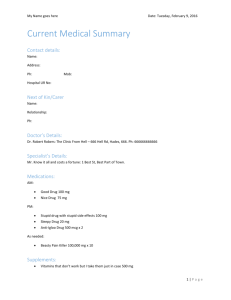
Document 11997986
advertisement

Chronic Fatigue Syndrome How to Make a Disease “Evaporate” 1 “This illness is to fatigue what a nuclear bomb is to a match. It’s an absurd mischaracterization.” Laura Hillenbrand May 2014 Mary Dimmock Matthew Lazell-­‐Fairman This document is a pre-release of a longer work currently under development. Every attempt has been made to accurately and fully document how the case definition of chronic fatigue syndrome evolved over the last thirty years. Significant errors and omissions may be sent to mecfsaction@yahoo.com and will be addressed in the final version. This version of the document is available online at http://bit.ly/1oz1K1d . We ask that you not post this version online elsewhere as this will change. It may be printed for personal use. If it is quoted, please include the author, the title, the version date and this link in the citation (May, 2014). Copyright May 2014. All rights reserved. Table of Contents Preface 3 1. Overview 4 2. The Birth and Evolution of CFS Dismissing Myalgic Encephalomyelitis Chronic Fatigue Syndrome is Born: The Holmes Definition The Growing Focus on Medically Unexplained Chronic Fatigue and Psychological Issues Establishing Oxford and Fukuda Institutionalizing the Psychological and Broadening out the Scope: The Empirical Britain’s NICE criteria Resurrecting ME The Problem with the Name The Classification of CFS in Medical Dictionaries Disease Experts and HHS Face Off HHS’ Current Definition-­‐Related Initiatives 6 8 9 12 15 18 19 21 22 24 25 6 3. Irreconcilable Differences – One Disease or Many HHS’ View: Many Definitions, The Same Disease The View of ME Experts: Many Definitions, Different Diseases The View of ME Patients The View from the Outside 27 27 29 31 32 4. The Impact of Poorly Characterized Definitions 33 5. CFS as a Social and Political Creation 34 7. Appendices and References Table 1: Summary of the primary CFS, ME/CFS and ME definitions Table 2: Changing Prevalence Rates over time Bibliography 37 37 38 40 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 2 Preface In 2010, my son developed myalgic encephalomyelitis (ME), a disease that causes profound neurological, immunological and energy production dysfunction, after contracting Giardia while backpacking in Asia. Since then, I have watched, helpless, as this disease has ripped his life to shreds, turning the promise of a vibrant and spirited future into a soul-crushing existence that has been so unrelentingly harsh and circumscribed, so brutal, so cornered and with so little hope that I have wondered how he has manages to keep going. But worse than the heartbreak, it has been profoundly disturbing and surreal to watch as the world around my son, especially the medical community, not only dismisses his disease but ridicules and even brutalizes him for believing that it is real and serious. When my son first became sick, I struggled to understand what was happening to him physically. Then I struggled to understand why there was such a disparity between what he was experiencing and the response of doctors, the public and especially of the U.S. Health and Human Services, the government agency responsible for our nation’s public health. I naively thought that perhaps patients and advocates just needed to do a better job of helping CDC, NIH and FDA understand the disease. But after four years of talking to ME patients and researchers, reading about ME science, history and politics and trying to engage with Health and Human Services on more occasions than I can count, I am left with the simple fact that Health and Human Services has known about ME for over thirty years – since before my son was even born - and has utterly failed to take ME seriously or provide even a small fraction of the funding needed to address this crisis. HHS has provided erroneous medical education that has trivialized ME, confused doctors on the nature of ME and harmed patients, including my son, with inappropriate treatment recommendations. Worst of all, HHS’ actions have buried ME inside of chronic fatigue syndrome, a man-made waste-bin of medically unexplained fatiguing conditions inextricably linked to psychiatric illness. The impact on ME research, medical care and patient lives has been devastating – and entirely predictable. I spent my career in the pharmaceutical industry and everything I know about science says that the failure to carefully define what you are studying – in this case to correctly and precisely define the disease - is bad science that will drown your work in conflicting, uninterpretable results. Yet for the past thirty years, such bad science has held ME hostage and destroyed the lives of ME patients - one million Americans and 17 million worldwide! The story of this disease is about the ugly side of public health policy in this country – the politics, the personal agendas, the bad science, the neglect and arrogance, the lack of transparency and the utter refusal to listen to ME patients and their doctors. It is the story of how thirty years of failed U.S. public health policy toward ME has sentenced ME patients to an inescapable living hell devoid of hope and support. What has happened to ME patients is morally and scientifically wrong. For this to continue into the future would be outrageous, especially given what is known, what has been known, about the biology of this disease. For the sake of ME patients everywhere, HHS’ public health policy for ME must change. But that will not happen until we find allies in the media, Congress and the public. To do that, we will need to counter the misinformation and misunderstanding that has held ME hostage. My hope is that this paper can help with a small part of that by documenting how ME has been buried inside of the wastebin created by called “chronic fatigue syndrome.” Mary Dimmock May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 3 1. Overview “There has been a creeping movement to include other types of medical conditions under the rubric of CFS…This serves to broaden the scope of the clinical entity to the point at which it is no longer definable.” Dr. H. J. Wedner, 1993 Annual Meeting of the Infectious Diseases Society of America2 Myalgic Encephalomyelitis (ME), also called chronic fatigue syndrome in the United States and in some other countries, is a debilitating disease that causes significant neurological, immunological, autonomic and energy production dysfunction.3,4 The disease is characterized by mandatory, hallmark symptoms like cognitive impairment, unrefreshing sleep and especially post-exertional malaise or PEM, recognized for 40 years or more as the sine qua non of ME. PEM is a distinctive symptom that causes an exacerbation of all symptoms following even trivial mental or physical activity and is associated with a distinctive and measurable impairment in energy metabolism and lowered anaerobic threshold. It is difficult to make definitive statements about the nature of this disease because of the use of the overly broad disease definitions that are the subject of this paper. However, the best available information indicates that ME affects an estimated 1 million Americans of all ages and races, causing significant debility. One clinician has noted that severest patients can be as severely sick as AIDS patients are in the last two months of their lives.5 This degree of functional impairment, quantifiable by a standard exercise test used by a number of medical societies, leaves as many as 87% of patients unable to work;6 those few patients who are able to work spend the rest of their time recovering from the effort. An estimated 25% of patients are bedridden or housebound with up to 60% bedridden on their worst days.7 The sickest patients never leave their beds, living in a dark world where all light and sound are filtered out in a hopeless attempt to avoid exacerbating their symptoms.8 Recovery is rare, typically estimated at 5-10%9 and the limited information available suggests that patents may die up to 25 years prematurely from cancer, cardiovascular disease or suicide.10 The best current estimate of the economic impact of myalgic encephalomyelitis on the U.S economy is $18-24 billion dollars annually.11 ME has occurred in isolated cases and also in outbreaks around the world and throughout the twentieth century. The name “benign myalgic encephalomyelitis” was first used in 1956 following an outbreak in London’s Royal Free Hospital in 1955. Dr. Melvin Ramsay published the first definition of myalgic encephalomyelitis in 1986 that described the essential features of ME, including the distinctive muscle fatigability after trivial activity. Beginning in 1934, there were also a number of outbreaks of ME in the United States. But it was the outbreaks in Incline Village, Nevada and Lyndonville, New York in 1984 that started the transmuting of ME into chronic fatigue syndrome, a nebulous condition of medically unexplained chronic fatigue inextricably linked to psychiatric illness. In 1988, in response to the Incline Village and Lyndonville outbreaks, the United States renamed ME to chronic fatigue syndrome (CFS) and created the Holmes definition. The Holmes definition was the first of a set of fatigue-focused CFS definitions that did not require that patients have hallmark symptoms of ME like post-exertional malaise to be given a diagnosis of CFS. Next came the 1991 Oxford definition, published by a group of British psychiatrists and CDC’s 1994 Fukuda definition, which replaced the Holmes definition. Like the Holmes definition, the Oxford and Fukuda definitions focus on fatigue and do not require hallmark symptoms of ME like PEM. In fact, Oxford requires no symptoms at all except for the single symptom of medically May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 4 unexplained chronic fatigue. Both Oxford and Fukuda allow the inclusion of patients with some primary psychiatric illness, excluding only specific primary psychiatric illness. After Oxford and Fukuda, the next CFS definition to be created was the Empirical definition, published by CDC in 2005. The Empirical definition increased the prevalence of the disease 10-fold over CDC’s earlier prevalence estimate and was shown to encompass more psychiatric illness. The Empirical definition has been largely discredited outside of CDC and as a result, the 1994 Fukuda and 1991 Oxford definitions are still the most commonly used CFS definitions today, twenty years later. These CFS definitions have been associated with a variety of disease theories, including the biopsychosocial theory, most commonly associated with the Oxford definition. This theory holds that CFS is perpetuated by a maladaptive avoidance of activity that has caused deconditioning. According to this theory, cognitive behavioral therapy and exercise are used to reverse “false illness beliefs” and the presumed deconditioning. Others hold that CFS is linked to a personality disorder or is a somatoform illness caused by an excessive focus on bodily symptoms. Others view CFS as a collection of medically unexplained fatiguing illnesses. Still other researchers have used the Fukuda CFS definition to pursue biomedical theories about the neurological, immunological, autonomic and energy production dysfunction. But the key issue here is that regardless of the theory used, all of these CFS definitions are so broad that “CFS” patient cohorts can include patients who do not have ME and who can have psychiatric illness or fatigue due to any number of unexplained causes. For their part, ME experts have published disease-specific definitions that explicitly require the hallmark criteria of ME and exclude primary psychiatric illness - the 2003 Canadian Consensus Criteria, the 2006 Pediatric Criteria and the 2011 ME International Consensus Criteria. These definitions have been shown to be associated with significantly lower rates of primary psychiatric disorder, significantly higher rates of severe functional impairment and a significantly more abnormal immunological profile than the Oxford, Fukuda and Empirical definitions. From a research perspective, there are a number of specific biological findings in ME that distinguish these patients from patients with psychiatric disease and various other fatiguing conditions, particularly the energy production impairment associated with PEM and the neurological and immunological changes. In 2013, fifty internationally recognized ME experts recommended that HHS adopt the Canadian Consensus Criteria for both research and clinical use because it reflects the disease that patients actually have, including hallmark symptoms like post-exertional malaise. HHS refused and instead is creating its own criteria – the fourth to be created by HHS - through a set of initiatives that continue to lump ME into the overly broad and non-specific “CFS” rubric. HHS has maintained that all of these diverse “CFS” definitions represent the same group of patients that can be managed with the same clinical diagnostic and treatment guidelines for all “CFS” patients even though some are harmful or inappropriate for ME patients. CDC has also questioned the nature and importance of PEM as a required hallmark symptom. ME experts have published a number of articles disagreeing with those statements and the use of overly broad definitions. They have also objected to this disease being conceptualized as a psychiatric or behavioral problem,12 a long-standing problem that still exists today in the biopsychosocial and somatoform theories of CFS. But ultimately, the recommendations of these ME experts have had little effect on how the concept of CFS has evolved because these experts lacked the power to counter the influence of HHS or those promoting the biopsychosocial theory of CFS. These controversies even carry over into the medical dictionaries that are used for medical records, insurance billing and mortality and morbidity tracking. This includes the International May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 5 Classification of Diseases (ICD), published by the World Health Organization (WHO). WHO has defined CFS to be a neurological disease but the U.S. has reclassified CFS to be just a symptom, a subcategory of the symptom of “Malaise and Fatigue”. The second of these dictionaries is the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association in 2013. While DSM-5 does not specifically list ME or CFS, there are a number of researchers who believe that CFS is a prime example of “somatic symptom disorder”, a new and controversial disorder in the DSM-5, diagnosed in patients when the medical provider has decided that they have an excessive focus on their health. Today, the collective concept of “CFS” comprises a medical rashomon effect as a result of the disparate definitions, unrelated patient cohorts and ultimately irreconcilable views on the true nature of this disease. This concept of “CFS” is not based on the biological pathologies of ME. It is a political and social creation, borne of political agendas, cognitive biases that view this disease as a psychological problem, a remarkable level of scientific sloppiness and a stubborn refusal to acknowledge the biological reality of ME. Because of this confusion, the term ME is used in this paper when referring to the disease first described by Dr. Ramsay. The impact of this definitional confusion has been profound and devastating. More than any other single factor, this definitional confusion is at the heart of our country’s failure to address the ME crisis for the last thirty years. It has confounded ME research, thwarted ME drug development, resulted in harmful medical education, driven researchers from the field and led doctors to not believe that their ME patients are really sick. Worst of all, it has obliterated ME patients’ lives for 10, 20, 30 years. There are numerous problems with HHS’ public health policy toward ME – lack of commitment, woefully inadequate research funding, outdated and downright harmful medical education, and HHS’ refusal to transparently engage this community, just to name a few. All must be addressed. But as long as this definitional chaos continues, ME will remain forever medically unexplained, held hostage by the bad science and politics of “CFS”. 