Positron emission tomography studies in eating disorders:
advertisement

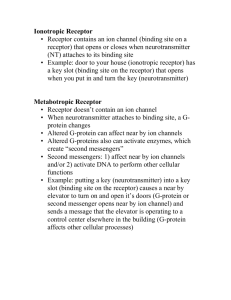
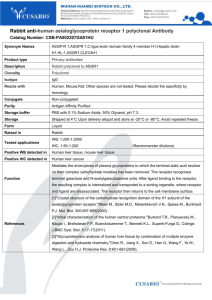
Nuclear Medicine and Biology 32 (2005) 755 – 761 www.elsevier.com/locate/nucmedbio Positron emission tomography studies in eating disorders: multireceptor brain imaging, correlates with behavior and implications for pharmacotherapyB Guido K. Franka, Walter H. Kayeb,T a Department of Child and Adolescent Psychiatry, Center for Eating Disorders Research, School of Medicine, University of California San Diego, San Diego, CA 92123, USA b Department of Psychiatry, Western Psychiatric Institute and Clinic, School of Medicine, University of Pittsburgh, Pittsburgh, PA 15213, USA Received 6 June 2005; accepted 6 June 2005 Abstract Modern imaging techniques that visualize disease-specific organ neurotransmitter or protein receptor sites are increasingly able to define pathological processes on a molecular level. One of those imaging modalities, positron emission tomography (PET), for the assessment of brain neuroreceptor binding has revolutionized the in vivo assessment of biologic markers that may be related to human behavior. Such studies may help identify chemical targets that may be directly related to psychiatric pathology and, thus, opportunities for pharmacological intervention. In this review, we describe results from PET studies in eating disorders (EDs). Eating disorders are frequently debilitating illnesses that are quite homogeneous in their presentation. Those studies that identified particular serotonin and dopamine receptor alterations can distinguish recovered ED subjects from controls as well as ED subgroups. Furthermore, correlations of receptor binding with behavioral constructs, such as harm avoidance or novelty seeking, could be found. These recognized receptors may now help us to move away from rather nonspecific treatment approaches in psychiatric research and clinic to the possibility of more syndrome- and symptom-specific treatment approaches. D 2005 Elsevier Inc. All rights reserved. Keywords: Receptor; Imaging; Serotonin; Dopamine; Positron emission tomography; Eating disorder 1. Introduction Molecular imaging, which is the visualization of molecular information that is pertinent to a specific disease, has been receiving increasing attention [1]. Using advanced neuroimaging techniques such as positron emission tomography (PET) and single photon emission tomography (SPECT), disorders such as depression, schizophrenia or eating disorders (EDs) can now be studied on the level of receptors that are involved in regional brain neurotransmission. Those receptors may be related to depressive feelings and anxiety, agitation or changes in the ability to eat or sleep. B This study was supported by NIMH MH46001, MH42984, K05MD01894 and T32-MH18399. T Corresponding author. Tel.: +1 412 647 9845; fax: +1 412 647 9740. 0969-8051/$ – see front matter D 2005 Elsevier Inc. All rights reserved. doi:10.1016/j.nucmedbio.2005.06.011 Similar to other psychiatric disorders, the conceptual framework of the pathophysiology and etiology of the EDs has undergone significant changes in the past decades with the advent of modern neuroscience research. The etiology of EDs is still unknown. However, several lines of research have raised the possibility that trait disturbances of brain neurotransmitters may contribute to the pathogenesis of ED. These neurotransmitter systems include serotonin and dopamine pathways as well as a number of neuropeptides [2]. A major reason for our lack of understanding of brain and behavior in the past was that tools for measuring neurotransmitter activity and brain pathways have been limited to indirect measures of brain function such as concentrations of neurotransmitters in cerebrospinal fluid (CSF) or hormonal responses to drug challenges. Brain imaging techniques now give us the opportunity to assess regional brain activity and neuroreceptor function in vivo in humans and, thus, may help us understand how neuronal circuits are related to behavior and pathophysiology. 