Regional cerebral blood flow after recovery from bulimia nervosa
advertisement

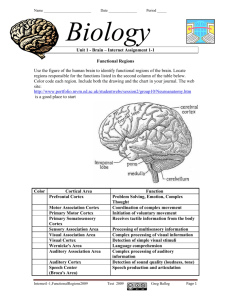
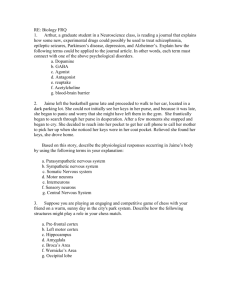
Psychiatry Research: Neuroimaging Section 100 Ž2000. 31᎐39 Regional cerebral blood flow after recovery from bulimia nervosa Guido K. Frank, Walter H. KayeU , Phil Greer, Carolyn C. Meltzer, Julie C. Price Western Psychiatric Institute and Clinic, Uni¨ ersity of Pittsburgh Medical Center, 3811 O’Hara Street, E-724, Pittsburgh, PA 15213, USA Received 27 June 2000; received in revised form 13 September 2000; accepted 14 September 2000 Abstract When ill, women with bulimia nervosa ŽBN. show alterations of regional cerebral blood flow ŽrCBF.. In this study we investigated rCBF in nine women in long-term recovery from BN ŽRBN, n s 9., i.e. more than 1 year without bingeingrpurging behavior, normal weight, stable food intake, and regular menses, and compared them with age-matched healthy control women ŽCW, n s 13.. Positron emission tomography ŽPET. was used for the assessment of rCBF. There were no significant differences in rCBF between groups. However, rCBF was significantly inversely related to length of recovery in RBN for the left and right prefrontal cortex ŽBA 10., right medial orbital frontal cortex ŽBA 11., left subgenual cingulate ŽBA 25., right anterior cingulate ŽBA 32., left sensory motor cortex ŽBA 1,2,3,4., left and right lateral temporal ŽBA 21., and left occipital cortex ŽBA 17., as well as left thalamus. This finding suggests that previously reported alterations in rCBF during the ill state of BN may be a state-related phenomenon that remits with recovery. It is also possible that reductions in rCBF occur in a later stage of recovery from BN. 䊚 2000 Elsevier Science Ireland Ltd. All rights reserved. Keywords: Bulimia nervosa; Recovery; Cerebral blood flow; Positron emission tomography U Corresponding author. Tel.: q1-412-624-3507; fax: q1-412-624-6618. E-mail address: kayewh@msx.upmc.edu ŽW.H. Kaye.. 0925-4927r00r$ - see front matter 䊚 2000 Elsevier Science Ireland Ltd. All rights reserved. PII: S 0 9 2 5 - 4 9 2 7 Ž 0 0 . 0 0 0 6 9 - X 32 G.K. Frank et al. r Psychiatry Research: Neuroimaging 100 (2000) 31᎐39 1. Introduction Bulima nervosa ŽBN. is a psychiatric disorder characterized by regular bingeing and purging behavior that typically has its onset during adolescence ŽAmerican Psychiatric Association, 1994.. Psychosocial factors have been implicated in the development of this disorder ŽStice, 1999; Troop and Treasure, 1997.. However, family and genetic studies suggest a hereditary transmission of BN ŽKendler et al., 1991; Lilenfeld and Kaye, 1998.. In addition, disturbances of the serotonin system after long-term recovery suggest a biologic traitrelated disturbance in BN ŽKaye et al., 1998; Smith et al., 1999.. Functional brain imaging provides us with the opportunity to investigate brain mechanisms in vivo, and helps localize regional disturbances associated with psychiatric disorders ŽWeight and Bigler, 1998.. Several brain-imaging studies have investigated cerebral blood flow and metabolism in BN. Nozoe et al. Ž1995. found that regional cerebral blood flow ŽrCBF. in acutely ill BN was elevated in inferior frontal and left temporal cortical areas, and changed in relation to a test meal. It was suggested that frontal andror temporal cortical areas might be involved in the pathophysiology of BN. Most recently, it was proposed that CBF in BN may vary in relation to restricting or binge-eating phases ŽHirano et al., 1999.. Regional relative glucose metabolism was found