Document 12006433
advertisement

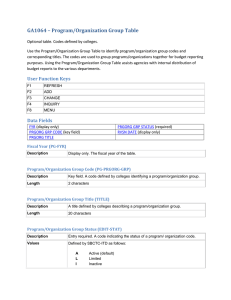
Appetite (2001) 37, 9±14 doi:10.1006/appe.2001.0407, available online at http://www.idealibrary.com on 1 Original Article Reduced gastrin releasing peptide in cerebrospinal fluid after recovery from bulimia nervosa G.K. Franka,W.H. Kayea, E.E. Ladenheimb and C. McConahaa a b School of Medicine, Department of Psychiatry,Western Psychiatric Institute and Clinic,University of Pittsburgh; School of Medicine, Department of Psychiatry and Behavioral Sciences, The Johns Hopkins University, Baltimore (Received 20 September 2000, revision11April 2001, accepted in revised form 20 April 2001) People with anorexia (AN) and bulimia nervosa (BN) have altered patterns of eating. It is possible that alterations of the neuropeptide gastrin releasing peptide (GRP), a bombesin (BBS) -like peptide with potent central anorexigenic activity, could contribute to disturbed eating behavior. To avoid the confounding effects of pathologic eating behavior, we measured cerebrospinal fluid (CSF) GRP concentrations in women who were long-term recovered ( >1 year, normal weight, and regular menstrual cycles, no bingeing or purging) from AN (REC AN, N 12) or BN (REC BN, N 21) compared to healthy control women (NC, N 15). CSF GRP was significantly lower (2 941(3), p < 001) in REC BN (96 31 pg/ml) compared to NC (134 55 pg/ml) and REC AN (116 29 pg/ ml). Persistent GRP abnormalities after recovery from BN raise the possibility that this alteration might be traitrelated and contribute to episodic hyperphagia in BN. # 2001 Academic Press Introduction The eating disorders (EDs) anorexia (AN) and bulimia nervosa (BN) are characterized by disturbed eating behaviors and comorbid disturbances of mood, impulse control, and temperament. Women with AN show a pattern of food restriction and emaciation; however, some AN are pure food restrictors, whereas others also show binge-purging type behaviors. Women with BN are usually at a normal body weight, and engage in a pattern Supported in part by grants from NIMH #2 R01 MH 42984-09 ``The Neurobiology of Feeding Behavior in Bulimia''; Children's Hospital Clinical Research Center, Pittsburgh, PA (#5M01 RR00084), and NIMH #2 R01 MH 46001-07A1 ``Serotonin: A Trait Disturbance in Anorexia Nervosa''. Address correspondence to: Walter H. Kaye, M.D., University of Pittsburgh, Western Psychiatric Institute and Clinic, Room E-724, 3811 O'Hara Street, Pittsburgh, PA 15213, U. S. A. Fax: 1 412 624 6618. Email: kayewh@msx.upmc.edu 0195±6663/01/040009+06 $35.00/0 of food restriction alternating with regular binge-purge episodes. The etiology of EDs is not known (American Psychiatric Association, 1994). Recent studies suggest that EDs are familial and that a genetic predisposition might contribute to their etiology (Lilenfeld et al., 1998; Strober et al., 2000). A number of neuropeptides contribute to the modulation of appetite regulation (Kalra et al., 1999). It is theoretically possible that a disturbance of the modulation of one or more neuropeptide systems plays a role in disturbed eating behavior in humans. One neuropeptide system of interest is human gastrin releasing peptide (GRP). GRP is a 27 amino acid peptide that shares a similar decapeptide with bombesin (BBS; Brown et al., 1980), and belongs to the family of ``bombesin-like peptides.'' BBS was first isolated from amphibian skin (Anastasi et al., 1971) and showed anorexigenic effects when administered peripherally or centrally in mammals (Gibbs and Smith, 1988). GRP is not as potent as BBS, but otherwise has similar effects (Morley et al., 1985). Peripheral and central # 2001 Academic Press 10 G. K. Frank et al. administration of GRP attenuates food intake in mammals and humans (Bray 1995; Flynn, 1994). Peripherally, BBS-like receptors are distributed throughout the gastrointestinal (GI) tract, with receptors that have specifically high affinity for GRP (von Schrenck et al., 1990). They take part in the regulation of GI hormone and enzyme secretion, cell growth, smooth muscle activity and blood glucose levels (Dietrich, 1994; Walsh et al., 1981). In the central nervous system (CNS), distinct BBS-like