1047. [Rec#: 2648]
Thomson MA, Oxamn AD, Davis DA, et al. outreach visits
to improve health professional practice and health care
outcomes (Cochrane Review). In: The Cochrane
Library, Issue 4. Oxford: Update Software; 1998. [
Rec#: 2622]
Sunin RM. Intervention with Type A behaviors. J Consult
Clin Psychol 1982;50:933-949. [Rec#: 2365]
Tiep BL. Reversing disability of irreversible lung disease.
West J Med 1991;154(5):591-7. [Rec#: 886]
Sunin RM, Bloom LJ. Anxiety management training for
pattern A behavior. J Behav Med 1978;1:25-35.
[Rec#: 2369]
Tierney WMHui SL, McDonald CJ. Delayed feedback of
physician performance versus immediate reminders to
perform preventive care. Effects on physician
compliance. Med Care 1986;24:659-666. [Rec#: 2672]
Surwit RS, Feinglos MN. The effects of relaxation on
glucose tolerance in non-insulin-dependent diabetes.
Diabetes Care 1983;6:176-179. [Rec#: 2275]
Syrjala KL, Cummings C, Donaldson GW. Hynopsis or
cognitive behavioral training for the reduction of pain
and nausea during cancer treatment: A controlled
clinical trial. Pain 1992;48: 137-146. [Rec#: 2345]
Tobin DL, Reynolds RVC, Holroyd KA, Creer TL . Selfmanagement and social learning theory. In: Holroyd
KA, Creer TL. (Eds.) Self-Management of Chronic
Disease: Handbook of Clinical Interventions and
Research. Orlando, FL: Academic Press; 1986. [Rec#:
914]
Taal E, Riemsma RP, Brus HL, Seydel ER, Rasker JJ,
Wiegman O. Group education for patients with
rheumatoid arthritis. Patient Educ Couns 1993;20(23):177-87. [Rec#: 883]
Toeus C, Kaplan R, Atkins C. The costs and effects of
behavioral programs in chronic obstructive pulmonary
disease. Med Care 1984;22(12):1088-1100. [Rec#:
2308]
Taggart VS, Zuckerman AW, Lucas S, Acty-Lindsey A,
Bellanti JA. Adapting a self-managment education
program for asthma for use in an outpatient clinic.
Ann Allergy 1987;58:173-178. [Rec#: 2164]
Bradley C (ed). Handbook of Psychology and Diabetes
Research. Berkshire, England: Hardwood Academic;
1994. [Rec#: 2446]
Toobert DJ, Glasgow RE. Problem-solving and diabetes
self care. Journal of Behavioral Medicine
1991;14(1):71-86. [Rec#: 2447]
Tani GS, Hankin JH. A self-learning unit for patients with
diabetes. Journal of the American Dietetic Association
1971;58:331-335. [Rec#: 2147]
Tulpule TH, Tulpule AT. Yoga, a method of relaxation for
rehabilitation after myocardial infarction. Ind Heart J
1980;32:1-7. [Rec#: 2376]
Tasker PR. The organization of successful diabetes
management in primary care. Diabetic Medicine
1998;15(3):S58. [Rec#: 2612]
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT,
Hamalainen H, Ilanne-Parikka P, et al. Prevention of
type 2 diabetes mellitus by changes in lifestyle among
subjects with impaired glucose tolerance. N Engl J
Med 2001;344(18):1343-50. [Rec#: 3422]
Tattersall RB, McCulloch DK, Aveline M. Group therapy
in the treatment of diabetes. Diabetes Care
1985;8:180-188. [Rec#: 2196]
Telch CF, Telch MJ. Group coping skills instruction and
supportive group therapy for cancer patients: A
comparison of strategies. Journal of Consulting and
Clinical Psychology 1986;54:802-808. [Rec#: 2346]
Turk D, Meichenbaum D. A Cognitive-behavioral approach
to pain management. In: Wall P, Melzack R.
Textbook of Paid . London: Churchill Livingstone;
1994. p. 1337. [Rec#: 2085]
Terent A, Hagfall O, Cederholm U. The effect of education
and self-monitoring of blood glucose on glycosolated
hemoglobin in Type 1 diabetes. Acta Medica
Scandinavica 1985;217:47-53. [Rec#: 2148]
Turk D, Speers M. Diabetes Mellitus: A cognitive
functional analysis of stress. In: Burish T, Bradley L.
(Eds) Coping with chronic disease: Research and
applications. New York: Academic; 1983. [Rec#:
2276]
Thompson LW, Gallagher D, Nies Get al. Evaluation of the
effectiveness of professionals and non-professionals as
instructors of "Coping with Depression" classes for
elders. Gerontologist 1983;23:390-396. [Rec#: 2674]
Turner JA, Clancy S. Comparison of operant-behavioral
and cognitive-behavioral group treatment for chronic
low back pain. Journal of Consulting and Clinical
Psychology 1988;56:261-266. [Rec#: 2299]
Thompson PB. Effectiveness of relaxation techniques in
reducing anxiety and stress factors in type A postmyocardial infarction patients. Dissert Abstr
1977;37A:5616-5617. [Rec#: 2407]
183
Rejected Articles
Turner JA, Clancy S, McQuade KJ, Cardenas DD .
Effectiveness of behavioral therapy for chronic low
back pain: A component analysis. Journal of
Consulting and Clinical Psychology 1990;58:573-579.
[Rec#: 2300]
Wagner EH, Austin BT, Von Korff M. Organizing care for
patients with chronic illness. Milbank Q
1996;74(4):511-44. [Rec#: 894]
Wake N, Hisashige A, Katayama T, Kishikawa H,
Ohkubo Y, Sakai M, et al. Cost-effectiveness of
intensive insulin therapy for type 2 diabetes: a 10-year
follow-up of the Kumamoto study. Diabetes Res Clin
Pract 2000;48(3):201-10. [Rec#: 3420]
Turner MO, Taylor D, Bennett R, Fitzgerald JM. A
randomized trial comparing peak expiratory flow and
symptom self- management plans for patients with
asthma attending a primary care clinic. Am J Respir
Crit Care Med 1998;157(2):540-6. [Rec#: 936]
Walford S, Gale EAM, Allison SP, Tattersall RB. Selfmonitoring of blood glucose. Improvement of diabetic
control. Lancet 1978;i :732-735. [Rec#: 2711]
Udelman HUdelman D. Group therapy with rheumatoid
arthritis patients. Am J Psychother 1978;32:288-299.
[Rec#: 2676]
Wallace N, Wallace DC. Group education after myocardial
infarction: Is it effective? Med J Aust 1977;245-247.
[Rec#: 2373]
van Elderen-van Kemenade T, Maes S, van den Broek Y.
Effects of a health education program with telephone
follow-up during cardiac rehabilitation. Br J Clin
Psychol 1994;33 ( Pt 3):367-78. [Rec#: 888]
Wasilewski YM. Future challenges in asthma management
research [editorial; comment]. J Asthma
1993;30(4):237-9. [Rec#: 895]
Vasterling J, Jenkins RA, Tope DM, Burish TG . Cognitive
distraction and relaxation training for the control of
side effects due to cancer chemotherapy. Journal of
Behavioral Medicine 1993;16:65-80. [Rec#: 2347]
Wasson J, Gaudette C, Whaley F, Sauvigne A, Baribeau P,
Welch HG. Telephone care as a substitute for routine
clinic follow-up. JAMA 1992;267:1788-1793. [Rec#:
2650]
Vickery DM. Medical self-care: a review of the concept
and program models. Am J Health Promotion
1986;Summer:23-28. [Rec#: 2301]
Watkins JD, WilliamsTF, Martin DA. A study of diabetic
patients at home. American Journal of Public Health
1967;57:452-459. [Rec#: 2102]
Vickery DM, Kalmer H, Lowry D, Constantine M, Wright
E, Loren W. Effect of a self-care education program
on medical visits. JAMA 1983;250(21):2952-6.
[Rec#: 890]
Watts FN. Behavioral aspects of the management of
diabetes mellitus: Education, self-care and metabolic
control. Behavior Research and Therapy 1980;18:171180. [Rec#: 2278]
Vignos P, Parker W, Thompson H. Evaluation of a clinic
education program for patients with rheumatoid
arthritis. J Rheumatol 1976;3:155-156. [Rec#: 2675]
Watts NB, Spanheimer RG, DiGirolamo M, Gebhart SS,
Musey VC, Siddiq YK, et al. Prediction of glucose
response to weight loss in patients with non- insulindependent diabetes mellitus. Arch Intern Med
1990;150(4):803-6. [Rec#: 3423]
Vijan SStevens DLHerman et al. Screening, prevention,
counseling, and treatment for the complications of
type II diabetes mellitus. Putting evidence into
practice. Journal of General Internal Medicine
1997;12 (9):567. [Rec#: 2613]
Webb KL, Dobson AJ, Tupling HE, Harris GW, O'Connell
DL, Atkinson J, et al. Evaluation of a diabetes
education program. Australia New Zeland Journal of
Medicine 1982;12:153-160. [Rec#: 2153]
Vinicor F. Is diabetes a public-health disorder? Diabetes
Care 1994;17 Suppl 1:22-7. [Rec#: 891]
Wetstone SL, Sheehan TJ, Votaw RG, et al. Evaluation of a
computer based education lesson for patients with
rheumatoid arthritis. J Rheumatology 1985;12:907912. [Rec#: 2356]
VinicourF, Cohen SJ, Mazzuca SA, Moorman N, Wheeler
M, Keubler T, et al. Diabetes: A randomized trial of
the effects of physician and/or patient education on
diabetes patient outcomes. Journal of Chronic Disease
1987;40:2345-2356. [Rec#: 2277]
Wheeler M, Ours P, Swinder C, Wheeler L. A clinical trial
of a computer based self-education program for
diabetics. Diabetes 1804;33:6A. [Rec#: 2993]
Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH.
Collaborative management of chronic illness. Ann
Intern Med 1997;127(12):1097-102. [Rec#: 3480]
Wheeler ML, Warren-Boulton E. Diabetes patient
education programs: quality and reimbursement.
Diabetes Care 1992;(Suppl 1):36. [Rec#: 2171]
Wagner EH. Population-based management of diabetes
care. Patient Educ Couns 1995;26(1-3):225-30. [Rec#:
893]
184
Rejected Articles
Whitehouse FW, Whitehouse IJ, Cox MS, Goldman J,
Kahkonen DM, Prtamian JO, et al. Outpatient
regulation of the isulin-requiring person with diabetes
(an alternative to hospitalization). J Chron Dis
1983;36:433-438. [Rec#: 2185]
Wing RR/Marcus MD, Epstein LH, Salata R. Type II
diabetic subjects lose less weight than their
overweight non-diabetic spouses. Diabetes Care
1987;10:563-533. [Rec#: 2287]
Wylie-Rosett J. Development of new educational strategies
for persons with diabetes. J Am Diet Assoc
1982;81:268-271. [Rec#: 2702]
Whitehouse FW, Whitehouse IJ, Smith J, Hohl Rd.
Teaching the person with diabetes: experience with a
follow-up session. Diabetes Care 1979;2:35-38.
[Rec#: 2708]
Wysocki M, Czyzyk A, Slonska Z, Krolewski A, Janecsko
D. Health behavior and its determinants among
insulin-dependent diabetics: results of the Diabetes
Warsaw Study. Diabete Metab 1978;4: 117-122.
[Rec#: 2169]
Williams TF, Martin DA, Hogan MD, et al . The clinical
picture of diabetic control studied in four settings. Am
J Public Health 1967;57:441-451. [Rec#: 2306]
Wilson DP, Endres RK. Compliance with blood glucose
monitoring in children with Type I diabetes mellitus.
Journal of Paediatrics 1986;108:1022-1024. [Rec#:
2280]
Yoon R, McKenzie DK, Bauman A, Miles DA. Controlled
trial evaluation of an asthma education program for
adults. Thorax 1993;48(11):1110-6. [Rec#: 902]
Yoshida M, Morishima T, Izumi K, Abe H. A computer
assisted instruction of exercise therapy for diabetics.
In: Shigeta Y, Lebovitz HE, Gerich JE, Malaisse WJ.
Best approach to the ideal therapy of diabetes mellitus.
Amsterdam: Excerpta Medica; 1987. p. 391-394.
[Rec#: 2161]
Wilson-Pessano S, Scamagas P, Arsham GM, Chardon L,
Stamatki C, German DF, et al. An evaluation of
approaches to asthma self-management education for
adults: The AIR/Kaisr-Permanente study. Health
Educ Q 1987;17 :333-343. [Rec#: 2162]
Wilson RM, Clarke P, Barkes H, Heller SR, Tattersall RB.
Starting insulin treatment as an outpatient. Journal of
the American Medical Association 1986;256:877-880.
[Rec#: 2155]
Zeiger RS, Heller S, Mellon MH, Wald J, Falkoff R, Schatz
M. Facilitated referral to asthma specialist reduces
relapses in asthma emergency room visits [published
erratum appears in J Allergy Clin Immunol 1992
Aug;90(2):278]. J Allergy Clin Immunol
1991;87(6):1160-8. [Rec#: 938]
Wilson SR, Scamagas P, German DF, Hughes GW, Lulla
S, Coss S, et al. A controlled trial of two forms of selfmanagement education for adults with asthma [see
comments]. Am J Med 1993;94(6):564-76. [Rec#:
901]
Ziegler O, Koloppo M, Louis J, Musse JP, Patris A, Debry
G, et al. Self-monitoring of blood glucose and insulin
dose alteration in type 1 diabetes mellitus. Diabetes
Res Clin Pract 1993;21(51-59). [Rec#: 2200]
Wilson W, Ary DV, Biglan A, Glasgow RE, Toobert DJ,
Campbell DR. Psychosocial predictors of self-care
behaviors (compliance) and glycemic control in noninsulin-dependent diabetes mellitus. Diabetes Care
1986;9(6):614-22. [Rec#: 899]
Zimmerman L, Pozehl B, Duncan K, Schmitz R. Effects of
music in patients who had chronic cancer pain.
Western Journal of Nursing Research 1989;11:298309. [Rec#: 2349]
Wing RR. Behaviorial strategies for weight reduction in
obese Type II diabetic patients. Diabetes Care
1989;12:139-144. [Rec#: 2641]
Zimmet P, Gilbert P, Gifford S, Songer T. The Diabetes
Education and Control Program in Victoria and its
evaluation. Transactions of the Menzies Foundation
1987;13:57-73. [Rec#: 2288]
Wing RR, Epstein LH, Nowalk MP, Lamparski D.
Behavioral self-regulation in the treatment of patients
with diabetes mellitus. Psychological Bulletin
1986;99:78-89. [Rec#: 2282]
Zurawski RM, Smith TW, Houston BK. Stress
management for essential hypertension: Comparison
with a minimally effective treatment, predictors of
response to treatment, and effects on reactivity. J
Psychosomatic Res 1987;31:453-462. [Rec#: 2455]
Wing RR, Epstein LH, Nowalk MP, Scott N, Koeski R.
Compliance to self-monitoring of blood glucose: A
marked item technique compared with self-report.
Diabetes Care 1985;8:456-460. [Rec#: 2284]
Wing RR, Koeski R, Epstein LH, Nowalk MP, Gooding
MS, Becker D. Long term effects of modest weight
loss in Type II diabetic patients. Archives of Internal
Medicine 1987 ;147:1749-1753. [Rec#: 2286]
185
Evidence Table 1: Diabetes
First Author
Year
(ID)
Allen BT, 1990
(#2201)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
RCT
Jadad Score: 3
Diagnostic criteria:
FBS
Comorbidities:
Obesity and
cholesterol
Intervention
Arm Sample Size
1 Dietary monitoring (Office visit)
Education (Office visit)
Education (One-on-one)
Education (Reading material)
Exercise diary (Office visit)
Feedback (Office visit)
Practice methods (Protocols)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
No
n/a
n Entered: n/a
n Analyzed: 27
2
Dietary monitoring (Office visit)
Education (Office visit)
Education (One-on-one)
Education (Reading material)
Exercise diary (Office visit)
Feedback (Office visit)
Practice methods (Protocols)
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Patients who self monitored diabetes using
urine testing (arm 1) had similar statistically
significant reductions in fasting blood glucose,
glycosylated hemoglobin, and weight as did
patients utilizing serum glucose testing (arm 2).
No appreciable differences between groups
were noted.
Follow-up times: 1 MO, 2 MO, 3 MO, 4 MO, 5
MO, 6 MO
n Entered: n/a
n Analyzed: 27
Anderson R M, 1995 Diabetes (n/a)
(#747)
CCT
1
Usual Care (n/a)
n Entered: n/a
n Analyzed: 23
Jadad Score: 0
Diagnostic criteria:
n/a
Comorbidities:
n/a
2
Education (Group meeting)
Education (Video/audio tapes)
Feedback (Group meeting)
n Entered: n/a
n Analyzed: 22
Excluded from meta-analysis as not
randomized.
Patients receiving a patient empowerment
education program (arm 2) had reductions in
glycosylated hemoglobin that were greater than
controls and were statistically significant
(p=0.05). Intervention subjects also improved in
all self-efficacy sub-scales, which were
sustained at 12-week follow-up.
Follow-up times: 6 WK, 12 WK
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
186
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Anon, DICET, 1994
(#2614)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes
(Types I and II)
Intervention
Arm Sample Size
1 Control (n/a)
Reminders (Mail)
RCT
n Entered: 135
n Analyzed: 111
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Jadad Score: 2
Diagnostic criteria:
n/a
2
Comorbidities:
Hypertension,
neuropathy, and
cholesterol
Arseneau D L, 1994
(#749)
Diabetes (Type II)
Practice methods (Reading material)
Reminders (Computer program)
Reminders (Mail)
n Entered: 139
n Analyzed: 124
1
Education (Group meeting)
Education (Instructional manuals)
RCT
n Entered:
20
n Analyzed: n/a
Jadad Score: 1
Diagnostic criteria:
n/a
Comorbidities:
n/a
2
Education (Group meeting)
Education (Office visit)
n Entered:
20
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
No
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Patients randomized to intervention (arm 2) had
a greater number of MD evaluations but no
difference in diabetes related hospitalizations
compared with controls (arm 1). BMI trends
were higher in intervention patients compared
with controls, but there were no treatment
differences in glycosylated hemoglobin, systolic
or diastolic blood pressure. There were also no
significant differences in diabetes knowledge,
anxiety, depression, satisfaction with treatment
or self reported well-being.