to be lower in the parietal cortex in ill BN compared to controls in one study ŽDelvenne et al., 1997., whereas another group did not find such alterations ŽAndreason et al., 1992.. Glucose metabolism, however, correlates with blood flow in healthy subjects ŽFox et al., 1988.. Thus, such alterations could be associated with alterations in rCBF. The etiology of BN is not known. In addition to pathologic eating behavior, BN is characterized by disturbed emotional states such as increased anxiety and depressive feelings in the ill and recovered states ŽKaye et al., 1998.. Emotional states are thought to be related to brain regions such as the amygdala, orbital frontal and cingulate cortex, and the thalamus ŽDrevets and Raichle, 1992; Charney and Deutch, 1996., and altered mood states might be associated with disturbances of cerebral activity, i.e. blood flow, in these regions ŽReiman, 1997; Krishnan, 1999.. Thus, pathologic behaviors in BN could be reflected by localized alterations of brain cortical activity. However, studies of ill BN women are potentially confounded by the many physiologic disturbances associated with bingeing and purging. A strategy to avoid confounding factors of the ill state is to study women after recovery from BN. If alterations persist after recovery, it is possible that such alterations may be traits that might contribute to the onset of the disorder. Alternatively, persistent alterations could be the consequence of abnormal eating behavior. In this study we investigated rCBF in women in long-term recovery from BN ŽRBN. compared to healthy control women ŽCW., in order to investigate if rCBF alterations persist after recovery. 2. Methods 2.1. Subjects Nine women who had previously met DSM-IIIR criteria for BN were recruited. No subject had a history of anorexia nervosa ŽAN., and they must have maintained a body weight of greater than 85% of average body weight Ž%ABW, Metropolitan Life Insurance Company, 1959. since development of an eating disorder. Subjects were previously treated in the eating disorders treatment program at the Western Psychiatric Institute and Clinic, University of Pittsburgh, PA, USA or were recruited through advertisements. To be considered ‘recovered’, subjects had to ᎏ for at least 1 year before the study ᎏ Ž1. maintain a weight above 90% ABW, Ž2. have regular menstrual cycles, and Ž3. have not binged, purged, or engaged in restrictive eating patterns. Additional exclusion criteria were the use of psychoactive medication such as antidepressants and alcohol or drug abuse or dependence within 3 months of the study. Thirteen healthy CW were recruited through local advertisements. The CW had no history of an eating disorder or any psychiatric, G.K. Frank et al. r Psychiatry Research: Neuroimaging 100 (2000) 31᎐39 major medical, or neurologic illness. They had no first-degree relatives with an eating disorder. They had normal menstrual cycles, and had been within a normal weight range since menarche. All subjects completed a diary in which they listed individual food items consumed for individual meals, portion sizes, and exercise frequency. The Schedule for Affective Disorders and SchizophreniaLifetime Version ŽSADS-L, Endicott and Spitzer, 1978., modified by Merikangas and co-workers, was used to assess subjects for lifetime Axis I DSM-III-R diagnoses. The SADS-L was administered by a trained Master’s or doctoral level clinical interviewer, and reviewed by a psychiatrist Žblind to clinical information., who validated final DSM-III-R Axis I diagnoses. Positron emission tomography ŽPET. imaging was