receptor subtypes have been identified in brain tissue such as the bed nucleus of the stria terminalis, the olfactory tubercle, the putamen and neocortex, with a neuromedin B and a GRP preferring subtype (Ladenheim et al., 1992; Wolf & Moody, 1985). Both subtypes have been implicated in the modulation of BBS-like peptide induced food suppression (Ladenheim et al., 1996). In addition, central GRP also modulates temperature regulation and grooming behavior in animals (Cowan, 1988). Disturbances of neuropeptides could be a consequence of disturbed eating behavior or malnutrition, or pre-morbid traits that contribute to a vulnerability to develop an ED. Determining whether abnormalities are a consequence or a potential antecedent of pathological feeding behavior is a major question in the study of eating disorders. It is impractical to study people with ED prospectively due to the young age of onset and difficulty in pre-morbid identification of people who will develop an ED. Therefore, we decided to study women who had recovered for more than a year from AN or BN. Any persistent psychobiological abnormalities might be trait-related and potentially have contributed to the pathogenesis of this disorder. In this study we measured cerebrospinal fluid (CSF) values of human GRP, a human BBS-like peptide. We hypothesized that AN would have increased and BN decreased CSF values of GRP. Materials and methods Thirty-three women who had previously met DSM-IV criteria for an ED were recruited: 21 women recovered from normal weight BN (REC BN), and 12 subjects recovered from binge eating/purging (eight) or restricting type (four) AN (REC AN). The REC BN women had never had AN. Recovered ED subjects were compared to 15 female normal controls (NC), who were recruited through advertisements in local newspapers and who were without lifetime psychiatric or major medical illnesses. In the year before the study, all participating recovered subjects had to maintain a body weight of > 90% average body weight (ABW; Metropolitan Life Insurance, 1959); have regular menstrual cycles; have not binged, purged (i.e. not engaged in self-induced vomiting, the use of laxatives or diuretics), excessively exercised, or engaged in restrictive eating patterns; and have not met criteria for substance-use related disorders. Subjects were free of medication for 6 weeks prior to the study and gave informed consent. The control women (NC) had no history of an eating disorder or any psychiatric, medical, or neurologic illness. They had normal menstrual cycles, and had been within a normal weight range since menarche. They also had no first degree relatives with an eating disorder. Methods and psychological assessment data are described in detail elsewhere (Kaye et al., 1998a, 1999). For many of the subjects, CSF 5-hydroxyindole acetic acid had been measured previously. A lumbar puncture (LP) for obtaining CSF samples was performed during the first 10 days of the follicular phase of the menstrual cycle. Subjects were admitted to a research laboratory on the Eating Disorders Unit of Western Psychiatric Institute and Clinic at 9 a.m. on the day prior to the LP for adaptation to the laboratory and for psychological assessments. Subjects fasted overnight, and the LP was performed the next day between 9 a.m. and 9:30 a.m. LP samples were frozen in liquid nitrogen and stored at ÿ80 C. For the GRP assay a commercial kit for radio immuno assay (RAI) from Peninsula Laboratories, Inc., San Carlos, CA, was used. The antibody in that kit shows 100% cross reactivity with human GRP, as well as with BBS. No cross reactivity is reported for human gastrin I, human big gastrin1 peptide, gastric inhibitory peptide, or substance P. The variability of the assay between runs was 4 3% (mean SD). Plasma -hydroxybutyrate (BHBA), a ketone body, was assessed as an index of starvation. BHBA was measured by the enzymatic method of Williamson et al. (1962). Statistical analyses were performed using the SPSS software package (SPSS, Chicago, IL; Barcikowski 1984). Data exploration assessed whether data were normally distributed (Shapiro-Wilk test). When the assumption of normality was met, One-Way