Features associated with diet pill use in individuals with eating disorders
advertisement

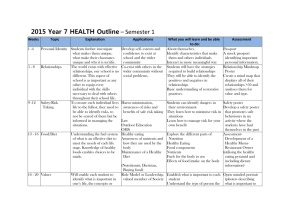
Author's personal copy Available online at www.sciencedirect.com Eating Behaviors 9 (2008) 73 – 81 Features associated with diet pill use in individuals with eating disorders Lauren Reba-Harrelson a , Ann Von Holle a , Laura M. Thornton b , Kelly L. Klump c , Wade H. Berrettini d , Harry Brandt e , Steven Crawford e , Scott Crow f , Manfred M. Fichter g , David Goldman h , Katherine A. Halmi i , Craig Johnson j , Allan S. Kaplan k , Pamela Keel l , Maria LaVia a , James Mitchell m , Katherine Plotnicov b , Alessandro Rotondo n , Michael Strober o , Janet Treasure p , D. Blake Woodside q , Walter H. Kaye b , Cynthia M. Bulik a,r,⁎ a Department of Psychiatry, University of North Carolina at Chapel Hill, NC, United States Department of Psychiatry, University of Pittsburgh Medical Center, Western Psychiatric Institute and Clinic, Pittsburgh, PA, United States c Department of Psychology, Michigan State University, East Lansing, MI, United States d Center of Neurobiology and Behavior, University of Pennsylvania, Philadelphia, PA, United States e Center for Eating Disorders, Sheppard Pratt Health System, Towson, MD, United States f Department of Psychiatry, University of Minnesota, Minneapolis, MN, United States g Klinik Roseneck, Hospital for Behavioral Medicine and University of Munich (LMU), Germany h National Institute of Alcohol Abuse and Alcoholism, Rockville, MD, United States i Weill Cornell Medical College, New York Presbyterian Hospital — Westchester Division, White Plains, NY, United States j Laureate Psychiatric Clinic and Hospital, Tulsa OK, United States k Program for Eating Disorders, Toronto General Hospital, University Health Network, University of Toronto, Canada l Department of Psychology, University of Iowa, United States m University of North Dakota School of Medicine and Health Sciences, Department of Clinical Neuroscience and Neuropsychiatric Research Institute, Fargo, ND, United States n Department of Psychiatry, Pharmacology and Biotechnologies, University of Pisa, Pisa, Italy o UCLA Semel Institute for Neuroscience and Human Behavior, David Geffen School of Medicine, University of California at Los Angeles, Los Angeles, CA, United States p Department of Psychiatry, Institute of Psychiatry, King's College, London, England, United Kingdom q Department of Psychiatry, University of Toronto, Toronto, Canada r Department of Nutrition, University of North Carolina, Chapel Hill, NC, United States b Received 12 January 2007; received in revised form 7 March 2007; accepted 25 April 2007 Abstract We investigated the relation between diet pill use and eating disorder subtype, purging and other compensatory behaviors, body mass index (BMI), tobacco and caffeine use, alcohol abuse or dependence, personality characteristics, and Axis I and Axis II Abbreviations: AN, Anorexia Nervosa; BN, Bulimia Nervosa; RAN, Restricting type, Anorexia Nervosa; PAN, Purging type, Anorexia Nervosa; BAN, Binging type, Anorexia Nervosa; PBN, Purging type, Bulimia Nervosa; NPBN, Non-purging type, Bulimia Nervosa; ANBN, Anorexia Nervosa, Bulimia Nervosa; EDNOS, Eating Disorder Not-Otherwise-Specified: Types 1, 2, and 3. ⁎ Corresponding author. Department of Psychiatry, University of North Carolina at Chapel Hill , 101 Manning Drive, CB #7160, Chapel Hill, NC 27599-7160, United States. Tel.: +1 919 843 1689; fax: +1 919 966 5628. E-mail address: cbulik@med.unc.edu (C.M. Bulik). 1471-0153/$ - see front matter © 2007 Elsevier Ltd. All rights reserved. doi:10.1016/j.eatbeh.2007.04.001 Author's personal copy 74 L. Reba-Harrelson et al. / Eating Behaviors 9 (2008) 73–81 disorders in 1,345 participants from the multisite Price Foundation Genetics Studies. Diet pill use was significantly less common in women with restricting type of AN than in women with other eating disorder subtypes. In addition, diet pill use was associated with the use of multiple weight control behaviors, higher BMI, higher novelty seeking, and the presence of anxiety disorders, alcohol abuse or dependence, and borderline personality disorder. Findings suggest that certain clinical and personality variables distinguish individuals with eating disorders who use diet pills from those who do not. In the eating disorder population, vigilant screening for diet pill use should be routine clinical practice. © 2007 Elsevier Ltd. All rights reserved. Keywords: Eating disorders; Diet pills; Weight control behaviors; Novelty seeking Abuse of diet pills by individuals with eating disorders is well-documented clinically, with prevalence estimates reported as high as 50% (Celio et al., 2006; Mitchell, Pomeroy, & Huber, 1988; Roerig et al., 2003; Steffen, Roerig, Mitchell, & Crosby, 2006). However, empirical studies of features associated with abuse of