performed during the first 10 days of the follicular phase of the menstrual cycle for all subjects. Subjects were admitted to a research laboratory on the eating disorders unit of the Western Psychiatric Institute and Clinic at 21.00 h of the day prior to the PET study for adaptation to the laboratory and for psychological assessments. The PET study was done the following day. All subjects were served the same standardized diet Žlow in protein breakfast., approximately 4 h prior to PET scanning. All subjects gave written informed consent according to local IRB regulations. 2.2. MR scanning All subjects underwent magnetic resonance ŽMR. imaging prior to the PET scan on a Signa 1.5 Tesla scanner ŽGE Medical Systems, Milwaukee, WI, USA. using a standard head coil. A volumetric spoiled gradient recalled ŽSPGR. sequence ŽTE s 5, TRs 25, flip angle s 40⬚, NEX s 1; field of views 24 cm, image matrix s 256 = 192 pixels. acquired in the coronal plane was used to guide region-of-interest ŽROI. selection. Fast spin echo T2 and proton density weighted images were also routinely acquired to exclude significant neuropathology. Pixels that corresponded to scalp and calvarium were removed from the SPGR MR images ŽSandor and Leahy, 1997. and the MR and PET image data were then co-registered ŽWoods et al., 1993.. 33 2.3. PET imaging w 15 Ox water was used as a radiotracer. Subjects were positioned in a Siemens 951Rr31 PET scanner ŽCTI PET Systems, Knoxville, TN, USA. with the head oriented so that the lowest imaging plane was approximately 1 cm above and parallel to the cantho-meatal line. A softened thermoplastic mold with generous holes for eyes, nose, and ears was fitted closely around the head and attached to the headholder to minimize subject motion. Subjects were advised to keep their eyes closed. The subjects’ ears were unplugged. A 10min transmission scan was obtained and used for attenuation correction. Following bolus intravenous injection of 50 mCi of w 15 Ox water, a 20-frame dynamic emission scan was acquired over 3 min in two-dimensional imaging mode. Arterial blood was sampled at a rate of 6 mlrmin over 3.5 min, using a Siemens liquid activity monitoring system. This device detects radioactivity events with dual BGO scintillation crystals. PET data were corrected for radioactive decay, attenuation and scatter, and reconstructed using a Hanning cut-off at 0.8 of the Nyquist rate. 2.4. Data analyses ROIs were hand drawn on the co-registered MR images and applied to the dynamic PET data to generate time᎐activity curves. The following ROIs were selected: prefrontal cortex wBrodmann area ŽBA. 10x, medial orbital frontal cortex ŽBA 11., lateral orbital frontal cortex ŽBA 47., medial temporal cortex Žamygdalo-hippocampal complex., lateral temporal cortex ŽBA 21., striatum, anterior cingulate ŽBA 32., anterior mesial cingulate ŽBA 24., subgenual cingulate ŽBA 25., sensory motor cortex ŽBA 1,2,3,4., parietal cortex ŽBA 7., occipital cortex ŽBA 17., thalamus and striatum. ROI sampling of the cerebellum ŽCer. was also performed. ROIs were expressed as left and right separately, except for the cerebellum. The w 15 Ox water data were analyzed using a traditional one-tissue compartment model ŽRaichle et al., 1983.. In this model, blood flow was measured as the clearance of w 15 Ox water from blood to brain ŽK 1 , ml miny1 mly1 . while accounting for 34 G.K. Frank et al. r Psychiatry Research: Neuroimaging 100 (2000) 31᎐39 arterial input function timing delays. Cerebral blood flow was assessed on a regional basis ŽrCBF. via regional values of K 1. In addition, we