Follow-up times: 2 YR
Excluded from meta-analysis as no usual care
or comparable control group.
Though knowledge and% ideal body weight
significantly improved for Learning Activity
Packages (arm 1) at 5 months and HgbA1c and
behavior improved for diabetes class arm, only
knowledge scores were significantly higher at 5
months for the LAP arm.
Follow-up times: 2 MO, 5 MO
187
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Aubert RE, 1998
(#2581)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes
(Types I and II)
RCT
Intervention
Arm Sample Size
1 Control (n/a)
Advocacy training (One-on-one)
Counseling/therapy (One-on-one)
Education (Group meeting)
Follow up (One-on-one)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Jadad Score: 1
Diagnostic criteria:
MD
n Entered:
67
n Analyzed: n/a
2
Comorbidities:
Obesity, DM,
tobacco abuse, and
cholesterol
Advocacy training (One-on-one)
Consultation w/specialists (Protocols)
Counseling/therapy (One-on-one)
Counseling/therapy (Telephone)
Education (Group meeting)
Education (One-on-one)
Follow up (One-on-one)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
No
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Intervention subjects (arm 2) had greater
decreases in HbA1c levels than those receiving
usual care (arm 1) (1.7% versus 0.6% p<0.01).
Fasting serum glucose was lower in intervention
subjects by a mean of 48 mg/dl versus 15 mg/dl
(p=0.003). Self-rated health also improved in
the intervention group (p=0.02).
Follow-up times: 6 MO, 12 MO
n Entered:
71
n Analyzed: n/a
Bethea DC, 1989
(#2105)
Diabetes
(Types I and II)
1
Control (n/a)
Education (One-on-one)
Education (Reading material)
CCT
n Entered:
12
n Analyzed: 12
Jadad Score: 0
Diagnostic criteria:
n/a
Comorbidities:
n/a
2
Education (One-on-one)
Education (Reading material)
Education (Video/audio tapes)
n Entered:
12
n Analyzed: 12
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Excluded from meta-analysis as not
randomized.
Use of videotape instruction (arm 2) resulted in
similar diabetes knowledge levels compared
with conventional instruction in hospitalized
patients (arm 1).
Follow-up times: 45 MI
188
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Bloomgarden ZT,
1987
(#2172)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes
(Types I and II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered: 180
n Analyzed: 139
RCT
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Jadad Score: 2
2
Diagnostic criteria:
n/a
Comorbidities:
Heart disease,
hypertension, kidney
disease, tobacco
abuse, cholesterol
and retinopathy
Education (Group meeting)
Education (Other mechanisms)
Education (Video/audio tapes)
n Entered: 165
n Analyzed: 127
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Follow-up time not in 3 - 12 months.
Though subjects randomized to an education
intervention (arm 2) demonstrated increased
knowledge compared with usual care group
(arm 1) (p=0.007) and had significant reductions
in HbA1c and fasting blood glucose, these
reductions in biochemical markers were not
significantly greater than in the usual care
group. There were also no changes in
cholesterol, blood pressure, or foot lesions and
health service utilization was unaffected.
Follow-up times: 18 MO
189
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Boehm S, 1993
(#754)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
RCT
n Entered:
41
n Analyzed: 41
Jadad Score: 1
Diagnostic criteria:
n/a
2
Comorbidities:
n/a
Cognitive-behavioral (Office visit)
Contracts (Office visit)
Material incentive (Other mechanisms)
n Entered:
32
n Analyzed: 32
3
Cognitive-behavioral (Office visit)
Contracts (Office visit)
Feedback (Office visit)
Material incentive (Other mechanisms)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Behavioral strategy interventions (arms 2, 3 and
4) resulted in no differences in glycosylated
hemoglobin and weight loss between
intervention and control groups.
Follow-up times: n/a
n Entered:
42
n Analyzed: 42
4
Cognitive-behavioral (Office visit)
Contracts (Office visit)
Education (Group meeting)
Education (Instructional manuals)
Feedback (Office visit)
Material incentive (Other mechanisms)
n Entered:
41
n Analyzed: 41
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
190
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Campbell EM, 1996
(#2586)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Control (n/a)
Education (One-on-one)
RCT
n Entered:
59
n Analyzed: 59
Jadad Score: 1
Diagnostic criteria:
n/a
Comorbidities:
Hypertension and
tobacco abuse
2
Education (Group meeting)
Education (One-on-one)
n Entered:
66
n Analyzed: 38
3
Education (Group meeting)
Education (One-on-one)
n Entered:
57
n Analyzed: 34
4
Cognitive-behavioral (Home visit)
Cognitive-behavioral (One-on-one)
Cognitive-behavioral (Telephone)
Contracts (One-on-one)
Education (One-on-one)
Feedback (One-on-one)
Social support (n/a)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Control (arm 1) were more likely to have an
increase in intensity of diabetes treatment at 6month follow-up (p=0.04) than intervention
subjects (arms 2, 3, and 4). Behavior program
(arm 4) and group education (arm 2) patients
had greater improvement in knowledge scores
at 6-month follow-up, but differences were not
sustained at 12 months. Greater reductions in
diastolic blood pressure were seen for those
attending behavioral interventions (p=0.02). No
difference in change between groups occurred
for HbA1c, BMI, total cholesterol, or systolic
blood pressure.
Follow-up times: 3 MO, 6 MO, 12 MO
n Entered:
56
n Analyzed: 51
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
191
Evidence Table 1: Diabetes (con't)
Condition (Type)
Study Design
First Author
Quality
Year
Population
(ID)
Characteristics
D'Eramo-Melkus GA, Diabetes (Type II)
1992
(#2202)
RCT
Intervention
Arm Sample Size
1 Control (n/a)
Education (n/a)
n Entered:
28
n Analyzed: 19
Jadad Score: 2
Diagnostic criteria:
HgbA1C and GTT
2
Comorbidities:
Obesity
Education (Group meeting)
Education (One-on-one)
Education (n/a)
Goal setting (Group meeting)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
Yes
n/a
n Entered:
28
n Analyzed: 19
3
Counseling/therapy (One-on-one)
Education (Group meeting)
Education (One-on-one)
Education (n/a)
Goal setting (Group meeting)
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Fasting blood glucose (mM) at 6 months:
Arm 1 = 12.2 (5.5)
Arm 2 = 9.5 (3.6)
Arm 3 = 9.0 (3.0)
HbA1 (%) at 6 months:
Arm 1 = 10.5 (3.2)
Arm 2 = 9.2 (3.3)
Arm 3 = 8.3 (2.7)
Weight (lbs) at 6 months:
Arm 1 = 205.1 (25.6)
Arm 2 = 200.7 (30.4)
Arm 3 = 191.8 (31.7)
Follow-up times: 3 MO, 6 MO
n Entered:
26
n Analyzed: 19
de Bont AJ, 1981
(#2210)
Diabetes (Type II)
1
RCT
Jadad Score: 2
Diagnostic criteria:
n/a
Comorbidities:
Obesity and tobacco
abuse
Control (n/a)
Counseling/therapy (Home visit)
Counseling/therapy (n/a)
n Entered: n/a
n Analyzed: 65
2
Counseling/therapy (Home visit)
Counseling/therapy (n/a)
n Entered: n/a
n Analyzed: 65
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Excluded from meta-analysis as no usual care
or comparable control group.
Patients in both intervention group (arm 2) and
control group (arm 1) lost weight. Though
cholesterol levels fell significantly in the low fat
group (arm 2) (p<0.001), mean plasma glucose
and HbA1c remained unchanged.
Follow-up times: 6 MO
192
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Emori KH, 1964
(#2118)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
RCT
n Entered:
13
n Analyzed: 13
Jadad Score: 2
Diagnostic criteria:
MD
2
Comorbidities:
Obesity
Falkenberg MG, 1986 Diabetes (Type II)
(#2190)
RCT
n Entered:
13
n Analyzed: 13
1
Comorbidities:
Obesity
Control (n/a)
Education (Group meeting)
n Entered:
18
n Analyzed: 22
Jadad Score: 2
Diagnostic criteria:
n/a
Education (One-on-one)
Education (Reading material)
Education (Video/audio tapes)
2
Education (Group meeting)
Education (Instructional manuals)
n Entered:
27
n Analyzed: 22
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Follow-up time not in 3 - 12 months.
Intervention subjects (arm 2) had greater
knowledge (p<0.005) and lower glycosylated
levels (10.4% versus 11.8%, p<0.05) than usual
care group (arm 1) did at 4-6 weeks after the
program concluded. Change in body weight was
not different between groups.
Follow-up times: 5 DY, 4 WK
HbA1 (%) at 6 months:
Arm 1 = 8.1 (1.0)
Arm 2 = 7.2 (0.9)
Follow-up times: 3 MO, 9 MO
193
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Frost G, 1994
(#791)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
RCT
n Entered:
30
n Analyzed: 25
Jadad Score: 3
Diagnostic criteria:
n/a
2
Comorbidities:
n/a
Counseling/therapy (Instructional
manuals)
Counseling/therapy (Reading material)
Dietary monitoring (Instructional manuals)
Dietary monitoring (Office visit)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Fasting blood glucose (mmol/L) at 12 weeks:
Arm 1 = 9.8 (3.1)
Arm 2 = 9.6 (3.0)
Weight (kg) at 12 weeks:
Arm 1 = 82.9 (14.8)
Arm 2 = 84.8 (23.5)
Follow-up times: 4 WK, 12 WK
n Entered:
30
n Analyzed: 25
Glasgow RE/Toobert Diabetes (Type II)
DJ, 1989
(#2209)
RCT
1
Usual Care (n/a)
n Entered:
22
n Analyzed: 18
Jadad Score: 1
Diagnostic criteria:
HgbA1C and MD
2
Education (Group meeting)
n Entered:
20
n Analyzed: 20
Comorbidities:
n/a
Insufficient statistics for meta-analysis.
Individuals participating in 2 nutrition groups
(arms 2 and 3) demonstrated decreased caloric
intake compared with usual care group (arm 1).
The addition of a social learning program (arm
3) had a significant decrease in weight at 2month follow-up. Intervention conditions
produced a marginal improvement in fasting
blood glucose (p<0.08).
Follow-up times: 2 MO, 2 MO
3
Dietary monitoring (Group meeting)
Education (Group meeting)
n Entered:
23
n Analyzed: 23
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
194
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Glasgow RE, 1992
(#2212)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
RCT
n Entered:
50
n Analyzed: 52
Jadad Score: 1
Diagnostic criteria:
Welborn
2
Comorbidities:
Heart disease and
arthritis
Glasgow R E, 1996
(#799)
Diabetes
(Types I and II)
Cognitive-behavioral (Group meeting)
Education (Group meeting)
Exercise program (Group meeting)
n Entered:
52
n Analyzed: 52
1
Usual Care (n/a)
n Entered: n/a
n Analyzed: n/a
RCT
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
Yes
Jadad Score: 2
2
Diagnostic criteria:
MD
Comorbidities:
n/a
Clinical reviews w/patient (Telephone)
Consultation w/specialists (Office visit)
Education (Reading material)
Education (Video/audio tapes)
Feedback (Computer program)
Reminders (Telephone)
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Glycosolated hemoglobin (%) at 6 months:
Arm 1 = 6.4 (1.4)
Arm 2 = 6.7 (1.7)
Weight (lbs) at 6 months:
Arm 1 = 181.0 (34.7)
Arm 2 = 186.1 (32.6)
Follow-up times: 10 WK
Insufficient statistics for meta-analysis.
Patients who received a brief intervention (arm
2) had no improvement in HbA1C at 3-month
follow-up when compared with usual care group
(arm 1). However serum cholesterol was
significantly lower (p<0.001) in the intervention
group as were 4 dietary behavioral measures.
Though patient satisfaction was improved,
quality of life was not.
Follow-up times: 3 MO
n Entered: n/a
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
195
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Greenfield S, 1988
(#803)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (n/a)
RCT
Intervention
Arm Sample Size
1 Control (n/a)
Clinical reviews w/patient (One-on-one)
Education (Office visit)
Education (Reading material)
Jadad Score: 1
n/a
n/a
n/a
n/a
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
HbA (%) at 12 weeks:
Arm 1 = 10.6 (2.2)
Arm 2 = 9.1 (1.9)
Follow-up times: 12 WK
n Entered:
34
n Analyzed: 33
Diagnostic criteria:
n/a
2
Comorbidities:
n/a
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Advocacy training (Office visit)
Clinical reviews w/patient (Office visit)
Education (Reading material)
n Entered:
39
n Analyzed: 33
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
196
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Hanefield M, 1991
(#2595)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
RCT
Intervention
Arm Sample Size
1 Control (n/a)
Counseling/therapy (Office visit)
Reminders (Office visit)
Jadad Score: 2
n Entered: 378
n Analyzed: 346
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Diagnostic criteria:
FBS and GTT
Comorbidities:
Hypertension,
obesity, tobacco
abuse, and
hyperlipoproteinemia
2
Clinical reviews w/patient (One-on-one)
Counseling/therapy (Office visit)
Education (Group meeting)
Education (Reading material)
Placebo medication (n/a)
Reminders (Office visit)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Intervention subjects (arms 2 and 3) reported
greater physical activity than controls (arm 1) at
5-year follow-up (p<0.01). Intervention subjects
also had better control of glucose and lower
systolic blood pressure (143 versus 154 mmHg,
p<0.01) and required fewer antidiabetic drugs.
Though no differences between groups were
noted for myocardial infarction incidence,
cumulative incidence mortality rates suggested
a benefit from intervention.
Follow-up times: 2 YR, 5 YR
n Entered: 382
n Analyzed: 328
3
Cholesterol lowering medication (n/a)
Clinical reviews w/patient (One-on-one)
Counseling/therapy (Office visit)
Education (Group meeting)
Education (Reading material)
Reminders (Office visit)
n Entered: 379
n Analyzed: 334
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
197
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Hassell J, 1975
(#2121)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (n/a)
Intervention
Arm Sample Size
1 Control (n/a)
Education (One-on-one)
RCT
n Entered:
24
n Analyzed: 22
Jadad Score: 2
Diagnostic criteria:
n/a
Hoskins PL, 1993
(#2597)
Comorbidities:
n/a
Diabetes
(Types I and II)
2
Education (Group meeting)
RCT
n/a
n/a
n/a
n/a
n/a
n Entered:
65
n Analyzed: 65
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
No
No
n/a
n/a
n/a
n/a
n/a
Education (n/a)
Practice methods (Protocols)
Reminders (n/a)
(Care provided by specialists and
generalists)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
No
n/a
n Entered:
21
n Analyzed: 19
1
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Control (n/a)
Education (n/a)
Jadad Score: 1
2
Diagnostic criteria:
MD
Comorbidities:
Hypertension and
obesity
n Entered:
69
n Analyzed: 69
3
Education (n/a)
Practice methods (Protocols)
(Care provided by generalists alone)
n Entered:
72
n Analyzed: 72
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no relevant
outcomes.
Classroom teaching methods (arm 2) resulted in
greater diabetes knowledge compared with
traditional bedside teaching methods (arm 1)
(77% post-test scores compared with 56%).
Follow-up times: n/a
Excluded from meta-analysis as no usual care
or comparable control group.
Subjects who participated in a system of care
shared between specialist and generalist (arm
2) had significantly greater visit compliance than
those with generalists alone (arm 3) (72%
versus 35%, p<0.04). HbA1c improved
significantly in all 3 groups but no differences
between groups were noted. Nor were there
blood pressure differences between groups and
weight decreased marginally in all 3 groups
though this was statistically significant only in
the shared care group (arm 2) (p<0.04).
Follow-up times: 1 YR
198
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Jaber LA, 1996
(#2598)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
RCT
n Entered:
22
n Analyzed: 17
Jadad Score: 2
Diagnostic criteria:
n/a
2
Comorbidities:
Hypertension,
obesity, and
hyperlipedemia
Jennings PE, 1987
(#2126)
Diabetes (Type I)
1
Jadad Score: 1
2
Comorbidities:
n/a
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
Tailored:
Group Setting:
n Entered:
30
Feedback:
n Analyzed: 30
Psychological:
Primary MD:
Patient directed discussion group (Group Tailored:
meeting)
Group Setting:
Feedback:
n Entered:
30
Psychological:
n Analyzed: 30
Primary MD:
n/a
n/a
n/a
n/a
n/a
Yes
Yes
No
No
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Fasting blood glucose (mmol/L) at 4 months:
Arm 1 = 11.0 (3.9)
Arm 2 = 8.5 (2.3)
Glycated hemoglobin (%) at 4 months:
Arm 1 = 12.1 (3.7)
Arm 2 = 9.2 (2.1)
Follow-up times: 4 MO
n Entered:
23
n Analyzed: 17
RCT
Diagnostic criteria:
n/a
Consultation w/specialists (One-on-one)
Counseling/therapy (One-on-one)
Education (One-on-one)
Education (Reading material)
Feedback (One-on-one)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Usual Care (n/a)
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
HbA1 level (%) at 12 months:
Arm 1 = 10.9 (2.3)
Arm 2 = 9.9 (2.3)
Follow-up times: 6 MO, 12 MO
199
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Kaplan, 1985
(#2817)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Control (n/a)
Education (Group meeting)
RCT
n Entered: n/a
n Analyzed: 15
Jadad Score: 1
Diagnostic criteria:
FBS and MD
2
Comorbidities:
Obesity
Cognitive-behavioral (Group meeting)
Dietary monitoring (Self-delivery)
Education (Group meeting)
n Entered: n/a
n Analyzed: 16
3
Cognitive-behavioral (Group meeting)
Contracts (Group meeting)
Exercise diary (Self-delivery)
Exercise program (Group meeting)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Those participating in the diet intervention (arm
2) lost more weight than the other 3 groups
(arms 1, 3, and 4) (p<0.05). HDL cholesterol
was also significantly higher in this group
(p<0.01). No differences in glycosylated
hemoglobin between groups were noted.