756 G.K. Frank, W.H. Kaye / Nuclear Medicine and Biology 32 (2005) 755 – 761 Table 1 Summary of PET findings in EDs using serotonin and dopamine ligands Author Imaging technology Frank et al. [7] Audenaert et al. [6] Bailer et al. [8] Goethals et al. [39] Kaye et al. [16] Bailer et al. [40] Bailer et al. [40] Henry et al., submitted for publication Tiihonen et al. [20] Tauscher et al. [21] Bailer et al., submitted for publication Bailer et al., submitted for publication Frank et al. [13] PET 5-HT2A SPECT 5-HT2A PET 5-HT2A SPECT 5-HT2A PET 5-HT2A PET 5-HT1A PET 5-HT1A PET 5-HT1A Recovered subjects n Frontal cortex Cingulate cortex Mesial temporal cortex Parietal cortex AN nl A nl nl A nl z z A A nl nl nl z z A nl A nl nl nl z z nl BN AN AN-BN BN 16 15 10 10 9 13 12 10 A nl nl nl z z z z nl nl AN-BN 8 10 5 PET 5-HTT BN 8 nl PET DA D2/D3 AN, AN-BN 10 PET 5-HT1A SPECT 5-HTT PET 5-HTT Ill subjects AN AN-BN BN BN BN An example of visualization of now commonly studied pre- and postsynaptic neuroreceptors in the living human brain with specific radioligands is shown in Fig. 1. Those studies open the opportunity to develop disease-specific targets for pharmacological intervention. In this review, we show evidence that we can start to bridge the gap between basic research and applied human behavioral research. This involves the comprehensive study of receptor systems in healthy controls and psychiatric disorders, and the A Basal ganglia Midbrain raphe A A A z development of maps of normal and pathological neuroreceptor distribution. 2. Anorexia nervosa Anorerxia nervosa (AN) is a disorder that usually begins during adolescence in females and is associated with an intense fear of gaining weight, feeling fat, emaciation and amenorrhea. There are thought to be two Fig. 1. Available receptors for PET imaging. Note the different receptor distribution for various receptor types: serotonin 5-HT1A receptor with presynaptic binding in the midbrain raphe nuclei and cortical post synaptic binding; 5-HT2A receptor binding that is exclusively postsynaptic; 5-HTT with mid brain, cortical and basal ganglia presynaptic binding; dopamine D2/D3 receptor binding localized in the basal ganglia. [11C] and [18F] radiopharmaceuticals indicate receptor-specific ligand types. G.K. Frank, W.H. Kaye / Nuclear Medicine and Biology 32 (2005) 755 – 761 subtypes: restricting type AN (AN-R) and binge-eating/ purging AN (AN-B/P) [3]. Comorbid obsessive–compulsive disorder (OCD) is common, as are depression and anxiety [4]. Neurotransmitters such as serotonin or dopamine are distributed throughout the brain via specific neuronal pathways. Their influence on behavior is believed to be through action on specific receptors that tend to be located postsynaptically and, for some receptor types, also presynaptically in regions such as the midbrain. Radioligands exist for several of the serotonin receptor types. One of the most commonly assessed receptor type is the 5-HT2A receptor frequently studied using [18F]altanserin binding. This receptor type is involved in the regulation of feeding, mood and anxiety, and in antidepressant action [5]. Three studies have assessed 5-HT2A receptor binding in ill and recovered AN women. Ill subjects [6] showed reduced receptor binding in the left frontal, bilateral parietal and occipital cortex. Recovered AN-R [7] subjects also had reduced [18F]altanserin binding, most strongly in mesial temporal and parietal cortical areas as well as in the cingulate cortex. In another study, women recovered from AN-B/P had reduced [18F]altanserin binding relative to controls in the left subgenual cingulate, left parietal and right occipital cortex [8]. In that study, 5-HT2A binding was positively related to harm avoidance and negatively to novelty seeking in cingulate and temporal regions, with negative relationships between 5-HT2A binding and drive for thinness. Recent studies have been assessing the 5-HT1A receptor with [11C]WAY100635 as the radiotracer in AN and bulimia nervosa (BN). Recovered AN-B/P subjects had significantly increased [11C]WAY100635 binding in cingulate, lateral and 757 mesial temporal, lateral and medial orbital frontal, parietal and prefrontal cortical regions and in the dorsal raphe compared to control women [8]. No differences were found for recovered AN-R subjects relative to controls. For AN-R, the increased [11C]WAY100635 postsynaptic receptor binding in mesial temporal and subgenual cingulate regions was positively correlated with harm avoidance. Those findings (Table 1) now suggest that AN subgroups may be identified by assessing 5-HT1A and 5-HT2A receptor binding. Furthermore, those findings highlight the possibility of disturbances of the anterior cingulate cortex and mesial temporal cortex in