calculated relative rCBF measures similar to previous studies ŽDrevets et al., 1992.. These measures were based on average w 15 Ox water tissue activity images determined over all 20 dynamic frames. Regional measures of relative blood flow were determined as the ratio of the regional average w 15 Ox water tissue uptake to the whole brain w 15 Ox water uptake. radioactivity ratios. Similarly, this method does not show significant group differences among all ROIs sampled. However, for RBN women, there were significant negative relationships between rCBF Ž K 1 . and length of recovery in several ROIs such as the frontal and lateral temporal cortical areas ŽTable 4.. Fig. 1 shows a representative relationship in the left prefrontal cortex. There were no significant relationships between rCBF and the remaining demographic variables shown in Table 1 for either RBN or CW. 2.5. Statistical analyses 4. Discussion The SPSS software package was used for analyses ŽBarcikowski, 1984.. Due to small sample sizes, between-group comparisons were made using the non-parametric Mann᎐Whitney U-test. Correlations were examined with Spearman correlation coefficients. All values are expressed as mean " standard deviation ŽS.D... Statistical significance was defined as P- 0.05. 3. Results CW and RBN women ŽTable 1. were of similar age, and current, as well as, lifetime low ABW. Lifetime high weight was significantly higher in RBN. Absolute rCBF values expressed as K 1 , ŽTable 2. were similar between CW and RBN women for all right and left hemispheric ROI. Cer K 1 values were similar between groups ŽCW: mean 0.65, S.D. 0.09; RBN: mean 0.63, S.D. 0.09; Ps ns.. Table 3 shows the relative rCBF measures that were based on the w 15 Ox water tissue These data suggest that RBN and CW have similar rCBF for the cortical and subcortical regions sampled. However, in the RBN, rCBF was negatively associated with duration of recovery in a large portion of cerebral cortical regions. In the acute phase of the illness, BN women have been found to have increased rCBF in the right inferior frontal cortex, and in the left temporal cortex compared to CW ŽNozoe et al., 1995.. In addition, a recent case report suggested rCBF changes in relation to the state of illness. That is, there was increased rCBF in the right temporal, parietal and occipital cortex during a binge-eatingrpurging phase compared to a phase with food restriction ŽHirano et al., 1999.. The findings in our study support the possibility that altered blood flow previously found during the ill state of BN could be a state-related phenomenon that normalizes with recovery. In addition, the negative relationship with recovery in multiple cortical areas could indicate more of a global than regio- Table 1 Demographic variables a Age Žyears. Current weight Ž% ABW. Lifetime high weight Žin %ABW. Lifetime low weight Žin %ABW. Length of recovery Žmonths. CW Ž n s 13. RBN Ž n s 9. U P 27.1" 6.1 102.4" 5.9 107.7" 6.6 96.0" 5.7 ᎐ 29.9" 4.5 111.0" 14.8 123.9" 9.8 95.0" 12.2 56.8" 45.4 40 37 6 37 ᎐ 0.1 0.2 -0.01 0.4 ᎐ a Notes. Values are expressed as mean " standard deviation; Mann᎐Whitney U statistic, U; percent average body weight, %ABW; control women, CW; recovered bulimic women, RBN. Region Žcorresponding Brodmann area. Prefrontal cortex ŽBA 10. Medial orbital frontal cortex ŽBA 11. Lateral orbital frontal cortex ŽBA 47. Subgenual cingulate ŽBA 25. Anterior mesial cingulate ŽBA 24. Anterior cingulate ŽBA 32. Sensory motor cortex ŽBA 1,2,3,4. Parietal cortex ŽBA 7. Medial temporal cortex Žamygdalohippocampal complex. Lateral temporal cortex