diet pills are lacking. Given potential adverse effects associated with abuse of these agents (e.g., side effects, tolerance, withdrawal) (Carek & Dickerson, 1999; Dietz, 1981; Shekelle, Morton, & Maglione, 2003), particularly in populations already at elevated medical risk, it is important to explicate the nature of diet pill abuse and its consequences in individuals with eating disorders. Accordingly, the aims of this study were to report the prevalence of lifetime diet pill use across eating disorder subtypes and identify factors associated with their use. We hypothesized that individuals with the restricting type of anorexia nervosa (RAN) would use diet pills less frequently than those with other subtypes. This may be due to the documented hesitancy of individuals with RAN to use medications of any variety (Kaplan & Olmsted, 1997), and the presence of low novelty seeking/elevated harm avoidance in this subgroup (Klump et al., 2000), which may render them less likely to experiment with anorexogenic agents. We also hypothesized that diet pill use would be positively associated with various purging behaviors (i.e., vomiting, laxative use, diuretic use, emetic use), highest lifetime BMI, excessive exercise, tobacco use, caffeine use and alcohol abuse or dependence, impulsivity, and novelty seeking. Further, we hypothesized that diet pill use would be positively associated with trait anxiety reflecting that greater anxiety and worry about weight gain may prompt the use of more substances to achieve lower weight. In addition we hypothesized that diet pill use would be associated with specific Axis I (anxiety and alcohol abuse or dependence) and Axis II disorders acknowledging the co-occurrence of anxious and impulsive traits in individuals with eating disorders (Cassin & von Ranson, 2005; Fichter, Quadflieg, & Rief, 1994) and the likelihood of these traits either alone or in combination leading to more extreme measures to decrease anxiety associated with weight. 1. Methods 1.1. Participants Participants were from two cohorts recruited for the multisite International Price Foundation Genetic Studies of Eating Disorders: one ascertained through a proband with BN (“BN Affected Relative Pair Study”; Kaye et al., 2004) and another ascertained through a proband with AN and including their parents (“AN Trios”). These studies were designed to identify susceptibility loci contributing to risk for eating disorders. Informed consent was obtained from all study participants, and all sites received approval from their local Institutional Review Board. Brief descriptions of each study are provided below. 1.1.1. BN Affected Relative Pair Study (BN-ARP) Probands and female and male biological relatives affected with AN, BN, or Eating Disorders Not Otherwise Specified (EDNOS) were recruited from 10 sites in North America and Europe including Pittsburgh, New York, Los Angeles, Toronto, Munich, Philadelphia, Pisa, Fargo, Minneapolis, and Boston. Probands were required to meet modified DSM-IV (American Psychiatric Association (APA), 1994) lifetime diagnosis of BN, purging type (PBN), where purging must have included regular vomiting, with other means of purging also allowed, and binge eating and vomiting must have occurred at least twice a week for a duration of at least six months. For the Author's personal copy L. Reba-Harrelson et al. / Eating Behaviors 9 (2008) 73–81 75 complete list of psychiatric and medical inclusion and exclusion criteria applied to probands and relatives see Kaye et al. (2004). 1.1.2. AN Trios study Female and male probands affected with AN were recruited from 9 sites in North America and Europe including Pittsburgh, New York, Los Angeles, Toronto, Munich, Pisa, Fargo, Baltimore, and Tulsa. Probands were required to meet the following criteria: (1) modified DSM-IV (APA, 1994) lifetime diagnosis of AN, with or without amenorrhea; (2) low weight that is/was less than 5th percentile of BMIs for age and sex (Hebebrand, Himmelmann, Heseker, Schafer, & Remschmidt, 1996) for the First National Health and Nutrition Examination Survey (NHANES) epidemiological sample; (3) onset prior to age 25; (4) weight that is/was controlled through restricting and/or purging, which includes vomiting, use of laxatives, diuretics, enemas, suppositories, or ipecac; (5) age between 13 and 65; (6) Caucasian (one grandparent from another racial group is acceptable); and (7) study diagnostic criteria had to be met at least three years prior to entry into the study. This last inclusion criterion ensured that individuals with AN who were likely to develop binge eating would be appropriately classified, as research has shown that most binge eating develops within the first three years of illness in AN (Eckert, Halmi, Marchi, Grove, & Crosby, 1995; Eddy et al., 2002; Strober, Freeman, & Morrell, 1997; Tozzi et al., 2005). Potential participants were excluded if they reported maximum BMI since puberty N27 kg/m2 for females and N27.8 kg/m2 for males. This exclusion of individuals who were overweight or obese was based designed to increase sample homogeneity. Further information on inclusion and exclusion criteria can be found in Reba et al. (2005). The total number of female participants from both cohorts with a diagnosis of AN (any type), BN, either subtype, or ED-NOS was 1465. Individuals were excluded from the present analyses if they had missing or inconsistent data regarding diet pill use (120) reducing the analyzable final sample to 1345. 