ANOVA assessed whether group means were similar, and Scheffe's post hoc tests compared individual group differences. All variables aside from age and CSF GRP were normally distributed. When the assumption of normality was not met, Kruskal-Wallis test assessed three group comparisons, and Mann-Whitney U tests assessed individual group differences. Correlations were investigated using Pearson Correlations for normally distributed and Spearman Correlation Coefficients for non-normally distributed variables. All data are expressed as mean standard deviation (SD). Group differences were considered significant if p < 005. Gastrin releasing peptide and bulimia nervosa 11 Results Age was similar between groups (Table 1). However, % ABW at the time of the study was higher in REC BN compared with NC and REC AN, and in NC 35 30 CSF GRP (pmol/ml) 25 20 15 compared with REC AN. Lifetime high % ABW was higher in REC BN compared with NC and REC AN. Lifetime low % ABW was lower in REC AN compared with NC and REC BN. BHBA was similar between groups. There was no difference between length of recovery between groups. One CSF GRP value for the NC group was excluded as a non-true outlier (195 pg/ml). There was a significant difference between group CSF GRP levels (Table 1). Figure 1 shows a scatterplot with the distribution of the GRP values across groups. The CSF GRP in REC BN showed some overlap in distribution with NC and AN. However, the majority of CSF GRP data points in REC BN women was below 10 pmol/ml (15/21), whereas the majority of data points for NC (12/15) and REC AN (9/ 12) was above 10 pmol/ml. Separate comparisons showed lower CSF GRP values in REC BN compared to NC (p 0003; when applying Bonferroni correction p < 0009), and REC AN (p < 005, p 01 with Bonferroni correction), and similar values when comparing NC and REC AN (p 04). There was no significant relationship between CSF GRP and age, body weight, or duration of recovery. Discussion 10 5 0 NC (N = 15) REC AN (N = 12) REC BN (N = 21) Figure 1. Scatterplot comparing the distribution of cerebrospinal fluid (CSF) gastrin releasing peptide (GRP) between groups. NC, normal controls; REC AN, recovered anorexic women; REC BN; recovered bulimic women. Consistent with a portion of our hypothesis, REC BN women had reduced CSF GRP levels although no abnormalities were found in REC AN subjects. To our knowledge, BBS-like immunoreactivity has not been previously assessed in people recovered from an ED. However, subjects who were studied while ill with AN had normal CSF BBS. In addition, schizophrenics had lower CSF BBS, whereas CSF BBS was not related to anxiety, depression, or mania (Gerner & Yamada, 1982; Gerner et al., 1985; Saiz Ruiz et al., 1992). The finding of reduced CSF GRP levels after recovery from BN raises the question of whether this Table 1. Clinical and biological data on subjects NC (N 15) Age (years) Length of recovery (months) % ABW High % ABW Low % ABW BHBA (mmol/ml) CSF GRP (pg/ml) 222 31 Ð 103 8a,c 108 7c 95 7c 1328 967 134 55c REC AN (N 12) 239 33 33 21 94 7b,c 105 13c 68 8d 2014 1505 116 29 REC BN (N 21) 267 64 39 25 112 10d 126 15d 96 8c 1131 1074 96 31d p < 2 59 F 05 F 181 F 146 F 556 F 18 2 94 ns ns 000 000 000 ns 001 NC, Normal control women; REC AN, women recovered from anorexia nervosa; REC BN women recovered from bulimia nervosa; % ABW average body weight; BHBA; -hydroxybutyric acid; EDI (numbers in parentheses indicate available number of subjects data), Eating Disorders Inventory-2. All data are expressed as mean SD; One way ANOVA (F, df 2) for normally distributed values with Scheffe's test for post hoc comparisons; Kruskall-Wallis test (2df 2) for 3-group comparison of non-normal distributed values with Mann-Whitney U test for post hoc comparison using Bonferroni correction; p < 005 for a vs. b, p < 001 for c vs. d. 12 G. K. Frank et al. neuropeptide is involved in the pathophysiology, or even the etiology, of BN. GRP is an anorexigenic agent. Recent animal literature suggests alterations of BBS activity in response to feeding that is localized to the hypothalamus and nucleus accumbens (Plamondon et al., 1997). Mice lacking the BBS receptor