ŽBA 21. Occipital cortex ŽBA 17. Thalamus Striatum a Left brain hemispheric rCBF Ž K1 , ml miny1 mly1 . Right brain hemispheric rCBF Ž K1 , ml miny1 mly1 . CW Ž n s 13. RBN Ž n s 9. U P CW Ž n s 13. RBN Ž n s 9. U P 0.61" 0.13 0.59" 0.12 0.64" 0.12 0.71" 0.15 0.62" 0.13 0.68" 0.14 0.59" 0.10 0.58" 0.09 0.56" 0.11 0.55" 0.09 0.53" 0.11 0.62" 0.13 0.64" 0.18 0.61" 0.11 0.64" 0.11 0.56" 0.06 0.58" 0.08 0.48" 0.07 45.0 45.5 53.5 40.0 57.0 52.5 47.0 58.0 29.0 0.4 0.4 0.7 0.2 0.9 0.7 0.5 1.0 0.1 0.59" 0.12 0.63" 0.12 0.62" 0.12 0.64" 0.12 0.66" 0.16 0.60" 0.12 0.58" 0.12 0.57" 0.10 0.53" 0.09 0.54" 0.11 0.54" 0.09 0.60" 0.15 0.60" 0.14 0.57" 0.12 0.58" 0.09 0.56" 0.07 0.57" 0.06 0.48" 0.10 44.5 31.0 46.5 51.0 38.0 54.5 53.0 48.5 35.5 0.3 0.1 0.4 0.7 0.2 0.8 0.7 0.5 0.1 0.53" 0.09 0.75" 0.15 0.76" 0.15 0.66" 0.12 0.51" 0.08 0.77" 0.14 0.68" 0.11 0.61" 0.09 48.5 53.5 42.5 42.0 0.5 0.7 0.3 0.3 0.54" 0.10 0.73" 0.16 0.71" 0.16 0.67" 0.13 0.49" 0.09 0.70" 0.10 0.69" 0.09 0.64" 0.08 40.0 53.0 52.0 51.5 0.2 0.7 0.7 0.7 Notes. Values are expressed as mean " standard deviation; Mann᎐Whitney U statistic, U; Brodmann area, BA; regional cerebral blood flow, rCBF; rCBF expressed as unidirectional clearance of tracer from blood, K 1 ; control women, CW; recovered bulimic women, RBN. G.K. Frank et al. r Psychiatry Research: Neuroimaging 100 (2000) 31᎐39 Table 2 Absolute regional cerebral blood flow ŽrCBF. values a 35 36 Region Žcorresponding Brodmann area. Prefrontal cortex ŽBA 10. Medial orbital frontal cortex ŽBA 11. Lateral orbital frontal cortex ŽBA 47. Subgenual anterior inferior cingulate ŽBA 25. Anterior mesial cingulate ŽBA 24. Anterior cingulate ŽBA 32. Sensor motor cortex ŽBA 1,2,3,4. Parietal cortex ŽBA 7. Medial temporal cortex Žamygdalohippocampal complex. Lateral temporal cortex ŽBA 21. Occipital cortex ŽBA 17. Thalamus Striatum a Left brain w15 Ox water activity relative to whole brain activity Right brain w15 Ox water activity relative to whole brain activity CW Ž n s 13. RBN Ž n s 9. U P CW Ž n s 13. RBN Ž n s 9. U P 1.67" 0.10 1.63" 0.10 1.71" 0.08 1.98" 0.14 1.84" 0.15 1.83" 0.17 1.62" 0.08 1.66" 0.06 1.71" 0.08 1.62" 0.12 1.61" 0.12 1.72" 0.14 1.89" 0.14 1.86" 0.07 1.90" 0.22 1.62" 0.04 1.70" 0.08 1.67" 0.10 44 54 47 33 49 36 52 40 43 0.5 1.0 0.7 0.1 0.8 0.2 0.9 0.3 0.5 1.58" 0.08 1.66" 0.10 1.62" 0.08 1.77" 0.13 1.79" 0.14 1.68" 0.16 1.58" 0.06 1.61" 0.10 1.67" 0.09 1.58" 0.10 1.54" 0.09 1.66" 0.16 1.80" 0.16 1.75" 0.13 1.73" 0.12 1.63" 0.10 1.67" 0.10 1.61" 0.08 49 27 43 49 41 44 41 38 33 0.8 0.1 0.5 0.8 0.4 0.5 0.4 0.3 0.1 1.57" 0.07 1.89" 0.13 1.97" 0.13 1.81" 0.08 1.59" 0.08 2.00" 0.12 1.96" 0.05 1.83" 0.07 43 31 47 43 0.5 0.1 0.7 0.5 1.56" 0.07 1.84" 0.12 1.93" 0.12 1.85" 0.11 1.50" 0.10 1.92" 0.11 1.92" 0.08 1.86 " 0.10 29 33 50 45 0.1 0.1 0.8 0.6 Notes. Values are expressed as mean " standard deviation; Mann᎐Whitney U statistic, U; Brodmann area, BA; regional cerebral blood flow, rCBF; rCBF expressed as the ratio of the regional average w 15 Ox water tissue uptake to the whole brain w 15 Oxwater uptake; control women, CW; recovered bulimic women, RBN. G.K. Frank et al. r Psychiatry Research: Neuroimaging 100 (2000) 31᎐39 Table 3 Regional cerebral w 15 Ox water activity in relation to whole brain w 15 Ox water activity Žrelative rCBF. a G.K. Frank et al. r Psychiatry Research: Neuroimaging 100 (2000) 31᎐39 37 Table 4 Regional cerebral blood flow ŽrCBF. and correlation with length of recovery a RBN Ž n s 9. Region Žcorresponding Brodmann area. Prefrontal cortex ŽBA 10. Medial orbital frontal cortex ŽBA 11. Lateral orbital frontal cortex