2. The Birth and Evolution of CFS Dismissing Myalgic Encephalomyelitis Myalgic encephalomyelitis is not a new disease. Throughout the twentieth century, a number of documented outbreaks and sporadic cases of ME occurred across the globe, including outbreaks in Los Angeles in 1934, Iceland in 1946, Florida, Maryland, Alaska and London, England in the 1950s and Texas, Scotland, Switzerland and England in the 1960s and 1970s.13 The outbreak in London was at the Royal Free Hospital in 1955 and forced the closure of the hospital for over two months. Almost 300 members of the staff fell victim, 149 of them were nurses and over two hundred had to be hospitalized, 40 percent for more than one month.14 Following the Royal Free Hospital outbreak, the name benign myalgic encephalomyelitis first appeared in a Lancet editorial in 1956.15 Reports and reviews of outbreaks and episodic cases of ME surfaced in the literature that described the key features of the disease.16 In 1959, Dr. Donald Henderson of CDC and Dr. Alexis Shelokov of NIH published a report that summarized 23 outbreaks of the disease from around the world.17 The World Health Organization officially recognized ME as a neurological disease in the International Classification of Diseases (ICD) in 1969.18 In 1977, British physician Dr. Melvin Ramsay, consultant physician in infectious diseases at Royal Free Hospital, noted that a “unique fatigue pattern might be associated with May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 6 mitochondrial damage.”19 In 1978, the Royal Society of Medicine held a symposium on ME to discuss the disease and plan research where it was reiterated that ME is a distinct nosological entity that is organic, not psychological in nature.20 In 1986, Dr. Melvin Ramsay established the first case definition to describe the essential features of myalgic encephalomyelitis.21 This description included what he described as a distinctive form of muscle fatigability that occurred after even trivial effort and from which patients exhibited a delayed recovery. In 1984, reflecting Ramsay’s description of muscle fatigability and foreshadowing the research being done today on the effects of exercise by ME experts like Dr. Chris Snell and Dr. Julia Newton, Dr. DL. Arnold reported that patients had abnormal muscle acidosis upon exercise, which could represent excessive lactic acid formation indicative of a disorder of metabolic regulation.22 But starting in 1984, the same year as Arnold’s study was published, there were two outbreaks of ME in Incline Village, Nevada and Lyndonville, New York that began the transmuting of myalgic encephalomyelitis into a vaguely defined syndrome of medically unexplained chronic fatigue inextricably associated with psychiatric illness. As documented in various sources23 including Osler’s Web,24 published by Hilary Johnson in 1996, a 1990 Newsweek article25 and a 1996 Primetime Live Investigation,26 Dr. Paul Cheney and Dr. Daniel Petersen of Incline Village, Nevada began seeing patients with a severe flu-like illness, dramatic cognitive issues and crippling exhaustion in the fall of 1984. According to these sources, as more and more people were affected from Incline Village and surrounding townships and they started showing up in clusters - teachers, a group of casino workers, the local girl’s basketball team – Drs. Cheney and Petersen repeatedly begged CDC to investigate.27 One year later, CDC finally sent two epidemiologists, Dr. Jon Kaplan and Dr. Gary Holmes, to Incline Village. According to PrimeTime Live,28 the two investigators “looked at charts and test results, took some blood samples and headed back to the CDC without a word.“ Hilary Johnson, author of Osler’s Web, who reported extensively on the outbreaks and the U.S. government’s handling of CFS over the years, told PrimeTime Live that the attitudes behind the scenes at CDC reflected Dr. Kaplan’s attitude – “complete and utter ridicule” of the disease.29 About the same time, Dr. David Bell of Lyndonville, New York was also dealing with an outbreak of ME. Like Drs. Cheney and Petersen, he also called CDC. According to PrimeTime Live, not only did CDC not respond, it didn’t even tell Dr. Bell that a similar outbreak was happening in Nevada.30 Lacking support from CDC, Drs. Petersen and Cheney tried to do what they could for their patients. According to PrimeTime Live, this included ordering MRI scans, which they paid for out of their own pockets. Cheney and Petersen were told by a neuroradiologist that the scans looked like those of AIDS patients,31 which led them to question whether the illness involved immunodeficiency or general immune dysfunction. But in May of 1986, CDC issued a report on the Incline Village outbreak,32 which it characterized as “chronic fatigue”. According to PrimeTime Live, Dr. Cheney’s reaction to the report was that “the overall message, the tone of the paper was that this [disease] did not appear to be anything - at all.”33 Some researchers, including Dr. Stephen Straus of the National Institute of Allergy and Infectious Diseases (NIAID) at NIH, did investigate a possible connection between CFS and Epstein Barr Virus and whether CFS could be due to a reactivation of the virus. Based on that theory, Dr. Straus conducted a clinical trial assessing the effectiveness of Acyclovir but the study failed to show a difference in efficacy between placebo and treated patients. In the study publication, Dr. Straus stated that observed clinical improvement seen was due to “either spontaneous remission of the syndrome or a placebo effect and further stated that “subjective May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 7 improvement correlated with various measures of mood”34 – in other words, the patients were not sick but rather just moody. According to Dr. Judith Richman of the University of Illinois, the failure of the Acyclovir study to demonstrate a link to a viral etiology coincided with a substantial shift that emphasized a psychological conceptualization of the disease.35 Certainly, Dr. Straus helped spark this shift in his own expression of bias. In a 1987 Nightline interview, Dr. Straus stated, “From my own research, I know that this disorder is so subjective that patients will commonly feel better no matter what you give them.”36 In a 1988 New York Times article, he stated that these patients were “psychologically different long before they developed the syndrome”, anxious, depressed and neurotic on the one hand or driven and under undue stress from busy lives on the other.37 According to MECFS Forums, a patient forum, in a 1988 publication, Dr. Straus stated, “A less casual appraisal, however, often uncovers histories of unachievable ambition, poor coping skills, and somatic complaints.”38 It should be noted that Dr. Straus’ “appraisal”, in its “casual” deviation from objective science, quickly put patients between a rock and a hard place: having to prove they did not have “unachievable ambition” but also didn’t suffer from neuroticism or from a “fear of movement” that a group of British psychologists were beginning to promote at about this time. Chronic Fatigue Syndrome is Born: The Holmes Definition In 1988, dismissing the objective physical and laboratory abnormalities that Drs. Petersen and Cheney had seen, and apparently intent on discouraging “unproven assumptions about viral origins” according to Dr. Vincent Racaniello,39 CDC published the Holmes definition40 and established the trivializing name “chronic fatigue syndrome.” The Holmes definition was the first of what was to become a set of CFS definitions focused on medically unexplained chronic fatigue as the primary symptom. Minor symptoms included any eight choices out of a list of non-specific symptoms like weakness, malaise, subjective fever, decreased memory, confusion and sleep disturbance. Holmes was intended to be a restrictive case definition to make it easier for research to identify associations and as such, provided a long list of exclusionary diagnoses that included either a history of or a new onset of psychiatric disease. Because of the restricted criteria but also because of methodological issues with how the studies were conducted, the earliest prevalence studies estimated a prevalence of 0.0073%, a rate equal to 23,000 patients if applied to the total 2012 U.S. census of 314 million (Table 2). This prevalence rate was exceedingly low compared to later estimates.41 Inexplicably, given their knowledge of the disease and their role in bringing it to the attention of CDC, Dr. Cheney, Dr. Petersen and Dr. Bell were not listed as authors on the Holmes definition. Dr. Alexis Shelokov of NIH and Dr. J. Gordon Parish from England, two individuals with extensive experience with ME, were on the panel that discussed the definition42 but according to a 2001 article co-authored by Professor Emeritus Malcolm Hooper, Margaret Williams and E.P. Marshall, Dr. Shelokov and Dr. Parish “refused to sign the final document and withdrew from the panel because the proposed definition and new name were too different from the ME with which they were so familiar.”43 Of the sixteen final authors, it is unclear if the others had any experience treating patients with ME with the notable exception of Dr. Anthony Komaroff, a Boston researcher and clinician who had been involved in studies on Incline Village patients and who had also studied and treated ME patients in the Boston area. In fact, Dr. Komaroff had conducted a SPECT scan study on those patients that showed that patients had neurological changes similar to the AIDS dementia complex patients and dissimilar to patients with depression.44 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 8 In practice, over the coming years as researchers used the Holmes definition, they soon determined that patients who met the Holmes CFS criteria were indistinguishable from patients with non-specific chronic fatigue and that the use of eight or more minor and non-specific symptoms increased the likelihood that individuals with psychiatric problems would be misdiagnosed with CFS.45 The Growing Focus on Medically Unexplained Chronic Fatigue and Psychological Issues At least by the late 1980’s and early 1990’s, the published literature showed that scientists were acutely aware of the range of specific multi-system pathologies involved in ME and were in fact reporting on a variety of immune abnormalities, neurological issues and findings that indicated viral disease.46 For instance, according to a 2011 article by journalist David Tuller, a Harvard-led research team reported in the 1992 Annals of Internal Medicine that the Incline Village patients had “abnormal MRI brain scans, significant alterations in white blood cell counts and functioning, and signs of active infection with a recently discovered pathogen, HHV-6.” In the study report, Debra Buchwald, lead author, stated, “Neurologic symptoms, MRI findings, and lymphocyte phenotyping studies suggest that the patients may have been experiencing a chronic, immunologically mediated inflammatory process of the central nervous system.”47 It’s worth noting that in this same timeframe, HIV/AIDS researchers were investigating the possibility that HHV-6 was a potential co-factor involved in the pathogenesis of HIV/AIDS.48 But as pointed out by David Tuller, Dr. Reeves of CDC, in a letter to the Annals, rejected the findings of the Buchwald study, concluding, “The disease that Buchwald and co-workers described is not the chronic fatigue syndrome or any other clinical entity.”49 In fact, according to the PrimeTime Live report on the Incline Village outbreak, Dr. William Reeves, head of CDC’s CFS program from 1989 to 2010, stated, “One, there is no viral cause for this problem. Two, there are no immune system abnormalities in patients with chronic fatigue and three, there are no clusters.” When the interviewer then asked him what had happened in Incline Village, he replied, “That was hysteria.”50 That response speaks volumes about the gulf in understanding at that time between CDC on the one hand and the clinicians and researchers studying and treating ME patients on the other. And while CDC no longer states that what happened in Incline Village was hysteria, CDC has maintained, as recently as 2012, that it has not been able to confirm the occurrence of outbreaks, when specifically asked by CFSAC to allocate funds to study patients from past cluster outbreaks.51 CDC was not alone in recasting this disease as a psychological problem. As early as 1970, Dr. A.W. Beard and Dr. Colin McEvedy of the Department of Psychological Medicine at Middlesex Hospital in London had set that tone when they reanalyzed case notes from the Royal Free Hospital outbreak and decided, reportedly without seeing any patients according to Dr. Byron Hyde,52 that the outbreak was “epidemic hysteria.”53 This reinterpretation was rejected by the physicians who had actually treated those patients.54 In 1991, Dr. Susan Abbey of Toronto Hospital in Canada and Dr. Paul E. Garfinkel, psychiatrist at the University of Toronto, stated a similar position to that of Beard and McEvedy when they argued that “chronic fatigue syndrome will meet the same fate as neurasthenia - a decline in social value as it is demonstrated that the majority of its sufferers are experiencing primary psychiatric disorders or psychophysiological reactions.”55 But the individuals who pushed this psychological conceptualization the hardest were a group of British psychiatrists who viewed CFS as a psychological and behavioral problem.56 In 1989, Professor Simon Wessely, currently at Kings College in London and one of the key authors of