1.2. Measures The Price Foundation studies included a comprehensive assessment battery measuring traits, characteristics, and behaviors of relevance to eating disorders. These variables were chosen to aid in the identification of subphenotypes and relevant covariates to enhance and refine our genome wide linkage analyses. 1.2.1. Demographic and clinical variables The data included age at interview, age at illness onset, duration of illness, current, lowest, and highest BMI. 1.2.2. Eating disorder diagnoses Lifetime histories of eating disorders and the presence or absence of eating disorder behaviors (e.g. dieting, binge eating, etc.) were assessed with the Structured Interview for Anorexia Nervosa and Bulimic Disorders (SIAB) (Fichter, Herpertz, Quadflieg, & Herpertz-Dahlmann, 1998) and with an expanded version of Module H of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) (First, Spitzer, Gibbon, & Williams, 1997). 1.2.3. Definition of diet pill use The presence or absence of lifetime diet pill use was assessed for all participants using screening interviews developed for each study. The lifetime diet pill use variable was constructed from the questions that addressed both current and past diet pill use. Current use was determined by the question, “How many diet pills do you currently consume each week?” (0 = no current use; N0 = current use). The same dichotomy was created for worst past use. Individuals who reported either current use or past use were labeled as lifetime diet pill users. Further, the interviewer queried the type and brand of each diet pill used (i.e., ma huang, Dexatrim, etc.). Due to variability in brands used across countries and over time, we do not report on types of diet pills used. Although, we present the percentage of individuals who reported current diet pill use, we are interested in factors associated with ever using diet pills and therefore our analyses focus on the dichotomized variable of lifetime diet pill use. 1.2.4. Personality traits Temperament and character dimensions were measured with the Temperament and Character Inventory (TCI) (Cloninger, Przybeck, Svrakic, & Wetzel, 1994) which assesses four temperament dimensions (novelty seeking, harm Author's personal copy 76 L. Reba-Harrelson et al. / Eating Behaviors 9 (2008) 73–81 avoidance, reward dependence, and persistence) and three character dimensions (self-directedness, cooperativeness and self-transcendence) (Cloninger et al., 1994). 1.2.5. State-trait anxiety. Trait levels of anxiety were assessed with the State-Trait Anxiety Inventory (STAI Form Y-1) (Spielberger, Gorsuch, & Luchene, 1970). 1.2.6. Purging and other compensatory behaviors Vomiting, laxative use, emetic use, diuretic use, and excessive exercise were assessed with the SIAB (Fichter et al., 1998). 1.2.7. Tobacco and caffeine use. Tobacco use was assessed using the Fagerstrom Test for Nicotine Dependence (Fagerstrom, 1978). Caffeine use was assessed for all participants using screening interviews developed for each study. 1.2.8. Axis I and II psychiatric disorders Axis I mood and anxiety disorders were assessed with the SCID I (First, Spitzer et al. 1997). Cluster B and C personality disorders were assessed with the Structured Clinical Interview for DSM-IV personality disorders (SCID-II) (First, Gibbon, Spitzer, Williams, & Benjamin, 1997). 1.3. Statistical analyses All statistical analyses were conducted using SAS/STAT® 9.1 software (SAS Institute, 2004). To determine the prevalence of lifetime diet pill use in individuals with eating disorders across subtypes, chi-square tests were used to test between-group differences. Eating disorder subtypes included anorexia nervosa, restricting type (RAN), anorexia nervosa binging type (BAN), anorexia nervosa purging type (PAN), bulimia nervosa purging type (PBN), bulimia nervosa non-purging type (NPBN), anorexia nervosa and bulimia nervosa (ANBN), and eating disorder not-otherwisespecified (EDNOS). All subgroups met DSM-IV criteria for either AN (criterion D not required), BN or ED-NOS, and were further specified as follows: those with RAN did not binge eat or purge (i.e., engage in self-induced vomiting, laxative misuse, diuretic, emetic, or enema use), while those with BAN engaged in binge eating and/or