Reduced 5-HT2A Receptor Binding after Recovery from Anorexia Nervosa
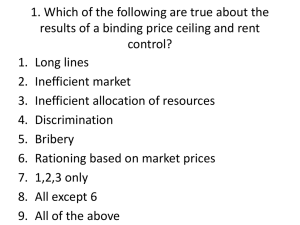
advertisement

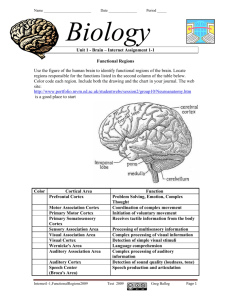
Reduced 5-HT2A Receptor Binding after Recovery from Anorexia Nervosa Guido K. Frank, Walter H. Kaye, Carolyn C. Meltzer, Julie C. Price, Phil Greer, Claire McConaha, and Kelli Skovira Background: Several lines of evidence suggest that a disturbance of serotonin neuronal pathways may contribute to the pathogenesis of anorexia nervosa (AN). This study applied positron emission tomography (PET) to investigate the brain serotonin 2A (5HT2A) receptor, which could contribute to disturbances of appetite and behavior in AN. Methods: To avoid the confounding effects of malnutrition, we studied 16 women recovered from AN (REC AN, ⬎1 year normal weight, regular menstrual cycles, no bingeing or purging) compared with 23 healthy control women (CW) using [18F]altanserin, a specific 5-HT2A receptor antagonist on PET imaging. Results: REC AN women had significantly reduced [18F]altanserin binding relative to CW in mesial temporal (amygdala and hippocampus), as well as cingulate cortical regions. In a subset of subjects (11 CW and 16 REC AN), statistical parametric mapping (SPM) confirmed reduced mesial temporal cortex 5HT2A receptor binding and, in addition, showed reduced occipital and parietal cortex binding. Conclusions: This study extends research suggesting that altered 5-HT neuronal system activity persists after recovery from AN and may be related to disturbances of mesial temporal lobe function. Altered 5-HT neurotransmission after recovery also supports the possibility that this may be a trait-related disturbance that contributes to the pathophysiology of AN. Biol Psychiatry 2002;52: 896 –906 © 2002 Society of Biological Psychiatry Key Words: Anorexia nervosa, serotonin, receptor, limbic system Introduction A norexia nervosa (AN) is a disorder that most often has its onset during adolescence in young women and is invariably characterized by the relentless pursuit of From the Department of Psychiatry, Western Psychiatric Institute and Clinic (GKF, WHK, CM, KS), and Department of Radiology, Presbyterian University Hospital (CCM, JCP, PG), University of Pittsburgh, School of Medicine, Pittsburgh, Pennsylvania. Address reprint requests to Walter H. Kaye, M.D., University of Pittsburgh, Western Psychiatric Institute and Clinic, 3811 O’Hara Street, Pittsburgh PA 15213. Received November 7, 2001; revised February 15, 2002; accepted February 21, 2002. © 2002 Society of Biological Psychiatry thinness, obsessive fears of being fat, and emaciation. Consequently, AN has the highest mortality among the psychiatric disorders (Sullivan 1995). Depression, anxiety, and obsessive– compulsive behaviors are common. People with AN tend to have a characteristic cluster of personality and temperament traits including perfectionism, over control, rigidity, and harm avoidance (Palmer and Jones 1939). Such behaviors may be traits because they occur premorbidly and persist after weight and eating normalize (Casper 1990; Klump et al 2000; Srinivasagam et al 1995). The etiology of AN is presumed to be complex and has traditionally been thought to be influenced by developmental and social factors (Garner 1993; Treasure and Campbell 1994); however, the stereotypic clinical presentation, gender distribution, and age of onset suggest a biologic vulnerability. Recent studies show that AN is familial (Lilenfeld et al 1998; Strober et al 2000) with three large-scale, community-based twin studies suggesting that eating disorders have a heritability of between 0.5 and 0.8 (Bulik et al 1998). The clustering of the disorder in families may be related in part to a genetic transmission of risk. A considerable number of animal and human studies suggest that altered central nervous system serotonin (5-HT) activity may contribute to the appetitive and behavioral alterations found in AN. For example, increased intrasynaptic 5-HT, or directly activated 5-HT receptors, tend to reduce food consumption (Blundell 1984; Leibowitz and Shor-Posner 1986), and alterations in 5-HT activity be implicated in disturbances of mood and impulse control (Higley and Linnoila 1997; Kaye 1997; Lucki 1998; Mann 1999). In fact, most studies have shown that ill AN patients have disturbances (i.e., a reduction) of central 5-HT activity (Kaye et al 1988; Walsh et al 1998; Wolfe et al 1997). Behavioral or 5-HT disturbances in ill AN patients may be a consequence of malnutrition or premorbid traits that contribute to a vulnerability to develop AN. Determining whether abnormalities are a consequence or a potential antecedent of pathologic feeding behavior is a major question in the study of eating disorders. It is impractical to study AN prospectively because of the young age of onset and difficulty in premorbid identification of people 0006-3223/02/$22.00 PII S0006-3223(02)01378-1 Serotonin Receptor Activity in Anorexia who will develop the disorder. Another strategy is to study women who are recovered from AN. Any persistent psychobiological abnormalities might be trait related and potentially contribute to the pathogenesis of this disorder. In fact, increased levels of cerebrospinal fluid (CSF) 5-hydroxy indoleacetic acid (5-HIAA), the major metabolite of 5-HT, have been found after long-term recovery from AN (Kaye et al 1991). Other studies of recovered AN found reduced appetite suppression in response to the 5-HT challenge drug D-fenfluramine (Ward et al 1998), but normal 5-HT-related endocrine secretion (O’Dwyer et al 1996; Ward et al 1998). The 5-HT neurotransmitter system is widespread throughout the brain, (Nieuwenhuys et al 1988), and the loci of CNS pathophysiology responsible for serotonin and behavioral abnormalities in people with AN are unknown. Positron emission tomography (PET) technologies hold the promise of understanding previously inaccessible brain 5-HT function in vivo and its dynamic relationship with human behaviors. In this study, the radioligand [18F]altanserin, a specific 5-HT2A receptor antagonist, was used together with PET imaging to determine whether the 5-HT2A receptor system was altered in women who were recovered from AN. The 5-HT2A receptor system is of potential interest in AN because it has been implicated in the modulation of feeding (inducing hypophagia), mood, and anxiety as well as in antidepressant efficacy (Bonhomme and Esposito 1998; De Vry and Schreiber 2000; Simansky 1996; Stockmeier 1997). In addition, some but not all studies have found differences in allele frequencies of the 5-HT2A receptor in AN (Hinney et al 2000). Because 5-HT2A receptors are in high concentrations in the cortex, this study sought to determine whether PET could identify alterations of specific cortical brain regions in AN. Recently, we showed in a group of women recovered from bulimia nervosa (REC BN) reduced cortical 5-HT2A receptor binding that was significant in the orbital frontal cortex (Kaye et al 2001). Women with AN and BN share increased CSF 5-HIAA after recovery (Kaye et al 1998a, 1998b). Thus, we hypothesized that postsynaptic cortical 5-HT2A receptor densities would be downregulated in response