May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 9 the 1991 Oxford definition, stated that the symptoms of the disease are “perpetuated by a cycle of inactivity and deterioration in exercise tolerance… and is compounded by the depressive illness that is often part of the syndrome”57 He further stated “Cognitive behavioural therapy (CBT)… helps the patient understand how genuine symptoms arise from the frequent combination of physical inactivity and depression.” In a highly cited 1989 article, Professor Wessely stated that CFS patients more closely resembled patients with psychiatric disorders than patients with neuromuscular disorders associated with peripheral fatigue.58 In 1990, Professor Wessely compared the current outbreaks of ME to the nineteenth century concept of neurasthenia, originally described as an organic disease but that Professor Wessely viewed as a “culturally sanctioned expression of distress.”59 Also in 1990, Professor Wessely went on to explain that patients developed “chronic activity avoidance” as a maladaptive response to an acute illness and it was this activity avoidance behavior that resulted in fatigue, deconditioning and the other symptoms of “CFS”.60 Again, one has to question how patients with so-called “unachievable ambition” might also suffer from the unquenchable desire to avoid activity. These allegations squarely placed patients in a conundrum of having to prove they were seeking a perfect “Goldilocks zone” of not being pathologically ambitious, yet never being slothful. This theory, called the biopsychosocial approach61 to CFS, is still in active use today,62 even though, to my knowledge, no scientific proof has been offered and even though the theory fails to account for existing research demonstrating the biological pathology of ME.63 Proponents have stated that this approach is essential to overcome the mind-body dualism, a goal that might have been desirable to many both inside of and outside of HHS, given the importance of treating the whole patient. But there is a vast difference between a humane understanding that heart disease might be aggravated by stress or lead to secondary depression and the idea that a contrived behavioral trait is the sole determinant that is keeping a patient sick. Therefore, this concern with the mind-body dualism must be viewed with skepticism since, as applied to CFS, the approach is almost entirely devoid of the disease’s biological pathology beyond acknowledging that an infection might have initially triggered the disease.64 As a result, the studies that have pursued the biopsychosocial approach, including the well-funded but highly disputed Oxford CFS PACE trial conducted in Britain,65 have focused almost solely on psychological and behavioral disease theories and treatments; CBT to change the patient’s “false illness beliefs” and graded exercise treatment (GET) to address the presumed deconditioning.66 As discussed further below, a closely related psychological theory holds that CFS is a somatic (somatoform) disorder in which a patient has an excessive focus on his bodily symptoms and excessive concern over his health.67 But regardless of the specifics of the disease theory, when CFS is seen through this psychological lens, it becomes a disease of faulty behavior, not faulty biology.68 The question of whether there is any scientific proof for these psychological theories is a critical one. In a paper exploring the concept of somatic disorder, Dr. Per Dalen, Swedish professor of psychiatry, stated, “the boundaries of the somatization syndrome [somatoform disorder] largely coincide with the current limits of received medical knowledge.”69 In other words, somatoform disorder becomes the default explanation when medical science has no organic explanation. As an example of this effect, Dr. Dalen cited the disturbances in sensitivity and blood circulation first seen when chain saws were introduced into forest work. Lacking a medical explanation, these reports by patients were initially interpreted as psychosomatic illness until vibration related illnesses became an accepted medical concept. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 10 In the case of ME, the tremendous reach of these psychological theories even today cannot be overstated. Just one example is a 2012 article on CFS in the Academy of American Family Physicians stated: “Patients with poor social adjustment, a strong belief in an organic cause for fatigue, or some sort of sickness benefit (i.e., financial incentive) tend to have worse responses to [cognitive behavioral] therapy.”70 Such a singular, slanted focus on psychological and social problems as the explanation for continued ill health would never be tolerated for other organic diseases such as cancer, multiple sclerosis, heart disease or AIDS. Doing so in ME has been both a significant impediment to progress and a source of great stigma for ME patients. In March 1991, NIAID and the National Institute of Mental Health sponsored a conference,71,72,73 whose purpose was to review the use of the Holmes criteria, make recommendations for its modification and discuss approaches to assessing disease severity. While Dr. Cheney was listed as a contributor, so were a number of individuals who viewed CFS as a psychological disease, including Dr. Stephen Straus, Dr. Susan Abbey, Professor Simon Wessely and Dr. Peter Manu, a University of Connecticut researcher.74 The final report acknowledged the concern that patients with psychiatric illness and other chronic diseases were being misdiagnosed with “CFS” by the broader medical community and that even the experts were applying the case criteria inconsistently. But, remarkably, the report then went on to recommend that the definition be modified, not to make the criteria more restrictive but rather to exclude fewer patients because of psychiatric illnesses. Further, the report advocated for “an integrative approach that gives consideration to issues relating to comorbidity and possible common pathogenic pathways in patients with CFS and psychic stress.” The net effect of these recommendations was to create a catchall that was destined to include psychiatric illness and that completely failed to parse out ME patients into a better-defined research group. Given the concern that patients with psychiatric illness were incorrectly being given a diagnosis of CFS, it might seem inexplicable that the report would then go on to recommend excluding fewer patients with psychiatric illness. But given the contemporaneous statements of conference attendees and others about the connection between this disease and psychiatric disorder, it is not surprising that the conference report took the position that this increased psychiatric focus in the definition would “lead to a better understanding of factors underlying CFS.” Far from bridging the mind-body dualism as many might have understood the intent, the approach allowed the attendees to effectively shape-shift the concept of the disease to fit their beliefs that the disease was psychogenic. It’s instructive to compare the focus of the 1991 NIH conference against the proceedings of the first international symposium of ME experts, spearheaded by Dr. John Richardson and held in Cambridge, England in 1990. Judged by the proceedings of the Cambridge symposium,75 the discussion focused on the range of biological dysfunction that ME experts are investigating today – neurological, immunological, cognitive, muscle and exercise, cardiac, neuropsychiatric and the role of infection. The diagnostic importance of recognizing post-exertional malaise was highlighted. The proceedings also noted that the disease was being conflated with psychiatric illness and raised the concern that such a psychological focus could cause important disease factors to be overlooked or could in fact even obscure the existence of the disease itself. The difference in perspective on the nature of this disease between the 1990 Cambridge symposium proceedings and the report of the 1991 NIH conference is dramatic. Unfortunately, the Cambridge conference does not seem to have influenced the NIH conference, held the following year. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 11 In the same year as the NIH conference (1991), the U.S. government also made the decision to categorize CFS as a subtype of “Malaise and Fatigue” in the Signs And Symptoms chapter of the ICD-9-CM, the U.S. version of the International Classification of Diseases (ICD).76 Its inclusion in the Symptoms chapter of ICD-9-CM further distanced CFS from WHO’s decision to categorize ME as a neurological illness and further reinforced the U.S. government’s emerging view of CFS as a non-specific symptom that did not deserve consideration as a real disease. In sharp contrast, in 1992, when the World Health Organization added CFS to ICD-10, it decided to categorize CFS as a neurological disease and assign it the same code as used for ME.77 The issues with how the definition of CFS was evolving were obvious to researchers even at this early point in the history of CFS. In 1993, Dr. Stephen Straus mediated a discussion at the annual meeting of the Infectious Disease Society of America. One of the speakers, Dr. H. James Wedner, Professor of Immunology and Allergy at Washington University and a clinician who had treated CFS patients, pointedly stated that the continued broadening of the scope of CFS was making it indefinable.78 “…There has been a creeping movement to include other types of medical conditions under the rubric of CFS. For example, various forms of post-infectious fatigue, fibromyalgia, and non-psychiatric and depressive disorders were permitted by consensus of a National Institutes of Health (NIH) workshop [the 1991 NIH workshop referenced above]. Somatoform disorders and panic disorder became part of what could be encompassed within the CFS case definition. This serves to broaden the scope of the clinical entity to the point at which it is no longer definable.” This was a strong indictment of how those responsible for CFS within Health and Human Services were consciously expanding and reshaping the definition of CFS. Yet, Dr. Wedner’s concerns did nothing to reign in the “creeping movement” being promoted by key individuals both inside of and outside of HHS. Establishing Oxford and Fukuda In the early and mid 1990’s, there were a number of new definitions created for CFS, including the 1990 Australian definition (which was not extensively used),79 the 1991 Oxford definition80 and the 1994 Fukuda definition,81 which replaced the Holmes definition. The Oxford and Fukuda definitions, still the two most commonly used today, were ostensibly created in part to address the problems in consistency and cross-study comparability seen in the Holmes definition. But given the backdrop of the 1991 NIH conference and the reconceptualization of CFS as a psychological disease,82 it is not surprising that, because of their vagueness, both the Oxford and Fukuda definitions further broadened the diagnostic criteria, allowed the inclusion of primary psychiatric illness and became increasingly focused on the broad umbrella of medically unexplained chronic fatigue. The 1991 Oxford definition was developed under the primary influence of the group of British psychiatrists who promoted the biopsychosocial approach to CFS; these included Professor Wessely, Professor Michael Sharpe, Professor of Psychiatry, University of Oxford and Professor Peter White, Department of Psychological Medicine, St Barts Hospital, London. The Oxford definition does not require any of ME’s hallmark symptoms like post-exertional malaise for a diagnosis. In fact, Oxford has a stunning absence of any criteria at all - except for 6 months of debilitating, medically unexplained fatigue, which can be either mental or physical in nature and which must be subjective, not physiological. Further, primary psychiatric illness is allowed while all “medical conditions known to produce fatigue” are excluded, whether seen at the initial visit or subsequently. Oxford does nothing more than describe the relatively non-specific and illMay 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 12 defined symptom of chronic fatigue, a symptom that is associated with many diseases including heart disease, multiple sclerosis and cancer. But by excluding all known causes and focusing on medically unexplained fatigue, Oxford virtually guarantees that “CFS” will be interpreted as psychological. Reflecting the report from the 1991 NIH conference discussed above, the 1994 Fukuda definition, developed by CDC with input from Professor Michael Sharpe and Professor Simon Wessely,83 also adopted an overly broad approach that does not require that patients have hallmark criteria of ME for a diagnosis of “CFS”. Fukuda, designed for research, only requires 6 months of medically unexplained chronic fatigue and then specifies that patients have any four of eight other symptoms. Like Oxford, Fukuda excludes patients with any medical condition that could cause fatigue and has dropped all physical signs. Fukuda excludes some forms of primary psychiatric illness84 but does not list anxiety disorders, somatoform disorders or all forms of depression as exclusionary.85 In fact, as Dr. Leonard Jason of DePaul University and an authority on the definitional issues has noted, patients with depression can easily qualify for a diagnosis of CFS because they have fatigue plus four of the Fukuda symptoms, exclusive of PEM.86 This is problematic for research and the development of treatments because patients with ME have different underlying pathologies from depressed patients, a fact that has been well demonstrated by exercise testing and neurological studies.87 The Fukuda definition states that the rationale for inclusion of psychiatric illness is that “such psychiatric conditions are highly prevalent in persons with chronic fatigue and the chronic fatigue syndrome, and the exclusion of persons with these conditions would substantially hinder efforts to clarify the role that psychiatric disorders have in fatiguing illnesses.” Not only does this statement betray a predominate focus on psychological problems but when combined with other statements in the definition it demonstrate that the Fukuda definition was designed to provide a conceptual framework for the study of CFS and other medically unexplained fatiguing illnesses88 in one lumped-together category. This is significant because, like the Oxford definition, the Fukuda definition was never intended to provide a clear and distinct definition for ME patients but rather mixes ME patients with disparate groups who have a variety of other illnesses, including psychiatric illness. The Fukuda definition acknowledges the importance of stratifying patients by factors like coexisting psychiatric illness but in practice, few studies appear to have done that.89 As a result of the broadening of the criteria, compounded by various methodological