AN. Since these disturbances persist after recovery, it is possible they are trait disturbances. The anterior cingulate cortex receives afferents from the amygdala and has direct projections to the premotor frontal cortex and other limbic regions. It plays a crucial role in initiation, motivation and goal-directed behaviors [9], as well as reward [10]. The amygdala mediates the interpretation of fear and the representation of emotional stimuli values [11]. It is possible that AN have disturbed processing of emotional stimuli valence, resulting in poor flexibility in reevaluating actual danger of those stimuli and reduced adaptation to new situations. Future studies will need to determine whether relationships between 5-HT2A and 5-HT1A receptor activity and measures for anxiety such as harm avoidance can be replicated. This could be an exciting avenue for the link of neurochemistry and behavior. The implication of such findings may be tremendous. If it is possible to reliably identify a network of neurotransmission that is involved in an aspect of anxious response to stimuli, which is an integral part of a disease process, then pathological behavioral response Fig. 2. Exemplary increased [11C]raclopride binding in an anorexic woman compared to an age-matched control woman [13]. 758 G.K. Frank, W.H. Kaye / Nuclear Medicine and Biology 32 (2005) 755 – 761 might be specifically intervened with, for instance, a particular receptor agonist or antagonist. Imaging techniques such as PET may help to assess drug–neuroreceptor binding in relation to treatment response. The dopamine (DA) receptor system has received some attention in the past regarding its involvement in the pathophysiology of AN with one study [12], showing low CSF levels of the DA metabolite homovanillic acid (HVA). Most recently, we found in a group of subjects who recovered from both AN-R and AN-B/P an increased DA D2/D3 receptor binding in the anteroventral striatum, which includes the nucleus accumbens, an area involved in reward and learning [13] (Fig 2). 5-HT and DA neurotransmission is closely intertwined, and future in vivo studies will have to assess behavioral consequences of receptor expression and the interaction of various receptor systems. 5-HT and DA receptor activation may act on other central neurotransmitter systems such as glutamatergic neurotransmission via the NMDA receptor [14].Thus, there is a variety of possible implications of 5-HT and DA receptor alterations. The DA system has been receiving increased attention in addiction as well as obesity research. It might be possible that AN and subjects with various forms of addictive behaviors are at opposite extremes, and the study of chemical pathways that are involved could give us clues for intervention research. Most available therapeutic drugs in psychiatry are acting on several receptor types or are somewhat nonspecific, such as reuptake inhibitors. With the new knowledge about disorder-specific disturbances, it will eventually be possible to develop more specific drugs for intervention. That includes development of more substances that bind more specifically to particular receptor sites guided by neuroimaging, as well as assessment of central receptor availability prior to, during and after treatment. 3. Bulimia nervosa Bulimia nervosa is characterized by recurrent binge eating followed by behaviors to counteract weight gain, such as self-induced vomiting. Individuals with BN often maintain a normal weight but present with a fear of gaining weight and food and body weight-related preoccupations. Bulimia nervosa is usually associated with increased depressive and anxious feelings. Impulsive behaviors and cluster B behaviors are common [3]. The 5-HT system has consistently been shown to be disturbed in BN as well as in AN [15]. However, BN, after recovery, had higher CSF 5-HT metabolite 5-hydroxyindoleacetic acid (5-HIAA) compared to AN after recovery, and during the ill phase, BN CSF 5-HIAA was inversely correlated with bingeeating/purging episode frequency. Serotonin receptor alterations may have specific implications on behavior. Kaye et al. [16] found reduced orbitofrontal 5-HT2A receptor binding in recovered BN. Orbitofrontal alterations could reflect behavioral disturbances in BN that include impulsiveness and altered emotional processing [17]. Altered orbitofrontal activity, as found in borderline personality disorder [18], could indicate a common area for impulse control disturbance. In addition, BN women failed to show common correlations of age and 5-HT2A binding. This finding raises the possibility that BN women may have alterations of developmental mechanisms of the 5-HT system. Reduced 5-HT2A activity after recovery could reflect a trait disturbance involved in alterations of mood, anxiety and impulse control. 