Follow-up times: 3 MO
n Entered: n/a
n Analyzed: 18
4
Cognitive-behavioral (Group meeting)
Contracts (Group meeting)
Dietary monitoring (Self-delivery)
Education (Group meeting)
Exercise diary (Self-delivery)
Exercise program (Group meeting)
n Entered:
.
n Analyzed: 16
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
200
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Kaplan RM, 1987
(#2175)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
RCT
Intervention
Arm Sample Size
1 Control (n/a)
Education (Group meeting)
Education (n/a)
Financial incentives (Group meeting)
Jadad Score: 2
n/a
n/a
n/a
n/a
n/a
n Entered: n/a
n Analyzed: n/a
Diagnostic criteria:
FBS and MD
Comorbidities:
Obesity
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
2
Cognitive-behavioral (Group meeting)
Dietary monitoring (Other mechanisms)
Education (n/a)
Exercise program (Group meeting)
Feedback (Group meeting)
Financial incentives (Group meeting)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
At 18-months follow-up diabetic patients
receiving behavioral interventions in a combined
diet and exercise program (arms 2, 3, and 4)
achieved greater reductions in glycosylated
hemoglobin than those receiving only diet,
exercise, or control interventions (arm 1)
(p<0.05). Changes between other interventions
were not significant. Improvements in quality of
life measures were also greatest in the
combined group (arm 2) (p<0.05).
Follow-up times: 3 MO, 6 MO, 12 MO, 18 MO
n Entered: n/a
n Analyzed: n/a
3
Cognitive-behavioral (Group meeting)
Contracts (Group meeting)
Education (Group meeting)
Exercise program (Group meeting)
Feedback (Group meeting)
Financial incentives (Group meeting)
n Entered: n/a
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
201
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Condition (Type)
Study Design
Quality
Population
Characteristics
Intervention
Arm Sample Size
4 Cognitive-behavioral (Group meeting)
Dietary monitoring (Group meeting)
Education (n/a)
Exercise program (Group meeting)
Financial incentives (Group meeting)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Yes
Yes
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
n Entered: n/a
n Analyzed: n/a
Kendall PA, 1990
(#2207)
Diabetes (Type II)
1
RCT
Jadad Score: 1
Diagnostic criteria:
n/a
Education (Group meeting)
Education (Instructional manuals)
Education (Video/audio tapes)
n Entered: n/a
n Analyzed: 41
2
Comorbidities:
n/a
Education (Group meeting)
Education (Reading material)
Education (Video/audio tapes)
n Entered: n/a
n Analyzed: 42
Kinmonth AL, 1998
(#2599)
Diabetes (Type II)
1
Control (n/a)
Education (Group meeting)
RCT
Jadad Score: 1
n Entered: 161
n Analyzed: 108
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Excluded from meta-analysis as no usual care
or comparable control group.
Both diet guide (arm 1) and exchange lists
treatment group (arm 2) demonstrated
significantly higher levels of self-efficacy
compared with their pre-workshop scores
(p<0.05). Knowledge scores were also
significantly higher in both groups (p<0.01).
Applied nutrition knowledge scores were
however greater for the diet guide group
(p<0.01).
Follow-up times: 3 MO, 6 MO
Excluded from meta-analysis as no usual care
or comparable control group.
The intervention group (arm 2) reported better
communication with doctors, greater treatment
satisfaction and sense of well-being. BMI and
202
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Korhonen T, 1983
(#2259)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diagnostic criteria:
MD
Comorbidities:
Heart disease,
hypertension,
obesity, and tobacco
abuse
Diabetes (n/a)
Intervention
Arm Sample Size
2 Advocacy training (Reading material)
Education (Group meeting)
Education (Instructional manuals)
Practice methods (Group meeting)
1
Control (n/a)
Clinical reviews w/patient (Office visit)
Education (One-on-one)
Education (Reading material)
Jadad Score: 1
2
Comorbidities:
n/a
Clinical reviews w/patient (Office visit)
Education (Group meeting)
Education (One-on-one)
n Entered:
39
n Analyzed: 37
1
Usual Care (n/a)
n Entered: n/a
n Analyzed: 51
RCT
Jadad Score: 1
Diagnostic criteria:
n/a
Comorbidities:
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
No
Yes
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
No
No
No
No
n Entered:
38
n Analyzed: 37
Diagnostic criteria:
n/a
Diabetes (n/a)
Yes
Yes
No
Yes
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
triglyceride concentrations were, however, lower
in the intervention group (arm 2) then in the
control group (arm 1).
Follow-up times: 1 YR
n Entered: 199
n Analyzed: 142
RCT
Kumana CR/Ma JT,
1988
(#2130)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
2
Education (Reading material)
n Entered: n/a
n Analyzed: 56
Fasting blood glucose (mmol/L) at 6 months:
Arm 1 = 7.9 (3.6)
Arm 2 = 8.3 (3.6)
Follow-up times: 1 MO, 3 MO, 6 MO, 9 MO, 12
MO, 15 MO, 18 MO
Excluded from meta-analysis as no relevant
outcome.
Of diabetic patients receiving drug information
sheets (arm 2), those who recalled receipt had
the greatest improvement in follow-up test
scores (4.53 to 6.16, p<0.001) but follow-up test
scores were significantly higher (p<0.001) in
both intervention group (arm 2) and usual care
group (arm 1).
Follow-up times: 2 MO
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
203
Evidence Table 1: Diabetes (con't)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
First Author
Year
(ID)
Laitinen JH/Ahola
IE/Sarkkinen
ES/Winberg RL, 1993 RCT
(#2176)
Jadad Score: 1
Diagnostic criteria:
FBS and WHO
Comorbidities:
Heart disease,
hypertension,
obesity, CHF, and
stroke
Intervention
Arm Sample Size
1 Control (n/a)
Counseling/therapy (Office visit)
Education (Office visit)
n Entered:
46
n Analyzed: 38
2
Goal setting (Group meeting)
n Entered:
40
n Analyzed: 38
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Yes
Yes
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Fasting blood glucose (mmol/L) at 3 months:
Arm 1 = 7.5 (2.9)
Arm 2 = 6.6 (1.9)
Glycated hemoglobin A (%) at 3 months:
Arm 1 = 7.8 (2.0)
Arm 2 = 7.1 (1.8)
Weight (kg) at 3 months:
Arm 1 = 88.8 (14.0)
Arm 2 = 88.3 (14.1)
Follow-up times: 3 MO, 15 MO
204
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Litzelman D K, 1993
(#828)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
RCT
n Entered: 205
n Analyzed: n/a
Jadad Score: 2
Diagnostic criteria:
FBS, HgbA1C, and
NDDG
Comorbidities:
n/a
2
Counseling/therapy (Office visit)
Dietary monitoring (Group meeting)
Dietary monitoring (Self-delivery)
Education (Group meeting)
Education (Office visit)
Clinical reviews w/patient (Other
mechanisms)
Contracts (Reading material)
Education (Reading material)
Education (Video/audio tapes)
Practice methods (Other mechanisms)
Reminders (Mail)
Reminders (Other mechanisms)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Yes
No
Yes
No
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Foot care education, behavioral contracts, and
reinforcement (arm 2) resulted in 0.41 times
fewer serious foot lesions and more appropriate
foot care behavior (p=0.0001). Intervention
subjects (arm 2) were also more likely to have
foot examinations than were those in the usual
care group (arm 1) (68% vs. 28%, p<0.001).
Follow-up times: 12 MO
n Entered: 191
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
205
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
McCulloch DK, 1983
(#2264)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type I)
RCT
Jadad Score: 2
Intervention
Arm Sample Size
1 Control (n/a)
Education (One-on-one)
Education (Reading material)
Education (n/a)
Feedback (n/a)
Diagnostic criteria:
HgbA1C
Comorbidities:
Obesity
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
HbA1 (%) at 6 months:
Arm 1 = 11.6 (0.9)
Arm 2 = 10.6 (2.1)
Arm 3 = 9.6 (2.3)
n Entered:
15
n Analyzed: 13
2
Education (One-on-one)
Education (Reading material)
Education (n/a)
Feedback (Group meeting)
Feedback (n/a)
Practice self care skills (Group meeting)
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
BMI (kg/m2) at 6 months:
Arm 1 = 23.9 (2.3)
Arm 2 = 23.7 (1.7)
Arm 3 = 23.8 (2.0)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
No
Follow-up times: 6 MO, 9 MO
n Entered:
14
n Analyzed: 13
3
Education (One-on-one)
Education (Reading material)
Education (Video/audio tapes)
Education (n/a)
Feedback (n/a)
n Entered:
15
n Analyzed: 13
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
206
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Mulrow C, 1987
(#2266)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
RCT
Intervention
Arm Sample Size
1 Education (Group meeting)
Education (Reading material)
Education (Video/audio tapes)
Feedback (Group meeting)
Jadad Score: 2
Yes
Yes
Yes
No
n/a
n Entered:
40
n Analyzed: 34
Diagnostic criteria:
MD
Comorbidities:
Obesity
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
2
3
Education (Group meeting)
Tailored:
Feedback (Group meeting)
Group Setting:
Unstructured group time (Group meeting) Feedback:
Psychological:
n Entered:
40
Primary MD:
n Analyzed: 35
Yes
Yes
Yes
No
n/a
Education (Group meeting)
No
Yes
No
No
n/a
n Entered:
40
n Analyzed: 35
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Patient education utilizing videotapes (arm 1)
had significant weight loss at 7 months
compared to education without videotapes
(arms 2 and 3), but changes were not sustained
at 11 months. There were no significant
changes in HbA1c.
Follow-up times: 7 MO, 11 MO
207
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Pratt C, 1987
(#2139)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
RCT
n Entered:
28
n Analyzed: n/a
Jadad Score: 1
Diagnostic criteria:
n/a
2
Comorbidities:
n/a
Education (Group meeting)
Education (Reading material)
n Entered:
19
n Analyzed: n/a
3
Cognitive-behavioral (Group meeting)
Education (Group meeting)
Education (Reading material)
Feedback (Group meeting)
Goal setting (Group meeting)
Social support (Group meeting)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Follow-up time not in 3 - 12 months.
No differences in weight or glycosylated
hemoglobin were noted between intervention
groups (arms 2 and 3) and usual care group
(arm 1) at 8- or 16-week follow-up.
Follow-up times: 8 WK
n Entered:
32
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
208
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Rabkin SW, 1983
(#2195)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
RCT
Intervention
Arm Sample Size
1 Counseling/therapy (One-on-one)
Dietary monitoring (One-on-one)
Education (One-on-one)
Education (Reading material)
Jadad Score: 2
2
Comorbidities:
Neuropathy and
cholesterol and
retinopathy
Diabetes (Type II)
1
Jadad Score: 2
Comorbidities:
Hypertension and
obesity
Cognitive-behavioral (Group meeting)
Dietary monitoring (Group meeting)
Education (Group meeting)
n Entered:
20
n Analyzed: 20
RCT
Diagnostic criteria:
MD
Yes
No
No
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
n Entered:
20
n Analyzed: 18
Diagnostic criteria:
n/a
Rainwater N, 1982
(#2140)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Counseling/therapy (Office visit)
Education (Hospitalization)
Feedback (Office visit)
n Entered:
11
n Analyzed: 10
2
Cognitive-behavioral (Group meeting)
Counseling/therapy (Office visit)
Education (Group meeting)
Feedback (Office visit)
n Entered:
12
n Analyzed: 10
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Patients attending a behavior modification group
(arm 2) had greater weight loss than those in
individual counseling (arm 1) at 12 weeks
follow-up (p<0.05) but had higher triglyceride
levels (p<0.10). Fasting serum glucose was not
appreciably different between groups.
Follow-up times: 6 WK, 12 WK
Excluded from meta-analysis as no usual care
or comparable control group.
Self-management participants (arm 2) had
continued weight loss at 2, 3 and 6-month
follow-up, compared to those receiving
conventional treatment (arm 1), who, on
average, gained weight. Fasting blood glucose
significantly decreased for both groups over
time but was not significantly different between
groups. Systolic and diastolic blood pressures
increased in both groups over time but less so
for self-management subjects. Satisfaction
measures showed no differences.
Follow-up times: 1 MO, 2 MO, 3 MO, 6 MO
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
209
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Raz I, 1988
(#2141)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
RCT
n Entered:
26
n Analyzed: 23
Jadad Score: 2
Diagnostic criteria:
FBS, HgbA1C, and
PPBS
2
Education (Group meeting)
n Entered:
25
n Analyzed: 23
Comorbidities:
n/a
Rettig BA, 1986
(#2270)
Diabetes
(Types I and II)
1
Usual Care (n/a)
n Entered: 243
n Analyzed: 193
RCT
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Jadad Score: 2
2
Diagnostic criteria:
n/a
Comorbidities:
n/a
Education (Group meeting)
Education (Home visit)
n Entered: 228
n Analyzed: 180
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Fasting glucose (mg/dl) at 12 months:
Arm 1 = 201.0 (45.9)
Arm 2 = 157.5 (59.9)
HbA1c (%) at 12 months:
Arm 1 = 9.6 (4.6)
Arm 2 = 8.0 (5.3)
Weight (kg) at 12 months:
Arm 1 = 73.4 (25.0)
Arm 2 = 73.4 (22.1)
Follow-up times: 4 MO, 8 MO, 12 MO
Excluded from meta-analysis as no relevant
outcome.
Intervention subjects (arm 2) had no significant
differences compared to usual care group (arm
1) with respect to diabetes-related
hospitalizations over a 12-month period.
Similarly, length of hospitalization, emergency
room visits, and physician visits were no
different between groups despite significant
gains for intervention subjects in self-care
knowledge and skills in individual subject areas
as well as in aggregate (p<0.001).
Follow-up times: 6 MO, 1 YR
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
210
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Sadur C N, 1999
(#1668)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes
(Types I and II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
88
n Analyzed: 74
CCT
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Jadad Score: 0
2
Diagnostic criteria:
HgbA1C and
Registry
Comorbidities:
n/a
Clinical reviews w/patient (Telephone)
Cognitive-behavioral (One-on-one)
Consultation w/specialists (Group
meeting)
Counseling/therapy (One-on-one)
Education (Group meeting)
Referrals (Group meeting)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as not
randomized.
At 6 months, HbA1c levels decreased 1.3% for
intervention subjects (arm 2) as compared to
0.22% for usual care group (arm 1). Intervention
levels persisted at 12 months but control levels
had fallen to similar levels by then as well. Selfcare practices, self-efficacy, and satisfaction
with diabetes care were also greater for
intervention subjects compared with usual care
group.
Follow-up times: 6 MO, 18 MO
n Entered:
97
n Analyzed: 82
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
211
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Stevens J, 1985
(#2208)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Control (n/a)
Counseling/therapy (n/a)
RCT
n Entered: n/a
n Analyzed: 12
Jadad Score: 1
Diagnostic criteria:
FBS
2
Counseling/therapy (n/a)
n Entered: n/a
n Analyzed: 15
Comorbidities:
Obesity
3
Counseling/therapy (n/a)
n Entered: n/a
n Analyzed: 12
4
Counseling/therapy (n/a)
n Entered: n/a
n Analyzed: 13
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Yes
No
No
Yes
n/a
Yes
No
No
Yes
n/a
Yes
No
No
Yes
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Patients in all groups were consulted by a
nutritionist. Three intervention groups (arms 2,
3, and 4) received dietary plans that differed in
recommendations for fiber and oat bran intake.
These groups demonstrated decreased body
weight at 6-week follow-up for the oat bran
group (arm 4) compared to controls (arm 1)
(p<0.05). Glycosylated hemoglobin decreased
in all 3 dietary groups but only in the increased
fiber group (arm 3) was this difference
statistically significant compared with controls
(p<0.05).
Follow-up times: 2 WK, 6 WK
212
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Vanninen E, 1992
(#2174)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Control (n/a)
Education (n/a)
n Entered:
40
n Analyzed: 38
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Education (Office visit)
Education (One-on-one)
Education (Reading material)
Exercise program (Self-delivery)
Feedback (One-on-one)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
RCT
Jadad Score: 2
Diagnostic criteria:
FBS
2
Comorbidities:
Heart disease,
hypertension,
obesity, tobacco
abuse, and
cholesterol
Vinicor F, 1987
(#892)
Diabetes
(Types I and II)
n/a
n/a
n/a
n/a
n/a
Yes
No
Yes
No
Yes
Usual Care (n/a)
n Entered: 129
n Analyzed: 68
RCT
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
No
Jadad Score: 2
2
Diagnostic criteria:
FBS and PPBS
Comorbidities:
Heart disease,
hypertension, kidney
disease, neuropathy,
obesity, CHF, and
Contracts (One-on-one)
Education (Computer program)
Education (Home visit)
Education (One-on-one)
Reminders (Telephone)
Fasting blood glucose (mmol/L) at 12 months:
Arm 1 = 7.3 (2.1)
Arm 2 = 6.3 (1.8)
HbA (%) at 12 months:
Arm 1 = 7.3 (1.6)
Arm 2 = 6.6 (1.6)
Follow-up times: 12 MO
n Entered:
38
n Analyzed: 38
1
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
BMI (kg/m2) at 12 months:
Arm 1 = 32.1 (4.5)
Arm 2 = 31.4 (5.1)
Follow-up time not in 3 - 12 months.
Significant improvements for patients receiving
education (arm 2) were noted in HbA1c, fasting
plasma glucose, weight and blood pressure, but
greatest improvements were noted in the group
receiving both patient and physician education
(arm 4).