purging. Those with PBN engaged in purging, while those in the NPBN group refrained from purging behavior. Individuals in the ANBN subgroup were categorized as having a lifetime diagnosis of both AN and BN. Individuals who did not meet full eating disorder criteria were grouped together in the eating disorder not-otherwisespecified category (EDNOS), including those with subthreshold AN or BN, or full-criterion purging disorder, defined by recurrent purging in the absence of objective binge episodes among normal weight individuals (Keel, Haedt, & Edler, 2005). In terms of demographic characteristics, we used analysis of variance (ANOVA) to examine differences across eating disorder subgroups. For all comparisons, statistical significance was set at an alpha level of 0.01. A series of multivariable logistic regression analyses were used to examine predictive relationships between diet pill use (coded present or absent) and a range of predictors. To determine the proportion of diet pill users in the analysis population, a multivariable Poisson regression using the population as the offset and the number of diet pill users as the response was used. In the first analysis, dichotomous variables lifetime self-induced vomiting, other purging behaviors (defined as laxative, diuretic, emetic use), excessive exercise, tobacco use, and caffeine use were used as predictors. In the second, the continuous variables trait anxiety and novelty seeking were included, whereas in the third model, presence or absence of Axis I and II disorders was entered as predictors. Age was included as a covariate in all of the analyses models to control for the effects of age on the lifetime prevalence of eating disorders; eating disorder subtype was included as a covariate in the latter two models. To determine the odds of diet pill use by BMI status (e.g., lowest, highest, or current BMI), we adjusted for eating disorder subtype and age. Each logistic regression model assigned diet pill use as a response and lowest, highest and current BMI status as covariates. Each parameter estimate corresponding to BMI status was adjusted by FDR adjustment (Benjamini & Hochberg, 1995). For logistic regression analyses using the BN-ARP data, we corrected for non-independence using Generalized Estimating Equations (GEE) (Diggle, Liang, & Zeger, 1994; Liang & Zeger, 1986; Zeger, Liang, & Albert, 1988). GEE is a statistical approach based on regression techniques that is used to investigate clustered data. In the current study, biologically related family members comprised each cluster in the GEE analyses. However, because our study included Author's personal copy L. Reba-Harrelson et al. / Eating Behaviors 9 (2008) 73–81 77 Table 1 Demographic characteristics by eating disorder subgroup Age at assessment Age of onset Lowest BMI Current BMIa Highest BMI Duration of illness RAN N = 319, M (SD) PAN N = 199, M (SD) BAN N = 123, M (SD) PBN N = 256, M (SD) NPBN N = 22, M (SD) ANBN N = 361, M (SD) EDNOS N = 65, M (SD) 24.97 (7.83) 16.28 (3.43) 13.79 (1.90) 17.99 (2.84) 21.05 (2.51) 7.33 (6.64) 26.47 (7.76) 16.25 (2.84) 14.15 (1.96) 18.34 (2.55) 21.43 (2.39) 9.29 (7.29) 27.93 (8.57) 16.64 (3.19) 13.72 (2.00) 18.30 (2.63) 21.17 (2.19) 9.76 (7.90) 27.55 (8.69) 17.59 (3.57) 19.35 (1.70) 22.76 (2.97) 25.52 (3.20) 8.27 (7.74) 28.64 (10.71) 19.55 (5.65) 19.25 (1.99) 22.09 (2.95) 25.97 (3.42) 7.90 (9.28) 28.96 (8.70) 17.08 (3.78) 15.06 (1.89) 19.90 (2.67) 23.14 (2.74) 10.49 (7.48) 27.09 (8.80) 17.29 (3.36) 19.01 (1.49) 21.94 (2.63) 24.18 (3.17) 6.60 (7.74) Note. RAN = Restricting type, Anorexia Nervosa; PAN = Purging type, Anorexia Nervosa; BAN = Binging type, Anorexia Nervosa; PBN = Purging type, Bulimia Nervosa; NPBN = Non-purging type, Bulimia Nervosa; ANBN = Anorexia Nervosa, Bulimia Nervosa; EDNOS = Eating Disorder Not-Otherwise-Specified. family members of varying relatedness (i.e., first, second, and third-degree relatives as well as unrelated controls), the GEE analyses were conducted in two steps. First, models were fit to the data via the GEE method for probands and their siblings only using the exchangeable working correlation matrix to obtain an estimate of the familial correlation among these first-degree relatives. Second, models were re-fit to the entire dataset of relatives using familial correlations estimated from the probands and siblings as the user-defined working correlation matrix. The model parameters and statistics from these models were then used as the final solution. This approach to the analyses can be considered conservative, as the proband/sibling correlations are likely overestimates of the expected correlations among clusters of unrelated individuals and second- and third-degree relatives. Such overestimation is likely to result in fewer, rather than more, significant findings. 