5-HT receptor imaging before and during active drug treatment may now help shed light on the question why BN subjects need higher doses of SSRIs compared to depressed subjects [19]. In contrast to reduced 5-HT2A binding in BN, increased 5-HT1A receptor binding in ill BN subjects was reported by Tiihonen et al. [20] using PET in all studied brain regions, but most prominently in prefrontal, cingulate and a parietal cortex area. Data from our own group support those findings with generalized increased postsynaptic 5-HT1A binding in recovered BN subjects (Henry at al submitted). Furthermore, the finding of increased 5-HT1A binding in recovered bulimic type AN [8] suggest that increased 5-HT1A binding might be a trait disturbance for bulimic type ED disturbance, but not for restrictor type AN (Table 1). Other studies have found reduced 5-HT transporter (5-HTT) [21] binding in thalamus and hypothalamus in ill BN. Bailer et al. [8] found reduced 5-HTT binding in recovered AN-B/P in raphe and mesial temporal regions, but normal 5-HTT binding in recovered BN subjects. Recent studies [22,23] using platelet 5-HTT binding raise the possibility that disturbed 5-HTT function may be related to mood instability or failure to respond to SSRIs in BN subjects. Thus, although it is likely that a 5-HTT alteration occurs in bulimia, the exact nature of this dysfunction remains uncertain. Still, it is likely that with a comprehensive biological assessment that includes neuroreceptor imaging, genotype and assessment of the drug-metabolizing P450 liver enzyme system, it will be possible to determine prior to treatment drug response likelihood and chance for experiencing of significant side effects. 4. Healthy subjects Many studies have found that CSF levels of 5-HIAA are inversely related to impulsivity and aggression in humans and nonhuman primates [24,25]. Thus, high concentrations of CSF 5-HIAA, which can be assumed to reflect increased extracellular 5-HT, are associated with inhibited behaviors in nonhuman primates, whereas low concentrations of CSF 5-HIAA are associated with impulsive temperament in man and monkey. Recently, brain imaging studies have found negative relationships among 5-HT1A receptor binding and aggression [26], selftranscendence [27] and anxiety [21] in frontal, temporal and cingulate cortical regions. Our group (Kaye, submitted for publication) has replicated these studies by finding that frontal, cingulate and temporal postsynaptic and brainstem G.K. Frank, W.H. Kaye / Nuclear Medicine and Biology 32 (2005) 755 – 761 11 autoreceptor raphe [ C]WAY100635 binding potential was significantly and inversely related to novelty seeking and self-transcendence in healthy control women. Little is known about the relationship between CSF 5-HIAA levels and 5-HT1A receptors. Nevertheless, it would make sense to assume that increased extracellular 5-HT would synergistically interact with 5-HT1A receptor activity. These accumulating data raise the question of whether increased 5-HT1A binding is related to some phenomenon common to novelty seeking, aggression and self-transcendence. One possibility is that each of these symptoms reflects some aspect of behavioral inhibition and self-control. These findings may shed light on temperament and personality. That is, people with increased 5-HT1A receptor function tend to be more inhibited and restrained, whereas people with low levels of 5-HT1A receptor function tend to be more stimuli seeking and uninhibited. 