ŽBA 47. Subgenual anterior inferior cingulate ŽBA 25. Anterior mesial cingulate ŽBA 24. Anterior cingulate ŽBA 32. Sensory motor cortex ŽBA 1,2,3,4. Parietal cortex ŽBA 7. Medial temporal cortex Žamygdalo-hippocampal complex. Lateral temporal cortex ŽBA 21. Occipital cortex ŽBA 17. Thalamus Striatum Correlation of length of recovery with rCBF Left brain hemisphere Right brain hemisphere rho P rho P y0.85 y0.61 y0.61 y0.77 y0.55 0.3 y0.67 y0.66 y0.54 y0.69 y0.67 y0.71 y0.6 0.004 0.084 0.081 0.015 0.128 0.429 0.047 0.051 0.13 0.041 0.047 0.034 0.086 y0.76 y0.82 y0.55 y0.51 y0.54 y0.88 y0.29 y0.53 y0.2 y0.83 y0.43 y0.52 y0.55 0.017 0.006 0.125 0.16 0.13 0.002 0.445 0.139 0.598 0.006 0.252 0.152 0.128 a Notes. Spearman correlation coefficient, rho; Brodmann area, BA; regional cerebral flow, rCBF; recovered bulimic women, RBN. Fig. 1. Scatterplot for length of recovery in relationship to regional cerebral blood flow ŽrCBF. in the recovered bulimic women ŽRBN. group for the left prefrontal cortex; rCBF expressed as unidirectional clearance of tracer from blood, K 1 wml miny1 mly1 x. 38 G.K. Frank et al. r Psychiatry Research: Neuroimaging 100 (2000) 31᎐39 nally localized effect of BN pathophysiology on rCBF. The meaning of changes in cerebral blood flow are conjectural since multiple factors contribute to rCBF regulation, such as neuronal-cellular and microvascular-enzymatic processes ŽReis and Golanov, 1997; Harder et al., 1998; Raichle, 1998.. Alternatively, cerebral blood pressure and thus flow may be influenced by the systemic blood pressure and sympathetic tone. Moreover, the PET measures of rCBF may depend on the functional integrity of the blood-brain barrier, and capillary surface area in the brain. In acutely ill BN women it is possible that sympathetic tone is contributory to increased rCBF since there is an increase in adrenergic tone during bingeing and purging and a reduction of norepinephrine release when abstinent from those behaviors ŽKaye et al., 1990; Pirke, 1996.. The strong inverse relationship of rCBF with length of recovery in the RBN women, however, could also indicate that rCBF reductions occur in this group later in recovery. This has to be investigated in subsequent studies. Previous brain imaging studies have reported that acutely ill BN have structural changes ŽHoffman et al., 1989; Krieg, 1991.. Thus, we cannot rule out that other factors, such as persistent structural alterations in cortical regions due to pathologic eating behavior contributed to this finding. In a preliminary analysis in our lab, we compared whole brain gray ŽGM. and white ŽWM. matter values between the two groups using customized software ŽIDL, Research Systems, Boulder, CO, USA. that separates GM and WM and calculates corresponding volumes. However, no significant differences were found between groups Ždata not shown.. We detected some regional asymmetry in rCBF, such as in the anterior cingulate cortex, between the left and the right side in both groups, but no regional differences were found between groups. We previously showed that after recovery from BN, those women still show increased symptoms of depression or anxiety, and on eating disorders scales ŽKaye et al., 1998.. Despite this, an exploratory analysis of current depression or anxiety symptoms in the RBN group did not show significant correlations with rCBF. A limitation of this study is the relatively small sample size which limits the statistical power of this investigation. Thus, in future studies we will assess rCBF in groups of women currently ill from eating disorders, and increase