to the suggested 5-HT hyperactivity in AN after recovery (Rioux et al 1999; Roth et al 1998) similar to our previous finding in REC BN. We hypothesized that, if regional cortical alterations occur in AN, they are most likely to be present in frontal or limbic regions because such regions have been particularly implicated in the modulation of mood and impulse control (McAllister 1992). Methods and Materials Sixteen women who had recovered from restricting type AN (REC RAN) were recruited. No subject had a history of bingeing or purging. Subjects were previously treated in the eating BIOL PSYCHIATRY 2002;52:896 –906 897 disorders treatment program at the Western Psychiatric Institute and Clinic (Pittsburgh, PA) or were recruited through advertisements. All subjects underwent four levels of screening: 1) a brief phone screening; 2) an intensive screening assessing psychiatric history, lifetime weight, and exercise and menstrual cycle history as well as eating pattern and exercise history for the past 12 months; 3) a comprehensive assessment using structured and semistructured interviews; and 4) a face-to-face interview with a psychiatrist. To be considered “recovered,” subjects had to 1) maintain a weight above 85% average body weight (Metropolitan Life Insurance Company 1959); 2) have regular menstrual cycles; and 3) have not binged, purged, or engaged in significant restrictive eating patterns for at least 1 year before the study. Additionally, subjects must not have used psychoactive medication such as antidepressants or met criteria for alcohol or drug abuse or dependence, major depressive disorder or severe anxiety disorder within 3 months of the study. Twenty-one healthy control women (CW) were recruited through local advertisements. The CW had no history of an eating disorder or any psychiatric, medical, or neurologic illness. They had no firstdegree relative with an eating disorder. They had normal menstrual cycles and had been within normal weight range since menarche. This study was conducted according to local institutional review board regulations, and all subjects gave written informed consent. The PET imaging was performed during the first 10 days of the follicular phase for all subjects. Subjects were admitted to a research laboratory on the eating disorders unit of Western Psychiatric Institute and Clinic at 9:00 pm of the day before the PET study for adaptation to the laboratory and for psychologic assessments. The PET study was done the next day. All subjects had the same standardized, monoamine controlled (low protein) breakfast on the morning of the study. Blood was drawn for assessment of -hydroxybutyrate (BHBA), a plasma ketone body that is relatively sensitive to reflecting the presence of starvation (Fichter et al 1990), as well as for evaluation of gonadal hormone levels (estradiol, E2). The Structured Clinical Interview for DSM-IV Axis I Disorders (First et al 1996) was used to assess the lifetime prevalence of Axis I psychiatric disorders, and the Structured Interview for Anorexia and Bulimia (Fichter et al 1998) to assess lifetime diagnosis of an eating disorder. These interviews were administered by a trained masters- or doctoral-level clinical interviewer and blindly reviewed by a psychiatrist or trained PhD-level psychologist, who validated final DSM-IV Axis I diagnoses. Current psychopathology was assessed with a battery of standardized instruments including the Beck Depression Inventory (Beck et al 1961), the Spielberger State–Trait Anxiety Inventory (Spielberger et al 1970), the Frost Multidimensional Perfectionism Scale (Frost et al 1990), and the Temperament and Character Inventory (Cloninger et al 1994) for assessment of harm avoidance, novelty seeking, and reward dependence. All subjects underwent magnetic resonance (MR) imaging before the PET scan on a Signa 1.5 Tesla scanner (GE Medical Systems, Milwaukee, WI) using a standard head coil. A volumetric spoiled gradient recalled (SPGR) sequence (TE ⫽ 5, TR ⫽ 25, flip angle ⫽ 40°, NEX ⫽ 1; field of view ⫽ 24 cm, image matrix ⫽ 256 ⫻ 192 pixels) acquired in the coronal plane was 898 BIOL PSYCHIATRY 2002;52:896 –906 used to guide region of interest (ROI) selection. Fast spin-echo T2 and proton density weighted images were also routinely acquired to exclude significant neuropathology. Pixels that corresponded to scalp and calvarium were removed from the SPGR MR images (Sandor and Leahy 1997), and the MR and PET image data were then coregistered (Woods et al 1993). The 5-HT2A receptor–specific radioligand [18F]altanserin was used and synthesized as described by Lemaire et al (1991). Subjects were studied using two PET scanners, ECAT HR⫹ and 951R/31 (CTI PET Systems, Knoxville, TN) because the 951RPET scanner was replaced by the HR⫹ during the course of this study. The 951R/31 acquires 31 slices over a 108-mm axial field of view (FOV). The HR⫹ scanner acquires 63 continuous slices over a 152-mm axial FOV. All subjects were studied in two dimensional (2D) imaging mode (septa extended). Under these conditions, the 951R/31 has a point source resolution in air reconstructed (without smoothing) of approximately 6.0 mm full-width at half-maximum (FWHM) in the in-plane, and 5.0 mm FWHM in the axial orientation (Spinks et al 1992). In 2D, the HR⫹ scanner has an approximated in-plane resolution of 4.9 mm (1–10 cm radius) at FWHM, and an axial resolution of 4.4 mm FWHM (Brix et al 1997). All REC AN women were studied on the HR⫹ PET scanner. Eleven CW were studied on the HR⫹ scanner and 12 were studied on the 951R PET scanner. Data on the 12 CW studied with the 951R PET scanner were previously published (Kaye et al 2001). The CW studies on the HR⫹ and the 951R PET scanners had similar age and body mass index (BMI). A comparison of regional 5-HT2A receptor binding potential values between CW sub groups using nonparametric Mann–Whitney U tests yielded similar binding across groups, with a U value range between 5 and 52, and corresponding p values between 0.9 and 0.2. For example, CW values were as follows: prefrontal cortex, 2.41 ⫾ 0.2 (HR⫹ scanner) and 2.40 ⫾ 0.3 (951R scanner), U ⫽ 50, p ⫽ .8; mesial temporal cortex, 1.64 ⫾ 0.2 (HR⫹ scanner) and 1.70 ⫾ 0.2 (951R scanner), U ⫽ 46, p ⫽ .6. Because these two groups of CW were similar, and because the methods for 5HT2A binding assessment used relative measures (regional binding divided by the binding in a reference region, discussed below), the data on CW were combined. Subjects were positioned with the head oriented parallel to the cantomeatal line. A softened thermoplastic mold with generous holes for eyes, nose, and ears was fitted closely around the head and attached to the headholder to minimize subject motion. A 10-min transmission scan was obtained and used for attenuation correction. Following bolus intravenous injection of 10 mCi high-specific activity (ⱖ1.04 Ci/mol) [18F]altanserin, dynamic emission scanning with arterial blood sampling was performed until 90 min postinjection. The arterial input function was determined by approximately 35 0.5-mL hand-drawn samples collected over the scanning interval (including 20 samples in the initial 2 min postinjection). Blood samples were