2. Results 2.1. Descriptive statistics Demographic information for the entire sample is presented in Table 1. Current diet pill use was endorsed by 3.4% (N = 45) of the sample. Lifetime diet pill use was endorsed by 32.3% (N = 434) of the sample. 34 individuals, or 2.5% of the total sample, used diet pills alone (with no vomiting or other forms of purging). Fig. 1 presents the percentage of individuals who endorsed lifetime diet pill use by eating disorder subtype. Fig. 1. Age-adjusted rates of diet pill use across eating disorder subgroups. Author's personal copy 78 L. Reba-Harrelson et al. / Eating Behaviors 9 (2008) 73–81 Table 2 Results from logistic regression analysis (using GEE) predicting odds of diet pill use by vomiting, purging, excessive exercise, tobacco use, and caffeine use, adjusted for age at interview, and prevalence of diet pill use by presence and absence of behaviors Behavior % Diet pill users in those with behavior present % Diet pill users in those with behavior Chi-square ( p) (ndiet pill users / n awith behavior) absent (ndiet pill users / n awithout behavior) Vomiting 42.8% (363/848) Purging 49.7% (313/630) Excessive 34.7% (185/533) exercise Tobacco use 45.1% (139/308) Caffeine use 37.2% (360/967) OR (95% CI) 14.3% (71/496) 17.0% (120/707) 30.7% (249/812) 47.52 (<0.0001) 3.06 (2.23–4.21) 58.46 (<0.0001) 3.20 (2.39–4.28) 1.09 (0.30) 1.15 (0.88–1.50) 28.4% (295/1037) 19.1%(58/303) 5.14 (0.02) 1.43 (1.06–1.94) 21.63 (<0.0001) 2.17 (1.56–3.03) Total N's may differ due to missing data. In terms of odds of diet pill use by BMI status, odds of diet pill use were positively associated with all BMI measures— current (χ2 = 16.57, df = 1, p b 0.0001); highest (χ2 = 29.36, df = 1, p b 0.0001); and lowest (χ2 = 10.55, df = 1, p = 0.0012). The associations remained significant at an alpha level of 0.01 after the FDR. For the entire sample (N = 1345), mean current BMI was 19.74 (10.91–33.91), mean highest BMI was 22.76 (13.87–35.42), and mean lowest BMI was 15.58 (7.81–27.48). For one unit increase in current BMI there was a 10% increase in odds of diet pill use. For one unit increase in lifetime high BMI there was a 14% increase in odds of diet pill use. For one unit increase in lifetime low BMI there was a 12% increase in odds of diet pill use. The higher the BMI of a participant, the higher the odds of diet pill use, adjusting for age and ED type. Expected differences emerged across eating disorder subtypes. Significantly more individuals in the PAN, BAN, PBN, and ANBN subtypes reported diet pill use than individuals in the RAN subgroup. The highest prevalence of use was reported by individuals with PAN (41%), PBN (44%), and ANBN (42%). Age at interview (F(6,1344) = 6.96, p b .0001), age at onset of eating disorder (F(6,1344) = 6.95, p b .0001), lowest BMI (F(6,1344) = 319.10, p b .0001), current BMI (F(6,1344) = 96.28, p b .0001), highest BMI (F(6,1344) = 88.80, p b .0001), and duration of illness (F(6,1344) = 8.75, p b .0001) each differed significantly as a function of eating disorder subtype. 2.2. Logistic regression analyses Table 2 presents the odds of using diet pills in individuals who used other weight control behaviors, and who used licit substances (tobacco and caffeine), and reports the frequency with which individuals who did and did not exhibit Table 3 Results from logistic regression analyses (using GEE) predicting odds of diet pill use by Axis I and Axis II disorders, adjusted for eating disorder subtype and age at interview, and prevalence of diet pill use by presence and absence of disorders Variable % Diet pill users in those with behavior present (ndiet pill users / n awith behavior) % Diet pill users in those with behavior absent (ndiet pill users / n awithout behavior) Depression Any anxiety disorder Bipolar I Bipolar II Alcohol abuse or dependence Antisocial Personality Disorders (PD) Borderline PD Histrionic PD Narcissistic PD 34.9% (320/916) 36.6% (309/844) 25.1% (95/379) 24.7% (121/490) 3.36 (0.07) 7.24 (0.007) 1.38 (0.97–1.97) 1.47 (1.11–1.95) 50% (9/18) 54.5% (12/22) 46.8% (176/376) 31.9% (418/1309) 31.7% (412/1299) 26.3% (249/947) 0.41 (0.52) 1.02 (0.31) 6.86 (0.009) 1.40 (0.51–3.86) 1.76 (0.61–5.06) 1.53 (1.12–2.09) 70% (7/10) 32.2% (402/1248) 0.87 (0.35) 2.09 (0.43–10.09) 56.6% (77/136) 69.2% (9/13) 19% (4/21) 29.7% (333/1122) 32.2% (401/1246) 32.8% (406/1238) Total N's may differ due to missing data. Chi-square (p) 11.14 (0.0008) 2.73 (0.10) 5.09 (0.02) OR (CI) 2.18 (1.39–3.41) 3.24 (0.92–11.36) 0.28 (0.08–0.99) Author's personal copy L. Reba-Harrelson et al. / Eating Behaviors 9 (2008) 73–81 79 those behaviors reported diet pill use. All odd ratios were adjusted for age. Of all the demographic and weight control variables, significant differences were found for vomiting (χ2 = 47.53, df = 1, p b .0001), other types of purging (χ2 = 58.46, df = 1, p b .0001), and caffeine use (χ2 = 21.63, df = 1, p b 0.0001). Vomiting, other types of