5. Implications Imaging of molecular targets that are involved in disease is a rapidly growing field with a wide range of applications from cancer, to joint disease and to psychiatric disorders [1]. Positron emission tomography imaging of 5-HT and DA as well as other targets has enormous potential for understanding how medication works in the brain of humans with psychiatric disorders. In the past, treatment has tended to be empirical because there have been no methods of predicting which drug to use or what dose to choose, or an understanding why some people do not respond to a medication. Positron emission tomography imaging with these radioligand tools has begun to be used to understand medication response, for example, 5-HTT transporter function after SSRI blockade, or effects of atypical antipsychotic drugs on dopamine and 5-HT receptors [28-30]. Receptor occupancy varies significantly across various compounds at the clinically recommended doses, and the treatment effect in relation to binding has yet to be determined in may cases [31]. Nevertheless, many pharmaceutical companies have recognized opportunities to understand the effects of available drugs, as well as test the effects of new compounds using external imaging [32,33]. As an example, SSRI medications are not effective when AN patients are malnourished and underweight, and have limited efficacy in BN. SSRIs block 5-HTT-mediated reuptake of 5-HT in the synapse, which results in increased extracellular 5-HT, which in turn gradually desensitizes and possibly down-regulates the 5-HT1A autoreceptor [34]. It is not known whether some individuals fail to respond to SSRIs because of aberrant 5-HTT function and/or some inability to desensitize highly elevated somatic dendritic 5HT1A autoreceptor activity. Moreover, it is not known whether SSRI effects on specific postsynaptic 5-HT1A and 5-HT2A receptor activity in frontal, cingulate and temporal regions are associated with specific symptom reduction such as less harm avoidance. However, one study suggests 759 that treatment with the SSRI paroxetine may reduce harm avoidance scores in a group of generalized anxiety disorder patients [35]. Positron emission tomography imaging with radioligands now provides a tool capable of answering questions for the research community together with the pharmaceutical industry regarding mechanisms that are part of the disease process as well as therapeutic intervention with psychotropic drugs. In addition, it is possible that such imaging tools may also prove to be useful in the near future as a clinical tool for understanding why some individuals with depression or schizophrenia are not responsive to medication. That is, in some individuals, PET imaging with radioligands could determine whether such people have abnormal 5-HTT or 5-HT1A function, which in turn might help the treating physician to use alternative treatment options. It is worthwhile noting that conventional methods of characterizing pathological behavior [e.g., using the Diagnostic and Statistical Manual of Mental Disorders (DSM-VITR) [36] are based on relatively broad clinical syndromes, such as depression. In fact, it is possible that depressed mood is related to disturbances of brain neurocircuits modulating mood, and there may be many different causes of depression, each related to a different loci of pathology within these neurocircuits. Moreover, the way the brain encodes behavior may not reflect conventional diagnosis, for example, as described above, relationships between 5-HT1A receptors and impulse control, which is found in both healthy subjects and people with EDs. Positron emission tomography imaging with radioligands offers the opportunity to understand relationships between receptors, circuits and behavior. Few studies have been done in EDs in comparison to depressive disorders or OCD. The overlap and comorbidity of both major depression and OCD with EDs require studies that will directly compare those disorders. Studies comparing psychiatric disorders will help to find common pathways and distinct areas of disturbance that may identify targets for successful drug interventions. It is important to note that neuronal activity is an integration of many factors such as neuronal firing, synaptic transmitter release and reuptake, metabolism of neurotransmitters, receptor sensitivity, second messenger systems and other intracellular mechanisms, and the relationship with other neuronal pathways. Positron emission tomography neuroimaging with radioligands offers the opportunities to understand the complexities and interactions of these components in vivo. It may be that the pattern of dysfunction of components making up 5-HT functional activity is different in ED, anxiety disorders and depression, although the end result is a compromise of 5-HT functional activity that may share common symptoms. In fact, subjects with major depression had reduced 5-HT1A receptor binding [37] as did a group of panic disorder patients [38], whereas our studies suggest increased 5-HT1A binding in, for instance, bulimic ED subjects who have frequent comorbid depression or anxiety disorders. 