centrifuged and the plasma radioactivity concentration measured (Cobra II, Packard Instruments, Cleveland, OH). Additionally, 3-mL blood samples were acquired at 2, 10, 30, 60, and 90 min after [18F]altanserin injection and used to determine the fraction of unmetabolized [18F]altanserin (of total plasma radioactivity concentration) using high-performance liquid chromatography G.K. Frank et al (HPLC). Plasma data were corrected for the presence of radiolabeled metabolites of [18F]altanserin using the HPLC data (Lopresti et al 1998). The PET data were also corrected for radioactive decay and scatter and reconstructed with a Hanning window and a cutoff at 0.8 of the Nyquist rate. The ROIs were hand drawn on the coregistered MR images and applied to the dynamic PET data to generate time-activity curves. The following ROIs were selected: prefrontal cortex (Brodmann’s area [BA] 10), medial orbital frontal cortex (BA 11), lateral orbital frontal cortex (BA 47), mesial temporal cortex (amygdalo– hippocampal complex), lateral temporal cortex (BA 21), supragenual cingulate (BA 24/32, five planes superior to anterior most part of genu corporis callosi), pregenual cingulate (BA 24/32, anterior to anterior most part of genu of the corpus callosum), and subgenual cingulate (BA 25, inferior to the genu of the corpus callosum), parietal cortex (BA 7), and sensorimotor cortex (BA 1,2,3,4). We also performed ROI sampling of the cerebellum, and this was used as the reference region because of the low concentration of 5-HT2A receptors (Pazos et al 1987). The ROIs were expressed as the mean of left and right values. All subjects were assigned a number at the local PET facility, and imaging data were analyzed blindly. The data on 12 CW from the 951R scanner had previously been assessed similarly under blind conditions (Kaye et al 2001). For the kinetic analyses, the Logan graphic method was applied based on sampled ROI data from 8 to 90 min following [18F]altanserin injection. The regression slope value (distribution volume, DV) for each ROI was calculated (Logan et al 1990). The cerebellar data were assumed to represent free and nonspecifically bound radioactivity concentrations. The ratio of regional [18F]altanserin binding (DV ROI) in relation to cerebellar [18F]altanserin binding (DV Cer) was calculated (DVROI/DVCer ⫽ Dvratio, DVR), and the DVR was used as a specific binding measure (Smith et al 1998). Recent literature suggests that the cerebellum is not totally devoid of 5HT2A receptors (Dwivedi and Pandey 1998; Staley et al 2001). Although the number of such cerebellar 5HT2A receptors is low, an influence on ROI-specific binding could not be excluded. We therefore also compared the cerebellar DV between groups. The ROI-based data analysis may be confounded by how individual regions are drawn, as well as by potentially missing areas of binding alterations due to a limited number of assessed ROIs. Thus, an additional analysis using statistical parametric mapping was performed on all subjects studied on the HR⫹ scanner, using Statistical Parametric Mapping (SPM) software (Frackowiak et al 1997; Friston 1995). We created DVR images for all subjects on the HR⫹ scanner by applying the Logan modeling method on a pixel-by-pixel basis for each PET image and dividing each pixel by the cerebellar binding value (Smith et al 1998). All MR images were normalized to the Montreal Neurologic Institute (MNI, Canada) standard brain that is derived from 152 subjects (Evans et al 1993). The normalized DVR images were then smoothed with a Gaussian filter (12 mm FWHM). Statistical parametric maps were created based on the t statistic (Friston 1995), assigning a p value to each voxel (probability image). An initial uncorrected p value of ⬍0.05 was selected as threshold for display in the probability image. Regions considered significant had to be either of significant Serotonin Receptor Activity in Anorexia BIOL PSYCHIATRY 2002;52:896 –906 899 Table 1. Demographic Variables between Groups and Behavioral Assessment Data CW (n ⫽ 23) Age (years) Current BMI AN onset (years of age) Duration of recovery (years) Estradiol (pmol/mL) Plasma BHBA (mol/mL) Drive for Thinness (EDI) Depression (BDI) Perfectionism (MPS) Novelty seeking (TCI) Harm avoidance (TCI) Reward dependence (TCI) State anxiety (STAI) Trait anxiety (STAI) REC AN (n ⫽ 16) Mean SD Mean SD U Exact Sig. 25.3 21.4 — — 35 100 0.6 1 54 21 12 20 26 28 5.3 1.3 — — 26 103 1.2 1.5 13 5 4 2 5 7 24.5 20.5 14.2 4.3 74 42 15.3 (12) 3.3 (12) 101 (12) 20 (12) 15 (12) 16 (12) 32 (12) 38 (12) 6.1 1.8 2.9 3.3 51 14 6.4 3.6 29 7 8 4 7 10 155 105 — — 28.5 31 14.5 87.5 28.5 109 87 59 78 53.5 .4 .024 — — .1 .1 ⬍.001 .047 ⬍.001 .5 .15 .01 .04 .04 (12) indicates that only 12 of the REC AN women completed self-assessment questionnaires. Group comparison by Mann–Whitney U test. CW, healthy comparison women; REC AN, recovered anorexic women; Sig., significance; BMI, body mass index; BHBA, beta hydroxy butryic acid; EDI, Eating Disorders Inventory; TCI, Temperament and Character Inventory; BDI, Beck Depression Inventory; STAI, State and Trait Anxiety Inventory. cluster size or voxel significance (p ⬍ .05) after correction for multiple comparisons. We also assessed, in an exploratory analysis, possible structural differences between groups, because such alterations theoretically could confine 5-HT receptor distribution findings. We used SPGR images and compared these by group with the voxel-based morphometry tool kit (VBM) within SPM (Ashburner and Friston 2000). In short, this analysis is a voxelwise comparison of the local concentration of gray and white matter. For this approach, SPGR images from each subject were aligned to a vertical, midsagittal plane (Woods et al 1992) and spatially transformed into the MNI standard reference atlas described above. All images were separated into GM, WM, and CSF. Differences in between-subject global activity were removed by analysis of covariance (ANCOVA) on a pixel-by-pixel basis with global counts as the covariate. The resulting image data were then convolved with a three-dimensional Gaussian filter (12 mm FWHM). Groups were compared using t statistic– based parametric maps and multiple comparison corrections as above. The SPSS statistical software package (Barcikowski 1984) was used for all other statistical analyses. Because of the relatively small sample size, between-group comparisons were made with nonparametric Mann–Whitney U two independent samples tests calculating two-sided exact significance levels. Multiple comparisons were corrected using the Bonferroni correction. Correlations were examined with Spearman correlation coefficients. Factors that were considered possible confounds of 5-HT2A receptor binding were explored with analyses of covariance (ANCOVA). To assess possible seasonal influences on 5HT2A binding, we compared the distribution of PET scans over the 12 months between groups using a chi-square test. All values are expressed as mean ⫾ SD. As level of significance a p value of p ⬍ .05 was selected. Results Demographic Variables and Behavioral Assessments The REC AN and CW women were of similar ages (Table 1). Although current BMI was significantly lower