issues with how CFS patients were identified, both Oxford and Fukuda resulted in significantly higher prevalence estimates of CFS than the prevalence of around 23,000 estimated with the Holmes definition. In 1997, Professor Wessely estimated Oxford prevalence at 2.2% and Fukuda prevalence at 2.6%,90 rates equal to 6.9 million and 8.2 million people respectively in the U.S. if applied to the total 2012 U.S. census of 314 million people (Table 2). These rates fell to 0.7% for Oxford and 0.5% for Fukuda when psychiatric illness was excluded, demonstrating clearly that those with psychiatric illnesses were disproportionately included in these definitions. Over time, studies of prevalence that have used the Fukuda definition have ranged from the high of 2.6% reported above down to a low of 0.07% with the most frequently accepted prevalence rate being the 0.42% rate reported in a study by Dr. Leonard Jason (Table 2). Obviously, as discussed below, such a wide variance in prevalence is a reflection of the use of overly broad, non-specific definitions, the methodological issues with how those criteria were used to identify CFS patients and even the researcher’s conceptualization of the disease. In addition to establishing the diagnostic criteria, Fukuda also recommended a minimal set of diagnostic tests, following recommendations made at the 1991 NIH conference. The tests May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 13 recommended by Fukuda (e.g. complete blood count, a liver function test, urinalysis) are almost invariably normal in ME patients and are intended to be done solely to exclude other diseases. While the Oxford definition itself does not provide recommendations for testing, some who use the Oxford definition have also promoted a similar reductive testing approach.91 For reasons that are outside the scope of this paper, no diagnostic tests have been approved for this disease but its clear that this minimalist approach, combined with an overly broad definition, has had the impact of ensuring that the disease would not be taken seriously while guaranteeing that it would remain medically unexplained. The Oxford definition appears to have been used most often by researchers who have adopted the biopsychosocial theory of CFS and who believe that “CFS” is a result of or perpetuated by behavioral or psychiatric problems.92 The Fukuda definition has been used by researchers who are investigating the various biomedical pathologies like immunological, autonomic and neurological dysfunction associated with ME but is also used by researchers who view CFS as a non-specific umbrella of fatigue related conditions in which symptoms like PEM are not required. Fukuda also appears to be used by those who have adopted a biopsychosocial model. Regardless of the disease theories held by researchers, both the Fukuda criteria and the Oxford criteria encompass patient cohorts with significantly different conditions93because hallmark criteria are optional, because primary psychiatric illness is allowed and because of choices made in how cases of the disease are assessed. The obvious question is why CFS was defined so broadly that it failed to specifically describe ME patients and included such diverse patient cohorts. In a letter apparently sent about the time of the 1994 publication of Fukuda and obtained by advocate Craig Maupin through a FOIA,94 NIH’s Dr. Straus congratulated CDC’s Dr. Keiji Fukuda on “his efforts to forge an international consensus that has scientific merit and is politically acceptable.” Betraying the unspoken intent behind the Fukuda definition, Dr. Straus made the following points: “My own sense is that a few years of use [with the Fukuda definition] in the field will once again verify that there is no demonstrable or reproducible differences between individuals who meet the full CFS criteria and those who can be said to suffer Idiopathic Chronic Fatigue. This would beg the question of whether additional revisions to the definition are warranted, or its entire abandonment.” “I predict that fatigue itself will remain the subject of considerable interest but the notion of a discrete form of fatiguing illness will evaporate. We would, then, be left with Chronic Fatigue that can be distinguished as Idiopathic or Secondary to an identifiable medical or psychiatric disorder. I consider this a desirable outcome.” “What I would most like to see is that fatigue is not abandoned as a subject for careful consideration because of further failures of CFS case definitions or frustrations arising out of shrill pressures to justify an entity of dubious validity such as CFIDS [CFIDS is Chronic Fatigue and Immune System Dysfunction, an alternative name for CFS].” “The notion of a discrete form of fatiguing illness will evaporate.” Indeed. But my son didn’t evaporate. ME patients didn’t evaporate. They just became invisible, disbelieved and ignored. Especially when put into the context of Dr. Straus’ other statements, can there be any more damning evidence that some within HHS, whether through scientific misunderstanding or conscious intent, had rejected ME as a real disease and were morphing it into a vague condition of medically unexplained chronic fatigue associated with psychological problems? May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 14 Institutionalizing the Psychological and Broadening out the Scope: The Empirical In 1996, the recasting of ME as a psychological condition was given further institutional support through a report of the Joint Working Group of the Royal Colleges of Physicians, Psychiatrists and General Practitioners on Chronic Fatigue Syndrome.95 This report discouraged the use of the term ME, reported a prevalence of 1-2% (significantly more than Dr. Jason’s generally accepted prevalence estimates of 0.42%), found that 75% of the patients had psychiatric disorders and recommended cognitive behavioral therapy and graded exercise as treatments. A Lancet editorial was very critical of this report, stating “We believe that the report was haphazardly set-up, biased, and inconclusive, and is of little help to patients or their physicians.”96 Unfortunately, and demonstrating his own biases, Dr. Straus of NIH gave a ringing endorsement of the report’s recommendation, stating, “The report constitutes, arguably, the finest contemporary position statement in the field, and physicians and patients are well advised to read it.” He further endorsed the biopsychosocial approach to CFS and how that approach “stresses the complex interplay of social, behavioural and emotional factors in the presentation and perpetuation of [CFS] symptoms.”97 It’s worth noting that in his statement, Dr. Straus didn’t even mention the biological factors involved in the “presentation and perpetuation” of this disease. In 1998, in his acceptance speech for the Rudy Perpich Award presented at the conference of the American Association for Chronic Fatigue Syndrome,98 Dr. Phillip Lee, U.S. Assistant Secretary of Health, voiced his concern that the biopsychosocial school had gone too far in its excessive emphasis on the social, behavioral and emotional factors in CFS as evidenced by the Royal Colleges Report and the handling of CFS in the U.S. ICD-9-CM where CFS had been classified as just a symptom. He reminded the audience of what Dr. Wedner had said; that “Chronic Fatigue Syndrome is neither a disease nor a syndrome. It is a committee definition.” He strongly disagreed with Dr. Straus’ endorsement of the Royal Colleges report and the biopsychosocial approach. But again, in spite of his clarity on the issues and his level in the organization, it doesn’t appear that Dr. Phillip Lee and any others who might have felt similarly were able to influence the policies and actions being taken on this disease by HHS. In February 2000, NIH held the “Chronic Fatigue Syndrome State-of-the-Science Consultation”99 which provided further evidence of NIH’s psychological conceptualization of the disease. As originally planned, the conference, which was being held to shape NIH’s CFS research priorities and recommend optimal approaches to CFS research, included only four attendees, Dr. Stephen Straus, Professor Simon Wessely, Professor Michael Sharpe (at the time at the Departments of Psychiatry and Clinical Neurosciences of the University of Edinburgh) and Dr. Mark Demitrack, a psychiatrist from Eli Lily. Dr. Straus, Professor Wessely and Professor Sharpe all promoted the biopyschosocial view of the disease. Because of vocal patient opposition, three ME clinicians were invited at short notice; Dr. Nancy Klimas or Miami, Dr. Peter Rowe of Baltimore and Dr. Tony Komaroff, although Dr. Komaroff could not attend. Predictably, the resultant report downplayed the importance of biological pathologies, focused on psychological issues, stated that the majority of CFS patients had psychiatric illness, stated that “beliefs about illness” should be investigated and discussed the use of CBT as a treatment. The February 2000 conference had reportedly been originally recommended by the CFS Coordinating Committee (CFSCC), the group that provided advice to HHS at the time. As a result of the controversy surrounding the February 2000 conference, the CFSCC organized a second conference in October 2000,100 a conference that included a number of well known ME expert clinicians and researchers. Unlike the February conference, this conference focused on issues like neuroendocrinology, cognition, chronic pain, sleep, immunology, orthostatic intolerance, fatigue, functional status, and disability. It focused on dysregulation of biological May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 15 systems, not the dysregulation of thoughts and beliefs. Further, unlike the February 2000 report, which had stated that the case definition was “unrepresentative of the true spectrum of illness,”101 the October 2000 report stated that there was a need to “constrain the diagnostic criteria.” In other words, like Dr. Wedner in 1993, the researchers at the October 2000 conference were highlighting the problems that were occurring as a result of the broadening of the CFS case definition. But as before, their concerns appeared to have little influence on the evolution of the CFS case definition, as it would later play out in development of the Empirical case definition described below. In 2000, the U.S. General Accounting Office (GAO) released a report102 critical of HHS’ handling of CFS, especially for lack of coordination between NIH and CDC, lack of communication on CDC research and CDC’s misuse of $12.9M in funds earmarked for CFS research. During this timeframe, the CFS NIH program was moved from NIH to the Office of the Director in 1999 and then in 2002 to the Office of Research on Women’s Health (ORWH). The CFS program had originally been placed in the National Institute of Allergy and Infectious Diseases (NIAID) because of the early association with EBV but was moved to ORWH, according to staff, to make it easier to reach across institutes.103 But given the record of statements of HHS leaders like Dr. Straus104 and Dr. Reeves and the way that NIH’s February 2000 CFS “State of the Science Consultation” was conducted, it’s necessary to question whether that decision to move CFS out of NIAID was, at least in part, a political decision that reflected the belief of some staff at NIH and HHS that this disease was caused by psychological and behavioral problems.105 But whatever motivations were in play at the time, the transfer to ORWH coincided with a further marginalization of the disease and did little to improve access to research funds. For its part, CDC held a series of closed workgroup meetings between 2000 and 2002 to discuss the ambiguities with Fukuda that were causing substantial difficulties and inconsistencies in how cases of CFS were determined.106 These workgroups also discussed how to uniformly apply standard instruments (largely patient-reported) to measure symptoms like fatigue, how to assess psychiatric comorbidity and how to identify the dimensions of symptoms in patients with unexplained chronically fatiguing illnesses, including but not limited to CFS. Betraying CDC’s primary focus on medically unexplained fatigue and the dismissal of ME’s hallmark symptoms, the resultant paper,107 published in 2003, stated that CFS is “defined by unexplained disabling fatigue and a combination of non-specific accompanying symptoms.” It also eased Fukuda’s earlier restrictions on previous major depressive psychiatric illness and further emphasizing the non-physical nature of the disease, stated that the existence of any physical signs (as opposed to symptoms reported by patients) “should prompt the search for alternative diagnoses.” The paper then recommended a set of largely patient-reported instruments and defined specific cutoffs to assess the various symptoms of the disease. Finally, demonstrating the broader scope of disease under consideration in CDC’s newly defined approach, the paper called for empirical studies that would “delineate the different syndromes contained in unexplained fatigue.” This was not a definition designed to describe ME. In 2005, CDC published “Chronic Fatigue Syndrome – A clinically empirical approach to its definition and study”, based on the 2003 paper and the results of the called for empirical study.108 The study examined patients that had come from an earlier CDC surveillance study that had used the Fukuda definition (Wichita 2000) but the report noted that the diagnosis of CFS in this study was not consistent with how these same patients had been diagnosed in the earlier study. In fact, only 28% maintained their original diagnosis of CFS,109 indicating that 72% May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 16 no longer had CFS. This is a remarkably high number, given that so few ME patients are known to recover.110 And yet, remarkably, the report concluded that the study had proven that the Empirically defined approach addressed the lack of reproducibility and consistency seen with the use of Fukuda and that the approach was capable of distinguishing between CFS and chronic fatigue. Finally, the report recommended the use of the Empirical approach for both research and for clinical evaluation and follow-up care. CDC went on to use this “Empirical approach to defining cases of CFS” in other studies. First, CDC performed a prevalence study in Georgia,111 which reported a ten-fold increase in the prevalence of CFS over CDC’s earlier Fukuda-based prevalence estimates and a 6-fold increase over Dr. Jason’s earlier prevalence estimates. In fact, at 2.54%, the rate of prevalence seen in this study was higher than the 2.2% that Professor Wessely found in a study that used the Oxford definition, as noted above. Yet, remarkably, in an editorial published in the same journal at the same time as the study was released, Professor Peter White, of the Barts and London School of Medicine and Dentistry embraced this