Follow-up times: 26 MO
n Entered: 117
n Analyzed: 69
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
213
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Condition (Type)
Study Design
Quality
Population
Characteristics
cholesterol
Intervention
Arm Sample Size
3 Consultation w/specialists (Telephone)
Education (Detailed reading material)
Education (Group meeting)
Education (Protocols)
Feedback (Group meeting)
Practice methods (Group meeting)
Reminders (Computer program)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Yes
Yes
Yes
No
Yes
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
No
Yes
n Entered: 130
n Analyzed: 62
4
Consultation w/specialists (Telephone)
Contracts (One-on-one)
Education (Computer program)
Education (Detailed reading material)
Education (Group meeting)
Education (Home visit)
Education (One-on-one)
Education (Protocols)
Feedback (Group meeting)
Practice methods (Group meeting)
Reminders (Computer program)
Reminders (Telephone)
n Entered: 133
n Analyzed: 58
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
214
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Ward WK, 1985
(#2152)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes
(Types I and II)
Intervention
Arm Sample Size
1 Control (n/a)
Education (Group meeting)
Education (Reading material)
RCT
n Entered:
14
n Analyzed: 14
Jadad Score: 1
Diagnostic criteria:
FBS
2
Comorbidities:
n/a
Weinberger M, 1995
(#896)
Diabetes (Type II)
Education (Group meeting)
Education (Reading material)
Feedback (Group meeting)
n Entered:
16
n Analyzed: 16
1
RCT
Usual Care (n/a)
n Entered:
71
n Analyzed: 188
Jadad Score: 2
Diagnostic criteria:
n/a
Comorbidities:
n/a
2
Clinical reviews w/patient (Telephone)
Education (Telephone)
Feedback (Telephone)
Practice methods (Detailed reading
material)
Practice methods (Telephone)
Referrals (Telephone)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Thirty minutes of professional instruction for
self-monitoring blood glucose with Chem-strip
bG (arm 2) compared with reading package
instructions and practice (arm 1) resulted only in
a lower percent error in blood glucose
estimation (p<0.02).
Follow-up times: n/a
Fasting blood glucose (mg/dl) at 12 months:
Arm 1 = 193.1 (57.9)
Arm 2 = 174.1 (59.0)
Glycohemoglobin (%) at 12 months:
Arm 1 = 11.1 (2.4)
Arm 2 = 10.5 (2.7)
Follow-up times: 1 YR
n Entered: 204
n Analyzed: 188
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
215
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Werdier JD, 1984
(#2401)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
CCT
n Entered: n/a
n Analyzed: 82
Jadad Score: 0
Diagnostic criteria:
n/a
White N, 1986
(#2154)
Comorbidities:
n/a
Diabetes (Type II)
2
n Entered: n/a
n Analyzed: 81
1
RCT
Jadad Score: 2
Diagnostic criteria:
FBS and PPBS
Comorbidities:
Obesity
Counseling/therapy (One-on-one)
Control (n/a)
Counseling/therapy (One-on-one)
Education (Group meeting)
n Entered:
21
n Analyzed: 16
2
Emotional support (Group meeting)
Feedback (Group meeting)
n Entered:
20
n Analyzed: 16
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
Yes
n/a
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as not
randomized.
Subjects receiving diabetes counseling (arm 2)
had significant reductions in post-prandial blood
glucose compared with usual care group (arm
1) (p=0.009) at 6-month evaluation.
Follow-up times: 6 MO
Glycohemoglobin (%) at 6 months:
Arm 1 = 10.1 (3.0)
Arm 2 = 9.2 (2.0)
Overweight (%) at 6 months:
Arm 1 = 45.0 (16.0)
Arm 2 = 34.0 (28.0)
Serum glucose (mg/dl) at 6 months:
Arm 1 = 243.0 (120.0)
Arm 2 = 161.0 (48.0)
Follow-up times: 3 MO, 6 MO
216
Evidence Table 1: Diabetes (con't)
Condition (Type)
Study Design
First Author
Quality
Year
Population
(ID)
Characteristics
Wing RR/Epstein LH, Diabetes (Type II)
1985
(#2156)
RCT
Intervention
Arm Sample Size
1 Contracts (Group meeting)
Education (Group meeting)
Financial incentives (Group meeting)
Jadad Score: 1
n Entered: n/a
n Analyzed: n/a
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
Yes
No
n/a
Diagnostic criteria:
FBS and GTT
2
Comorbidities:
Hypertension and
obesity
Cognitive-behavioral (Group meeting)
Contracts (Group meeting)
Dietary monitoring (Group meeting)
Education (Group meeting)
Exercise program (Group meeting)
Financial incentives (Group meeting)
Group Competition (Other mechanisms)
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Patients randomized to a behavior modification
group (arm 2) lost more weight than nutrition
education (arm 3) or standard care (arm 1)
groups during a 4-month treatment period
(p<0.01). However, 16 months later, differences
in weight loss across these 3 groups were not
significant.
Follow-up times: 4 MO, 10 MO, 16 MO
n Entered: n/a
n Analyzed: n/a
3
Contracts (Group meeting)
Education (Group meeting)
Education (Reading material)
Financial incentives (Group meeting)
n Entered: n/a
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
217
Evidence Table 1: Diabetes (con't)
Condition (Type)
Study Design
First Author
Quality
Year
Population
(ID)
Characteristics
Wing RR/Epstein LH, Diabetes (Type II)
1986
(#2158)
RCT
Intervention
Arm Sample Size
1 Cognitive-behavioral (Group meeting)
Dietary monitoring (Group meeting)
Financial incentives (Group meeting)
Jadad Score: 2
Diagnostic criteria:
MD
Comorbidities:
Obesity
n Entered:
25
n Analyzed: 22
2
Cognitive-behavioral (Group meeting)
Dietary monitoring (Group meeting)
Education (Group meeting)
Financial incentives (Group meeting)
n Entered:
25
n Analyzed: 23
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Two groups of randomized patients: a standard
behavioral weight control program (arm 1) and a
weight control program that included selfmonitoring of blood glucose and instruction in
the relationship between weight and glucose
levels (arm 2), both demonstrated significant
weight loss (mean of 6.3 +/- 4.0 kg) at 12 weeks
but with no difference between groups.
Significance was not maintained at one year.
Nor were there any differences between groups
for glycosylated hemoglobin, fasting blood
glucose, total cholesterol, blood pressure,
medication use, or depression scores.
Follow-up times: 12 WK, 62 WK
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
218
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Wing RR, 1988
(#2283)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type II)
RCT
Jadad Score: 2
Diagnostic criteria:
NDDG
Intervention
Arm Sample Size
1 Control (n/a)
Dietary monitoring (Group meeting)
Education (Group meeting)
Financial incentives (Group meeting)
Follow up (Group meeting)
Goal setting (Group meeting)
Material incentive (Group meeting)
Practice self care skills (Group meeting)
Comorbidities:
Obesity
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
n Entered:
10
n Analyzed:
9
2
Cognitive-behavioral (Group meeting)
Contracts (Group meeting)
Dietary monitoring (Group meeting)
Education (Group meeting)
Feedback (Group meeting)
Financial incentives (Group meeting)
Follow up (Group meeting)
Goal setting (n/a)
Material incentive (Group meeting)
Practice self care skills (Group meeting)
Reminders (Group meeting)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
After a 16-week treatment program, both selfregulation group (arm 2) and monitoring only
group (arm 1) significantly improved in
biochemical and weight measures but with no
differences between arms. Though weight loss
was significant for both arms at one-year followup, lack of difference between arms remained.
HgbA1c values were unchanged in both arms
compared to pretreatment values.
Follow-up times: 16 WK, 1 YR
n Entered:
10
n Analyzed:
8
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
219
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Wise PH, 1986
(#2205)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes
(Types I and II)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered: n/a
n Analyzed: 41
CCT
Jadad Score: 1
2
Diagnostic criteria:
n/a
Comorbidities:
n/a
Education (Computer program)
n Entered: n/a
n Analyzed: 46
3
Education (Computer program)
Feedback (Computer program)
n Entered: n/a
n Analyzed: 46
4
Education (Computer program)
Education (Self-delivery)
Feedback (Computer program)
n Entered: n/a
n Analyzed: 41
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Yes
No
No
No
n/a
Yes
No
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as not
randomized.
Significant decreases in HbA1c levels were
seen for individuals participating in computerbased interactive teaching programs with
feedback (arm 2) compared with usual care
group (arm 1) (p<0.05). Knowledge increased in
these groups as well.
Follow-up times: 5 MO
220
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Wood ER, 1989
(#2159)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (n/a)
Intervention
Arm Sample Size
1 Control (n/a)
Education (Hospitalization)
CCT
n Entered: n/a
n Analyzed: 40
Jadad Score: 1
Diagnostic criteria:
MD
Comorbidities:
n/a
2
Education (Group meeting)
Education (Hospitalization)
Feedback (Group meeting)
Practice self care skills (Group meeting)
n Entered: n/a
n Analyzed: 53
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Yes
Yes
Yes
No
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as not
randomized.
Hospitalized patients receiving a comprehensive
inpatient diabetes education program (arm 2)
had better compliance compared with control
group (arm 1) at 4-month follow-up with regard
to self-care behaviors including exercise, insulin
administration and diet, however only exercise
reached statistical significance (p=0.05). Blood
glucose was also lower (p=0.10) as was the
number of emergency room visits (20 for
controls versus 2 in experimental program,
p=0.005).
Follow-up times: 1 MO, 4 MO
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
221
Evidence Table 1: Diabetes (con't)
First Author
Year
(ID)
Worth R, 1982
(#2198)
Condition (Type)
Study Design
Quality
Population
Characteristics
Diabetes (Type I)
RCT
Intervention
Arm Sample Size
1 Clinical reviews w/patient (Office visit)
Education (Office visit)
Self monitoring (Self-delivery)
Jadad Score: 2
Diagnostic criteria:
Insulin by regular
urine test
n Entered:
13
n Analyzed: n/a
2
Comorbidities:
n/a
Clinical reviews w/patient (Office visit)
Education (Office visit)
Self monitoring (Self-delivery)
n Entered:
13
n Analyzed: n/a
3
Clinical reviews w/patient (Office visit)
Education (Office visit)
Self monitoring (Self-delivery)
n Entered:
12
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
The method of monitoring diabetic control had
no effect on glycosylated hemoglobin,
postprandial blood glucose, serum cholesterol,
or body weight.
Follow-up times: 3 MO
222
Evidence Table 2: Osteoarthritis
First Author
Year
(ID)
Barlow JH, 2000
(#3274)
Condition (Type)
Study Design
Quality
Population
Characteristics
Osteoarthritis
(OA and RA)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered: 258
n Analyzed: 311
RCT
Jadad Score: 2
Diagnostic criteria:
MD
Comorbidities:
n/a
2
Cognitive-behavioral (Group meeting)
Education (Group meeting)
Education (Instructional manuals)
Follow up (Group meeting)
Goal setting (Group meeting)
Practice self care skills (Group meeting)
n Entered: 344
n Analyzed: 311
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
223
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Yes
Yes
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Functioning (modified Health Assessment
Questionnaire (0-3)) at 4 months:
Arm 1 = 1.4 (1.0)
Arm 2 = 1.4 (1.0)
Pain (VAS (0-10)) at 4 months:
Arm 1 = 6.4 (2.5)
Arm 2 = 6.4 (2.5)
Follow-up times: 4 MO, 12 MO
Evidence Table 2: Osteoarthritis (con't)
First Author
Year
(ID)
Cohen J L, 1986
(#770)
Condition (Type)
Study Design
Quality
Population
Characteristics
Osteoarthritis
(OA, RA and other,
NOS)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
36
n Analyzed: 34
RCT
Jadad Score: 2
2
Diagnostic criteria:
MD
Comorbidities:
n/a
Advocacy training (Group meeting)
Arthritis self-management (Group
meeting)
Arthritis self-management (Instructional
manuals)
Arthritis self-management (Office visit)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Clinical reviews w/patient (Group meeting) Tailored:
Group Setting:
n Entered: n/a
Feedback:
n Analyzed: n/a
Psychological:
Primary MD:
No
Yes
Yes
No
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Though knowledge of arthritis and use of
exercise increased for both intervention groups
compared with no intervention, delivery by
professional compared with layperson resulted
in no differences with respect to pain,
depression, physical function, social support or
non-exercise behaviors.
Follow-up times: 6 WK, 14 WK
n Entered:
32
n Analyzed: 28
3
Education (Group meeting)
Education (Instructional manuals)
n Entered:
28
n Analyzed: 24
Doyle TH, 1982
(#2427)
Osteoarthritis (OA only)
1
RCT
Clinical reviews w/patient (One-on-one)
n Entered: n/a
n Analyzed: n/a
Jadad Score: 1
Diagnostic criteria:
n/a
Comorbidities:
n/a
2
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Excluded from meta-analysis as no usual care
or comparable control group.
After 20 weeks of treatment, improvement was
seen for pain and range of motion in both arms
with no difference seen between groups.
Follow-up times: 20 WK
224
Evidence Table 2: Osteoarthritis (con't)
First Author
Year
(ID)
Goeppinger J, 1989
(#801)
Condition (Type)
Study Design
Quality
Population
Characteristics
Osteoarthritis
(OA and RA)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered: n/a
n Analyzed: 121
RCT
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Functioning (Health Assessment Questionnaire
disability score (0-3)) at 4 months:
Arm 1 = 1.0 (0.6)
Arm 2 = 1.0 (0.6)
Arm 3 = 1.1 (0.6)
Jadad Score: 1
2
Diagnostic criteria:
n/a
Contracts (Group meeting)
Education (Group meeting)
n Entered: n/a
n Analyzed: 121
Comorbidities:
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
n/a
Pain (Pain Index) at 4 months:
Arm 1 = 25.7 (8.7)
Arm 2 = 25.4 (8.7)
Arm 3 = 26.6 (8.7)
Follow-up times: 4 MO
3
Contracts (Group meeting)
Education (Group meeting)
Education (Reading material)
Education (Video/audio tapes)
n Entered: n/a
n Analyzed: 121
Keefe F, 1996
(#2082)
Osteoarthritis (OA only)
1
Cognitive-behavioral (Group meeting)
Education (Reading material)
RCT
n Entered: n/a
n Analyzed: n/a
Jadad Score: 1
Diagnostic criteria:
n/a
Comorbidities:
n/a
2
Cognitive-behavioral (Group meeting)
Counseling/therapy (Group meeting)
Education (Reading material)
n Entered: n/a
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Excluded from meta-analysis as no usual care
or comparable control group.
Patients receiving spouse-assisted coping skills
training (arm 2) had lower levels of pain and
psychological disability and higher self-efficacy
and more frequent use of pain-coping strategies
after 10 weeks of treatment than did those
receiving the cognitive-behavioral intervention
(arm 1). Subjects in the pain-coping skills
training without spouse assistance (arm 3) had
higher self-efficacy, coping, and marital
adjustment and lower pain and psychological
225
Evidence Table 2: Osteoarthritis (con't)
First Author
Year
(ID)
Condition (Type)
Study Design
Quality
Population
Characteristics
Intervention
Arm Sample Size
3 Education (Group meeting)
Education (Reading material)
n Entered: n/a
n Analyzed: n/a
Keefe F J, 1990a
(#907)
Osteoarthritis (OA only)
1
RCT
Usual Care (n/a)
n Entered:
31
n Analyzed: 35
Jadad Score: 1
Diagnostic criteria:
X-ray and MD
2
Comorbidities:
Obesity
Cognitive-behavioral (Group meeting)
Cognitive-behavioral (Video/audio tapes)
Consultation w/specialists (Group
meeting)
Counseling/therapy (Telephone)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
disability as compared to the cognitivebehavioral group.
Follow-up times: 10 WK
Functioning (AIMS physical disability scale) at 6
months:
Arm 1 = 2.0 (1.3)
Arm 2 = 2.1 (1.3)
Arm 3 = 2.3 (1.3)
Pain (AIMS pain scale) at 6 months:
Arm 1 = 5.7 (1.6)
Arm 2 = 5.7 (1.7)
Arm 3 = 4.6 (1.7)
Follow-up times: 6 MO, 12 MO
n Entered:
32
n Analyzed: 35
3
Counseling/therapy (Telephone)
Education (Group meeting)
n Entered:
36
n Analyzed: 35
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
Yes
No
226
Evidence Table 2: Osteoarthritis (con't)
First Author
Year
(ID)
Keefe F J, 1990b
(#908)
Condition (Type)
Study Design
Quality
Intervention
Population
Characteristics
Arm Sample Size
Osteoarthritis (OA only)
1 Usual Care (n/a)
RCT
n Entered:
31
n Analyzed: 28
Jadad Score: 1
Diagnostic criteria:
X-ray and MD
2
Comorbidities:
Obesity
Cognitive-behavioral (Group meeting)
Cognitive-behavioral (Video/audio tapes)
Consultation w/specialists (Group
meeting)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
No
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Duplicate population Keefe F J, 1990b
Patients who received pain coping skills training
(arm 2) had significantly lower levels of pain
(p<0.01) and psychological disability (p<0.001)
than those who received arthritis education (arm
3) or usual care (arm 1). Physical disability was
no different between groups after treatment.
Follow-up times: 10 WK
n Entered:
32
n Analyzed: 31
3
Education (Group meeting)
n Entered:
36
n Analyzed: 35
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
227
Evidence Table 2: Osteoarthritis (con't)
First Author
Year
(ID)
Laborde JM, 1983
(#2355)
Condition (Type)
Study Design
Quality
Intervention
Population
Characteristics
Arm Sample Size
Osteoarthritis (OA only)
1 Usual Care (n/a)
RCT
n Entered:
20
n Analyzed: 20
Jadad Score: 1
Diagnostic criteria:
Chart review and
self report
2
Education (Reading material)
n Entered:
35
n Analyzed: 35
Comorbidities:
n/a
3
Education (Group meeting)
Education (Reading material)
n Entered:
35
n Analyzed: 35
4
Education (Group meeting)
Education (Reading material)
n Entered:
35
n Analyzed: 35
5
Education (Group meeting)
Education (Reading material)
n Entered:
35
n Analyzed: 35
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
No
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Subjects receiving relaxation procedures (arm
4) had significantly less pain than those
receiving other interventions or those in the
control group (p<0.05). No differences were
noted with respect to stiffness, mobility,
medication taking behavior, or knowledge.