subtype-3, though with low affinity for BBS, developed obesity, a reduced metabolic rate, and hyperphagia (OhkiHamazaki et al., 1997). One interpretation of these data is that BN women have reduced satiety signaling. In support of this possibility is that women with BN often have increased lifetime high body weight compared to NC. In addition, elevated taste pleasantness for sweetness in BN (Franko et al., 1994) could be related to alterations in BBS-like peptide activity (Yamada et al., 1999). Based on the study design, we can only speculate about the source of CSF GRP measured. Peripheral BBS-like peptides may not be able to readily cross the blood brain barrier, but still might be able to access the brain (Merali et al., 1999). In animals, however, GRPlike peptides have been shown to be produced in central nerve fibers, and high GRP and GRP-like expression was found in the hypothalamus, the nucleus of the solitary tract, and in the trigeminal nucleus (Flynn, 1994; Moody et al., 1980). Thus, it is possible that the CSF GRP measured in this study was mainly released by centrally located nerve fibers. However, we cannot exclude that CSF GRP from peripheral organs, such as the lungs (Jaramillo et al., 1995), or the acid secreting glands of the stomach (Sjovall et al., 1990) contributed to the CSF GRP levels. Values of a number of neuropeptide systems have been found to be abnormal in ill AN and BN subjects such as corticotropin releasing hormone (CRH), opioids or proopiomelanocortin (POMC), leptin, neuropeptide Y (NPY), and peptide YY (PYY). However, values of these systems normalize after recovery (Gendall et al., 1999). Still, REC BN subjects have been found to have abnormalities of CNS serotonin (5-HT). BBS-like receptors are associated with the 5-HT system (Woodruff et al., 1996), and GRP has been found to excite 5-HT sensitive mesencephalic neurons in the dorsal raphe of rats in vitro (Pinnock & Woodruff, 1991; Pinnock et al., 1994). However, it has yet to be determined what functional implications such an interaction might have. GRP activity may be irreversibly attenuated in response to alcohol consumption (Madeira & PaulaBarbosa, 1999). On the other hand, the BBS peptides act as potent inhibitors of not just food but also alcohol ingestion in the rat (Kulkosky et al., 1985, 1993). It is well known that there is a high comorbidity of BN and alcohol abuse or dependence (Lilenfeld et al., 1998). We therefore divided REC BN women in to two groups: subjects with history of alcohol abuse (AA) or dependence (AD) (N 10), and REC BN women without such history (N 11). REC BN with a history of AA or AD (89 41) tended to have lower CSF GRP than REC BN without alcohol history (105 19), however, this was not statistically significant. In addition, we compared the REC BN without a history of AA or AD with the NC women. We still found CSF GRP in REC BN women significantly lower than in the NC group (p 003). In terms of limitations, this is a relatively small number of subjects. Only four of the REC AN women were pure food restrictors. The remaining REC AN subjects were binge eating-purging type AN. Even in the absence of symptoms according to the DSM-IV (American Psychiatric Association, 1994), elevated scores on measures for ED related pathology, depression, anxiety, and obsessionality occur in both recovered AN and BN women (Kaye et al., 1998a; Pollice et al., 1997; Srinivasagam et al., 1995). The REC BN women in this study had persistent symptoms that were mild to moderate in severity compared to the ill state; those data have been published previously (Kaye et al., 1998a). Our experience suggests that these are traits that persist after recovery (Kaye et al., 1998b). We did not find a relationship between CSF GRP and subtypes of AN, but the very small sample size makes such analyses difficult. In addition, future studies should investigate whether CSF values actually reflect activity of this peptide system in the brain, or other factors, such as peptide metabolism. Finally, it is possible that persistent disturbances of CSF GRP could be a secondary effect of years of malnutrition or other state-related factors. The design of this