purging, and caffeine use were positively associated with the use of diet pills. Excessive exercise (χ2 = 1.09, df = 1, p = .30) was not significantly associated with diet pill use. Regarding odds of diet pill use by trait anxiety and novelty seeking, significant differences emerged for TCI novelty seeking (χ2 = 6.43, df = 1, p = .01), OR = 1.02 (95% CI = 1.01–1.02); and STAI trait anxiety (χ2 = 11.67, df = 1, p = 0.0006), OR = 1.02 (95% CI = 1.01–1.03). For a one unit increase in TCI novelty seeking, the odds of diet pill use increased by 2.3%. For a one unit increase in STAI trait anxiety, the odds of diet pill use increased by 1.6%. Higher scores on both trait anxiety and novelty seeking were associated with higher odds of diet pill use. Table 3 presents the odds of diet pill use by Axis I and Axis II disorders, and prevalence of diet pill use by the presence and absence of disorders. Positively associated with diet pill use were alcohol abuse or dependence (χ2 = 6.86, df = 1, p = 0.009); borderline personality disorder (BPD) (χ2 = 11.14, df = 1, p = .0008); and any anxiety disorder (χ2 = 7.24, df = 1, p = 0.007). The definition of any anxiety disorder included agoraphobia, generalized anxiety disorder, obsessive–compulsive disorder, panic disorder, post-traumatic stress disorder, social phobia, and specific phobia. 3. Discussion Diet pill use is a significant problem in individuals with eating disorders in the clinic, yet few studies have investigated their use comprehensively. The objective of this study was to determine the prevalence of diet pill use and explore features associated with their use in a large, well-characterized sample of individuals with eating disorders. We found the presence of diet pill use to be positively associated with other weight control behaviors (vomiting and other forms of purging), BMI, caffeine use, personality characteristics (trait anxiety, higher novelty seeking), and several Axis I and II disorders (any anxiety disorder, borderline personality disorder, alcohol abuse or dependence). Confirming our hypothesis, across eating disorder subtypes, significantly greater numbers of individuals in the PAN, BAN, PBN, and ANBN subtypes reported use of diet pills compared to individuals with RAN. Given that individuals with RAN are more likely to display high constraint characteristics than individuals with purging-type eating disorders (Casper, Hedeker, & McClough, 1992) and by definition do not engage in binge eating or purging behaviors, a lower frequency of diet pill use in those with RAN was predicted. Diet pill use was also associated positively with vomiting and other forms of purging. Although the relative rarity of use of diet pills as the sole weight control strategy in our sample was most likely an artifact of our inclusion and exclusion criteria, at least in this sample, diet pill use seems more typically to emerge as part of a constellation of weight control behaviors including purging behaviors rather than a solitary behavior. Moreover, as there was no significant relation between excessive exercise and diet pill use, diet pill use may best be conceptualized as clustered with other purging methods. In terms of BMI, diet pill use was positively associated with current, highest and lowest lifetime BMI. However, odds ratios explain that the higher an individual's BMI, the higher the odds of diet pill use, adjusting for age and eating disorder type. Given the strong association between diet pill use and highest maximum BMI, it is of note that diet pill use is more likely by individuals who are (or have been) normal weight or overweight than by those who are (or have been) underweight. This may suggest that diet pill use in not an effective weight loss strategy or means to keep weight down. Diet pill use was also associated positively with increased novelty seeking, borderline personality disorder, and alcohol abuse or dependence. This association may support the existence of an eating disorder subgroup that exhibits a cluster of impulsive, problematic behaviors. Previously described as “multi-impulsive,” these individuals with BN have been found to display poor response to treatment (Fichter et al., 1994) as well as other negative outcomes (Keel & Mitchell, 1997; Myers et al., 2006). The identification of diet pill use as another behavior that may characterize these individuals is important for further understanding the nature of eating pathology in this particularly severe subgroup of eating disorder patients. Interestingly, the same pattern of findings did not hold for narcissistic personality disorder. Although not significant at our alpha level of 0.01, a trend-level difference emerged ( p b 0.02) which was in the opposite direction of that observed for novelty seeking, borderline personality disorder, and alcohol abuse or dependence. Although this could be a chance finding, the