Follow-up times: 2 WK
228
Evidence Table 2: Osteoarthritis (con't)
First Author
Year
(ID)
Lorig K, 1985
(#835)
Condition (Type)
Study Design
Quality
Population
Characteristics
Osteoarthritis
(OA and RA)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
65
n Analyzed: 129
RCT
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Jadad Score: 1
2
Diagnostic criteria:
MD
Lorig K, 1986
(#830)
Comorbidities:
n/a
Osteoarthritis (OA and
RA)
n Entered: 134
n Analyzed: 129
1
2
Diagnostic criteria:
MD
Comorbidities:
n/a
Usual Care (n/a)
n Entered:
32
n Analyzed: 29
RCT
Jadad Score: 2
Arthritis self-management (Group
meeting)
Arthritis self-management (Group
meeting)
n Entered:
34
n Analyzed: 29
3
Arthritis self-management (Group
meeting)
n Entered:
34
n Analyzed: 29
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Functioning (Disability (0-3)) at 4 months:
Arm 1 = 0.5 (1.0)
Arm 2 = 0.6 (1.0)
Pain (VAS (0-10)) at 4 months:
Arm 1 = 3.2 (2.5)
Arm 2 = 3.4 (2.5)
Follow-up times: 4 MO
Functioning (Health Assessment Questionnaire
(0-3)) at 4 months:
Arm 1 = 0.9 (1.0)
Arm 2 = 0.8 (1.0)
Arm 3 = 0.7 (1.0)
Pain (Double anchored VAS (0-15)) at 4
months:
Arm 1 = 7.3 (3.8)
Arm 2 = 8.9 (3.8)
Arm 3 = 7.4 (3.8)
Follow-up times: 4 MO
229
Evidence Table 2: Osteoarthritis (con't)
First Author
Year
(ID)
Lorig K, 1989
(#837)
Condition (Type)
Study Design
Quality
Population
Characteristics
Osteoarthritis
(OA and RA)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered: n/a
n Analyzed: 501
RCT
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Jadad Score: 1
Diagnostic criteria:
MD
Lorig K R, 1999
(#608)
Comorbidities:
n/a
Osteoarthritis
(Arthritis, NOS)
2
Arthritis self-management (Group
meeting)
n Entered: n/a
n Analyzed: 501
1
Usual Care (n/a)
n Entered: 476
n Analyzed: 561
RCT
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Functioning (Stanford Health Assessment
Questionnaire (0-3)) at 4 months:
Arm 1 = 0.7 (1.0)
Arm 2 = 0.7 (1.0)
Pain (Double anchored VAS (0-10)) at 4
months:
Arm 1 = 4.5 (2.5)
Arm 2 = 4.2 (2.5)
Follow-up times: 4 MO
Functioning (modified Health Assessment
Questionnaire disability score (0-3)) at 6
months:
Arm 1 = 0.9 (1.0)
Arm 2 = 0.8 (1.0)
Jadad Score: 2
2
Diagnostic criteria:
MD
Comorbidities:
Heart disease,
chronic respiratory
disease, CHF, and
stroke
Cognitive-behavioral (Group meeting)
Education (Group meeting)
Feedback (Group meeting)
Practice methods (Group meeting)
n Entered: 664
n Analyzed: 561
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Pain (adaptation of Medical Outcomes Study
pain scale (0-100)) at 6 months:
Arm 1 = 56.8 (25.0)
Arm 2 = 55.4 (25.0)
Follow-up times: 6 MO
230
Evidence Table 2: Osteoarthritis (con't)
First Author
Year
(ID)
Weinberger M, 1989
(#430)
Condition (Type)
Study Design
Quality
Intervention
Population
Characteristics
Arm Sample Size
Osteoarthritis (OA only)
1 Usual Care (n/a)
RCT
n Entered: 112
n Analyzed: 103
Jadad Score: 2
Diagnostic criteria:
X-ray and MD
2
Comorbidities:
n/a
Advocacy training (Telephone)
Clinical reviews w/patient (Telephone)
Reminders (Telephone)
4
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
n Entered: 109
n Analyzed: 99
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
Advocacy training (Office visit)
Advocacy training (Telephone)
Clinical reviews w/patient (Office visit)
Clinical reviews w/patient (Telephone)
Reminders (Telephone)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
n Entered: 109
n Analyzed: 95
3
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Advocacy training (Office visit)
Clinical reviews w/patient (Office visit)
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Education delivered by telephone (arms 2 and
4) compared with no telephone (arms 1 and 3)
resulted in improved physical health and
reduced pain (p=0.02) with trends suggesting
improved psychological health (p=0.10).
Follow-up times: 11 MO
n Entered: 109
n Analyzed: 97
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
231
Evidence Table 3: Post-Myocardial Infarction Care
First Author
Year
(ID)
Burgess AW, 1987
(#2652)
Condition (Type)
Study Design
Quality
Intervention
Population
Arm Sample Size
Characteristics
Myocardial infarction
1 Usual Care (n/a)
(Uncomplicated and
n Entered:
91
complicated)
n Analyzed: 77
RCT
Jadad Score: 2
2
Diagnostic criteria:
CPK-MB elevation,
ECG, Symptoms
DeBusk F, 1985
(#2669)
Comorbidities:
CHF
Myocardial infarction
(First occurrence
and reoccurrence)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Cognitive-behavioral (One-on-one)
Follow up (Mail)
Social support (One-on-one)
n Entered:
89
n Analyzed: 77
1
Usual Care (n/a)
n Entered:
37
n Analyzed: n/a
RCT
Jadad Score: 2
Diagnostic criteria:
CPK-MB elevation,
ECG, SGOT,
Symptoms
2
Control (n/a)
Counseling/therapy (One-on-one)
Exercise testing (n/a)
n Entered:
34
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
232
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Death at 13 months:
Arm 1 = 5 deaths
Arm 2 = 5 deaths
Return to work (% return to same or new job) at
13 months:
Arm 1 = 88% of 76 eligible subjects
Arm 2 = 88% of 77 eligible subjects
Follow-up times: 3 MO, 13 MO
Excluded from meta-analysis as no relevant
outcome.
The average increase in functional capacity
(i.e., peak treadmill workload on METS)
between 3 and 26 weeks was significantly
greater (p<0.05) in training groups (arms
2,3,4,5, and 6) than in the usual care group
(arm 1) (1.8 vs. 1.2 METs, respectively).
Follow-up times: 3 WK, 11 WK, 26 WK
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Condition (Type)
Study Design
Quality
Population
Characteristics
Comorbidities:
n/a
Intervention
Arm Sample Size
3 Counseling/therapy (One-on-one)
Exercise diary (Self-delivery)
Exercise monitoring (Telephone)
Exercise program (One-on-one)
Exercise program (Reading material)
Exercise testing (n/a)
Follow up (Telephone)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Yes
No
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
n Entered:
33
n Analyzed: n/a
4
Counseling/therapy (One-on-one)
Exercise diary (Self-delivery)
Exercise monitoring (Telephone)
Exercise program (One-on-one)
Exercise program (Reading material)
Exercise testing (n/a)
Follow up (Telephone)
n Entered:
33
n Analyzed: n/a
5
Counseling/therapy (One-on-one)
Exercise monitoring (Group meeting)
Exercise program (Group meeting)
Exercise testing (n/a)
n Entered:
30
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
233
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Condition (Type)
Study Design
Quality
Population
Characteristics
Intervention
Arm Sample Size
6 Counseling/therapy (One-on-one)
Exercise monitoring (Group meeting)
Exercise program (Group meeting)
Exercise testing (n/a)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Yes
Yes
No
Yes
No
n Entered:
31
n Analyzed: n/a
DeBusk RF, 1994
(#775)
Myocardial infarction
(Angina with
infarction)
1
n Entered: 292
n Analyzed: 244
RCT
Jadad Score: 3
Diagnostic criteria:
CPK-MB elevation,
ECG, Chest pain,
SGOT
Comorbidities:
Tobacco abuse,
substance abuse,
and psychiatric
problems
Control (n/a)
Counseling/therapy (Hospitalization)
2
Counseling/therapy (Computer program)
Counseling/therapy (Hospitalization)
Counseling/therapy (Office visit)
Counseling/therapy (Reading material)
Counseling/therapy (Telephone)
Counseling/therapy (Video/audio tapes)
Education (Hospitalization)
Education (Office visit)
Education (Telephone)
Feedback (Mail)
n Entered: 293
n Analyzed: 243
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
n/a
Excluded from meta-analysis as no usual care
or comparable control group.
At 12 months, 4.1% had died in the intervention
arm (arm 2), compared to 3.4% in the control
group (arm 1). LDL and total cholesterol
decreased more in the intervention arm
(p <0.001). Smoking cessation at 12 months
increased significantly for the case management
arm versus usual care (70% vs. 53%, p=0.03).
Functional capacity was higher in the
intervention arm at 6 months 9.3 METS vs. 8.4
METS. The% consuming a low fat diet
increased from 31% to 88% at 90 days in the
intervention arm but was similar to usual care
arm.
Follow-up times: 3 MO, 6 MO, 12 MO
234
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Dennis C, 1988
(#2656)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(Uncomplicated MI)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered: 102
n Analyzed: 99
RCT
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Jadad Score: 3
Diagnostic criteria:
CPK-MB elevation,
ECG, MD
2
Comorbidities:
n/a
Frasure-Smith N,
1985
(#790)
Myocardial infarction
(Uncomplicated,
complicated, first
and reoccurrence,
angina with infarction
and unspecified)
Jadad Score: 0
Diagnostic criteria:
n/a
Comorbidities:
Hypertension,
obesity, DM, CHF,
tobacco abuse, and
angina
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
Yes
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
n/a
Return to work (% working part- or full-time) at 6
months:
Arm 1 = 86% of 102 eligible subjects
Arm 2 = 92% of 99 eligible subjects
Follow-up times: 1 MO, 3 MO, 6 MO
n Entered:
99
n Analyzed: 99
1
Usual Care (n/a)
n Entered: 231
n Analyzed: 224
2
CCT
Clinical reviews w/patient (Telephone)
Consultation w/specialists (Mail)
Consultation w/specialists (Telephone)
Counseling/therapy (One-on-one)
Exercise testing (One-on-one)
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Death at 6 months:
Arm 1 = 2 deaths
Arm 2 = 1 death
Consultation w/specialists (Group
meeting)
Education (Home visit)
Psychological assessment/care (Home
visit)
Psychological assessment/care
(Telephone)
Excluded from meta-analysis as not
randomized.
Nurse-delivered stress monitoring and stress
reduction interventions resulted in lower stress
levels and fewer cardiac deaths (70% decrease)
for intervention patients (arm 2) compared with
usual care group (arm 1) but not reinfarction
rates. Differences between groups with respect
to SES may be responsible for these
differences.
Follow-up times: 1 YR
n Entered: 230
n Analyzed: 229
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
235
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Frasure-Smith N,
1989
(#2218)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(Uncomplicated,
complicated, first
and reoccurrence)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered: 233
n Analyzed: 179
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
CCT
2
Jadad Score: 1
Diagnostic criteria:
MD
Friedman M, 1982
(#2367)
Comorbidities:
Hypertension,
obesity, DM, tobacco
abuse, and
cholesterol
Myocardial infarction
(First occurrence
and reoccurrence)
Consultation w/specialists (Group
meeting)
Education (Home visit)
Psychological assessment/care (Home
visit)
Psychological assessment/care
(Telephone)
Follow-up times: 2 YR, 5 YR, 64 MO
1
Usual Care (n/a)
n Entered: 151
n Analyzed: 125
2
Counseling/therapy (Group meeting)
Jadad Score: 0
Comorbidities:
Heart disease,
hypertension, CHF,
tobacco abuse, and
cholesterol
Yes
Yes
No
Yes
n/a
Subjects receiving home-based nursing
interventions aimed at reducing stress (arm 2)
had significantly fewer MI recurrences than
usual care subjects (arm 1) over a 4-year followup period (p=0.04). The difference in mortality
was maximal at 18 months post-MI, but during
the remaining years mortality between groups
was equivalent. No difference in hospitalization
readmission rates was noted.
n Entered: 232
n Analyzed: 176
CCT
Diagnostic criteria:
CPK-MB elevation,
ECG, Patient History
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as not
randomized.
n Entered: 270
n Analyzed: 213
3
Cognitive-behavioral (Group meeting)
Counseling/therapy (Group meeting)
n Entered: 614
n Analyzed: 514
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Yes
Yes
No
Yes
n/a
Yes
Yes
No
Yes
n/a
Excluded from meta-analysis as not
randomized.
Subjects receiving interventions of both
cardiologic and behavioral counseling (arms 2
and 3) had lower 1-yr rates of reinfarction
(p<0.01) and death (p<0.05) than usual care
subjects (arm 1). Behavioral counseling (arm 3)
resulted in fewer reinfarctions (1.1% versus
3.3% p<0.05) than cardiologic counseling alone
(arm 2).
Follow-up times: 1 YR
236
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Friedman M, 1984
(#2362)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(First occurrence
and reoccurrence)
Intervention
Arm Sample Size
1 Counseling/therapy (Group meeting)
Psychological assessment/care (Group
meeting)
RCT
n Entered: 270
n Analyzed: 164
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
n/a
Jadad Score: 1
2
Diagnostic criteria:
CPK-MB elevation,
ECG, Clinical history
Froelicher E S, 1994
(#792)
Comorbidities:
Heart disease,
hypertension, CHF,
and tobacco abuse
Myocardial infarction
(Uncomplicated MI)
Cognitive-behavioral (Group meeting)
Counseling/therapy (Group meeting)
n Entered: 592
n Analyzed: 381
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
Patients receiving Type A behavioral counseling
(arm 2) had a 7.2% 3-year cumulative cardiac
recurrence rate compared with 13% for
individuals receiving only cardiologic counseling
(arm 1) (p<0.005). Three-year survival without
cardiac recurrence was also higher for the
behavioral counseling group (p<0.01) but no
differences were noted for arrhythmias or
hypertension.
Follow-up times: 3 YR
1
Usual Care (n/a)
n Entered:
84
n Analyzed: 52
RCT
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Jadad Score: 2
2
Diagnostic criteria:
MD
Exercise program (Hospitalization)
Feedback (Office visit)
n Entered:
88
n Analyzed: 52
Comorbidities:
n/a
Death at 24 weeks:
Arm 1 = 2 deaths
Arm 2 = 3 deaths
Arm 3 = 3 deaths
Return to work (% return to same job) at 24
weeks:
Arm 1 = 90% of 62 eligible subjects
Arm 2 = 95% of 63 eligible subjects
Arm 3 = 98% of 52 eligible subjects
Follow-up times: 3 MO, 6 MO
3
Counseling/therapy (Group meeting)
Education (Group meeting)
Exercise program (Hospitalization)
Feedback (Office visit)
n Entered:
86
n Analyzed: 52
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
237
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Gruen W, 1975
(#2360)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(Uncomplicated,
complicated, first
occurrence, and
unspecified)
CCT
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered: n/a
n Analyzed: 37
2
Jadad Score: 0
Diagnostic criteria:
n/a
Heller R F, 1993
(#809)
Comorbidities:
CHF, anxiety and
depression
Myocardial infarction
(Uncomplicated, first
and reoccurrence,
angina with and
without infarction,
and unspecified)
1
Jadad Score: 1
Diagnostic criteria:
n/a
Advocacy training (One-on-one)
Tailored:
Psychological assessment/care (One-on- Group Setting:
one)
Feedback:
Psychological:
n Entered:
38
Primary MD:
n Analyzed: n/a
Usual Care (n/a)
n Entered: 237
n Analyzed: 61
2
RCT
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Contracts (Reading material)
Education (Mail)
Education (Reading material)
Feedback (Reading material)
Reminders (Other mechanisms)
n/a
n/a
n/a
n/a
n/a
Yes
No
No
Yes
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as not
randomized.
Intervention subjects (arm 2) had 2.5 fewer
hospital days (p<0.05), less observed weakness
and depression (p<0.05), decreased anxiety
(p<0.001), and fewer supraventricular
arrhythmias (p<0.05) compared with usual care
patients (arm 1). No differences in chest pain
occurrence were noted.
Follow-up times: 4 MO
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
No
Death at 6 months:
Arm 1 = 3 deaths
Arm 2 = 6 deaths
Return to work (% return to same job) at 6
months:
Arm 1 = 76% of 66 eligible subjects
Arm 2 = 66% of 61 eligible subjects
Follow-up times: 6 MO
n Entered: 213
n Analyzed: 61
Comorbidities:
Heart disease,
hypertension,
obesity, tobacco
abuse, angina, and
cholesterol
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
238
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Horlick L, 1984
(#2219)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(Uncomplicated,
complicated, first
and reoccurrence,
and unspecified)
Intervention
Arm Sample Size
1 Control (n/a)
Education (Video/audio tapes)
n Entered:
33
n Analyzed: 65
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
RCT
2
Jadad Score: 1
Diagnostic criteria:
n/a
Lewin B, 1992
(#827)
Comorbidities:
CHF, anxiety and
depression
Myocardial infarction
(First occurrence
and reoccurrence)
1
Jadad Score: 4
Comorbidities:
Tobacco abuse
Return to work (% working part- or full-time) at
6 months:
Arm 1 = 92.8% of 29 eligible subjects
Arm 2 = 80.6% of 65 eligible subjects
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Insufficient statistics for meta-analysis.
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
Yes
No
Follow-up times: 6 WK, 6 MO, 12 MO
Follow-up times: 3 MO, 6 MO
n Entered:
83
n Analyzed: 65
RCT
Diagnostic criteria:
WHO
Education (Group meeting)
Education (One-on-one)
Education (Video/audio tapes)
Unstructured group time (Group meeting)
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Death at 6 months:
Arm 1 = 1 death
Arm 2 = 6 deaths
Control (n/a)
Counseling/therapy (Home visit)
Counseling/therapy (Office visit)
Counseling/therapy (Telephone)
Education (Reading material)
n Entered:
88
n Analyzed: 60
2
Counseling/therapy (Home visit)
Counseling/therapy (Office visit)
Counseling/therapy (Telephone)
Education (Instructional manuals)
Education (Video/audio tapes)
Anxiety and general emotional disturbance
scores for intervention subjects (arm 2) were
half that of controls (arm 1) at 1-year follow-up.
In the first 6 months of study, 18 control
compared with 6 intervention patients had
hospital admissions (p=0.02).
n Entered:
88
n Analyzed: 50
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
239
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Miller NH, 1984
(#2670)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(First occurrence
and reoccurrence)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
37
n Analyzed: n/a
RCT
Jadad Score: 2
2
Diagnostic criteria:
CPK-MB elevation,
ECG, SGOT,
Symptoms
Comorbidities:
n/a
Control (n/a)
Counseling/therapy (One-on-one)
Exercise testing (n/a)
n Entered:
34
n Analyzed: n/a
3
Counseling/therapy (One-on-one)
Exercise diary (Self-delivery)
Exercise monitoring (Telephone)
Exercise program (One-on-one)
Exercise program (Reading material)
Exercise testing (n/a)
Follow up (Telephone)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no relevant
outcome.