760 G.K. Frank, W.H. Kaye / Nuclear Medicine and Biology 32 (2005) 755 – 761 6. Conclusion The emergence of brain imaging techniques raises the possibility to assess brain function in vivo and assess human behavior in conjunction with biological correlates. The EDs AN and BN are relatively homogeneous disorders on one hand but with high comorbidity of affective and anxiety disorders on the other hand. This offers the opportunity to study the expression of various pathologies and their relationship with biologic pathology. The systematic research of neurotransmitter systems, such as the 5-HT and DA pathways, led to the successful identification of ED subtypes on a biologic basis and may now offer targets for the development of disease and symptom-specific pharmacological treatment. We expect that those new imaging methods give hope to the prospect of identifying biologic markers across the psychiatric spectrum. Psychiatric disorders can be viewed within the medical chronic disease model. New imaging techniques define what changes during the ill state persist after recovery and how pharmaceuticals may be able to intervene in the disease process and for relapse prevention in terms of receptor binding and associated behavior change. Improving the available pharmacological intervention strategies will greatly improve quality of life of the affected individuals. Acknowledgments We thank Roxanne Rockwell for her editorial assistance. References [1] Jaffer FA, Weissleder R. Molecular imaging in the clinical arena. JAMA 2005;293:855 – 62. [2] Kaye WH, Klump KL, Frank GK, Strober M. Anorexia and bulimia nervosa. Annu Rev Med 2000;51:299 – 313. [3] Task Force on DSM-IV APA M. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (Text Revision). Washington, DC (USA)7 American Psychiatric Press; 1994. [4] Bulik CM, Sullivan PF, Fear JL, Joyce PR. Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatr Scand 1997;96:101 – 7. [5] Barnes NM, Sharp T. A review of central 5-HT receptors and their function. Neuropharmacology 1999;38:1083 – 152. [6] Audenaert K, Van Laere K, Dumont F, et al. Decreased 5-HT2a receptor binding in patients with anorexia nervosa. J Nucl Med 2003;44:163 – 9. [7] Frank GK, Kaye WH, Meltzer CC, et al. Reduced 5-HT2A receptor binding after recovery from anorexia nervosa. Biol Psychiatry 2002;52:896 – 906. [8] Bailer U, Price JC, Meltzer CC, et al. Altered 5-HT2A receptor activity after recovery from bulimia-type anorexia nervosa: relationships to harm avoidance and drive for thinness. Neuropsychopharmacology 2004;29:1143 – 55. [9] Devinsky O, Morrell M, Vogt B. Contributions of anterior cingulate cortex to behaviour. Brain 1995;118:279 – 306. [10] Richmond B, Liu Z, Shidara M. Neuroscience. Predicting future rewards. Science 2003;301:180 – 9. [11] LeDoux J. The emotional brain, fear, and the amygdala. Cell Mol Neurobiol 2003;23:727 – 38. [12] Kaye WH, Frank GK, McConaha C. Altered dopamine activity after recovery from restricting-type anorexia nervosa. Neuropsychopharmacology 1999;21:503 – 6. [13] Frank G, Bailer U, Henry S, et al. Increased dopamine D2/D3 receptor binding after recovery from anorexia nervosa measured by positron emission tomography and [11C]raclopride. Biol Psychiatr 2005;Jun 28 [epub ahead of print]. [14] Carlsson ML, Martin P, Nilsson M, et al. The 5-HT2A receptor antagonist M100907 is more effective in counteracting NMDA antagonist- than dopamine agonist-induced hyperactivity in mice. J Neural Transm 1999;106:123 – 9. [15] Jimerson DC, Lesem MD, Kaye WH, Brewerton TD. Low serotonin and dopamine metabolite concentrations in cerebrospinal fluid from bulimic patients with frequent binge episodes. Arch Gen Psychiatry 1992;49:132 – 8. [16] Kaye WH, Frank GK, Meltzer CC, et al. Altered serotonin 2A receptor activity in women who have recovered from bulimia nervosa. Am J Psychiatry 2001;158:1152 – 5. [17] Steiger H, Young SN, Kin NM, et al. Implications of impulsive and affective symptoms for serotonin function in bulimia nervosa. Psychol Med 2001;31:85 – 95. [18] Soloff PH, Meltzer CC, Becker C, Greer PJ, Kelly TM, Constantine D. Impulsivity and prefrontal hypometabolism in borderline personality disorder. Psychiatry Res 2003;123:153 – 63. [19] Fluoxetine in the treatment of bulimia nervosa. A