study, however, does not permit answering this question. Taken together, these data suggest that CSF GRP is reduced in CSF of REC BN. Lower CSF GRP in this group could be a trait-related disturbance that might add to hyperphagic behavior, and thus to the pathophysiology of this illness. However, this finding has to be replicated in a larger subject group. In addition, a possible interaction of BN and alcohol abuse on CSF GRP has to be investigated further. CSF GRP was not significantly reduced in REC AN. This supports that AN and BN may have, at least in part, different pathophysiologies. References American Psychiatric Association. (1994). Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Press. Anastasi, A., Erspamer, V. & Bucci, M. (1971). Isolation and structure of bombesin and alytesin, 2 analogous active peptides from the skin of the European amphibians Bombina and Alytes. Experientia 27, 166±167. Gastrin releasing peptide and bulimia nervosa 13 Barcikowski, R. S. (Ed.) (1984). Computer Packages and Research Design, vol. 3: SPSS & SPSSX. Lanham, MD: University Press of America. Bray, G. A. (1995). Nutrient intake is modulated by peripheral peptide administration. Obesity Research 3 (Suppl 4), 569S±572S. Brown, M., Marki, W., & Rivier, J. (1980). Is gastrin releasing peptide mammalian bombesin? Life Sciences 27, 125± 128. Cowan, A. (1988). Behavioral effects of bombesin. Annals of the New York Academy of Sciences 547, 204±209. Dietrich, J. B. (1994). Neuropeptides, antagonists and cell proliferation: bombesin as an example. Cellular and Molecular Biology 40, 731±746. Flynn, F. W. (1994). Bombesin-like peptides in the regulation of ingestive behavior. Annals of the New York Academy of Sciences 739, 120±134. Franko, D. L., Wolfe, B. E., & Jimerson, D. C. (1994). Elevated sweet taste pleasantness ratings in bulimia nervosa. Physiology and Behavior 56, 969±973. Gendall, K. A., Kaye, W. H., Altemus, M., McConaha, C. W., & La Via, M. C. (1999). Leptin, neuropeptide Y, and peptide YY in long-term recovered eating disorder patients. Biological Psychiatry 46, 292±299. Gerner, R. H., & Yamada, T. (1982). Altered neuropeptide concentrations in cerebrospinal fluid of psychiatric patients. Brain Research 238, 298±302. Gerner, R. H., van Kammen, D. P., & Ninan, P. T. (1985). Cerebrospinal fluid cholecystokinin, bombesin and somatostatin in schizophrenia and normals. Progress in Neuro-psychopharmacology and Biological Psychiatry 9, 73±82. Gibbs, J. & Smith, G. P. (1988). The actions of bombesin-like peptides on food intake. Annals of the New York Academy of Sciences 547, 210±216. Jaramillo, M. A., Gutierrez, J. A. & Margraf, L. R. (1995). Pulmonary releasing peptide expression in anencephaly. Pediatric Pathology and Laboratory Medicine 15, 377± 387. Kalra, S. P., Dube, M. G., Pu, S., Xu, B., Horvath, T. L., & Kalra, P. S. (1999). Interacting appetite-regulating pathways in the hypothalamic regulation of body weight. Endocrine Reviews 20, 68±100. Kaye, W. H., Greeno, C. G., Moss, H., Fernstrom, J., Fernstrom, M., Lilenfeld, L. R. R., Weltzin, T. E., & Mann, J. J. (1998a). Alterations in serotonin activity and psychiatric symptoms after recovery from bulimia nervosa. Archives of General Psychiatry 55, 927±935. Kaye, W., Gendall, K. & Strober, M. (1998b). Serotonin neuronal function and selective serotonin reuptake inhibitor treatment in anorexia and bulimia nervosa. Biological Psychiatry 44, 825±838. Kaye, W. H., Frank, G. K., McConaha, C. (1999). Altered dopamine activity after recovery from restricting-type anorexia nervosa. Neuropsychopharmacology 21, 503± 506. Kulkosky, P. J., Roque, M. & Sanchez, M. R. (1985). Bombesin and litorin inhibit ethanol intake. Peptides 6 (Suppl 2) 103±105. Kulkosky, P. J., Clayborne, Y. J. & Sandoval, S. L. (1993). Cholecystokinin and bombesin inhibit ethanol and food intake in rats selectively bred for ethanol sensitivity Alcoholism: Clinical and Experimental Research 17, 545±551. Ladenheim, E. E., Jensen, R. T., Mantey S. A. & Moran, T. H. (1992). Distinct distributions of two bombesin receptor subtypes in the rat central nervous system. Brain Research 593, 168±178. Ladenheim, E. E., Wirth, K. E. & Moran, T. H. (1996). Receptor