Though functional capacity improved in patients
randomized to either home (arms 3 and 4) or
group (arms 5 and 6) exercise training
compared with controls (arms 1 and 2), no
differences were seen between home and group
training. Frequency of exercise induced angina
or ischemic ST-segment depression was no
different between groups when measured at 26
weeks.
Follow-up times: 3 WK, 11 WK, 26 WK
n Entered:
33
n Analyzed: n/a
4
Counseling/therapy (One-on-one)
Exercise diary (Self-delivery)
Exercise monitoring (Telephone)
Exercise program (One-on-one)
Exercise program (Reading material)
Exercise testing (n/a)
Follow up (Telephone)
n Entered:
33
n Analyzed: n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
240
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Condition (Type)
Study Design
Quality
Population
Characteristics
Intervention
Arm Sample Size
5 Counseling/therapy (One-on-one)
Exercise monitoring (Group meeting)
Exercise program (Group meeting)
Exercise testing (n/a)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Yes
Yes
No
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
n/a
Tailored:
Group Setting:
n Entered:
14
Feedback:
n Analyzed: 14
Psychological:
Primary MD:
Cognitive-behavioral (Video/audio tapes) Tailored:
Education (Video/audio tapes)
Group Setting:
Feedback:
n Entered:
16
Psychological:
n Analyzed: 14
Primary MD:
n/a
n/a
n/a
n/a
n/a
No
No
No
Yes
n/a
Cognitive-behavioral (Video/audio tapes) Tailored:
Counseling/therapy (One-on-one)
Group Setting:
Education (Video/audio tapes)
Feedback:
Psychological:
n Entered:
16
Primary MD:
n Analyzed: 15
Yes
No
No
Yes
n/a
n Entered:
30
n Analyzed: n/a
6
Counseling/therapy (One-on-one)
Exercise monitoring (Group meeting)
Exercise program (Group meeting)
Exercise testing (n/a)
n Entered:
31
n Analyzed: n/a
Oldenburg B, 1985
(#2699)
Myocardial infarction
(First occurrence)
1
CCT
Jadad Score: 1
2
Diagnostic criteria:
MD
Usual Care (n/a)
Comorbidities:
Heart disease
3
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Excluded from meta-analysis as not
randomized.
Both intervention groups (arms 2 and 3) had
improved psychological measures related to
anxiety, distress, and Type A behavior,
compared with the usual care group (arm 1)
(p<0.05). The counseling group (arm 3)
demonstrated sustained significant reductions in
alcohol and tobacco consumption at 12-month
follow-up. A higher proportion of counseling
subjects reported returning to work by 12
months and a trend towards less chest pain and
related hospital admissions was also seen.
Follow-up times: 3 MO, 6 MO, 12 MO
241
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Oldenburg B, 1989
(#2698)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(First occurrence
and reoccurrence
and unspecified)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered: n/a
n Analyzed: n/a
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
No
No
No
No
No
RCT
Jadad Score: 1
2
Education (One-on-one)
Education (Video/audio tapes)
Diagnostic criteria:
n/a
n Entered: n/a
n Analyzed: n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Cognitive-behavioral (Group meeting)
Contracts (Group meeting)
Education (One-on-one)
Education (Video/audio tapes)
Exercise program (Group meeting)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Comorbidities:
Heart disease and
hypertension
3
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Subjects attending a behavioral group (arm 3)
had statistically significantly less anxiety and
depression over 12-month follow-up than the
usual care subjects (arm 1) (p<0.05). Type A
behavior was also reduced to a greater degree
than usual care or education intervention
subjects (p<0.01). Smoking decreased in all
groups but relapse rate for behavioral group
was almost half that of the other 2 groups
(p<0.05). The behavioral group also had fewer
physical symptoms and greater exercise
capacity (p<0.05).
Follow-up times: 4 MO, 8 MO, 12 MO
n Entered: n/a
n Analyzed: n/a
Oldridge N, 1991
(#2653)
Myocardial infarction
(First occurrence
and reoccurrence)
1
Usual Care (n/a)
n Entered: 102
n Analyzed: 54
RCT
Jadad Score: 1
Diagnostic criteria:
CPK-MB elevation,
ECG, Symptoms
2
Cognitive-behavioral (Group meeting)
Education (Group meeting)
Exercise program (Group meeting)
n Entered:
99
n Analyzed: 54
Death at 12 months:
Arm 1 = 4 deaths
Arm 2 = 3 deaths
Return to work (% return to work) at 12 months:
Arm 1 = 83.6% of 61 eligible subjects
Arm 2 = 79.3% of 54 eligible subjects
Follow-up times: 8 WK, 4 MO, 8 MO, 12 MO
Comorbidities:
n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
242
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Ott CR, 1983
(#2657)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(Uncomplicated,
complicated, first
and reoccurrence)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
84
n Analyzed: 59
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
RCT
2
Jadad Score: 1
Diagnostic criteria:
CPK-MB elevation,
ECG, Clinical history
Comorbidities:
Obesity and tobacco
abuse
Education (Hospitalization)
Exercise program (Hospitalization)
Exercise program (Office visit)
Exercise program (Self-delivery)
Feedback (Office visit)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
n Entered:
88
n Analyzed: 68
3
Counseling/therapy (One-on-one)
Education (Group meeting)
Education (Hospitalization)
Education (Reading material)
Education (Self-delivery)
Education (Video/audio tapes)
Exercise program (Hospitalization)
Exercise program (Office visit)
Feedback (Office visit)
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Same study population as Sivarajan, et al.,
1983. Using the Sickness Impact Profile survey
instrument, researchers found improved
physical and psychosocial function for those
receiving an exercise program coupled with
counseling about cardiac risk factors and
emotional adjustment after myocardial infarction
(arm 3). Differences between groups exceeded
any changes noted for those receiving an
exercise-only intervention and were significant
at a .01 to .05 level dependent upon specific
measured categories.
Follow-up times: 3 MO, 6 MO
n Entered:
86
n Analyzed: 62
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
243
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Payne T J, 1994
(#859)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(First occurrence
and reoccurrence)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
26
n Analyzed: 26
CCT
Jadad Score: 1
2
Diagnostic criteria:
MD, Stress test
Powell LH, 1984
(#2361)
Cognitive-behavioral (Group meeting)
Education (Group meeting)
Practice self care skills (Self-delivery)
n Entered:
60
n Analyzed: 26
Comorbidities:
Heart disease and
anxiety and
depression
Myocardial infarction
(First and
reoccurrence, angina
with infarction and
unspecified)
1
RCT
2
Control (n/a)
Counseling/therapy (Group meeting)
n Entered: 270
n Analyzed: 259
Jadad Score: 2
Cognitive-behavioral (Group meeting)
Cognitive-behavioral (Reading material)
Counseling/therapy (Group meeting)
Diagnostic criteria:
n/a
n Entered: 592
n Analyzed: 564
Comorbidities:
Heart disease,
hypertension, and
hypercholeterelemia
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as not
randomized.
Chest pain frequency and depression scores
were significantly lower for intervention subjects
(arm 2) at 1-month follow-up but no differences
between intervention and usual care (arm 1)
subjects were noted at 6-months.
Follow-up times: 1 MO, 6 MO
Excluded from meta-analysis as no usual care
or comparable control group.
Behavioral counseling (arm 2) targeted to “Type
A” life style resulted in greater reductions in
Type A behavior compared with standard
counseling (arm 1). Cardiovascular recurrence
rates were no different between counseling
groups but behavioral counseling subjects had
lower 2-year cardiovascular recurrences than
controls (2.76 versus 6.00
p<0.05) Total cholesterol and blood pressure
were similar between groups.
Follow-up times: 2 YR
244
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Rahe RM, 1979
(#2406)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(First occurrence
and unspecified)
Intervention
Arm Sample Size
1 Control (n/a)
Dietary monitoring (Office visit)
Education (Reading material)
RCT
n Entered:
22
n Analyzed: 17
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Jadad Score: 1
2
Diagnostic criteria:
n/a
Comorbidities:
Heart disease,
hypertension,
obesity, DM, CHF,
and tobacco abuse
Schulte MB, 1986
(#2438)
Myocardial infarction
(First occurrence and
unspecified)
Cognitive-behavioral (Group meeting)
Contracts (Group meeting)
Counseling/therapy (Group meeting)
Dietary monitoring (Office visit)
Education (Group meeting)
Education (Reading material)
Yes
Yes
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
No
n/a
Return to work (% who worked full-time before
MI who returned to work) at 12 months:
Arm 1 = 41.7% of 12 eligible subjects
Arm 2 = 94.1% of 17 eligible subjects
Follow-up times: 18 MO, 42 MO
n Entered:
22
n Analyzed: 17
1
Usual Care (n/a)
n Entered:
16
n Analyzed: 16
CCT
Jadad Score: 0
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Death at 12 months:
Arm 1 = 2 deaths
Arm 2 = 0 deaths
2
Diagnostic criteria:
n/a
Education (Group meeting)
Practice methods (Group meeting)
Practice methods (Video/audio tapes)
Practice self care skills (Group meeting)
Comorbidities:
n/a
n Entered:
29
n Analyzed: 29
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Excluded from meta-analysis as not
randomized.
Intervention subjects (arm 2) demonstrated
decreased anxiety (p<0.05) and increased self
care cardiac skills (p<0.01) compared with usual
care subjects (arm 1).
Follow-up times: 10 WK
245
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Sivarajan ES, 1983
(#2439)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(Uncomplicated,
complicated, first
and reoccurrence)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
84
n Analyzed: 63
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
RCT
2
Jadad Score: 1
Diagnostic criteria:
CPK-MB elevation,
ECG, Clinical history
Comorbidities:
Obesity and tobacco
abuse
Education (Hospitalization)
Exercise program (Hospitalization)
Exercise program (Office visit)
Exercise program (Self-delivery)
Feedback (Office visit)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
No
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Same study population as Ott, et al., 1983.
Though modest changes in diet were noted for
intervention subjects (arms 2 and 3), no
changes occurred between groups with respect
to weight or smoking.
Follow-up times: 3 MO, 6 MO
n Entered:
88
n Analyzed: 68
3
Counseling/therapy (One-on-one)
Education (Group meeting)
Education (Hospitalization)
Education (Reading material)
Education (Self-delivery)
Education (Video/audio tapes)
Exercise program (Hospitalization)
Exercise program (Office visit)
Feedback (Office visit)
n Entered:
86
n Analyzed: 62
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
246
Evidence Table 3: Post-Myocardial Infarction Care (con't)
First Author
Year
(ID)
Stern MJ, 1983
(#2377)
Condition (Type)
Study Design
Quality
Population
Characteristics
Myocardial infarction
(Unspecified)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
29
n Analyzed:
9
RCT
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Jadad Score: 1
2
Diagnostic criteria:
n/a
Comorbidities:
Hypertension and
tobacco abuse
Exercise program (Group meeting)
n Entered:
42
n Analyzed:
9
Myocardial infarction
(Unspecified)
Yes
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
n/a
n/a
n/a
n/a
n/a
1
Counseling/therapy (Group meeting)
Usual Care (n/a)
n Entered:
15
n Analyzed:
6
RCT
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
Yes
Yes
No
Jadad Score: 1
2
Diagnostic criteria:
MD
Comorbidities:
Hypertension,
tobacco abuse, and
CABG and high
cholesterol
Return to work (% who returned who hadn't
returned by baseline) at 12 months:
Arm 1 = 0% of 5 eligible subjects
Arm 2 = 60% of 5 eligible subjects
Arm 3 = 33.3% of 9 eligible subjects
Follow-up times: 3 MO, 6 MO, 1 YR
3
n Entered:
35
n Analyzed:
9
Turner L, 1995
(#887)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Death at 12 months:
Arm 1 = 1 death
Arm 2 = 0 deaths
Arm 3 = 0 deaths
Cognitive-behavioral (Group meeting)
Reminders (Group meeting)
n Entered:
30
n Analyzed: 18
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Excluded from meta-analysis as no relevant
outcome.
Subjective distress decreased in the stress
management group (arm 2) as compared to the
usual care group (arm 1). This study lacked
significant statistical power to detect potentially
meaningful between-group differences.
Follow-up times: n/a
247
Evidence Table 4: Hypertension
Condition (Type)
Study Design
First Author
Quality
Year
Population
(ID)
Characteristics
Blumenthal JA, 1991 Hypertension
(#752)
(Essential, Systolic
and Diastolic,
Treated and
Untreated)
RCT
Intervention
Arm Sample Size
1 Usual Care (n/a)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n Entered:
23
n Analyzed: 31
2
Dietary monitoring (Self-delivery)
Exercise program (Group meeting)
Jadad Score: 1
Diagnostic criteria:
MD and blood
pressure recordings
n Entered:
41
n Analyzed: 31
3
Comorbidities:
n/a
Given C, 1984
(#2309)
n Entered:
35
n Analyzed: 31
Hypertension
(Systolic and
diastolic, Treated,
and Medication
treatment)
1
RCT
2
Jadad Score: 1
Diagnostic criteria:
MD and blood
pressure recordings
Dietary monitoring (Self-delivery)
Exercise program (Group meeting)
Usual Care (n/a)
n Entered: n/a
n Analyzed: 62
Cognitive-behavioral (One-on-one)
Cognitive-behavioral (Prescription)
Education (Instructional manuals)
Education (One-on-one)
Feedback (One-on-one)
n Entered: n/a
n Analyzed: 62
Comorbidities:
n/a
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
248
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Diastolic BP (mmHg) at 16 weeks:
Arm 1 = 90 (6.2)
Arm 2 = 89 (6.8)
Arm 3 = 89 (6.4)
Systolic BP (mmHg) at 16 weeks:
Arm 1 = 133 (8.6)
Arm 2 = 133 (10.4)
Arm 3 = 136 (11.6)
Follow-up times: 16 WK
Diastolic BP (mmHg) at 24 weeks:
Arm 1 = 91.4 (5.6)
Arm 2 = 87.1 (7.1)
Systolic BP (mmHg) at 24 weeks:
Arm 1 = 138.0 (8.9)
Arm 2 = 135.1 (12.9)
Follow-up times: 6 MO
Evidence Table 4: Hypertension (con't)
First Author
Year
(ID)
Goldstein IB, 1982
(#2466)
Condition (Type)
Study Design
Quality
Population
Characteristics
Hypertension
(Essential, Systolic
and Diastolic,
Treated and
Untreated)
Intervention
Arm Sample Size
1 Control (n/a)
Blood pressure monitoring (Self-delivery)
Self monitoring (Self-delivery)
n Entered:
n Analyzed:
9
9
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
RCT
Jadad Score: 1
2
Blood pressure monitoring (Self-delivery) Tailored:
Medication therapy (n/a)
Group Setting:
Self monitoring (Self-delivery)
Feedback:
Psychological:
n Entered:
9
Primary MD:
n Analyzed:
9
Yes
No
No
No
No
3
Blood pressure monitoring (Self-delivery) Tailored:
Cognitive-behavioral (n/a)
Group Setting:
Self monitoring (Self-delivery)
Feedback:
Psychological:
n Entered:
9
Primary MD:
n Analyzed:
9
No
No
No
Yes
No
4
Blood pressure monitoring (Self-delivery) Tailored:
Nontraditional therapies (One-on-one)
Group Setting:
Self monitoring (Self-delivery)
Feedback:
Psychological:
n Entered:
9
Primary MD:
n Analyzed:
9
Yes
No
No
No
No
Diagnostic criteria:
Blood pressure
recordings
Comorbidities:
Tobacco abuse
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Diastolic BP (mmHg) at 8 weeks:
Arm 1 = 98.8 (6.7)
Arm 2 = 92.6 (6.7)
Arm 3 = 100.6 (6.7)
Arm 4 = 92.9 (6.7)
Systolic BP (mmHg) at 8 weeks:
Arm 1 = 144.7 (12.4)
Arm 2 = 129.4 (12.4)
Arm 3 = 152.3 (12.4)
Arm 4 = 145 (12.4)
Follow-up times: 2 WK, 4 WK, 6 WK, 8 WK, 3
MO, 4 MO, 5 MO
249
Evidence Table 4: Hypertension (con't)
First Author
Year
(ID)
Hafner RJ, 1982
(#2467)
Condition (Type)
Study Design
Quality
Population
Characteristics
Hypertension
(Essential, Systolic
and Diastolic,
Treated)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
n Analyzed:
8
7
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
RCT
Jadad Score: 1
2
Diagnostic criteria:
MD
Cognitive-behavioral (Group meeting)
Cognitive-behavioral (Self-delivery)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Cognitive-behavioral (Group meeting)
Tailored:
Cognitive-behavioral (Self-delivery)
Group Setting:
Nontraditional therapies (Group meeting) Feedback:
Psychological:
n Entered:
8
Primary MD:
n Analyzed:
7
Yes
Yes
No
Yes
No
n Entered:
n Analyzed:
8
7
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Diastolic BP (mmHg) at 20 weeks:
Arm 1 = 96.3 (6.7)
Arm 2 = 88.2 (6.7)
Arm 3 = 91.9 (6.7)
Systolic BP (mmHg) at 20 weeks:
Arm 1 = 150.5 (12.4)
Arm 2 = 132.9 (12.4)
Arm 3 = 139.2 (12.4)
Follow-up times: 8 WK, 3 MO, 5 MO
Comorbidities:
n/a
3
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
250
Evidence Table 4: Hypertension (con't)
First Author
Year
(ID)
Hoelscher TJ, 1986
(#2457)
Condition (Type)
Study Design
Quality
Population
Characteristics
Hypertension
(Essential, Systolic
and Diastolic,
Treated and
Untreated)
RCT
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
14
n Analyzed: 12
2
Jadad Score: 1
Diagnostic criteria:
Blood pressure
recordings
Comorbidities:
n/a
Cognitive-behavioral (One-on-one)
Feedback (One-on-one)
Practice self care skills (Self-delivery)
Psychological assessment/care (One-onone)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Diastolic BP (mmHg) at 9-10 week:
Arm 1 = 95.6 (6.7)
Arm 2 = 91.6 (9.0)
Arm 3 = 89.5 (6.9)
Arm 4 = 87.5 (5.9)
Yes
No
Yes
Yes
No
Systolic BP (mmHg) at 9-10 week:
Arm 1 = 146.9 (18.4)
Arm 2 = 138.1 (13.6)
Arm 3 = 135.7 (9.4)
Arm 4 = 140.3 (10.6)
Follow-up times: 6 WK, 9 WK
n Entered:
12
n Analyzed: 12
3
Feedback (One-on-one)
Practice self care skills (Self-delivery)
Psychological assessment/care (Group
meeting)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
n Entered:
12
n Analyzed: 12
4
Contracts (Group meeting)
Contracts (Telephone)
Feedback (One-on-one)
Practice self care skills (Self-delivery)
Psychological assessment/care (Group
meeting)
n Entered:
12
n Analyzed: 12
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
251
Evidence Table 4: Hypertension (con't)
First Author
Year
(ID)
Irvine MJ, 1986
(#2458)
Condition (Type)
Study Design
Quality
Population
Characteristics
Hypertension
(Diastolic, Treated
and untreated,
Medication
treatment)
Intervention
Arm Sample Size
1 Control (n/a)
Education (One-on-one)
Exercise program (One-on-one)
Nontraditional therapies (One-on-one)
2
Diagnostic criteria:
Blood pressure
recordings
Jacob RG, 1985
(#2459)
Comorbidities:
n/a
Hypertension
(Systolic and
diastolic, Untreated,
No medication
treatment)
RCT
Jadad Score: 1
Diagnostic criteria:
Blood pressure
recordings
Comorbidities:
Obesity and
cholesterol
n/a
n/a
n/a
n/a
n/a
n Entered:
16
n Analyzed: n/a
RCT
Jadad Score: 1
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Cognitive-behavioral (One-on-one)
Education (One-on-one)
Nontraditional therapies (One-on-one)
n Entered:
16
n Analyzed: n/a
1
Usual Care (n/a)
n Entered:
28
n Analyzed: 30
2
Cognitive-behavioral (Group meeting)
Cognitive-behavioral (Video/audio tapes)
Dietary monitoring (Self-delivery)
Education (Group meeting)
Financial incentives (Group meeting)
Practice self care skills (Self-delivery)
Reminders (Group meeting)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
Yes
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Excluded from meta-analysis as no usual care
or comparable control group.