the sample size of recovered BN women in order to replicate this finding. Our group recently reported other findings in this cohort of subjects. That is, the CW showed a negative relationship between binding of the serotonin 2A receptor Ž5-HT2A. and age in most cortical regions whereas no such relationship was found in the RBN. In addition, the RBN women had reduced 5HT2A binding in the orbital frontal cortex ŽKaye et al., submitted.. Moreover, neither CW nor the RBN women showed a correlation of rCBF with age which is consistent with previous reports of a lack of rCBF alterations with increasing age ŽMeltzer et al., in press.. We found no relationship between 5HT2A binding and blood flow values in either RBN or CW Ždata not shown., indicating that radiotracer delivery was distinguishable from receptor binding. In conclusion, we did not find differences in rCBF in RBN women compared to CW women. However, an inverse relation of rCBF with length of recovery in multiple cortical regions in RBN women was found. Thus, increased blood flow in acutely ill BN that was found in previous studies could be a state-related phenomenon, possibly related to noradrenergic activity, that remits with recovery. However, reduced rCBF in RBN in later stages of recovery cannot be ruled out. Thus this finding has to replicated in a larger sample, and using serial studies during various stages of recovery. References American Psychiatric Association, 1994, Diagnostic and Statistical Manual of Mental Disorders, 4th edition. Andreason, P.J., Altemus, M., Zametkin, A.J., King, A.C., Lucinio, J., Cohen, R.M., 1992. Regional cerebral glucose metabolism in bulimia nervosa wpublished erratum appears in American Journal of Psychiatry 1993 150, 174x. American Journal of Psychiatry 149, 1506᎐1513. Barcikowski, R.S., ŽEd.. 1984. Computer Packages and Research Design, Vol. 3: SPSS and SPSSX. University Press of America, Lanham, MD. G.K. Frank et al. r Psychiatry Research: Neuroimaging 100 (2000) 31᎐39 Charney, D.S., Deutch, A.A., 1996. Functional neuroanatomy of anxiety and fear: implications for the pathophysiology and treatment of anxiety disorders. Critical Reviews in Neurobiology 10, 419᎐446. Delvenne, V., Goldman, S., Simon, Y., De Maertelaer, V., Lotstra, F., 1997. Brain hypometabolism of glucose in bulimia nervosa. International Journal of Eating Disorders 21, 313᎐320. Drevets, W.C., Raichle, M.E., 1992. Neuroanatomical circuits in depression: implications for treatment mechanisms. Psychopharmacology Bulletin 28, 261᎐274. Drevets, W.C., Videen, T.O., Price, J.L., Preskorn, S.H., Carmichael, S.T., Raichle, M.E., 1992. A functional anatomical study of unipolar depression. Journal of Neuroscience 12 Ž9., 3628᎐3641. Endicott, J., Spitzer, R.L., 1978. A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Archives of General Psychiatry 35, 837᎐844. Fox, P.T., Raichle, M.E., Mintun, M.A., Dence, C., 1988. Nonoxidative glucose consumption during focal physiologic neural activity. Science 241, 462᎐464. Harder, D.R., Roman, R.J., Gebremedhin, D., Birks, E.K., Lange, A.R., 1998. A common pathway for regulation of nutritive blood flow to the brain: arterial muscle membrane potential and cytochrome P450 metabolites. Acta Physiologica Scandinavica 164, 527᎐532. Hirano, H., Tomura, N., Okane, K., Watarai, J., Tashiro, T., 1999. Changes in cerebral blood flow in bulimia nervosa. Journal of Computer Assisted Tomography 23, 280᎐282. Hoffman, G.W., Ellinwood E.H. Jr., Rockwell, W.J., Herfkens, R.J., Nishita, J.K., Guthrie, L.F., 1989. Cerebral atrophy in bulimia. Biological Psychiatry 25, 