in REC AN, the mean difference was less than 1 BMI unit. Subject groups had similar plasma BHBA values, a measure of ketone body metabolism, suggesting REC AN were not starving. In addition, plasma E2 was similar between groups. The REC AN subjects scored significantly higher on drive for thinness, perfectionism, state and trait anxiety, and depressive symptoms (Table 1). Groups did not differ significantly on harm avoidance or novelty seeking; however, reward dependence was significantly reduced in REC AN. Eight subjects of the REC AN group had a confirmed history of major depressive disorder (MDD), three a subthreshold MDD, and seven subjects had a history of obsessive– compulsive disorder (OCD). One subject in the REC AN group had a history of a panic disorder. None of the REC AN women had a history of any psychotic disorder. ROI-Based Analysis of 5-HT2A Receptor Binding The REC AN subjects had a significant reduction of 5-HT2A receptor binding in mesial temporal cortex, preand subgenual cingulate (Table 2) and a trend toward a reduction in the sensorimotor cortex. The REC AN and CW women had similar binding in the prefrontal cortex, medial, and lateral orbital frontal cortex and the lateral 900 G.K. Frank et al BIOL PSYCHIATRY 2002;52:896 –906 Table 2. Regional 5-HT2A Receptor Binding between Groups CW (n ⫽ 23) DVROI/DVCer REC AN (n ⫽ 16) DVROI/DVCer Region of interest Mean SD Mean SD U Exact Sig. Prefrontal cortex Lateral orbital frontal cortex Medial orbital frontal cortex Supragenual cingulate Subgenual cingulate Pregenual cingulate Lateral temporal cortex Mesial temporal cortex Parietal cortex Sensorimotor cortex 2.42 2.39 2.58 2.45 2.69 2.58 2.63 1.68 2.6 2.28 0.25 0.25 0.28 0.31 0.27 0.28 0.22 0.19 0.28 0.28 2.41 2.4 2.51 2.29 2.47 2.4 2.65 1.52 2.49 2.13 0.26 0.26 0.32 0.25 0.27 0.24 0.29 0.17 0.32 0.27 183 170 155 129 110 113 179 86 127 124 .9 .7 .4 .1 .035 .04 .9 .004 .2 .09 Group comparison by Mann–Whitney U test. DVROI/DVCER is the distribution volume of regional serotonin 2A (5-HT2A) receptor binding in relation to cerebellar value. CW, healthy comparison women; REC AN, recovered anorexic women; Sig., significance. temporal cortex. Ten ROIs were assessed. After correction for multiple comparisons, REC AN women continued to have reduced binding in the mesial temporal cortex (p ⫽ .04). Because the CW women were studied on two scanners, a comparison was done between CW (n ⫽ 11) and REC AN (n ⫽ 16) women who were scanned on the same scanner (ECAT HR⫹). Both groups were of similar ages and BMI. The REC AN subjects continued to show significantly reduced binding in the mesial temporal cortex (p ⫽ .008) and anterior medial cingulate (p ⫽ .02) and a trend toward reduced binding in the supragenual (p ⫽ .08) and subgenual (p ⫽ .05) cingulate, as well as the lateral orbital frontal (p ⫽ .1), parietal (p ⫽ .06), and sensorimotor cortex (p ⫽ .09). The cerebellar 5HT2A DV between CW (1.36 ⫾ 0.18) and REC AN (1.23 ⫾ 0.37) was similar (U ⫽ 118, p ⫽ .1). In addition, we compared the percentage of unmetabolized [18F]altanserin (parent) in plasma between control and anorexic subjects five times throughout the study (2, 10, 30, 60, and 90 min) using a repeated measures ANOVA. Data between CW and REC AN were similar (F ⫽ 0.6, p ⫽ .7). SPM-Based Analysis of 5-HT2A Receptor Binding This analysis revealed significant clusters of reduced 5-HT2A receptor binding in REC AN compared with CW after correction for multiple comparisons. In the left hemisphere, these regions were located in the mesial temporal cortex, middle temporal gyrus, and subcortical parietal lobe (Table 3 and Figure 1). In the right hemisphere, these regions were located in the middle temporal gyrus, amygdaloid complex, and subiculum– hippocampus. Analysis of Structural Images Using VBM/SPM There was no significant difference between groups on a voxel level. In particular, no mesial temporal or cingulate related alterations were found. Table 3. Cluster Sizes, p values, and Z Scores for Areas of Most Prominent 5-HT2A Binding Alterations for Right (r) and Left (l) Hemispheres for Statistical Parametric Mapping–Based Analysis Cluster Size Coordinates (mm) p (corrected) 4478 .001 7446 ⬍.001 Z score x y z Brain Region 4.31 3.80 3.43 3.77 3.42 3.25 ⫺50 ⫺30 ⫺38 32 26 56 ⫺44 ⫺28 ⫺52 4 ⫺12 ⫺40 ⫺14 ⫺22 26 ⫺36 ⫺30 ⫺16 Middle temporal gyrus (l) Mesial temporal cortex (l) Subcortical parietal lobe (l) Amygdaloid complex (r) Subiculum/hippocamps (r) Middle temporal gyrus (r) Subjects scanned on the HR⫹ scanner (CW n ⫽ 11; REC AN n ⫽ 16). CW, control women; REC AN, recovered anorexic women. Serotonin Receptor Activity in Anorexia BIOL PSYCHIATRY 2002;52:896 –906 901 reduced 5HT2A receptor binding compared with CW for the mesial temporal cortex (1.4 ⫾ 0.05 vs. 1.7 ⫾ 0.2, p ⫽ .001; p ⫽ .01 after correction for multiple comparisons) and a tendency toward reduced binding (p ⬍ .1) in sensorimotor, parietal, subgenual cingulate cortex, and basal ganglia (data not shown). Neither the CW nor the REC AN women had significant relationships between measures of behavior and 5-HT2A binding. There was no difference between groups in terms of the relationship between 5HT2A receptor binding and seasonality (X ⫽ 2.5, df ⫽ 1, p ⫽ .2). Discussion Figure 1. Clusters of significantly reduced 5HT2A binding in recovered anorexic women (REC AN, n ⫽ 16) compared with healthy comparison women (CW, n ⫽ 11) with all subjects scanned on the HR⫹ scanner. p ⬍ .05 for each voxel between groups, df ⫽ 1,25 based on the t-statistic; all clusters shown are significant after correction for multiple comparisons (p ⱕ .001). The upper image row shows significant clusters in a standard grid system. The lower row overlays significant clusters on a normalized reference MRI. Relationships of Demographic Values and Comorbidity with 5HT2A Receptor Binding The CW and REC AN groups each showed significantly negative relationships between age and 5-HT2A receptor binding for most cortical regions (Table 4). A comparison of slopes shows similarities for all regions for REC AN and CW. Neither group had significant relationships between 5-HT2A receptor binding and current BMI, plasma BHBA, or E2. Subgroups of REC AN subjects had similar regional binding when compared as to whether they had a lifetime history of MDD or OCD. The REC AN without a history of MDD (n ⫽ 5) continued to show significantly Table 4. Regional 5-HT2A Receptor Binding and Correlation with Age CW (n ⫽ 23) Prefrontal cortex Lateral orbital frontal cortex Medial orbital frontal cortex Supragenual cingulate Subgenual cingulate Pregenual cingulate Lateral temporal cortex Mesial temporal cortex Parietal cortex Sensorimotor cortex REC AN (n ⫽ 16) rho p rho p ⫺.5 ⫺.3 ⫺.5 ⫺.5 ⫺.5 ⫺.5 ⫺.5 ⫺.3 ⫺.5 ⫺.5 .01 .23 .03 .01 .03 .02 .03 .20 .01 .01 ⫺.4 ⫺.6 ⫺.6 ⫺.6 ⫺.4 ⫺.6 ⫺.5 ⫺.3 ⫺.5 ⫺.6 .13 .01 .01 .02 .10 .02 .04 .35 .56 .02 CW, healthy control women; REC AN, recovered anorexic women; rho, Spearman correlation coefficient. These data confirm that a disturbance of brain 5-HT neuronal function persists after recovery from AN. Directed ROI and whole brain SPM analyses suggested that the most substantial reduction in 5-HT2A receptor binding occurred in the mesial