At 6-month follow up, significantly greater
decreases were seen for both systolic BP and
diastolic BP in the relaxation arm (arm 2)
compared with control arm (arm 1) (p<0.01,
p<0.05, respectively).
Follow-up times: 10 WK, 22 WK
Diastolic BP (mmHg) at 24 weeks:
Arm 1 = 85.5 (6.7)
Arm 2 = 85.6 (6.7)
Systolic BP (mmHg) at 24 weeks:
Arm 1 = 138.4 (12.4)
Arm 2 = 137.4 (12.4)
Follow-up times: 2 MO, 6 MO, 7 MO, 1 YR
n Entered:
29
n Analyzed: 30
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
252
Evidence Table 4: Hypertension (con't)
Condition (Type)
Study Design
First Author
Quality
Year
Population
(ID)
Characteristics
Jorgensen RS, 1981 Hypertension
(#2452)
(Essential, Treated,
and Medication
treatment)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
n Analyzed:
8
8
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
RCT
2
Diagnostic criteria:
MD
Cognitive-behavioral (Group meeting)
Cognitive-behavioral (Video/audio tapes)
Feedback (Group meeting)
Follow up (Group meeting)
Practice self care skills (Group meeting)
Comorbidities:
n/a
n Entered:
10
n Analyzed:
8
Jadad Score: 1
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Diastolic BP (mmHg) at 12 weeks:
Arm 1 = 85.4 (6.7)
Arm 2 = 69.5 (6.7)
Systolic BP (mmHg) at 12 weeks:
Arm 1 = 137.8 (12.4)
Arm 2 = 110.8 (12.4)
Follow-up times: 6 WK
253
Evidence Table 4: Hypertension (con't)
First Author
Year
(ID)
Kostis JB, 1992
(#2472)
Condition (Type)
Study Design
Quality
Population
Characteristics
Hypertension
(Essential, Systolic
and Diastolic,
Treated and
Untreated)
Intervention
Arm Sample Size
1 Control (n/a)
Placebo medication (n/a)
n Entered:
26
n Analyzed: 33
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
RCT
2
Jadad Score: 2
Diagnostic criteria:
Blood pressure
recordings
Comorbidities:
n/a
3
Blood pressure lowering medication (n/a) Tailored:
Group Setting:
n Entered:
28
Feedback:
n Analyzed: 33
Psychological:
Primary MD:
Yes
No
No
No
No
Cognitive-behavioral (Group meeting)
Dietary monitoring (Self-delivery)
Education (Group meeting)
Exercise program (Self-delivery)
Goal setting (Group meeting)
Social support (Group meeting)
Yes
Yes
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Diastolic BP (mmHg) at 12 weeks:
Arm 1 = 100.9 (6.7)
Arm 2 = 90.7 (6.7)
Arm 3 = 92.7 (6.7)
Systolic BP (mmHg) at 12 weeks:
Arm 1 = 162.1 (12.4)
Arm 2 = 152.6 (12.4)
Arm 3 = 149.9 (12.4)
Follow-up times: 3 MO
n Entered:
38
n Analyzed: 33
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
254
Evidence Table 4: Hypertension (con't)
First Author
Year
(ID)
Lagrone R, 1988
(#2460)
Condition (Type)
Study Design
Quality
Population
Characteristics
Hypertension
(Essential, Systolic
and Diastolic,
Treated)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered: n/a
n Analyzed: 10
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
RCT
2
Jadad Score: 1
Diagnostic criteria:
Blood pressure
recordings
Comorbidities:
Obesity
Dietary monitoring (Self-delivery)
Education (Group meeting)
Exercise program (Self-delivery)
n Entered: n/a
n Analyzed: 10
3
Cognitive-behavioral (Group meeting)
Dietary monitoring (Self-delivery)
Education (Group meeting)
Exercise program (Self-delivery)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
No
Yes
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Yes
Yes
Yes
No
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Diastolic BP (mmHg) at 8 weeks:
Arm 1 = 94.6 (6.7)
Arm 2 = 84.9 (6.7)
Arm 3 = 86.9 (6.7)
Systolic BP (mmHg) at 8 weeks:
Arm 1 = 136.1 (12.4)
Arm 2 = 126.1 (12.4)
Arm 3 = 134.5 (12.4)
Follow-up times: 2 WK, 10 WK
n Entered: n/a
n Analyzed: 10
Leveille SG, 1998
(#1175)
Hypertension
(Not specified)
1
n Entered: 100
n Analyzed: 93
RCT
Jadad Score: 2
Diagnostic criteria:
n/a
Comorbidities:
Heart disease, DM,
arthritis, tobacco
abuse, and cancer
and stroke
Usual Care (n/a)
2
Education (Group meeting)
Education (Instructional manuals)
Education (Reading material)
Follow up (One-on-one)
Follow up (Telephone)
Goal setting (One-on-one)
The intervention group (arm 2) had fewer
disability days and less self-reported functional
decline but there were no differences based on
physical performance tests when compared with
the usual care group (arm 1). The number of
inpatient days was significantly less for
intervention subjects (33 days versus 116 days
for usual care group, p=0.049). Intervention
subjects also had greater physical activity
(p=0.03) and less psychoactive medication use
(p=0.04) than usual care group.
n Entered: 101
n Analyzed: 95
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
255
Evidence Table 4: Hypertension (con't)
First Author
Year
(ID)
Morisky DE, 1983
(#2304)
Condition (Type)
Study Design
Quality
Population
Characteristics
Hypertension
(Systolic and
diastolic)
Intervention
Arm Sample Size
1 Usual Care (n/a)
n Entered:
50
n Analyzed: 30
RCT
Jadad Score: 1
2
Diagnostic criteria:
MD and blood
pressure recordings
Comorbidities:
Heart disease,
kidney disease, DM,
and CHF
Counseling/therapy (One-on-one)
n Entered:
50
n Analyzed: 35
3
Education (One-on-one)
n Entered:
50
n Analyzed: 36
4
Cognitive-behavioral (Group meeting)
n Entered:
50
n Analyzed: 32
5
Counseling/therapy (One-on-one)
Education (One-on-one)
n Entered:
50
n Analyzed: 43
6
Cognitive-behavioral (Group meeting)
Counseling/therapy (One-on-one)
n Entered:
50
n Analyzed: 36
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
No
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Insufficient statistics for meta-analysis.
Study subjects assigned to any of the
experimental groups had a 30% improvement in
blood pressure control at 2 years and a 70%
improvement at 5 years compared to 22% for
the usual care group with no difference in
weight control or compliance in appointments.
There was a 57% reduction in the 5-year allcause mortality for intervention subjects
compared to those receiving usual care
(p<0.05).
Follow-up times: 2 YR, 5 YR
256
Evidence Table 4: Hypertension (con't)
First Author
Year
(ID)
Morisky DE, 1983
(#2304)
continued
Condition (Type)
Study Design
Quality
Population
Characteristics
Intervention
Arm Sample Size
7 Cognitive-behavioral (Group meeting)
Education (One-on-one)
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
Yes
No
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
Cognitive-behavioral (One-on-one)
Tailored:
Cognitive-behavioral (Video/audio tapes) Group Setting:
Feedback:
n Entered:
19
Psychological:
n Analyzed: 16
Primary MD:
Yes
No
No
Yes
No
n Entered:
50
n Analyzed: 36
8
Cognitive-behavioral (Group meeting)
Counseling/therapy (One-on-one)
Education (One-on-one)
n Entered:
50
n Analyzed: 42
Southam MA, 1982
(#2453)
Hypertension
(Essential, Systolic
and Diastolic,
Treated)
1
Usual Care (n/a)
n Entered:
23
n Analyzed: 16
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
RCT
2
Jadad Score: 2
Diagnostic criteria:
MD and blood
pressure recordings
Diastolic BP (mmHg) at 24 weeks:
Arm 1 = 90.8 (6.7)
Arm 2 = 85.8 (6.7)
Systolic BP (mmHg) at 24 weeks:
Arm 1 = 141.3 (12.4)
Arm 2 = 137.0 (12.4)
Follow-up times: 9 WK, 6 MO
Comorbidities:
Tobacco abuse
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
257
Evidence Table 4: Hypertension (con't)
First Author
Year
(ID)
Taylor CB, 1977
(#2464)
Condition (Type)
Study Design
Quality
Population
Characteristics
Hypertension
(Essential, Systolic
and Diastolic,
Treated)
Intervention
Arm Sample Size
1 Control (n/a)
Practice methods (Protocols)
n Entered:
14
n Analyzed: 10
Intervention
Characteristics
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
n/a
n/a
n/a
n/a
n/a
RCT
Jadad Score: 2
2
Diagnostic criteria:
Blood pressure
recordings and
Routine
hypertension workup
n Entered:
13
n Analyzed: 10
3
Comorbidities:
n/a
Counseling/therapy (One-on-one)
Feedback (One-on-one)
Practice methods (Protocols)
Cognitive-behavioral (One-on-one)
Cognitive-behavioral (Video/audio tapes)
Feedback (One-on-one)
Practice methods (Protocols)
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
Tailored:
Group Setting:
Feedback:
Psychological:
Primary MD:
Yes
No
Yes
Yes
No
Meta-Analysis Data* or Outcomes
Follow-up Time(s)
Diastolic BP (mmHg) at 24 weeks:
Arm 1 = 94.5 (6.7)
Arm 2 = 88.5 (6.7)
Arm 3 = 90.0 (6.7)
Systolic BP (mmHg) at 24 weeks:
Arm 1 = 138.0 (12.4)
Arm 2 = 137.0 (12.4)
Arm 3 = 137.8 (12.4)
Follow-up times: 8 WK, 6 MO
n Entered:
13
n Analyzed: 10
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
258
Evidence Table 5. Cost Articles
Article
numb
er
Author/
Year
Diabetes
2270
Rettig et
al.,
1986
Subjects (S), Followup period (F/U),
Research design (D)
and settings (ST)
Interventions
Costs of
intervention
Effectiveness
Health care costs or
utilizations
C/E Ratings
S : 393 type1 and type
2 diabetic patients
recruited from among
diabetic inpatients
(mean = 52, 67%
female)
F/U: 6 and 12 months
D: RCT
ST: Patient home
I: Needs assessment
and tailored individual
instruction at patient
home by a trained RN
or LPN from home
health nursing
agencies.
C: Usual care
Not reported, but
involving 4-day
intensive course in
diabetes self-care for
participating nurses,
and several home
visits (no more than
12 for each
individual).
At 6 months, intervention
subjects showed
significantly greater self-care
knowledge and skills than
control, although the actual
differences in self-care skills
were probably too small to
have any practical meaning.
No differences between the
groups were noted after 12
mo of F/U.
Based on self-report. At 4
month f/u, all respondents
reported a decline in
performing self-care
behaviors in comparison
with the 1-month f/u.
Compliance was lower for
the control group.
Intervention group showed
significantly better
compliance than control in
regards to exercise, diet,
administering insulin, and
better outcome measures
relating to improved
metabolic control and
significant reduction in blood
sugar levels.
No significant effect of
education program on
metabolic control or quality
of life.
At 6 and 12 months, no
difference was found
between control and
intervention subjects in
terms of diabetes-related
hospitalizations, length of
hospital stay, foot
problems, emergency
room and physician visits,
and sick days.
Not costeffective.
The intervention group
experienced a significantly
lower emergency room
visitation rate (p <.005): At
4 months, the 40 control
patients reported 20 ER
visits, and the 53
intervention patients
reported 2 ER visits. The
control patients reported
18 hospital readmission,
and the intervention
patients reported 8
hospital readmission.
Likely to be
cost-savings.
No significant effect of
education program on
costs of using health
services (although the
experimental groups
showed a trend to a
decrease in the length of
Not costeffective.
Possible
reasons
include the
quality of the
education
2159
Wood,
1989
S: 93 hospitalized
patients with type 1 or
2 diabetes, age 20 to
75 years old (mean 60,
53% female).
F/U: 1 mo, and 4
months.
D: RCT
ST: Hospital
I: Inpatient group
education program
which stressed both
knowledge and selfhelp behaviors.
C: Usual care
Not reported, but
each patient attended
two days of 2-hour
education program,
with an average
attendance of four to
st
six patients. The 1
session was taught
by a nurse educator,
nd
and the 2 by a
registered dietitian
and a community
health nurse.
2589
de
Weerdt
et al.,
1991
S : 558 insulin-treated
diabetic patients age
18-65 years old (mean
= 45)
F/U : 6 months
D: RCT
ST: 15 hospitals in
I: 1) Collaborative
group education led by
health-care worker
(HCW), 2) Same
education led by fellow
patients
C: Usual care
Direct costs of the
education program
(including the costs of
employing the
educators) and
indirect costs (costs
of the hours spent by
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
259
Evidence Table 5: Cost Articles (con't)
Netherlands (5 for
control)
the participants in
attending the
education) together
equal to US$100 per
patient (1990 dollar).
Adding the cost of
developing
educational materials
make the per-patient
cost to US$144 (1990
dollar). No difference
between I1 and I2.
2175
Kaplan
et al.,
1987
S : 76 volunteer adults
with type 2 diabetes
(44 women), mean age
= 55.
F/U: 3, 6, 12, and 18
months.
D: RCT
ST: Community
I: Behavioral-based
group intervention.
Each participant was
assigned to one of the
three 10-week
programs: 1) diet, 2)
exercise, 3) diet plus
exercise.
C: 10-week programs
of group education.
Direct cost for diet
and exercise
combined program is
estimated to be
$1000 (1986 dollar)
per participant
(including charges for
history and physical,
lab work, sessions,
and medical
consultations). This is
non-incremental cost.
0749
Arsenna
u et al.,
1994
S : 40 patients (mean
= 59) attending
diabetes education
program
F/U: 2 and 5 months
D: RCT
ST : Hospital
I : Individualized
learning activity
packages (LAP)
C: Classroom
instruction
Instruction at the
hospital costs $31 per
hour (1995 dollar),
The three LAPs were
developed to require
3.5 hours of
instructional time.
Thus using LAPs
could save individuals
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
70/76 completed follow-up
study. At 18 months, the
combination diet-andexercise group had achieved
the greatest reductions in
glycosylated hemoglobin
measures. In addition, this
group showed significant
improvements on a general
quality of life measure, equal
to 0.092 incremental years
of well-being for each
participant compared to
control.
At the 5-month f/u, the LAP
group scored significantly
higher on knowledge
assessment and decreased
percent of ideal body weight.
Patients who received
classroom instruction
exhibited significantly
decreased glycosylated
hospitalization, but it was
not significant). Almost
equal changes in the
number of visits to the
physician and GP were
found. No significant
difference in the daily
insulin dosage and
number of injections were
found between groups.
Compared with the control
group, frequency of selfblood glucose monitoring
increased significantly in
both experimental groups.
No significant effect of
education on the number
of sick days was found.
N/A.
program, and
the lack of
supportive
changes in
standard
therapy and
follow-up of the
education
given.
Not studied.
LAPs could
provide a
cheaper
means of edu.,
but less
effectiveness
in lowering
blood glucose
levels than
Authors
reported
cost/utility =
$10870/well
year. However,
cost is not
calculated
incrementally
(if so, the C/U
rate would be
more
favorable).
260
Evidence Table 5: Cost Articles (con't)
2586
Campbe
ll et al.,
1996
S : 238 type 2 DM
patients, 80 years or
younger (mean = 58,
51% female) without
previous formal
instruction in diabetes
care.
F/U: 3, 6, and 12
months
D: RCT
ST: Patients were
referred to a Diabetes
Education Service for
education programs.
Behavioral program
was conducted in
patient home.
I: Comparing relative
effectiveness of the
following programs: 1)
minimal instruction
program, 2) education
program of individual
visits, 3) education
program incorporating
a group education
course, 4) behavioral
program. (Note: 2) and
3) are standard care.)
3433
Glasgo
w et al.,
1997
S : 206 diabetic
patients 40 years and
older (mean age = 62,
62% female)
F/U: 12 months
D: RCT
ST: Outpatient clinics
1668
Sadur et
S : 185 patients of a
I: Individualized,
medical office-based
intervention focused
on dietary selfmanagement, involved
touch screen
computer-assisted
assessment that
provided feedback on
key barriers to dietary
self-management, goal
setting and problemsolving counseling.