increased prevalence and called for broadening CFS even further. He stated, “Our current criteria for diagnosing CFS are arbitrary, and we need to widen the net to capture all those people who become so chronically tired and unwell that they can't live their lives to their full potential.”112 A similar recommendation was made in two studies published by CDC staff in 2009;113,114 one of these studies, on which Professor Peter White was also an author, reported that the defining variables of CFS were obesity, sleep problems, depression, and the multiplicity of symptoms. It is undoubtedly true, as Professor White said, that there are people who are chronically tired and unwell” for a variety of reasons that may include issues like depression, sleep problems and obesity. But neither of these studies nor Professor White’s editorial demonstrated how lumping all these patients together as one undifferentiated group was a scientifically appropriate way to study the problem. And none demonstrated how broadening the CFS criteria even further would advance an understanding of ME. CDC also used the Empirical approach to study more than prevalence; the Empirical approach was used to assess what factors, including risk factors, were associated with CFS.115 In 2007, Dr. Jason reviewed the findings of a number of these studies.116 For instance, according to Dr. Jason, Dr. Brian Gurbaxan of CDC reported in 2006 that depression was the single factor best capable of distinguishing between CFS and controls but found little association with 20 biological factors.117 Further, in 2009, Dr. Christine Heim of Emory University, in collaboration with Dr. Reeves of CDC, reported that childhood trauma was associated with a 6-fold increased risk of CFS.118 In 2010, Dr. Urs Nater, of CDC and Emory University reported that CFS was associated with an “increased prevalence of maladaptive personality features and personality disorders.”119 Empirical studies were still being reported as late as 2012 when Dr. Nater reported that CFS was associated with maladaptive coping styles.120 But given the broader scope of “CFS” cases encompassed by the Empirical approach, it is critical to ask whether these patients actually had ME, since these interpretations were based on tautological reasoning.121 For example, if patients with psychiatric issues are merged into a cohort of “CFS” patients because the patients with psychiatric illness suffer memory and sleep problems and meet a vague CFS definition, then of course the resultant combined patient groups might have higher instances of childhood trauma or maladaptive coping, as the inclusion of primary psychiatric illness has skewed the results. Those outside of CDC quickly decided that the Empirical approach to determining which May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 17 patients had CFS was deeply flawed. In a 2008 paper evaluating the 2005 Empirical approach,122 Dr. Leonard Jason raised concerns with the dramatic increase in prevalence and also reported that 38% of major depressive disorder patients were misdiagnosed as having CFS. Dr. Jason also highlighted the fact that changes in the approaches used to assess cases of “CFS” could increase the percentage of “CFS” patients that had psychiatric or other conditions while failing to require that patients had the hallmark criteria of ME. Dr. Jason further noted that these assessment approaches and criteria might lead to the conclusion that only “distress and unwellness characterize CFS, thus inappropriately supporting a… construct called ‘functional somatic syndrome’.” Collectively, these factors would result in a broader range of patients being given a diagnosis of CFS, including those with primary psychiatric illness and also result in CFS itself being equated to psychiatric illness. Given the above noted problems in diagnosing cases of CFS, Dr. Jason has also questioned the validity of numerous studies that used the Empirical approach. For instance, using stricter disease criteria, he reported that a history of abuse was not a significant predictor of chronic fatigue syndrome.123 Dr. Jason did report that a history of child abuse was positively associated with other conditions, like PTSD and anxiety disorders, that can have associated fatigue.124 This finding is relevant because some of these patients could potentially qualify for a diagnosis of CFS. One source of confusion that needs to be highlighted involves how the 2005 “Empirical approach to the study of CFS” is referenced by CDC and in the literature. Many outside of CDC refer to the definition as the Empirical definition, the “standardized approach” or the 2005 Reeves definition. But CDC staff state that the 2005 definition is not an empirical definition but rather an operationalization of Fukuda and prefers to refer to this definition as the Fukuda definition.125 Some publications do the same.126 Given the dramatic increase in prevalence when using the Empirical approach and the concerns highlighted above, doing so only further confounds the muddled situation. Therefore, for purposes of clarity, this paper uses the name “Empirical definition” to refer to the “Empirical approach to defining cases of CFS” laid out in the 2003 and 2005 papers. While the Empirical definition has been largely discredited outside of CDC, CDC and other parts of HHS still use an upper prevalence limit of 4 million, a level that appears to be based on the findings of Empirical studies.127In addition, CDC has stated on a number of occasions that the Empirical definition describes the same set of patients as Fukuda in spite of the 10-fold increase in prevalence.128 CDC’s analysis demonstrating this equivalence has not been published. Most concerning for the future of ME research and clinical care of ME patients, as discussed further below, CDC has suggested that the IOM initiative use data from the CDC population-based surveillance study in its development of a new case definition. The most recent of the CDC surveillance studies was the Empirical study noted above. Given the problems noted with the Empirical definition, it’s difficult to understand the applicability of that data if the new IOM clinical criteria are intended to be specific to ME as described by patients and as defined by the Canadian Consensus Criteria and the ME International Consensus Criteria. Britain’s NICE criteria During the years when the U.S. was developing and using the Empirical definition, Britain developed the NICE Guidelines for CFS/ME,129 which were published in 2007. The NICE Guidelines were based in part on the York evidence review, which treated the various CFS definitions and studies as directly comparable.130 The resultant NICE guidelines are part diagnostic criteria but also include recommendations for management of CFS. Diagnostically, May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 18 NICE requires that patients have unexplained fatigue that is persistent, has resulted in a substantial reduction in activity and is characterized by post-exertional malaise. NICE then specifies that patients have one additional symptom out of a list of 10 non-specific symptoms that are similar to the Fukuda symptom list. Like Fukuda, NICE recommends a minimal set of diagnostic tests. It specifically excludes tests that ME experts routinely use (e.g. the tilt-table test to assess autonomic issues and serological testing for pathogens) and also recommends against the drugs, like fludrocortisone and antivirals, that experts use to treat these conditions. Finally, the guidelines also recommend against the use of supplements and against maintaining activity at lower levels in order to allow the body to heal. Instead, NICE recommends sleep hygiene, relaxation, GET and CBT. The rationale for CBT is to get the patient to “avoid overvigilance to symptoms” and to examine the “challenging thoughts and expectations” and relationship between “thoughts, feelings, behaviors and symptoms” that may affect the person’s state of illness. Not surprisingly, the NICE guidelines for CFS reflect the biopsychosocial approach to CFS outlined above. The implications for patients with ME is obvious. Normally in Britain, clinical guidelines like those for CFS would be reviewed every 2 years. But the NICE guidelines for CFS were placed on the static list in early 2014, which means they will not be reviewed for 5 years. The rationale for this was that NICE was not aware of any upcoming studies that would require an earlier review or call into question the current guidelines. But patient groups have broadly objected to this decision not only because of emerging science but also because the current recommendations ignored existing biomedical studies and instead focused on behavioral theories and approaches to treatment.131 Resurrecting ME In contrast to the overly broad “CFS” definitions discussed above, internationally recognized ME experts have established disease-specific definitions that much more accurately describe the neurological, immunological, autonomic and energy production impairment of ME and require hallmark symptoms like post-exertional malaise, unrefreshing sleep and cognitive dysfunction for a diagnosis of ME. The first ME definition was the 1986 Ramsay Criteria described above. Following that was the London Criteria, developed in 1994.132 The London Criteria was released in a report from a national task force on CFS and appears to only have been used in a few studies, most notably a study showing brainstem hypoperfusion. In 2003, a group of ME experts published the Canadian Consensus Criteria (CCC).133 The CCC shifted from the singular focus on the ubiquitous symptom of fatigue to a focus on the hallmark symptoms of the disease. Unlike the Oxford, Fukuda and Empirical CFS definitions, the Canadian Consensus Criteria requires that patients have the hallmark symptom of postexertional malaise plus fatigue, unrefreshing sleep and pain. In addition, patients must also have two or more neurological/cognitive symptoms plus at least one symptom from two of the following categories: autonomic, immunological & neuroendocrine manifestations. Primary psychiatric illness is not allowed. The Canadian Consensus Criteria established the term “ME/CFS”, intended to be a bridging term but that in hindsight may have contributed to the definitional confusion as discussed further below. Dr. Luis Nacul of the London School of Hygiene and Tropical Medicine, published the results of a large study in 2011 that used both the Canadian Consensus Criteria and the Fukuda definition to assess the prevalence of CFS and ME in a group of 143,000 people in the U.K. He found a May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 19 prevalence of 0.19% for patients meeting Fukuda criteria but only a prevalence of 0.11% for those meeting the Canadian Consensus Criteria – roughly one half that of Fukuda.134 (Table 2) The Canadian Consensus Criteria has been used in both clinical care and in research, is widely respected by patients and experts alike and provides significant information, including additional testing like tilt table testing, cortisol levels and NK cell activity that would aid a clinician in diagnosing ME. In addition, the Canadian Consensus Criteria has been used as the basis of clinical guidelines published by the International Association for CFS/ME (IACFS/ME), the “IACFS/ME Primer for Clinical Practitioners,”135 which is now in its second edition and includes additional information on diagnostics. Both the requirement for the hallmark criteria of post-exertional malaise and the exclusion of primary psychiatric illness are important differentiators between the Canadian Consensus Criteria on the one hand and the CFS definitions on the other, which only exclude certain psychiatric illness but allow others. The exclusion of psychiatric illness is also an important differentiator from the biopsychosocial theory of CFS, whose proponents have stated that as many as 70% of CFS patients have a psychiatric disorder preceding their CFS onset.136 In 2006, a pediatric ME definition was also published137 that was based on the Canadian Consensus Criteria and similarly requires post-exertional malaise and other hallmark criteria. In 2011, a group of 26 ME experts from 13 countries with a total of 400 years of experience with the disease published the ME International Consensus Criteria (ME-ICC),138 which used the Canadian Consensus Criteria as its basis. The ME-ICC dropped the 6-month waiting period seen in the earlier criteria and also dropped the requirement for fatigue. Instead, the ME-ICC distinguishes between the fatigue seen in other conditions and the fatigability seen in ME.139 It emphasizes the abnormal response to exertion and the post-exertional exacerbation of all symptoms, which the ME-ICC refers to as post-exertional neuroimmune exhaustion (PENE). (This paper uses the term “PEM” or “PEM/PENE” to refer to this post-exertional exacerbation of symptoms.) The ME-ICC also reintroduces the requirement that the disease result in a 50% reduction in premorbid activity, a requirement that had been seen in the Holmes definition. In addition to post-exertional neuroimmune exhaustion, patients must also have neurological symptoms, symptoms reflecting immune, gastrointestinal and genitourinary dysfunction and a symptom reflecting energy production and transportation impairments, including cardiovascular and respiratory issues. Like the CCC, the ME-ICC provides information that helps the clinician better understand the disease and also provides specific information, including specific signs like lowered anaerobic threshold that can help the clinician diagnose the disease. The ME-ICC has also been used as the basis of the “International Consensus Primer for Medical Practitioners”140 published by many of the authors of the ME-ICC. The ME-ICC has only recently been used in published studies and does not appear to have been used in prevalence studies yet. Finally, in response to the confusion that has resulted with the use of overly broad CFS definitions and interchangeable names, the ME-ICC adopted the name ME as the name of the disease and called for patients that met the ME-ICC to be removed from the broader CFS definitions. Some countries and at least one insurance company have moved to adopt these criteria. The Scottish Public Health Network has recommended that the Canadian Consensus Criteria be adopted clinically for the diagnosis of ME, because it better reflects the neurological nature of the disease, while recommending that the NICE criteria be used for CFS. 141 Professor Wessely objected to the recommendation to adopt the Canadian Consensus Criteria for ME in part May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 20 because he objected to the inclusion of certain neurological symptoms in the definition and because the report expressed reservations regarding CBT and GET for ME patients.142 Euromut, a Belgian health insurance company, has also endorsed