temporal cortex, including the amygdala and hippocampus. Recovered AN women have increased CSF 5-HIAA raising the possibility that they have increased brain 5-HT activity (Kaye et al 1991). One possible explanation for the findings in this study is that reduced 5-HT2A binding is a compensatory response for increased extracellular levels of 5-HT. Studies in animals confirm that reduced 5-HT2A receptor density occurs in response to increased intra synaptic 5-HT (Rioux et al 1999; Saucier et al 1998) or 5HT agonists (Eison and Mullins 1996). In addition, paroxetine treatment for depression reduces 5-HT2A receptors in the brain, presumably due to increased intrasynaptic 5-HT (Meyer et al 2001). Some, but not all, studies raise the question of whether an increased frequency of a variant of the 2A receptor is present in AN (Hinney et al 2000); however, it is unknown if this receptor variant has functional significance. It is also important to note that these PET imaging studies do not permit a determination of whether there is an alteration in affinity or number of the 5-HT2A receptor. We are not aware of any previous in vivo neuroreceptor studies in ill or recovered AN women; however, 5-HT2, or more specifically 5-HT2A receptor binding, has been assessed in depressed subjects. Some studies of MDD have found reduced 5-HT2A receptor binding in frontal, temporal, parietal, and occipital cortical regions before or after treatment (Attar-Levy et al 1999; Biver et al 1997; Yatham et al 2000). Other studies in depressed subjects (Meltzer and Reynolds 1999; Meyer et al 1999) did not find such changes. To our knowledge, no such studies have been done in anxiety disorders or OCD. Other types of brain imaging studies in AN have reported structural or functional alterations. Subjects with active AN have enlarged ventricles and sulci widening 902 BIOL PSYCHIATRY 2002;52:896 –906 (see review Ellison and Fong 1998). A 1H-MR scan revealed reduced lipid signals in the frontal white matter and occipital gray matter and was associated with decreased BMI (Roser et al 1999). These alterations have been thought to be reversible after recovery but recent data raise the question of persistent changes after recovery (Katzman et al 1997; Lambe et al 1997). A number of studies using single photon computed tomography (SPECT) or PET with 2-deoxy-glucose, have shown temporal alterations and less frequently frontal or cingulate changes. Gordon et al (1997) using SPECT found ill AN patients had unilateral temporal lobe hypoperfusion that persisted in subjects studied after weight restoration. Ellison et al (1998) using functional MR imaging, found that ill AN patients, when viewing pictures of high-caloric drinks, had increased signal changes in the left insular, cingulate gyrus, and left amygdala-hippocampus region and increased anxiety. Rauch et al (2000) using PET O-15 and pictures of high-calorie food, found ill AN patients had elevated regional cerebral blood flow in bilateral mesial temporal lobes and increased anxiety. Taken together, these studies suggest that temporal cortex alterations occur in AN. Similarly, our study found that the most pronounced change in 5-HT2A binding in REC AN women was in the mesial temporal cortex regions, including hippocampus and amygdala regions. The amygdala is thought to play a central role in the “interpretation of fear” (Charney and Deuth 1996; Davis 1992) and anxiety disorders (Benkelfat et al 1995; Reiman et al 1984; Van der Linden et al 2000). The mesial temporal cortex may also play a role in depressive symptoms (Byrum et al 1999; Kennedy et al 1997), OCD (Breiter and Rauch 1996; Zald et al 1996), memory processing (Marrazzi et al 1990), and aversive conditioning (Breiter and Rosen 1999; Buchel et al 1999; Schneider et al 1999; Zalla et al 2000). Thus, these data support the possibility, raised by recent neuroimaging studies, that alterations of the hippocampus–amygdala region may play a more general role in psychopathology (Fujita et al 2000). In a preliminary analysis, 5HT2A binding changes in our study were generally bilateral and not lateralized (data not shown); however, due to the relatively small sample size and increased variability when assessing lateralized binding, we cannot exclude a lataralization of altered binding in a larger group of subjects. Consistent with earlier studies (Srinivasagam et al 1995), REC AN women had increased depression, anxiety, and perfectionism. In fact, such symptoms, obsessions (Kaye 1997), and cognitive alterations (Bradley et al 1997; Strupp et al 1986) occur when people with AN are ill and persist after recovery. Theoretically, disturbed 5-HT neuronal transmission in the mesial temporal cortex areas in people with AN could be related to such symptoms. G.K. Frank et al This study raises the possibility that REC AN women have altered 5HT2A binding in cingulate regions as well as occipitoparietal and sensorimotor cortex. The anterior cingulate receives afferents from the amygdala and has direct projections to the premotor frontal cortex and other limbic regions. The anterior cingulate has been characterized as “executive” in function and contributes to attention by monitoring the motivational significance of stimuli (Devinsky et al 1995; Tucker et al 1995). Overall, the anterior cingulate cortex has a role in affect as well as visuospatial and memory functions and appears to play a crucial role in initiation, motivation, and goal-directed behaviors. The primary sensory and association cortices have input into the limbic system (Charney and Deuth 1996), and the parietal cortex may be involved in the circuitry of depression, anxiety (Davidson et al 1999), and memory consolidation (Izquierdo and Medina 1997). In another study, our group reported (Kaye et al 2001) that nine REC BN women, who never had AN, had a significant downregulation of 5-HT2A receptors in the orbital frontal cortex and a trend toward a reduction in the lateral orbital frontal cortex and the sensorimotor cortex. In addition, the CW showed a well-known negative relationship between age and 5-HT2A binding in most cortical regions (data on 12 of the CW in this study were reported in our previous study). Importantly, a relationship between age and 5HT2A binding was not found in the REC BN sample in regions of interest. Although AN and BN are related disorders because they are cross-transmitted in families, a number of factors distinguish the subgroups, such as extremes of eating behavior and impulse control. These data raise the possibility that regional differences in [18F]altanserin binding or relationships of [18F]altanserin binding to age may distinguish eating disorder subgroups after recovery. That is, REC BN women had a substantial reduction of [18F]altanserin 5HT2A receptor binding localized to the orbital frontal cortex (Kaye et al 2001). In contrast, REC AN show diminished [18F]altanserin in temporal as well as cingulate, parietal, and sensorimotor binding in this study. The disturbance of orbital frontal 5HT circuits in BN may contribute to a vulnerability for imprecise and poorly modulated self-control, whereas temporocingulate alterations in AN may contribute to impaired motivation