Follow-up components
included phone calls
and videotape
intervention relevant to
each participant.
C: Usual care
I: Multidisciplinary
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
$108.50 in
instructional fees.
Not reported, but
involving 1) two 1hour sessions, 2) two
initial sessions, and
30 minuets monthly
session for 1 year, 3)
at least two individual
sessions and a 3-day
small group education
course, as well as
two-hour group
follow-ups at 3 & 9
months, 4) 6 or more
individual visits from a
nurse educator
hemoglobin levels.
From the perspective
of a health care
organization, the
incremental cost for
the delivery of the
intervention totaled
$14,755, or $137 per
participant (1995
dollars).
The intervention produced
significantly greater
improvement than usual
care on multiple measures
of change in dietary
behavior (e.g., covariate
adjusted difference of 2.2%
of calories from fat; p
=0.023) and on serum
cholesterol levels (covariate
adjusted difference of
15mg/dl; p = 0.002) at 12month follow-up. There
were also signicicant
differences favoring
intervention on patient
satisfaction (p < 0.02). No
significant improvement on
either HbA1c or on BMI.
After the intervention, HbA1c
Not reported, but may
Individual and group
education programs had
higher attrition rates (40%)
than the behavioral and
minimal programs (10%). No
different outcomes were
found between groups in
terms of physiological
measures and BMI, except
for behavioral program
produced a greater
reduction in diastolic blood
pressure over 12 mos and a
greater reduction in the
cholesterol risk ratio over 3
mos. The behavioral
program patients reported
higher satisfaction.
classroom edu.
There were no differences
between groups over
three time periods in
proportion of patients
consulting an
ophthapmologist. The
behavioral program
patients were more likely
to have visited a podiatrist
after 6 months. The
groups did not differ in
terms of a mean number
of visits they had made to
a general practitioner , in
hospital admissions, or in
the proportion who had
changed the intensity of
their blood pressure
treatment.
Not studied.
Programs that
are more
intensive in
terms of
patient time
and resources
may not be
more effective,
and thus be
less costeffective.
Intervention group
For patients
$7-$8 per
mg/dl
reduction in
cholesterol
compare well
to estimates of
alternative
intervention
including
cholesterol
lowering
medications,
which can cost
from $350 to
$1400 per
patient year.
261
Evidence Table 5: Cost Articles (con't)
0828
al.,
1999
HMO aged 16-75
(mean = 56, 43%
female) and had either
poor glycemic control
or no HbA1c test
performed during the
previous year
F/U : 6 and 12 months
after randomization
D: RCT
ST: Outpatient clinic
outpatient diabetes
care management
delivered by a diabetes
nurse educator, a
psychologist, a
nutritionist, and a
pharmacist in cluster
visit settings of 10-18
patients/month for 6
months.
C: Usual care
not be more costly
than usual care since
3 providers saw 1218 patients for a 2hour session monthly
(somewhat higher
number of patients
than these same
providers would see
in one-on-one
sessions during the
same 2 hour), and
modestly reduced
physician visits.
Litzelma
n et al.,
1993
S : 395 patients with
type 2 DM who
underwent the initial
patient risk
assessment (352
completed the study)
(mean age = 60, 81%
female, most subjects
are poorly educated
and indigent black
women)
F/U : Completion of
intervention (12 month
from initial
assessment)
D: RCT
ST: Academic
outpatient clinic
I: Multifaceted,
including 1) patient
education and
behavioral contract
about foot-care, and
also reinforcement
reminders, 2) health
care system support of
identifiers on patient
folders to prompt
providers, 3) given
providers practice
guidelines and
informational flow
sheets on foot-related
risk factors for
amputation.
C: Usual care
The study materials,
including folders, foot
decals, postage,
printing, and
educational materials,
cost less than $5000.
The major expense of
the study was the
salary support for the
nurse-clinicians who
did the assessments
and for the research
assistant who
processed the charts.
S : 100 subjects with
arthritis. 85 completed
study. Mean age = 64.
73% female. 73% had
I1 = An Arthritis SelfManagement course
(ASM) group taught by
a male rheumatologist
The 12-hour course
taught by 2 layleaders would cost
from $0.00
Osteoarthritis
0830
Lorig et
al.,
1986
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
levels declined significantly
in the intervention subjects
compared to control
subjects. Several self-care
practices and several
measures of self-efficacy
improved significantly in the
intervention group.
Satisfaction with the
program was high.
Limitation: Failure to obtain
follow-up HbA1c levels and
questionnaires on 16% and
25% of subjects
respectively.
Patients receiving the
intervention were less likely
than control patients to have
serious foot lesions (odds
ratio 0.41, p = 0.05) and
other dermatological
abnormalities. Also they
were more likely to report
appropriate self-foot-care
behaviors, to have foot
examinations during office
visits (68% vs. 28%, p <
0.001), and to receive footcare education from health
care providers (42% vs.
18%, p < 0.001). Physicians
assigned to intervention
patients were more likely
than physicians assigned to
control patients to examine
patients’ feet.
patients had somewhat
higher ambulatory care
utilization and more
intensive pharmaceutical
management than control
subjects during the 6month intervention. This
excess utilization was
offset by fewer hospital
admissions after the
intervention. Both hospital
and outpatient utilization
were significantly lower for
intervention subjects after
the end of the program.
At the end of the
intervention, four
amputations had been
done in the control group
compared with one in the
intervention group.
(Incidence rate is too
small to test statistical
significance). Physicians
assigned to intervention
patients were more likely
than physicians assigned
to control patients to refer
patients to the podiatry
clinic, but no difference in
the pattern of patient
referral to orthopedics and
vascular surgery clinics.
Professional-taught groups
demonstrated greater
knowledge gain while laytaught groups had greater
No significant difference in
number of visits to
physician at 4 months
follow-up between groups
who had poor
diabetic
management,
providing this
intensive
management
program may
be cost neutral
in the short
term (< 2
years).
Indicative costeffective.
Insufficient
information
about cost
saving.
Lay-taught
ASM course
could be as
effective as
262
Evidence Table 5: Cost Articles (con't)
0835
OA.
F/U: 4 months
D: RCT
ST: Community sites
and a female physical
therapist.
I2 = An ASM course
group taught by 2
female lay-leaders.
C: No intervention.
Lorig et
al.,
1985
S : 190 subjects with
arthritis. Mean age =
67. 83% female. 77%
had OA.
F/U: 4 months RCT
and 20 months
longitudinal study.
D: RCT + longitudinal
study
ST: Community sites
I: An Arthritis SelfManagement course
(ASM) given in 6
sessions by lay
persons, based on a
standardized
educational protocol
emphasizing group
discussion, practice,
the use of contracts
and diaries to improve
compliance, and
weekly feedback. No
subsequent
reinforcement. (129
subjects)
C: Delayed
intervention for 4
months. (61 subjects)
Mazzuc
a et al.,
1999
S : 211 patients with
knee OA from the
general medicine clnic
of a municipal hospital
(Of which 25 lost to
f/u). Mean age = 63.
85% female.
F/U: 1 year
D: CT (Nonrandomized
Attention-controlled
clinical trial)
I : Self-care education:
Individualized
instruction and followup emphasizing
nonpharmacologic
management of joint
pain
C: A standard public
education presentation
and attentioncontrolling follow-up.
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
(volunteer) to $200
(1985 dollars). By one
health professional,
the course would cost
from $240 ($20/h) to
$600 ($50/h). The
costs of training and
support for layleaders were not
accounted.
$15 to $20 per
participant. (1983
dollars).
changes in relaxation than
the other two groups. The
subjects who received ASM
course were more likely to
exercise, and a tendency
toward less disability than
control subjects.
or change from baseline.
At 4 months, experimental
subjects significantly
exceeded control subjects in
knowledge, recommended
behaviors, and in lessened
pain. These changes
remained significant at 20
months.
At 4 months, there was a
tendency of decline in
visits to physicians by the
intervention group, but did
not reach statistical
significance at .05 level.
The 20 months
longitudinal study showed
the number of physician
visits reduced from
baseline to 4-month f/u,
and from 4 months to 8months, and remained
about the same from 8
months to 20 months.
These changes did not
reach statistical
signiciance.
The cost of
deliverying the selfcare education
intervention to 105
subjects was $6,163
(in 1996 dollars), or
equivalently, $58.70
per patient.
See health care costs or
utilizations.
The 94 subjects remaining
in intervention group
made 528 primary care
visits during the follow-up
year, while the 92
controlled patients made
616 visits. The average
subject in intervention
group generated $262 in
clinic costs, compared
with $322 for the average
professionaltaught yet
cheaper.
However, both
failed to
demonstrate
reduction in
number of
physician
visits.
Indicative costeffective.
Insufficient
information
about cost
saving.
For more than
50% of
patients
receiving the
intervention,
the reduced
outpatient
visits and costs
offset the
intervention
costs. 80% of
263
Evidence Table 5: Cost Articles (con't)
ST: Outpatient clinic
Groessl
&
Cronan,
2000
Hypertension
2457
Hoelsch
er et al.,
1986
subject in control group.
The frequencies and costs
associated with charges
for drugs, radiography,
and laboratory tests were
similar between groups.
the
intervention
costs was
offset within
one year due
to reduced
outpatient
visits.
Cost effective
and cost
saving. The
one-year costbenefit ratio
was $7.29:1.
The three-year
cost-benefit
ratio was
$22.05:1.
S : 363 members of a
HMO, 60 years of age
and older with OA.
Mean age = 70.
F/U: 3 years
D: RCT
ST: Community
I1: Social support
I2: Education
I3: A combination of
social support and
education
C: Usual care
$9450 for social
support group,
$18675 for education
group, and $14175
for combination
group, totaling
$42300 (all in 1992
dollars).
Feelings of helplessness
decreased in the
intervention groups but not
in the control group. All
groups showed increases in
self-efficacy and overall
health status.
Health care costs
increased less in the
intervention groups than in
the control group. Based
on the HMO data, health
care cost savings were
$1,156/participant for year
one and two, and
$1,279/participant for year
three (1992 dollars).
S: 50 (24 female) adult
average 51.1 years of
age with essential
hypertension recruited
via media
announcements.
Secondary
hypertension or with
mean baseline blood
pressures greater than
180 mm Hg systolic or
120 mm Hg diastolic
were excluded.
F/U: 6 weeks
D: RCT
ST: Patient home
I: 1) individualized
relaxation (IR), 2)
group relaxation (GR),
3) group relaxation
plus contingency
contracting for home
practice (GRCC)
C: Waiting list control
Measured by
therapist time
Measured by percent
reductions in systolic and
diastolic blood pressure, and
by eliciting home relaxation
practice
Not measured.
GR was
significantly
more cost
effective than
IR for systolic,
whereas both
GR and GRCC
were more
cost effective
than IR for
diastolic blood
pressure. For
amount of
relaxation
practice, GR >
GRCC > IR.
I1A: Medically directed
at-home rehabilitation
training for 23 weeks
I1B: Medically directed
Three months of athome rehabilitation
was estimated to be
approximately $328
Compared to the group
rehabilitation, medically
directed at-home
rehabilitation had about
Not studied.
Medically
directed athome
rehabilitation
Post Myocardial Infarction Care
2669
DeBusk
S: 198 men 70 years
et al.,
or younger, had had
1985
clinically
uncomplicated AMI,
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
264
Evidence Table 5: Cost Articles (con't)
mean age 52 ± 9
years.
F/U: 26 weeks
D: RCT
ST: Patient home or
community gymnasium
0827
Lewin et
al.,
1992
S: 176 male and
female patients with an
AMI and age less than
80 years (mean age =
55.8 ± 10.6 years)
F/U: 1 year
D: RCT
ST: Patient home
at-home training for 8
weeks
I2A: Supervised group
training in a
gymnasium for 23
weeks
I2A: Supervised group
training in a
gymnasium for 8
weeks
I3: Exercise testing
without subsequent
exercise training
C: Neither testing nor
training
I: A comprehensive
self-help rehabilitation
programme based on
a heart manual
Spouses were given
materials to support
and encourage
compliance by
patients. Included
follow-up and
feedback.
C: Standard care plus
a placebo package of
information and
informal counseling.
per patient (1982 or
1983 dollar). The
group rehabilitation
program was
approximately $720.
equally high adherence to
individually prescribed
exercise, increase in
functional capacity, and low
nonfatal reinfarction and
dropout rates. Compared to
the no-training and control
groups, the training groups
were significantly greater in
functional capacity, but not
different in cardiac events.
The authors
estimated the cost of
treatment per patient
to be £30 - £50 (1990
dollar).
Psychological adjustment
was better in the
rehabilitation group at 1
year. The improvement was
greatest among patients
who were clinically anxious
or depressed at discharge
from hospital.
has the
potential to
decrease the
cost of
rehabilitating
low-risk
survivors of
AMI.
The two groups
significantly differed in the
number of GP
consultations at six
months and after the
second six months; the
control group made a
mean of 1.8 more visits
than did the rehabilitation
group in the first 6
months, and a mean of
0.9 more visits in the
subsequent 6 months. In
addition, significantly more
control patients than
rehabilitation group
patients were admitted to
hospital in the first 6
months (18 vs. 6) but not
at 12 months (18 vs. 9).
Significantly fewer
rehabilitation group
patients were readmitted
to hospital in the first 6
months (8% vs. 24%).
Based on
physician selfreport data for
use of health
services.
Indicative costsaving.
Non-disease-specific Programs
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
265
Evidence Table 5: Cost Articles (con't)
1175
Leveille
et al.,
1998
S: 201 chronically ill
seniors aged 70 and
older (mean age =
77.1 years) with heart
disease, high blood
pressure, arthritis,
cancer, stroke, or
diabetes. More % of
female in intervention
than in control (63.4%
vs. 48.0%)
F/U: 1 year
D: RCT
ST: A large senior
center, in collaboration
with primary care
providers of MCOs.
I: A geriatric nurse
practitioner (GNP) led
multi-component
program including risk
factor and health
assessment, feedback
to PCPs, follow-up
visits and phone
contacts, physical
activity for disability
prevention, and
individual counseling
about disease selfmanagement as well
as group classes.
C: Access to all senior
center activities, but no
GNP.
The authors
estimated the
program cost
(primarily the salaries
for the GNP and the
social worker) to be
approximately $300
(1997 dollar) annually
per participant.
The intervention group
showed less decline in
function, as measured by
disability days and lower
scores on the Health
Assessment Questionnaire.
However, the measures by
SF-36 and a battery of
physical performance tests
did not show difference by
intervention. The
intervention led to
significantly higher levels of
physical activity and senior
center participation.
1510
Colema
n et
al./1999
S: 169 patients aged
65 and older (mean =
77) with the highest
risk for being
hospitalized or
experiencing functional
decline
F/U: 2 years
D: RCT
ST: Nine primary care
physician offices in a
large staff-model HMO
I: Chronic Care Clinics
attempted to
reorganize the delivery
of primary care
services to better meet
the needs of older
persons with chronic
illness, including
disease management
planning, medication
review, patient selfmanagement/support
group)
Not available.
After 24 months, no
significant improvements in
frequency of incontinence,
proportion with falls,
depression scores, physical
function scores, or
prescriptions of high risk
medications were
demonstrated. A higher
proportion of intervention
patients rated the overall
quality of their medical care
as excellent compared with
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
The number of
hospitalized participants
increased by 69% (from
13 to 22) among the
controls and decreased by
38% (from 21 to 13) in
the intervention group (p =
.083). The total number of
inpatient hospital days
during the study year
decreased by 72% in the
intervention group but
increased by 21% in the
control group
(p = .049). The 83 less
hospital days in the
intervention group yielded
a savings of
approximately $1200 per
participant. Outpatient
visits did not change in the
intervention group but
slightly increased in the
control group. There were
two less ER visits in the
intervention group but 8
less ER visits in the
control group.
At baseline, intervention
patients were more likely
to be hospitalized. During
the 24-month follow-up,
costs of medical care
including frequency of
hospitalization, hospital
days, emergency and
ambulatory visit, and total
costs of care were not
significantly different
between intervention and
control groups.
Indicative cost
saving, due to
less hospital
use.
Insufficient
information
(implied not
cost saving).
266
Evidence Table 5: Cost Articles (con't)
C: Usual care
0608
Lorig et
al.,
1999
S: 952 patients 40
years and older (mean
= 65) with heart
disease, lung disease,
stroke, or arthritis.
F/U: 6 months
D: RCT
ST: Community-based
sites (churches, senior
and community
centers, public
libraries, & health care
facilities)
I: Subjects received
the Chronic Disease
Self-Management
Program (CDSMP), a
community-based
patient selfmanagement
education course. The
content and
methodology of the
CDSMP were based
on needs
assessments. The
process of teaching
the course is based on
Self-Efficacy Theory.
The course was taught
by a pair of trained,
volunteer lay leaders.
C: Waiting list control
N/A = Not Available or Not Applicable
NOS = Not Otherwise Specified
* Unless otherwise specified, Mean (Standard Deviation) reported.
The authors
estimated the
program cost to be
approximately $70
(1998 dollar) per
intervention
participant. This
includes $26 for
training leaders, $14
for volunteer leader
stipend, $15 for
course materials, and
$15 administrative
costs. This analysis
does not take into
account the cost of
space or indirect
costs.
control patients (40% vs.
25%, p = 0.1)
At 6 months, treatment
subjects demonstrated
improvements in weekly
minutes of exercise,
frequency of cognitive
symptom management,
communication with
physicians, self-reported
health, health distress,
fatigue, disability, and
social/role activities
limitations, compared with
control subjects. Program
effects were similar across
all four diagnostic
subgroups.
Based on patient selfreport, the treatment
group reduced their
physician visits slightly
more, but not significantly,
than did the control group.
However, the decrease in
the number of
hospitalizations and in the
length of hospital stays
were significant at p <.05.
Assuming a cost of $1000
per day of hospitalization,
the 6-month health care
costs for each control
participant in this study
were $820 greater than for
each treatment subjects.
Cost-effective
and indicative
cost-saving
(approximately
a saving of
$750 per
participant,
according to
author
estimates
based on
patient selfreported
utilization
data).
267