fact that narcissistic personality disorder was associated with less diet pill use is intriguing and cautions against assuming that all cluster B personality disorders are similarly associated with diet pill usage. Author's personal copy 80 L. Reba-Harrelson et al. / Eating Behaviors 9 (2008) 73–81 Diet pill use was also associated with trait anxiety and anxiety disorders. Previous studies have shown that individuals with eating disorders who are impulsive also exhibit anxious traits (Cassin & von Ranson, 2005; Fichter et al., 1994). Within these populations, diet pill use together with the constellation of other substances and problematic behaviors may be impulsively driven responses to underlying anxiety about body weight and weight gain. It is noteworthy that diet pill use was not associated with major depression. This finding was contrary to our hypothesis but may be due to the fact that of the 916 individuals in the sample with major depressive disorder, 22% had a RAN diagnosis, and 29% had an ANBN diagnosis. Thus, the lack of an association between diet pill use and depression may be due to the fact that the highest frequencies of depression were in those who gravitated towards other weight control behaviors (e.g., excessive exercise). This study has the following limitations of note. The cross-sectional design necessitated retrospective reports which are susceptible to recall bias. Moreover, it is possible that our assessment of diet pill use may underestimate frequency of use. Self-report assessment has been shown to underestimate laxative use as compared to urine screening in individuals with AN (Turner, Batik, Palmer, Forbes, & McDermott, 2000). Further, in this study, diet pill use was assessed by interview and it is unknown whether structured interview reports are superior to self-report of diet pill use. Moreover, variability in our measurement of current and worst diet pill use, and diet pill brands, limited our focus to lifetime diet pill use. Finally, because part of the study sample (BN-ARP study) was collected for linkage analysis, targeting families with multiple affected individuals, ascertainment bias must be considered. Affected individuals who come from high density families may differ systematically from sporadic cases in ways we are unable to ascertain. In conclusion, diet pill use in individuals with eating disorders is associated with vomiting and other purging behavior, BMI, caffeine use, novelty seeking, trait anxiety, and other Axis I and II disorders (any anxiety disorder, borderline personality disorder, alcohol abuse or dependence,). Given the observed frequency of diet pill use in individuals with eating disorders, the unregulated nature of these substances, and the ease with which they can be obtained, assessment of diet pill use—including brand, source, and dosage, should be routine. Acknowledgements The author thanks the Price Foundation for the support of the clinical collection of participants and support of data analysis. The author acknowledges the staff of the Price Foundation Collaborative Group for their efforts in participant screening and clinical assessments. The author is indebted to the participating families for their contribution of time and effort in support of this study. This study was also supported by grant MH-66117 from the National Institutes of Health, Bethesda, MD. References American Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Washington, D.C.: American Psychiatric Association Press. Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B, 57, 289−300. Carek, P., & Dickerson, L. (1999). Current concepts in the pharmacological management of obesity. Drugs, 57, 883−904. Casper, R., Hedeker, D., & McClough, J. (1992). Personality dimensions in eating disorders and their relevance for subtyping. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 830−840. Cassin, S. E., & von Ranson, K. M. (2005). Personality and eating disorders: A decade in review. Clinical Psychology Review, 25, 895−916. Celio, C. I., Luce, K. H., Bryson, S. W., Winzelberg, A. J., Cunning, D., Rockwell, R., et al. (2006). Use of diet pills and other dieting aids in a college population with high weight and shape concerns. International Journal of Eating Disorders, 39, 492−497. Cloninger, C. R., Przybeck, T. R., Svrakic, D. M., & Wetzel, R. D. (1994). The Temperament and Character Inventory (TCI): A Guide to its development and use. St. Louis, MO: Center for Psychobiology of Personality. Washington University. Dietz Jr, A. J. (1981). Amphetamine-like reactions to phenylpropanolamine. Journal of the American Medical Association, 245, 601−602. Diggle, P., Liang, K., & Zeger, S. (1994). Analysis of longitudinal data. Oxford: Oxford Science. Eckert, E. D., Halmi, K. A., Marchi, P., Grove, W., & Crosby, R. (1995). Ten-year follow-up of anorexia nervosa: clinical course and outcome. Psychological Medicine, 25, 143−156. Eddy, K., Keel, P., Dorer, D., Delinsky, S., Franko, D., & Herzog, D. (2002). Longitudinal comparison of anorexia nervosa subtypes. International Journal of Eating Disorders, 31, 191−201. Fagerstrom, K. -O. (1978). Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addictive Behaviors, 3, 235−241. Fichter, M. M., Herpertz, S., Quadflieg, N., & Herpertz-Dahlmann, B. (1998). Structured interview for anorexic and bulimic disorders for DSM-IV and ICD-10: updated (third) revision. International Journal of Eating Disorders, 24, 227−249. Author's personal copy L. Reba-Harrelson et al. / Eating Behaviors 9 (2008) 73–81 81 Fichter, M. M., Quadflieg, N., & Rief, W. (1994). Course of multi-impulsive bulimia. Psychological Medicine, 24, 591−604. First, M. B., Gibbon, M., Spitzer, R. L., Williams, J. B. M., & Benjamin, L. S. (1997). Structured Clinical Interview for DSM-IV Axis-II Personality Disorders (SCID-II). New York: Biometrics Research, New York State Psychiatric Institute. First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (1997). Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition. New York: Biometrics Research, New York State Psychiatric Institute. Hebebrand, J., Himmelmann, G. W., Heseker, H., Schafer, H., & Remschmidt, H. (1996). Use of percentiles for the body mass index in anorexia nervosa: Diagnostic, epidemiological, and therapeutic considerations. International Journal of Eating Disorders, 19, 359−369. Kaplan, A., & Olmsted, M. P. (1997). Partial hospitalization. In D. M. Garner & P. F. Garfinkel (Eds.), Handbook of Treatment for Eating Disorders. London: Guilford. Kaye, W. H., Devlin, B., Barbarich, N., Bulik, C. M., Thornton, L., Bacanu, S. A., et al. (2004). Genetic analysis of bulimia nervosa: Methods and sample description. International Journal of Eating Disorders, 35, 556−570. Keel, P. K., Haedt, A., & Edler, C. (2005). Purging disorder: An ominous variant of bulimia nervosa? The International Journal Of Eating Disorders, 38, 191−199. Keel, P. K., & Mitchell, J. E. (1997). Outcome in bulimia nervosa. American Journal of Psychiatry, 154, 313−321. Klump, K. L., Bulik, C. M., Pollice, C., Halmi, K. A., Fichter, M. M., Berrettini, W. H., et al. (2000). Temperament and character in women with anorexia nervosa. Journal of Nervous Mental Disorders, 188, 559−567. Liang, K. Y., & Zeger, S. L. (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73, 13−22. Mitchell, J. E., Pomeroy, C., & Huber, M. (1988). A clinician's guide to the eating disorders medicine cabinet. International Journal of Eating Disorders, 7, 211−223. Myers, T. C., Wonderlich, S. A., Crosby, R., Mitchell, J. E., Steffen, K. J., Smyth, J., et al. (2006). Is multi-impulsive bulimia a distinct type of bulimia nervosa: Psychopathology and EMA findings. International Journal of Eating Disorders, 39, 655−661. Reba, L., Thornton, L., Tozzi, F., Klump, K. L., Brandt, H., Crawford, S., et al. (2005). Relationships between features associated with vomiting in purging-type eating disorders. International Journal of Eating Disorders, 38, 287−294. Roerig, J. L., Mitchell, J. E., de Zwaan, M., Wonderlich, S. E., Kamran, S., Engbloom, S., et al. (2003). The eating disorders medicine cabinet revisited: A clinician's guide to appetite suppressants and diuretics. International Journal of Eating Disorders, 33, 443−457. SAS Institute, I. (2004). SAS (Version 9.1.3). Cary, NC: SAS Institute Inc. Shekelle, P., Morton, S. C., & Maglione, M. (2003). Ephedra and ephedrine for weight loss and athletic performance enhancement: Clinical efficacy and side effects. Evidence Report/Technology Assessment, Vol. 76. Rockville, MD: Agency for Healthcare Research and Quality. Spielberger, C. D., Gorsuch, R. L., & Luchene, R. E. (1970). STAI Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press. Steffen, K. J., Roerig, J. L., Mitchell, J. E., & Crosby, R. D. (2006). A survey of herbal and alternative medication use among participants with eating disorder symptoms. International Journal of Eating Disorders, 39, 741−746. Strober, M., Freeman, R., & Morrell, W. (1997). The long-term course of severe anorexia nervosa in adolescents: Survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. International Journal of Eating Disorders, 22, 339−360. Tozzi, F., Thornton, L. M., Klump, K. L., Fichter, K. M., Halmi, K. A., Kaplan, A. S., et al. (2005). Symptom fluctuation in eating disorders: Correlates of diagnostic crossover. American Journal of Psychiatry, 162, 732−740. Turner, J., Batik, M., Palmer, L. J., Forbes, D., & McDermott, B. M. (2000). Detection and importance of laxative use in adolescents with anorexia nervosa. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 378−385. Zeger, S. L., Liang, K. Y., & Albert, P. S. (1988). Models for longitudinal data: A generalized estimating equation approach. Biometrics, 44, 1049−1060.