894᎐902. Kaye, W.H., Frank, G.K., Meltzer, C.C., Price, J.C., McConaha, C.W., Crossan, P., Klump, K.L., Devlin, B.J. Altered serotonin 2A receptor activity after recovery from bulimia nervosa. American Journal of Psychiatry, submitted for publication. Kaye, W.H., Greeno, C.G., Moss, H., Fernstrom, J., Fernstrom, M., Lilenfeld, L.R., Weltzin, T.E., Mann, J.J., 1998. Alterations in serotonin activity and psychiatric symptoms after recovery from bulimia nervosa. Archives of General Psychiatry 55, 927᎐935. Kaye, W.H., Gwirtsman, H.E., George, D.T., Jimerson, D.C., Ebert, M.H., Lake, C.R., 1990. Disturbances of noradrenergic systems in normal weight bulimia: relationship to diet and menses. Biological Psychiatry 27, 4᎐21. Kendler, K.S., MacLean, C., Neals, M., Kessler, R., Heath, A., Eaves, L., 1991. The genetic epidemiology of bulimia nervosa. American Journal of Psychiatry 148, 1627᎐1637. Krieg, J.C., 1991. Eating disorders as assessed by cranial computerized tomography ŽCCT, dSPECT, PET.. Advanced Experimental Medical Biology 291, 223᎐229. 39 Krishnan, K.R., 1999. Brain imaging correlates. Journal of Clinical Psychiatry 15, 50᎐54. Lilenfeld, L., Kaye, W.H., 1998. Genetic studies of anorexia and bulimia nervosa. In: Hoek, H.W., Treasure, J.L., Katzman, M.A. ŽEds.., Neurobiology in the Treatment of Eating Disorders. John Wiley & Sons, New York, pp. 169᎐194. Meltzer, C.C., Cantwell, M.N., Greer, P.J. Does cerebral blood flow decline in healthy aging? A PET study with partial volume correction. Journal of Nuclear Medicine Žin press.. Metropolitan Life Insurance Company, 1959. New Weight Standards for Men and Women, 40, Statistics Bulletin of the Metropolitan Insurance Co. Nozoe, S., Naruo, T., Yonekura, R., Nakabeppu, Y., Soejima, Y., Nagai, N., Nakajo, M., Tanaka, H., 1995. Comparison of regional cerebral blood flow in patients with eating disorders. Brain Research Bulletin 36, 251᎐255. Pirke, K.M., 1996. Central and peripheral noradrenalin regulation in eating disorders. Psychiatry Research 62, 43᎐49. Raichle, M.E., Martin, W.R., Herskovitch, P., Mintun, M.A., Markham, J., 1983. Brain blood flow measured with intravenous H 2 15 O. II. Implementation and validation. Journal of Nuclear Medicine 24, 790᎐798. Raichle, M.E., 1998. Behind the scenes of functional brain imaging: a historical and physiological perspective. Proceedings of the National Academy of Sciences USA 95, 765᎐772. Reiman, E.M., 1997. The application of positron emission tomography to the study of normal and pathologic emotions. Journal of Clinical Psychiatry 58, 4᎐12. Reis, D.J., Golanov, E.V., 1997. Autonomic and vasomotor regulation. International Reviews in Neurobiology 41, 121᎐149. Sandor, S., Leahy, R., 1997. Surface based labelling of cortical anatomy using a deformable atlas. IEEE Transactions in Medical Imaging 16, 41᎐54. Smith, K.A., Fairburn, C.G., Cower, P.J., 1999. Symptomatic relapse in bulimia nervosa following acute tryptophan depletion. Archives in General Psychiatry 56, 171᎐176. Stice, E., 1999. Clinical implications of psychosocial research on bulimia nervosa and binge-eating disorder. Journal of Clinical Psychology 55, 675᎐683. Troop, N.A., Treasure, J.L., 1997. Psychosocial factors in the onset of eating disorders: responses to life-events and difficulties. British Journal of Medical Psychology 70, 373᎐385. Weight, D.G., Bigler, E.D., 1998. Neuroimaging in psychiatry. Psychiatric Clinics of North America 21, 725᎐759. Woods, R.P., Mazziotta, J.C., Cherry, S.R., 1993. MRI-PET registration with automated algorithm. Journal of Computer Assisted Tomography 17, 536᎐546.