the Canadian Consensus Criteria for the diagnosis of this disease, which the report stated was called CFS in Belgium and ME in Netherlands.143 The Public Health Agency of Canada lists the 2003 Canadian Consensus Criteria in the “A to Z” listing of diseases and clinical criteria on its public website.144 Finally, for its part, the Norwegian Health Directorate circulated a draft recommendation in 2012 that recommended ME-ICC and Fukuda for diagnostic criteria.145 It appears that at this time, the Norwegian Health Directorate supports the use of the Canadian Consensus Criteria and Fukuda.146 And just as importantly, in 2011, following the publication of the positive effect of Rituxan in ME patients, the Norwegian Directorate of Health apologized to ME patients, stating "I think that we have not cared for people with ME to a great enough extent. I think it is correct to say that we have not established proper health care services for these people, and I regret that."147 But in the U.S., Health and Human Services has refused to adopt either the CCC or the MEICC. Both CDC and secondary medical education providers continue to use Fukuda, originally designed for research, as the foundation of clinical diagnostic criteria in clinical guidelines and fails to require hallmark criteria like PEM. The Problem with the Name It’s impossible to imagine a more trivial and misleading name than “chronic fatigue syndrome” as the name is too easily equated with simple tiredness. As a result, patients have encountered extensive stigma and disbelief. As Laura Hillenbrand, author and ME patient expressed it, “This illness is to fatigue what a nuclear bomb is to a match. It’s an absurd mischaracterization.”148 According to advocate Craig Maupin, Dr. Anthony Komaroff, one of the authors of the Holmes definition, noted that this impact was not anticipated when the term was coined, stating, “None of the participants in creating the 1988 case definition, and the illness name, ever expressed any concern that the name might appear to trivialize the illness. We simply were insensitive to that possibility, and we were wrong. Since ‘fatigue’ is an universal human experience, I’m afraid some people have responded to the word ‘fatigue’ in the name by thinking ‘I’m tired now and then like everyone, 'Why is this illness?'”149 Dr. Jason confirmed this reaction. In a study that examined the responses of both medical trainees and college undergraduates to the labels “chronic fatigue syndrome” and “myalgic encephalopathy”, Dr. Jason found that the participants’ perceptions of the illness and its severity was related to the label given to the illness150 and that “the “myalgic encephalopathy” label was associated with the poorest prognosis. He also found that it was more likely to be associated with a physiological rather than a psychological cause of the illness.” In 2001, at the recommendation of the CFS Coordinating Committee (CFSCC), a Name Change Workgroup was organized to assess the issues involved in changing the name. The committee ultimately recommended the illness be called “neuroendocrineimmune dysfunction syndrome (NDS)” in recognition of the range of systems affected.151 Because the CFSCC was disbanded before reviewing the Workgroup recommendations, the newly formed CFS Advisory Committee (CFSAC, the current advisory committee that advises HHS on this disease) reviewed this recommendation in 2003. CDC’s Dr. Reeves spoke against adopting a new name because among other things, he said it could set back medical research. The CFSAC ultimately tabled the name change recommendation and no further action was taken. Dr. Reeves’ concern is still May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 21 raised by some today. But that concern seems trivial compared to the problems that have arisen from using the same label, “CFS”, for such disparate and non-specific definitions. Today, CFS is the official label used for both Fukuda and Oxford. Doctors in the U.S. diagnose patients with “CFS” even if the patient meets the CCC or ME-ICC criteria.152 The Canadian Consensus Criteria uses the hybrid term “ME/CFS” and the NICE guidelines use the term “CFS/ME”. But the fact of the matter is that all of these terms – “CFS”, “ME”, “CFS/ME” and “ME/CFS” and even just “chronic fatigue” – are being used interchangeably with little regard to the underlying definitions and associated disease theories, creating a linguistic babel that thwarts all attempts at a shared understanding of meaning. Think about it this way. We know the difference between a Macintosh Apple (the fruit) and an Apple Macintosh (the computer) even though the labels use the same words. But imagine if people flipped the terms around willy-nilly, saying Apple Macintosh when they really meant a piece of fruit. You would be thinking internet and they would be thinking food. That‘s exactly what happens in this area. It’s surreal to watch people communicate past each other, thinking that they are talking about the same thing because they use the same words but fundamentally talking about different things. The Classification of CFS in Medical Dictionaries Another issue that has contributed to the confusion on the nature of this disease is the handling of the classification of CFS in the medical dictionaries that are used for medical records, insurance billing and mortality and morbidity tracking. This issue is important because these dictionaries influence how medical providers view this disease - that is, whether they see it as a real disease or a non-specific symptom and whether they view the disease as organic or psychiatric. The first of these medical dictionaries is the International Classification of Diseases (ICD) published by the World Health Organization. As mentioned earlier, in 1992, the WHO categorizes the term “CFS” as a neurological disease and has assigned it the same code (G93.3) as that used for ME.153 The National Center for Health Statistics (NCHS, part of CDC), which is responsible for ICD implementation in the United States, originally intended to follow suit in the U.S. version of the ICD-10 (the ICD-10-CM).154 But by 2004, in parallel with the studies being done with the Empirical Definition, NCHS made the decision, apparently without the input of disease experts or the public, to reclassify CFS from the neurological chapter to the ‘Symptoms and Signs” chapter of ICD-10-CM as a subtype of “chronic fatigue” under the heading of “Malaise and Fatigue”.155 That made CFS little more than a footnote of one of its symptoms. Despite repeated requests by CFSAC, patients and the IACFS/ME to move CFS back to the neurological chapter and despite this change being in violation of standards set by WHO, NCHS declined to move CFS back to the neurological chapter.156 While the exact date of rollout of ICD-10-CM has not been finalized (October 2015 is a possible date),157 when it is rolled out, CFS will be classified in the Symptom chapter. According to this classification, CFS is not an illness at all but just a symptom, the goal that Dr. Straus had articulated in his letter to Dr. Fukuda in 1994. Issues have arisen with the classification of CFS in the U.K as well. In 2001, the U.K.’s WHO Collaborating Centre at Kings College in London categorized CFS as a mental health illness equivalent to neurasthenia in the U.K.’s “WHO Guide to Mental Health in Primary Care.”158 This caused a number of authors and even textbooks to state that CFS was either classified as both a neurological and psychological illness or classified only as a psychiatric illness.159 However, the World Health Organization itself issued a ruling in 2001 and again in 2004 that these statements were incorrect and that the correct classification of CFS in ICD-10 was as a May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 22 neurological disease and not also as a psychological disease.160 WHO’s ruling and categorization of CFS as a neurological disease reflects the ICD-10 handling of other diseases like Alzheimer, which might have psychological symptoms like irritability as part of the disease but which is classified as a neurological disease. ICD-11 will allow a single term to be coded in two chapters.161 The second of these medical dictionaries is the controversial Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association in 2013. The DSM-5 contains a new disorder called “somatic symptom disorder” (SSD), which “is characterized by [6 months or more of] somatic symptoms that are either very distressing or result in significant disruption of functioning as well as excessive and disproportionate thoughts, feelings and behaviors regarding those symptoms.”162 SSD can be diagnosed in any patient, regardless of whether their symptoms are medically explained or not,163 as long as the medical provider determines that the patient is “excessively concerned” with his health. The DSM-5 does not specifically mention the terms “CFS” or “ME”, but CFS is often cited in the literature as the exemplar of somatoform illness, of medically unexplained symptoms (MUS) and of functional somatic syndromes, all of which are alternative or older terms associated with the concept of “somatic symptom disorder.”164 In fact, both Professor Simon Wessely and Professor Michael Sharpe, two of the Oxford definition authors, have taken the position that CFS, along with IBS, fibromyalgia, and a few other conditions are all examples of functional syndromes that are extremely similar and that can be effectively managed in the same way.165 In addition, Professor Wessely presented at a 2006 conference on “Somatic Presentation of Mental Disorders”, held by the American Psychiatric Association in collaboration with WHO and NIH, where he gave essentially the same message, tagging CFS as a functional somatic syndrome.166 Numerous experts, including particularly Dr. Allen Frances, chair of the DSM-IV Task Force, have highlighted the serious risk of over-psychologizing of bodily symptoms that can result from the misuse of the DSM-5’s SSD, especially since the judgment of when to diagnose SSD is “based on vague wording that can't possibly lead to reliable diagnosis.”167 This is not just an academic concern. Dr. Frances and also Dr. Diane O’Leary of Diagnostic Rights168 have pointed out that defining somatic symptom disorder too broadly leads to medical conditions being dismissed without proper investigation. In a letter to the DSM-5 Workgroup responsible for the SSD category, Dr. Frances warned of the impact of such a misdiagnosis, stating “When psychiatric problems are misdiagnosed in the medically ill, the patients are stigmatized as 'crocks' and the possible underlying medical causes of their problems are much more likely to be missed.”169 Expanding further on Dr. Frances’ point, Dr. O’Leary noted the example of female heart attack patients under the age of 55 who are 7 times more likely to be sent home from the E.R. than males of the same age under the assumption that their problems are not real. She also noted that, according to a survey of the American Autoimmune Diseases Association, “a staggering forty-five percent of autoimmune disease patients report having been denied medical care because doctors mistakenly diagnosed their symptoms as somatoform.” The risk of a misdiagnosis of SSD as defined by DSM-5 is significant, as demonstrated in a recent study of 6200 fibromyalgia, rheumatoid arthritis and osteoarthritis patients that found that 90% of fibromyalgia patients would be diagnosed with a mental health disorder using the somatic symptom disorder criteria while a substantial portion of the rheumatoid arthritis patients would also be misdiagnosed.170 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 23 If the risk is great for cardiac and rheumatoid arthritis patients, then the risk is even more serious for patients with misunderstood diseases like ME. One example is Connecticut teenager Justina Pelletier who had been diagnosed with mitochondrial disorder but then was rediagnosed by another doctor with a somatoform disorder and held in a psychiatric facility against her family’s wishes.171 A similar story is playing out with a young ME patient in Denmark. Karina Hansen was diagnosed with ME by an ME expert but then forcibly removed from her home in February 2013 and placed into a psychiatric facility where she has been held against her will and treated for a functional somatic disorder by staff from the Research Clinic for Functional Disorders and Psychosomatics.172 The clinic is run by Dr. Per Fink, who advocates for collapsing the separate diagnoses of CFS, fibromyalgia, IBS and other “functional” diseases into the single diagnosis called “Bodily distress syndrome” (BDS), which he believes is a result of emotional and bodily stress that can be treated by CBT, GET and anti-depressants.173 Efforts are currently underway to develop the new version of the ICD (ICD-11) and to align the mental health chapter of the ICD-11 with the DSM-5.174 Both CFS and ME have been removed from the beta version, making it unclear how these terms will be handled going forward.175 Regarding somatic disorder, it is also unclear at this time what will be done to reconcile ICD-11 and DSM-5. At this time, it appears that one approach being considered is similar to the DSM-5 approach described above176 and another approach appears to be include aspects of the Dr. Per Fink’s concept of Bodily distress syndrome (BDS) as described above noted above. But regardless of how these issues are ultimately resolved, the handling of CFS in ICD-11 and the concept of somatic disorder in both ICD-11 and DSM-5 is likely to hurt and further stigmatize ME patients. Given the wide-spread definitional confusion, the lack of medical understanding of the disease and the fact that some name CFS as the exemplar of somatoform illness, ME patients are at high risk of being diagnosed with a somatic disorder. Disease Experts and HHS Face Off In October 2012, the CFS Advisory Committee (CFSAC), the committee that gives advice to HHS on issues related to this disease, recommended that HHS hold a “workshop… to reach consensus for a case definition useful for research, diagnosis and treatment of ME/CFS beginning with the 2003 Canadian Consensus Criteria.”177 They asked for the workshop to be held as soon as possible, preferably by the end of 2012. But in August 2013, with no further discussion with CFSAC, HHS suddenly and unilaterally announced their intent to contract with the Institute of Medicine (IOM) of the National Academy of Sciences to develop their own clinical diagnostic criteria.178 Patient advocates immediately objected, citing the fact that the contract was established unilaterally, that the study would use non-experts to create the new definition, and that the recent IOM study on treatment of Gulf War illness (GWI) had been roundly criticized by Gulf War advocates for using criteria (chronic multi-symptom illness) that were so broad “as to include nearly any human health condition.”179 Finally, ME advocates objected because the IOM, by its own admission, has had virtually no experience in developing disease criteria, with the only other study being the one for the new definition for chronic multi-symptom illness in Gulf War veterans. The final report from that study stated that it was unable to establish a new definition because of the state of the evidence for Gulf War Illness.180 Given that the evidence base for CFS is likely worse than that for Gulf War Illness, it’s hard to imagine how the IOM can make an evidence-based recommendation for this disease. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 24 It wasn’t just ME advocates who were concerned with the plans to have the IOM develop new criteria. In October 2013, fifty internationally renowned ME experts sent a letter to Secretary Sebelius calling on HHS to adopt the 2003 Canadian Consensus Criteria for both research and clinical care.181 The experts also urged HHS to abandon its plans to contract with groups like the Institute of Medicine (IOM) to develop its own criteria and stated that such efforts were wasteful, unnecessary and threatened to move “ME/CFS science backward by engaging non-experts in the development of a case definition for a complex disease about which they are not knowledgeable.” HHS refused to accept the experts’ recommendation to adopt the Canadian Consensus Criteria,182 in part because the Canadian Consensus Criteria does not include evidence from the last 10 years.183 The irony of that statement is that HHS has also rejected the significant, replicated evidence for PEM as a hallmark symptom that can be objectively measured and has also disputed PEM’s importance as a required symptom.184 One must ask to what extent the Canadian Consensus Criteria was rejected because it does not fit HHS beliefs about the nature of this disease. HHS’ Current Definition-­‐Related Initiatives Having rejected the consensus based definition agreed to by the experts, HHS is moving forward with the IOM initiative plus two other initiatives to create its own definition - the fourth definition to be created by HHS - that will shape the nature of this disease and how it is defined and researched for years to come. The IOM contract ultimately put in place is using a panel that includes ME experts as well as those unfamiliar with the disease to reach consensus on an “evidence-based clinical diagnostic criteria for ME/CFS for use by clinicians.”185 It will also recommend new terminology and define an outreach strategy for medical professionals. To achieve these objectives, the IOM will get input from the public and also from CDC’s multi-site study and NIH’s Pathways to Prevention study, described next. Most significantly, the new criteria are intended to describe “ME/CFS” which has been defined to include ME, CFS, “Chronic Fatigue and Immune Dysfunction Syndrome (CFIDS), Neuroendocrine Immune Disorder and other terminologies in use for this illness.”186 This is an overly broad, vague definition that never states what “this illness” is, a critical shortcoming giving the controversies with the CFS definitions outlined above. HHS has said that it will be up to the IOM panel to determine what specific disease these new diagnostic criteria will describe.187 But it is important to ask whether it is usual practice to commission such a mixed panel to not only develop diagnostic criteria but also first decide what scope of disease those criteria will describe. The second HHS initiative is CDC’s multi-site study, which is intended to “characterize patients with CFS or myalgic encephalomyelitis (ME) in the clinical practices of clinicians with expertise in CFS/ME.”188 No case definition is being used to guide patient selection. Instead, clinicians have been instructed to include patients with CFS, ME and also post-infective fatigue. This raises the questions of whether these terms represent the same disease and whether all the multi-site clinicians use the diagnostic labels in the same way.189 The first phase of the study focused on patient-reported outcomes while the second phase is adding in some lab tests. Given the importance of PEM as a mandatory, hallmark symptom of this disease, patient advocates requested that the multi-site study use the replicated 2-day cardiopulmonary exercise test (CPET),190 to objectively demonstrate which patients have PEM and the associated energy metabolism impairment. But CDC declined and instead is using one day of exercise that will be May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 25 followed up with cognitive testing. Unlike CPET, no study, to my knowledge, has demonstrated that this approach can objectively determine which patients have post-exertional malaise. The third initiative is NIH’s Pathways to Prevention (P2P) initiative (previously called the Evidence-based Methodology Workshop). The P2P process,191 intended for non-controversial areas of science, uses a review of the evidence by non-experts to make recommendations on “key questions”. These key questions are intended to be developed with input from disease experts who also select speakers for the P2P Workshop. But the rest of the process – the review and analysis of the evidence, the running of the workshop and the final recommendations are driven largely by “non-experts” who are not allowed to have ever studied, treated or published on this disease. In its response to the CFSAC recommendation to hold a workshop to reach consensus on the case definition, HHS originally stated that the P2P initiative was intended to address the research case definition.192 Some communications from HHS have stated that P2P is intended to identify gaps in research. The final protocol for the P2P evidence review193 includes a key question on the methods used to diagnose ME/CFS and a key question on the harms and benefits of treatments for ME/CFS.194 When first drafted by the P2P Workgroup, which included disease experts, the key questions asked how ME and CFS differ. But that question is now gone and in its place, differences across definitions are being framed as subgroups. The protocol inclusion criteria for the diagnostic question are stated as “symptomatic adults (aged 18 or older) with fatigue” with no other underlying diagnosis. Evidence from all definitions, including the Oxford definition, will be considered. Emphasizing both its clinical focus and its focus on fatigue, the protocol states the focus is on “the clinical outcomes surrounding the attributes of fatigue, especially post-exertional malaise and persistent fatigue… because these are unifying features of ME/CFS that impact patients.” It’s important to consider the statement that PEM is an attribute of fatigue in light of another disease, like congestive heart failure that is also associated with fatigue. One hallmark of congestive heart failure is shortness of breath but one would never say that shortness of breath is an attribute of fatigue or equate shortness of breath to fatigue in examining either diagnostics or treatments for congestive heart failure. But that is the essence of what is being done here – the disease is being boiled down to fatigue. PEM is being inappropriately relegated to an attribute of fatigue and other key criteria of the disease like cognitive, neurological and immunological dysfunction are not included in the description of the report focus. The protocol’s key questions ask how the nature and accuracy of diagnostic methods and the benefits and harms of treatments compare across the patients represented by these definitions. But can the accuracy of diagnostic methods and the effectiveness of and harm due to treatments be compared across definitions if those definitions ultimately do not describe the same illness? Would an evidence review ever combine Oxford CFS and multiple sclerosis based on the fact that both cause fatigue and then compare the accuracy of diagnostic methods and the effectiveness of treatments? Of course not. So what is the difference here? Is it just that ME does not yet have a proven medical explanation? There are a number of other concerns specifically with P2P as noted by advocate Jennie Spotila,195 that include the lack of transparency, the lack of input, the lack of clarity on P2P’s goal and the use of non-experts. Additionally, as currently framed, this initiative does nothing to address the need for a research case definition as called for in the original 2012 CFSAC recommendation that P2P was originally stated to address. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 26 More broadly, across these three initiatives, there are four significant and interrelated concerns. First, as the experts have pointed out, they have already reached consensus on the use of the Canadian Consensus Criteria for both research and clinical use and conducting separate initiatives to develop separate criteria is a waste of money and time and risks setting the science of ME backwards. Second, by continuing to lump all these disparate definitions together, by failing to ask if these definitions represent the same illness or not and by failing to even ask if the CFS umbrella of “medically unexplained chronic fatigue” is a scientifically valid clinical entity to begin with, these initiatives are at serious risk of perpetuating the damage that has been done to ME research and clinical care by the CFS rubric for the last thirty years. The disease described by the Ramsay criteria, the Canadian Consensus Criteria and the ME International Consensus Criteria should never have been lumped inside of the CFS rubric and does not belong there now. Third, IOM and P2P are using evidence-based approaches, with both the CDC multi-site study and the P2P initiative providing input to IOM. The evidence-based approach is a valuable tool used across many scientific areas. But the “CFS” evidence base has been deeply polluted by disparate definitions and unrelated patient cohorts that all use the same label. As noted above by CDC’s Dr. Reeves, it’s even problematic to compare studies that all used Fukuda,196 because it’s impossible to assess how patients were diagnosed with CFS. If it is impossible to compare across Fukuda studies, how can Oxford, Canadian Fukuda and ME-ICC be validly compared. What is the relevance of these comparisons if the patient cohorts do not have the same illness? Unfortunately, as noted above, P2P is doing what so many other CFS evidence reviews have done197 - boiling the essence of this disease down to medically unexplained fatigue, the only attribute shared across these disparate definitions. The final concern is the use of non-experts to review the evidence and make decisions for a disease about which they are unfamiliar, especially when those decisions depend on such a controversial evidence base. This is especially a concern with P2P, where non-experts are doing the analysis and review and producing the recommendations. In what other area of science or medicine would non-experts be asked to review such a controversial evidence base to make recommendations for such an ill-defined and ill-scoped area of science about which they know nothing? In what other disease have the recommendations resulting from such a process then been used to supplant the recommendations of those with specific expertise in the disease? When the fifty ME experts wrote to Secretary Sebelius calling for the adoption of the Canadian Consensus Criteria, they specifically recommended against initiatives like the IOM because such efforts are wasteful and unnecessary and risk setting the science backwards. And yet that is exactly what is happening. 3. Irreconcilable Differences – One Disease or Many HHS’ View: Many Definitions, The Same Disease Today, even before HHS’ latest initiative, there are currently at least 7 different definitions in use for “CFS” and “ME” (Table 1) and a total of 20 reported by one author,198 definitions that vary dramatically in terms of what symptoms and signs are required, whether primary psychiatric illness is included or excluded, the magnitude of the resultant prevalence rates (Table 2) and May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 27 the approaches and tools used to diagnose patients. The breadth of this diversity reflects a fundamental difference in conceptualization of the nature of the disease, which Dr. Beth Unger of CDC underscored at a recent CFSAC meeting when she asked “If a patient doesn’t have [post-exertional malaise], would you not manage them as a CFS patient?”199 CDC has reportedly taken a similar position in a recent submission to IOM, in which the requirement for PEM/PENE is described as a limitation of the Canadian Consensus Criteria and the ME International Consensus Criteria because patients who do not have PEM/PENE would be excluded.200 This dramatic differences in conceptualization of “CFS” are also seen in the incompatible and irreconcilable theories about the nature of the disease, with the biopsychosocial or somatic theories201 contrasting sharply with the neurological, immunological and energy production theories being investigated by ME experts. What makes this problem even worse is the fact that all of these disparate definitions are explicitly treated as thought they are equivalent to each other and that the patients that meet any of the different criteria can be managed in the same way. For instance, today, the CDC CFS website claims that all of these disparate definitions describe the same group of patients,202 a position that reflects the statement noted earlier where CDC said that the Empirical and Fukuda definitions describe the same set of patients in spite of a 10-fold increase in prevalence and increased psychiatric illness.203 Further, the CDC CFS website states that the same set of diagnostic and treatment approaches can used for all “CFS” patients, even if the diagnostic or treatment recommendation was studied against only one of the CFS definitions. In fact, the CDC CFS website goes one step further and states that these same guidelines can even be used for “CFS-like” illness, defined as 6 months of fatigue but not having the symptoms required by Fukuda.204 This has significant implications for the appropriateness of CDC’s diagnostic and treatment clinical guidelines for ME patients. For instance, as a result of these guidelines, patients who meet the Canadian Consensus Criteria are told to exercise based largely on Oxford studies, even though exercise, especially in the hands of someone unfamiliar with PEM, is known to harm ME patients and can result in prolonged and potentially irreversible crashes.205 The CDC is not alone in saying that the range of conditions that fall under the “CFS” rubric are equivalent and can be diagnosed and treated in the same way. Other medical education sites and a number of evidence-based reviews have taken a similar approach. For instance, reflecting the PACE trial, the KevinMD site, created in partnership with the American College of