and integration of cognition and mood. In terms of limitations, we studied a relatively small number of AN subjects; however, a power analysis using the data for the mesial temporal cortex showed a power of 0.85 for detection of two-group differences for the sample size in this study. Still, it is possible that we did not detect more subtle 5-HT2A receptor alterations because of the small sample size. The REC AN women had a reduction of current BMI compared with CW; however, all subjects’ Serotonin Receptor Activity in Anorexia weights were in a normal weight range, and there was less than 1 unit of BMI difference between groups. An additional regression analysis using group and BMI as regressors showed a significant effect for group (t ⫽ ⫺2.5, p ⫽ .02) but no effect for BMI (t ⫽ ⫺0.1, p ⫽ .9). Moreover, no previous study demonstrated a relation of BMI and brain 5-HT2A receptor binding, and there was no relation of current BMI and receptor binding in either one of the groups of this study. Thus, there is no evidence that differences in weight account for the findings. The use of self-assessments for the evaluation of recovery may be a limitation, and different eating patterns between groups could theoretically alter 5HT2A receptor activity; however, plasma BHBA was similar between groups, suggesting a similar nutritional status. Similar plasma E2 values further supported normal menstrual function and status of recovery. Beside [18F]altanserin, other radioligands have been used for assessment of 5HT2A receptor imaging (Staley et al 1998); however, [18F]altanserin binds highly specific to 5HT2A receptors. It shows a high affinity (Ki ⫽ 0.51 nmol/mL) and high selectivity (90- to 400-fold less potent at ␣1 and 5HT2C receptor) for 5HT2A receptors and is superior compared with other 5HT2A ligands (Price et al 2001). The use of [18F]altanserin has been validated in the past (Smith et al 1998). A disadvantage of [18F]altanserin is its rapid metabolization that may increase nonspecific binding. [18F]altanserin cerebellar DV values were similar between groups in this study, however, supporting the assumption that nonspecific binding was similar between groups. In addition, the percentage of unmetabolized [18F]altanserin in plasma was similar between control and anorexic subjects. This suggested that altered 5HT2A binding between groups was not driven by different metabolism of [18F]altanserin. Recent studies have shown that the cerebellum is not totally devoid of 5HT2A receptors (Dwivedi and Pandey 1998; Staley et al 2001), and altered cerebellar 5HT2A binding could contribute to the study outcome. Because 5HT2A cerebellar data were similar between groups, however, ROI-specific binding in CW was not driven by reduced 5HT2A DV values in the reference region (i.e., cerebellum). When studies performed on different scanners are combined, different sensitivity or signal to noise ratio could contribute to altered findings; however, all PET scans were performed in 2D mode. More important, the analysis procedure used was a relative measure, thus accounting for eventual systematically increased or decreased binding detection. In addition, the binding values between the CW groups from the two scanners were similar and did not suggest any systematic errors. The comparison of groups with subjects BIOL PSYCHIATRY 2002;52:896 –906 903 studied on the HR⫹ scanner only (both by ROI- and SPM-based analyses), further supports the findings in the combined group. It is possible that structural alterations in the REC AN group might have contributed to this finding (Katzman et al 1997), but in our investigational analysis of gray matter volumes between groups, no structural alterations were found. In conclusion, this study supports previous findings of altered 5-HT neuronal transmission after recovery from AN. It is problematic to identify women with AN before they develop the disorder. Studying women after longterm recovery may be the best available approximation to identifying factors that might be involved in the development of AN. Although a scarring effects from the illness cannot be excluded, reduced 5-HT2A receptor binding in AN thus could be an indication of a trait related 5-HT disturbance or, alternatively, a secondary phenomenon in response to increased central 5HT transmission in this group. Supported in part by National Institute of Mental Health Grant No. R01 MH46001-07A1 and Children’s Hospital Clinical Research Center, Pittsburgh PA (#5 M01RR00084). References Ashburner J, Friston KJ (2000): Voxel-based morphometry—the methods. Neuroimage 11:805–821. Attar-Levy D, Martinot J-L, Blin J, Dao-Castellana M-H, Crouzel C, Mazoyer B, et al (1999): The cortical serotonin-sub-2 receptors studied with positron-emission tomography and [18F]-setoperone during depressive illness and antidepressant treatment with clomipramine. Biol Psychiatry 45:180 –186. Barcikowski RS (1984): Computer Packages and Research Design, vol. 3: SPSS & SPSSX. Lanham, MD: University Press of America. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961): An Inventory for measuring depression. Arch Gen Psychiatry 4:561–571. Benkelfat C, Bradwejn J, Meyer E, Ellenbogen M, Milot S, Gjedde A, Evans A (1995): Functional neuroanatomy of CCK4-induced anxiety in normal healthy volunteers [see comments]. Am J Psychiatry 152:1180 –1184. Biver F, Wikler D, Lotstra F, Damhaut P, Goldman S, Mendlewicz J (1997): Serotonin 5-HT2 receptor imaging in major depression: Focal changes in orbito-insular cortex. Br J Psychiatry 171:444 –448. Blundell JE (1984): Serotonin and appetite. Neuropharmacology 12B:1537–1551. Bonhomme N, Esposito E (1998): Involvement of serotonin and dopamine in the mechanism of action of novel antidepressant drugs: A review. J Clin Psychopharmacol 18:447–454. Bradley SJ, Taylor MJ, Rovet JF, Goldberg E, Hood J, Wachsmuth R, et al (1997): Assessment of brain function in 904 BIOL PSYCHIATRY 2002;52:896 –906 adolescent anorexia nervosa before and after weight gain. J Clin Exp Neuropsychol 1:20 –33. Breiter HC, Rauch SL (1996): Functional MRI and the study of OCD: From symptom provocation to cognitive-behavioral probes of cortico-striatal systems and the amygdala. Neuroimage 4:S127–138. Breiter HC, Rosen BR (1999): Functional magnetic resonance imaging of brain reward circuitry in the human. Ann N Y Acad Sci 877:523–547. Brix G, Zaers J, Adam LE, Bellemann ME, Ostertag H, Trojan H, et al (1997): Performance evaluation of a whole-body PET scanner using the NEMA protocol. National Electrical Manufacturers Association. J Nucl Med 38:1614 –1623. Buchel C, Dolan RJ, Armony JL, Friston KJ (1999): Amygdalahippocampal involvement in human aversive trace conditioning revealed through event-related functional magnetic resonance imaging. J Neurosci 19:10869 –10876. Bulik CM, Sullivan PF, Kendler KS (1998): Heritability of binge-eating and broadly defined bulimia nervosa. Biol Psychiatry 44:1210 –1218. Byrum CE, Ahearn EP, Krishnan KR (1999): A neuroanatomic model for depression. Prog Neuropsychopharmacol Biol Psychiatry 23:175–193. Casper RC (1990): Personality features of women with good outcome from restricting anorexia nervosa. Psychosom Med 52:156 –170. Charney DS, Deutch A (1996): A functional neuroanatomy of anxiety and fear: Implications for the pathophysiology and treatment of anxiety disorders. Crit Rev Neurobiol 10:419 – 446. Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD (1994): The Temperament and Character Inventory (TCI): A Guide to its Development and Use. St. Louis, MO: Center for Psychobiology of Personality, Washington University. Davidson RJ, Abercrombie H, Nitschke JB, Putnam K (1999): Regional brain function, emotion and disorders of emotion. Curr Opin Neurobiol 9:228 –234. Davis M (1992): The role of the amygdala in fear-potentiated startle: Implications for animal models of anxiety. Trend Pharmacol Sci 15:35–41. Devinsky O, Morrell MJ, Vogt BA (1995): Contributions of anterior cingulate cortex to behaviour. Brain 118:279 –306. De Vry J, Schreiber R (2000): Effects of selected serotonin 5-HT(1) and 5-HT(2) receptor agonists on feeding behavior: Possible mechanisms of action. Neurosci Biobehav Rev 24:341–353. Dwivedi Y, Pandey GN (1998): Quantitation of 5HT2A receptor mRNA in human postmortem brain using competitive RTPCR. Neuroreport 9:3761–3765. Eison AS, Mullins UL (1996): Regulation of central 5-HT2A receptors: A review of in vivo studies. Behav Brain Res 73:177–181. Ellison AR, Foong J (1998): Neuroimaging in Eating Disorders. In: Hoek HW, Treasure JL, Katzman MA, editors. Neurobiology in the Treatment of Eating Disorders. Chichester, UK: John Wiley. Ellison Z, Foong J, Howard R, Bullmore E, Williams S, Treasure J (1998): Functional anatomy of calorie fear in anorexia nervosa [letter]. Lancet 352:1192. G.K. Frank et al Evans AC, Collins DL, Mills SR, Brown ED, Kelly RL, Peters TM (1993): 3D statistical neuroanatomical models from 305 MRI volumes. Proceedings of the IEEE-Nuclear Science Symposium and Medical Imaging Conference, San Francisco, CA, November. Fichter MM, Herpertz S, Quadflieg N, Herpertz-Dahlmann B (1998): Structured Interview for Anorexic and Bulimic disorders for DSM-IV and ICD-10: updated (third) revision. Int J Eat Disord 24:227–249. Fichter MM, Pirke KM, Pollinger J, Wolfram GM, Brunner E (1990): Disturbances in the hypothalamo-pituitary-adrenal and other neuroendocrine axes in bulimia. Biol Psychiatry 27:1021–1037. First MB, Gibbon M, Spitzer RL, Williams JBW (1996): Users Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders—Research Version (SCID-I, version 2.0, February 1996 FINAL VERSION). New York: Biometrics Research Department, New York State Psychiatric Institute. Frackowiak RSJ, Friston KJ, Frith CD, Dolan RJ, Mazziotta J, editors (1997): Human Brain Function. San Diego, CA: Academic Press. Friston KJ (1995): Commentary and opinion: II. Statistical parametric mapping: Ontology and current issues. J Cereb Blood Flow Metab 15:361–370. Frost RO, Marten P, Lahart C, Rosenblate R (1990): The dimensions of perfectionism. Cogn Ther Res 14:449 – 468. Fujita M, Charney DS, Innis RB (2000): Imaging serotonergic neurotransmission in depression: Hippocampal pathophysiology may mirror global brain alterations. Biol Psychiatry 48:801–812. Garner DM (1993): Pathogenesis of anorexia nervosa. Lancet 341:1631–1635. Gordon CM, Dougherty DD, Fischman AJ, Emans SJ, Grace E, Lamm R, et al (2001): Neural substrates of anorexia nervosa: A behavioral challenge study with positron emission tomography. J Pediatr 139:51–57. Gordon I, Lask B, Bryant-Waugh R, Christie D, Timimi S (1997): Childhood-onset anorexia nervosa: Towards identifying a biological substrate. Int J Eat Disord 22:159 –165. Higley JD, Linnoila M (1997): Low central nervous system serotonergic activity is traitlike and correlates with impulsive behavior. A nonhuman primate model investigating genetic and environmental influences on neurotransmission. Ann N Y Acad Sci 836:39 –56. Hinney A, Remschmidt H, Hebebrand J (2000): Candidate gene polymorphisms in eating disorders. Eur J Pharmacol 410:147–159. Izquierdo I, Medina JH (1997): Memory formation: The sequence of biochemical events in the hippocampus and its connection to activity in other brain structures. Neurobiol Learn Mem 68:285–316. Katzman DK, Zipursky RB, Lambe EK, Mikulis DJ (1997): A longitudinal magnetic resonance imaging study of brain changes in adolescents with anorexia nervosa. Arch Ped Adolesc Med 151:793–797. Kaye WH (1997): Anorexia and bulimia nervosa, obsessional behavior, and serotonin. In: Kaye WH, Jimerson DC, editors. Eating Disorders. London: Balliere’s Tindell. Serotonin Receptor Activity in Anorexia BIOL PSYCHIATRY 2002;52:896 –906 905 Kaye WH, Frank GK, Meltzer CC, Price JC, McConaha CW, Crossan PJ (2001): Altered serotonin 2A receptor activity in women who have recovered from bulimia nervosa. Am J Psychiatry 158:1152–1155. Marrazzi MA, Mullings-Britton J, Stack L, Powers RJ, Lawhorn J, Graham V, et al (1990): Atypical endogenous opioid systems in mice in relation to an auto-addiction opioid model of anorexia nervosa. Life Sci 47:1427–1435. Kaye WH, Gendall K, Strober M (1998a): Serotonin neuronal function and selective serotonin reuptake inhibitor treatment in anorexia and bulimia nervosa. Biol Psychiatry 44:825–838. McAllister TW (1992): Neuropsychiatric sequelae of head injuries. Psychiatr Clin North Am 15:395–413. Kaye WH, Greeno CG, Moss H, Fernstrom J, Fernstrom M, Lilenfeld LR, et al (1998b): Alterations in serotonin activity and psychiatric symptomatology after recovery from bulimia nervosa. Arch Gen Psychiatry 55:927–935. Kaye WH, Gwirtsman HE, George DT, Ebert MH (1991): Altered serotonin activity in anorexia nervosa after long-term weight restoration: Does elevated cerebrospinal fluid 5-hydroxyindoleacetic acid level correlate with rigid and obsessive behavior? Arch Gen Psychiatry 48:556 –562. Meltzer CC, Reynolds CF (1999): In vivo assessment of aging changes in serotonin function [letter; comment]. Neuropsychopharmacology 21:323–324. Metropolitan Life Insurance Company (1959): New weight standards for men and women. Meyer JH, Kapur S, Eisfeld B, Brown GM, Houle S, DaSilva J, et al (2001): The effect of paroxetine on 5-HT(2A) receptors in depression: an [(18)F]setoperone PET imaging study. Am J Psychiatry 158:78 –85. Kaye WH, Gwirtsman HE, George DT, Jimerson DC, Ebert MH (1988): CSF 5-HIAA concentrations in anorexia nervosa: Reduced values in underweight subjects normalize after weight gain. Biol Psychiatry 23:102–105. Meyer JH, Kapur S, Houle S, DaSilva J, Owczarek B, Brown GM (1999): Prefrontal cortex 5-HT2 receptors in depression: An [18F]setoperone PET imaging study. Am J Psychiatry 156:1029 –1034. Kennedy SH, Javanmard M, Vaccarino FJ (1997): A review of functional neuroimaging in mood disorders: Positron emission tomography and depression. Can J Psychiatry 42:467– 475. Nieuwenhuys R, Voogd J, van Huijzen C (1988): The Human Central Nervous System. Heidelberg, Germany: SpringerVerlag. Klump KL, Bulik CM, Pollice C, Halmi KA, Fichter MM, Berrettini WH, et al (2000): Temperament and character in women with anorexia nervosa. J Nerv Ment Dis 188:559 – 567. Lambe EK, Katzman DK, Mikulis DJ, Kennedy SH, Zipursky RB (1997): Cerebral gray matter volume deficits after weight recovery from anorexia nervosa. Arch Gen Psychiatry 54:537–542. Leibowitz SF, Shor-Posner G (1986): Brain