multicenter, placebo-controlled, double-blind trial. Fluoxetine Bulimia Nervosa Collaborative Study Group. Arch Gen Psychiatry 1992;49:139 – 47. [20] Tiihonen J, Keski-Rahkonen A, Lopponen M, et al. Brain serotonin 1A receptor binding in bulimia nervosa. Biol Psychiatry 2004;55:871 – 873. [21] Tauscher J, Pirker W, Willeit M, et al. [123I] beta-CIT and single photon emission computed tomography reveal reduced brain serotonin transporter availability in bulimia nervosa. Biol Psychiatry 2001;49:326 – 32. [22] Gorwood P. Eating disorders, serotonin transporter polymorphisms and potential treatment response. Am J Pharmacogenomics 2004;4:9 – 17. [23] Steiger H, Richardson J, Israel M, et al. Reduced density of plateletbinding sites for [3H]paroxetine in remitted bulimic women. Neuropsychopharmacology 2005;30:1028 – 32. [24] Fairbanks LA, Melega WP, Jorgensen MJ, Kaplan JR, McGuire MT. Social impulsivity inversely associated with CSF 5-HIAA and fluoxetine exposure in vervet monkeys. Neuropsychopharmacology 2001;24:370 – 8. [25] Westergaard GC, Cleveland A, Trenkle MK, Lussier ID, Higley JD. CSF 5-HIAA concentration as an early screening tool for predicting significant life history outcomes in female specific-pathogen-free (SPF) rhesus macaques (Macaca mulatta) maintained in captive breeding groups. J Med Primatol 2003;32:95 – 104. [26] Parsey RV, Oquendo MA, Simpson NR, et al. Effects of sex, age, and aggressive traits in man on brain serotonin 5-HT1A receptor binding potential measured by PET using [C-11]WAY-100635. Brain Res 2002;954:173 – 82. [27] Borg J, Andree B, Soderstrom H, Farde L. The serotonin system and spiritual experiences. Am J Psychiatry 2003;160:1965 – 9. [28] Meltzer CC, Price JC, Mathis CA, et al. Serotonin 1A receptor binding and treatment response in late-life depression. Neuropsychopharmacology 2004;29:2258 – 65. [29] Moresco RM, Cavallaro R, Messa C, et al. Cerebral D2 and 5-HT2 receptor occupancy in Schizophrenic patients treated with olanzapine or clozapine. J Psychopharmacol 2004;18:355 – 65. [30] Rabiner EA, Bhagwagar Z, Gunn RN, Cowen PJ, Grasby PM. Preferential 5-HT1A autoreceptor occupancy by pindolol is attenuated in depressed patients: effect of treatment or an endophenotype of depression? Neuropsychopharmacology 2004;29:1688 – 98. [31] Talbot PS, Laruelle M. The role of in vivo molecular imaging with PET and SPECT in the elucidation of psychiatric drug action and new drug development. Eur Neuropsychopharmacol 2002;12:503 – 11. G.K. Frank, W.H. Kaye / Nuclear Medicine and Biology 32 (2005) 755 – 761 [32] Mamo D, Kapur S, Shammi CM, et al. A PET study of dopamine D2 and serotonin 5-HT2 receptor occupancy in patients with schizophrenia treated with therapeutic doses of ziprasidone. Am J Psychiatry 2004;161:818 – 25. [33] Tauscher J, Kapur S, Verhoeff NP, et al. Brain serotonin 5-HT(1A) receptor binding in schizophrenia measured by positron emission tomography and [11C]WAY-100635. Arch Gen Psychiatry 2002;59: 514 – 20. [34] Riad M, Watkins KC, Doucet E, Hamon M, Descarries L. Agonistinduced internalization of serotonin-1a receptors in the dorsal raphe nucleus (autoreceptors) but not hippocampus (heteroreceptors). J Neurosci 2001;21:8378 – 86. [35] Allgulander C, Cloninger CR, Przybeck TR, Brandt L. Changes on the Temperament and Character Inventory after paroxetine treatment in volunteers with generalized anxiety disorder. Psychopharmacol Bull 1998;34:165 – 6. 761 [36] APA. Diagnostic & Statistical Manual of Mental Disorders: DSM-VITR. Washington, DC7 American Psychiatric Association; 2000. [37] Bhagwagar Z, Rabiner EA, Sargent PA, Grasby PM, Cowen PJ. Persistent reduction in brain serotonin1A receptor binding in recovered depressed men measured by positron emission tomography with [11C]WAY-100635. Mol Psychiatry 2004;9:386 – 92. [38] Neumeister A, Bain E, Nugent AC, et al. Reduced serotonin type 1A receptor binding in panic disorder. J Neurosci 2004;24:589 – 91. [39] Goethals I, Vervaet M, Avdenaert K, Van de Wiek C, Ham H, Vandecapelle M, et al. Comparison of cortical 5-HT2A receptor binding in bulimia nervous patients and healthy volunteers. Am J Psychiatr 2004;161:1916 – 8. [40] Bailer VF, Frank GK, Henry SE, Price JC, Meltzer CC, Weissfeld L, et al. Altered brain serotonin 5-HT1A receptor binding after recovery from anorexia nervosa measured by positron emission tomography and [CarbonyIIIC] WAY-100635. Arch Gen Psychiatr 2005;62:1032 – 41.