subtype mediation of feeding suppression by bombesin-like peptides. Pharmacology, Biochemistry & Behavior 54, 705±711. Lilenfeld, L. R., Kaye, W. H., Greeno, C. G., Merikangas, K. R., Plotnicov, K. & Pollice, C. (1998). A controlled family study of anorexia nervosa and bulimia nervosa: Psychiatric disorders in first-degree relatives and effects of proband comorbidity. Archives of General Psychiatry 55, 603±610. Madeira, M. D., Paula-Barbosa, M. M. (1999). Effects of alcohol on the synthesis and expression of hypothalamic peptides. Brain Research Bulletin 48, 3±22. Merali, Z., McIntosh, J., & Anisman, H. (1999). Role of bombesin-related peptides in the control of food intake. Neuropeptides 33, 376±386. Metropolitan Life Insurance Company. (1959). New Weight Standards for Men and Women. Statistical Bulletin of Metropolitan Life Insurance Company. Moody, T. W., Thoa, N. B., O'Donohue, T. L. & Pert, C. B. (1980). Bombesin-like peptides in rat brain: localization in synaptosomes and release from hypothalamic slices. Life Sciences 26, 1707±1712. Morley, J. E., Bartness, T. J., Gosnell, B. A. & Levine, A. S. (1985). Peptidergic regulation of feeding. International Review of Neurobiology 27, 207±298. Ohki-Hamazaki, H., Watase, K., Yamamoto, K., Ogura, H., Yamano, M., Yamada, K. et al. (1997). Mice lacking bombesin receptor subtype-3 develop metabolic defects and obesity. Nature 390, 165±169. Pinnock, R. D. & Woodruff, G. N. (1991). Bombesin excites a subpopulation of 5-hydroxytryptamine-sensitive neurones in the rat dorsal raphe nucleus in vitro. Journal of Physiology 440, 55±65. Pinnock, R. D., Reynolds, T., Woodruff, G. N. (1994). Different types of bombesin receptors on neurons in the dorsal raphe nucleus and the rostral hypothalamus in rat brain slices in vitro. Brain Research 653, 119±124. Plamondon, H. & Merali, Z. (1997). Regulation of ingestion by CRF and bombesin-like peptides: distinct meal-related peptide level changes. American Journal of Physiology 272, R268±274. Pollice, C., Kaye, W. H., Greeno, C. G., Weltzin, T. E. (1997). Relationship of depression, anxiety, and obsessionality to state of illness in anorexia nervosa. International Journal of Eating Disorders, 21, 367±376. Saiz Ruiz, J., Carrasco Perera, J. L. & Hernanz, A. (1992). Plasma neuropeptides in affective and anxiety disorders. Archivos de Neurobiologia 55, 1±5. Sjovall, M., Ekblad, E., Lundell, L. & Sundler, F. (1990). Gastrin Releasing Peptide: neuronal distribution and spatial relation to endocrine cells in the human upper gut. Regulatory Peptides 28, 47±55. Srinivasagam, N. M., Plotnicov, K. H., Greeno, C., Weltzin, T. E., Rao, R. & Kaye, W. H. (1995). Persistent perfectionism, symmetry, and exactness in anorexia nervosa after long-term recovery. American Journal of Psychiatry 152,1630±1634. Strober, M., Freeman, R., Lampert, C., Diamond, J, Kaye, W. H. (2000). Controlled family study of anorexia 14 G. K. Frank et al. nervosa and bulimia nervosa: Evidence of shared liability and transmission of partial syndromes. American Journal of Psychiatry 157, 393±401. von Schrenck, T., Wang, L. H., Coy, D. H., Villanueva, M. L., Mantey, S., Jensen, R. T. (1990). Potent bombesin receptor antagonists distinguish receptor subtypes. American Journal of Physiology 259, G468±G473. Walsh, J. H., Kovacs, T. O., Maxwell, V., & Cuttitta, F. (1988). Bombesin-like peptides as regulators of gastric function. Annals of the New York Academy of Sciences 547, 217±224. Williamson, D. H., Mellanby, J. & Krebs, H. A. (1962). Enzymatic determination of D(ÿ) hydroxybutyric acid and acetoacetic acid in blood. Biochemistry Journal 82, 90±96. Wolf, S. S. & Moody, T. W. (1985). Receptors for GRP/ bombesin-like peptides in the rat forebrain. Peptides 6 (Suppl 1): 111±114. Woodruff, G. N., Hall, M. D., Reynolds, T. & Pinnock, R. D. (1996). Bombesin receptors in the brain. Annals of the New York Academy of Sciences 780, 223±243. Yamada, K., Wada, E., Imaki, J., Ohki-Hamazaki, H. Wada, K. (1999). Hyperresponsiveness to palatable and aversive taste stimuli in genetically obese (bombesin receptor subtype-3-deficient) mice. Physiology & Behavior 66, 863±867.