serotonin and eating behavior. Appetite 7(Suppl):1–14. Lemaire C, Cantineau R, Guillaume M, Plenevaux A, Christiaens L (1991): Fluorine-18-altanserin: A radioligand for the study of serotonin receptors with PET: Radiolabeling and in vivo biologic behavior in rats. J Nucl Med 32:2266 –2272. Lilenfeld LR, Kaye WH, Greeno CG, Merikangas KR, Plotnicov K, Pollice C, et al (1998): A controlled family study of anorexia nervosa and bulimia nervosa: Psychiatric disorders in first-degree relatives and effects of proband comorbidity. Arch Gen Psychiatry 55:603–610. Logan J, Fowler JS, Volkow ND, Wolf AP, Dewey SL, Schlyer DJ, et al (1990): Graphical analysis of reversible radioligand binding from time-activity measurements applied to [N-11Cmethyl]-(-)-cocaine PET studies in human subjects. J Cereb Blood Flow Metab 10:740 –747. Lopresti B, Holt D, Mason S, Huang Y, Ruszkiewicz J, Perevuznik J, et al (1998): Characterization of the radiolabeled metabolites of [18F]altanserin: Implications for kinetic modeling. In: Carson R, Daube-Witherspoon M, Herscovitch P, editors. Quantitative Brain Imaging with Positron Emission Tomography. San Diego, CA: Academic Press, pp 293–298. Lucki I (1998): The spectrum of behaviors influenced by serotonin. Biol Psychiatry 44:151–162. Mann JJ (1999): Role of the serotonergic system in the pathogenesis of major depression and suicidal behavior. Neuropsychopharmacology 21(2 Suppl):99S–105S. O’Dwyer AM, Lucey JV, Russell GF (1996): Serotonin activity in anorexia nervosa after long-term weight restoration: Response to D-fenfluramine challenge. Psychol Med 26:353– 359. Palmer HD, Jones MS (1939): Anorexia nervosa as a manifestation of compulsive neurosis. Arch Neurol Psychiatry 856 – 860. Pazos A, Probst A, Palacios JM (1987): Serotonin receptors in the human brain—IV: Autoradiographic mapping of serotonin-2 receptors. Neuroscience 21:123–139. Price JC, Lopresti BJ, Meltzer CC, Smith GS, Mason NS, Huang Y (2001): Analyses of [(18)F]altanserin bolus injection PET data. II: Consideration of radiolabeled metabolites in humans. Synapse 41:11–21. Reiman EM, Raichle ME, Butler FK, Herscovitch P, Robins E (1984): A focal brain abnormality in panic disorder, a severe form of anxiety. Nature 310:683–685. Rioux A, Fabre V, Lesch KP, Moessner R, Murphy DL, Lanfumey L (1999): Adaptive changes of serotonin 5-HT2A receptors in mice lacking the serotonin transporter. Neurosci Lett 262:113–116. Roser W, Bubl R, Buergin D, Seelig J, Radue EW, Rost B (1999): Metabolic changes in the brain of patients with anorexia and bulimia nervosa as detected by proton magnetic resonance spectroscopy. Int J Eating Disord 26:119 –136. Roth BL, Berry SA, Kroeze WK, Willins DL, Kristiansen K (1998): Serotonin 5-HT2A receptors: Molecular biology and mechanisms of regulation. Crit Rev Neurobiol 12:319 –338. Sandor S, Leahy R (1997): Surface-based labeling of cortical anatomy using a deformable atlas. IEEE Trans Med Imaging 16:41–54. Saucier C, Morris SJ, Albert PR (1998): Endogenous serotonin-2A and -2C receptors in Balb/c-3T3 cells revealed in serotonin-free medium: Desensitization and down-regulation by serotonin. Biochem Pharmacol 10:1347–1357. 906 BIOL PSYCHIATRY 2002;52:896 –906 Schneider F, Weiss U, Kessler C, Muller-Gartner HW, Posse S, Salloum JB, et al (1999): Subcortical correlates of differential classical conditioning of aversive emotional reactions in social phobia. Biol Psychiatry 45:863–871. Simansky KJ (1996): Serotonergic control of the organization of feeding and satiety. Behav Brain Res 73:37–42. Smith GS, Price JC, Lopresti BJ, Huang Y, Simpson N, Holt D, et al (1998): Test-retest variability of serotonin 5-HT2A receptor binding measured with positron emission tomography and [18F]altanserin in the human brain. Synapse 30:380 – 392. Spielberger CD, Gorsuch RL, Lushene RE (1970): STAI Manual for the State Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press. Spinks TJ, Jones T, Bailey DL, Townsend DW, Grootoonk S, Bloomfield PM (1992): Physical performance of a positron tomograph for brain imaging with retractable septa. Phys Med Biol 37:1637–1655. Srinivasagam NM, Kaye WH, Plotnicov KH, Greeno C, Weltzin TE, Rao R (1995): Persistent perfectionism, symmetry, and exactness after long-term recovery from anorexia nervosa. Am J Psychiatry 152:1630 –1634. Staley JK, Malison RT, Innis RB (1998): Imaging the Serotonergic System: Interactions of neuroanatomical and functional abnormalities of depression. Biol Psychiatry 44:354 – 549. Staley JK, Van Dyck CH, Tan PZ, Al Tikriti M, Ramsby Q, Klump H, et al (2001): Comparison of [(18)F]altanserin and [(18)F]deuteroaltanserin for PET imaging of serotonin(2A) receptors in baboon brain: Pharmacological studies. Nucl Med Biol 28:271–279. Stockmeier CA (1997): Neurobiology of serotonin in depression and suicide. Ann N Y Acad Sci 836:220 –232. Strober M, Freeman R, Lampert C, Diamond J, Kaye W (2000): Controlled family study of anorexia nervosa and bulimia nervosa: Evidence of shared liability and transmission of partial syndromes. Am J Psychiatry 157:393–401. Strupp BJ, Weingartner H, Kaye W, Gwirtsman H (1986): Cognitive processing in anorexia nervosa: A disturbance in automatic information processing. Neuropsychobiology 15:89 –94. G.K. Frank et al Sullivan PF (1995): Mortality in anorexia nervosa. Am J Psychiatry 152:1073–1074. Treasure J, Campbell I (1994): The case for biology in the aetiology of anorexia nervosa. Psychol Med 24:3–8. Tucker DM, Luu P, Pribram KH (1995): Social and emotional self-regulation. Ann N Y Acad Sci 769:213–239. Van der Linden G, van Heerden B, Warwick J, Wessels C, van Kradenburg J, Zungu-Dirwayi N, Stein DJ (2000): Functional brain imaging and pharmacotherapy in social phobia: Single photon emission computed tomography before and after treatment with the selective serotonin reuptake inhibitor citalopram. Prog Neuropsychopharmacol Biol Psychiatry 24:419 –438. Walsh BT, Devlin MJ (1998): Eating disorders: Progress and problems. Science 280:1387–1390. Ward A, Brown N, Lightman S, Campbell IC, Treasure J (1998): Neuroendocrine, appetitive and behavioural responses to d-fenfluramine in women recovered from anorexia nervosa. Br J Psychiatry 172:351–358. Wolfe BE, Metzger ED, Jimerson DC (1997): Research update on serotonin function in bulimia nervosa and anorexia nervosa. Psychopharmacol Bull 33:345–354. Woods RP, Cherry SR, Mazziotta JC (1992): Rapid automated algorithm for aligning and reslicing PET images. J Comput Assist Tomogr 16:620 – 633. Woods RP, Mazziotta JC, Cherry SR (1993): MRI-PET registration with automated algorithm. J Comput Assist Tomogr 17:536 –546. Yatham LN, Liddle PF, Shiah IS, Scarrow G, Lam RW, Adam MJ, et al (2000): Brain serotonin2 receptors in major depression: A positron emission tomography study. Arch Gen Psychiatry 57:850 –858. Zald DH, Kim SW (1996): Anatomy and function of the orbital frontal cortex, II: Function and relevance to obsessivecompulsive disorder. J Neuropsychiatry Clin Neurosci 8:249 –261. Zalla T, Koechlin E, Pietrini P, Basso G, Aquino P, Sirigu A, Grafman J (2000): Differential amygdala responses to winning and losing: A functional magnetic resonance imaging study in humans. Eur J Neurosci 12:1764 –1770.