Physicians recommends cognitive behavioral therapy for all “CFS” patients to break “the cycle of effort avoidance, decline in physical conditioning and increase in fatigue.”206 There are also numerous examples of evidence-based reviews that treat evidence from across these definitions as equivalent based on the single symptom of fatigue;207 NIH’s current Pathways to Prevention Study is the most recent example of that. Sometimes, the patient cohorts don’t even need to meet one of the defined “CFS” criteria to be classified as “CFS”. In 2014, Cochrane published the protocol for a planned evidence review of GET in CFS.208 The protocol equates CFS to 6 months of medically unexplained, disabling fatigue and includes disorders other than CFS as long as 90% of the patients have 6 months of unexplained chronic fatigue. No other symptoms are required, certainly not PEM, and no exclusions were mentioned. Similarly, the 2008 Cochrane Evidence Based Review for CBT in CFS209 included Oxford, Fukuda, and Australian definition studies and also included studies where the symptom requirements of Fukuda were dropped or where no “CFS” definition was May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 28 used at all as long as the patients had just 3 or 4 months of fatigue. Using such evidence, the 2008 Cochrane Review determined that CBT was effective for all patients diagnosed with “CFS”. Similarly, the PACE trial stated that CBT and GET were effective for both CFS diagnosed by Oxford and also CFS diagnosed according to CDC criteria. The referenced CDC definition was the Empirical definition, which was then modified to only require that patients have symptoms for one week instead of 6 months as required by the definition.210 But what diseases and conditions did all of these patients really have? It’s important to understand that in each of these cases, these loose criteria would have included patients with a variety of conditions like depression or fatigue from other causes, not just patients with ME. For instance, these other patients could have had depression-related fatigue that might have readily responded to exercise that could harm an ME patient. Collectively, this kind of definitional gymnastics is bad science and has greatly compounded the confusion surrounding this disease. The View of ME Experts: Many Definitions, Different Diseases ME experts strongly disagree with CDC’s assertion that these definitions represent the same disease or spectrum of diseases, pointing out that Fukuda, Empirical and Oxford select pools of patients with significantly higher rates of primary psychiatric disorder, significantly lower rates of severe functional impairment and a significantly less abnormal immunological profile than that seen in the Canadian Consensus Criteria or the ME International Consensus Criteria. Further, as the experts point out, some of these CFS definitions describe little more than tiredness and include a broad spectrum of unrelated patients. It’s not uncommon for a hierarchical approach to be used in diseases like cancer and multiple sclerosis where patients are stratified based on factors like severity, nature of the disease progression, specific biomarkers or genetics. But this is the exact opposite. In this case, biologically unrelated patients are being grouped together based solely on the symptom of chronic fatigue for which no medical explanation has yet been found. Dr. Leonard Jason of DePaul University is one of the experts who has raised these concerns repeatedly through a set of papers published over the past decade. He has shown that patients meeting the Canadian Consensus Criteria or the ME International Consensus Criteria have “more severe symptoms and physical functioning impairment” than Fukuda and further notes that fewer people meet the CCC and the ME-ICC than those meeting Fukuda.211,212 Dr. Jason has also shown that Fukuda’s criteria of chronic fatigue plus symptoms of unrefreshing sleep, joint pain, muscle pain and impairment in concentration overlap with depression213,214 and that the Empirical definition resulted in 38% of patients with major depressive disorder being misdiagnosed with CFS as noted above. Dr. Jason further pointed out that key decisions like the criteria for CFS and the choice of psychiatric instruments were influenced by “a societal and political context in which CFS was assumed to be a psychologically determined problem,” impacting how patients were selected and studies conducted.215 Dr. Jason added that even when looking at just Fukuda studies, the patient cohorts can be very disparate because of the non-specificity of the definition and the way that the definition has been applied,216 a point also made by Dr. Reeves himself217 as noted above. Finally, Dr. Jason pointed out that such differences could lead to the widely divergent prevalence rates218 that have been seen (Table 2). Other authors reinforce Dr. Jason’s points. In a 2001 report reflective of the loosening of criteria seen in Fukuda, Dr. DeBecker of Brussels, Belgium, stated that the Holmes definition had had less clinical heterogeneity and more symptom severity than that seen in the Fukuda definition.219 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 29 In a 2004 study, Kennedy showed that three different groups of patients – those with CFS, Gulf War Illness and Organophosphate exposure – all met the Fukuda definition and yet had differences in simple, easily performed clinical outcome measures.220 As noted above, in a large study in Britain published in 2011, Dr. Nacul found that the prevalence of patients who met the Canadian Consensus Criteria was 0.11, about one half the prevalence of Fukuda CFS patients.221 Dr. Nacul further stated that symptoms related to issues like neurocognitive and immunological dysfunction were significantly greater in patients who met the Canadian Consensus Criteria than in Fukuda. Similarly, in 2012, Dr. Michael Maes of Maes Clinics in Thailand demonstrated that roughly 50% of Fukuda patients have post-exertional malaise, which coincided with more severe illness, more severe feelings of infection, greater neurocognitive impairment, and significantly higher levels of immune-inflammatory variables.222 He called for patients with PEM to have a case definition separate from those without PEM. In a 2013 review, Dr. Ekua Brenu or the School of Medical Science at Griffith University in Australia, demonstrated significant differences in the immunological markers between patients that met Fukuda versus those who met the ME International Consensus Criteria and that these markers were significantly correlated with physical function.223 In another 2013 paper that compared case definitions, Dr. Johnston further emphasized this point, stating that the Fukuda criteria are “broadly inclusive and, thus, more likely to select widely heterogeneous patient groups.”224 These concerns are not limited to just the Fukuda and Empirical definitions. Similar concerns have been raised with the Oxford definition and the biopsychosocial approach to CFS. In Britain, the 2006 Group on Scientific Research into Myalgic Encephalomyelitis (GSRME), chaired by Dr. Ian Gibson, a member of Parliament and previous professor of biology, was established to increase public understanding of scientific research, to evaluate progress in the development of a full program of research and identify research and funding requirements for ME.225 The final report stated that the Oxford definition was focused on little more than long-term tiredness and included a broad spectrum of patients. Dr. Gibson stated, “One problem with investigating CFS/ME is that the ‘Oxford Criteria’, the guideline for selecting patients for research trials, is very vague and focuses on fatigue rather than the numerous other symptoms of CFS/ME. As such, the knowledge we do have of the illness may have been gleaned from people who did not genuinely have the condition.” From the research perspective, there are a number of studies that reinforce these findings by demonstrating the specific neurological, immunological, autonomic and energy production problems described in the Canadian Consensus Criteria and the ME International Consensus Criteria. Some of these studies demonstrate the specific physical findings, such as those neurological changes and energy production impairment that can easily distinguish patients with ME from patients with psychiatric illness and deconditioning.226 This is an important counterpoint to those researchers who hold that as many as 75% of “CFS” patients can have psychiatric illness or that CFS patients are deconditioned. Some have proposed that these diverse perspectives are a reflection of the heterogeneity and complexity of “CFS” and that this represents a continuum or spectrum of illness. HHS has appeared to take this position, both in how it treats these definitions in its medical education and most recently in how it framed the IOM initiative and particularly in the P2P initiative, where differences are framed as subgroups. However, that view is not correct. Yes, ME, with its different triggers, the influence of genetics, differences in onset and levels of severity and how the disease progresses over time is undoubtedly heterogeneous. But the “heterogeneity” of “CFS” has been artificially created by lumping unrelated conditions together based on the May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 30 singular factor of medically unexplained fatigue and then treating them as though they are all the same disease or group of related diseases. Imagine attempting to study the nature of bluebirds by first lumping them together with dragonflies and flying fish because they all “fly” and all lay eggs. You would never be able to draw conclusions about how bluebirds breed or breathe. And yet, this is what we have done to ME for thirty years, dumped it into a wastebin of unrelated diseases with no scientific proof that they all belong together. Putting a sharp edge on this point, Dr. Bruce Carruthers, the lead author on the Canadian Consensus Criteria and the ME International Consensus Criteria, stated in 2011 “There is a poignant need to untangle the web of confusion caused by mixing diverse and often overly inclusive patient populations in one heterogeneous, multi-rubric pot called ‘chronic fatigue syndrome.”227 What is hardest to comprehend about the claim that these diverse definitions represent the same patients is that even HHS staff and others have previously stated that CFS is not a discrete diagnostic entity228 and/or that these definitions are not all the same. In 1996, reflecting the position he had taken in his letter to Dr. Fukuda in 1994, Dr. Stephen Strauss of NIH stated, “Neither the American [Fukuda] nor the Oxford criteria assume the [chronic fatigue] syndrome to be a single nosological entity."229 Dr. Judith Prins, who has supported the biopsychosocial theory, stated, “CFS is neither a distinct nosological disorder nor a discrete diagnostic entity.” 230 The CDC website at one point stated that ME is not the same as CFS although it no longer states that.231 Finally, a 2010 article co-authored by Dr. William Reeves stated, “The 1994 International CFS case definition and the Canadian Consensus Criteria are different and do not necessarily identify similar groups of ill persons... The physical findings in persons meeting the Canadian definition may signal the presence of a neurologic condition considered exclusionary for CFS.”232 Dr. Reeves was correct. The 2003 Canadian Consensus Criteria does not define the same group of patients as those defined by the 1994 Fukuda definition. Nor does the Canadian Consensus Criteria define the same patients as the 1991 Oxford definition. And that is exactly the point that the ME experts have been making. These definitions define different groups of patients. Lumping them all together based solely on the symptom of unexplained chronic fatigue and with no regard for the differences in the underlying biological pathologies is the antithesis of the kind of good science that made progress in cancer by carefully delineating the biological differences between patient groups. But ultimately, the perspective of these disease experts and the knowledge about the biology of ME has not mattered and this “web of confusion” around CFS has flourished for three decades. The View of ME Patients Patients have produced a body of literature - YouTube videos, books, testimony at CFSAC meetings, news stories and submissions to various studies like the current IOM and P2P initiatives and last year’s FDA review of Ampligen and the April 2013 FDA Patient Focused Drug Development Initiative233 - that gives a consistent view on the nature of this disease, a view that reflects the Canadian Consensus Criteria and the ME International Consensus Criteria. Patients have repeatedly rejected the Oxford definition, the Fukuda definition, the Empirical definition and the Nice Guidelines for the simple fact that these definitions do not describe the disease they have and because these definitions include patients who do not have their disease. Patients have consistently called out PEM as a mandatory hallmark feature, a badge by which they readily recognize each other. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 31 Patients have also consistently rejected the idea that this disease is psychological, a fact that is sometimes used against them by scientific publications and news articles that have erroneously stated that patients are “anti-psychiatric” or unwilling to accept any research that doesn’t fit their theory of the disease. For instance, Professor Wessely stated, “For many it is better to have an incurable disease such as CFS than a psychological disorder even if that might be treatable.”234 Dr. Brurberg of the Norwegian Knowledge Centre for the Health Services in Oslo stated that “patient groups and researchers with vested interests in the belief that ME is a distinct somatic disease seem unwilling to leave the position that ME is an organic disease only.”235 But such statements entirely miss the concerns of patients. Patients are not objecting to the support that psychiatry could provide in dealing with the tremendous physical, emotional, social and financial losses that these patients face. Nor have patients rejected the use of anti-depressants when those medications help with sleep dysfunction. What patients overwhelming object to is that some researchers, with the support of their governments, have focused on social, behavioral and psychiatric factors in the research, diagnosis and treatment of this disease while essentially ignoring the evidence for biological pathologies in ME. Such a singular focus on social, psychological and behavioral factors to the exclusion of biological factors is nonsensical and unscientific to ME patients whose vibrant health abruptly blew up. ME is not the first disease to be so trapped by psychological theories. The scientific literature is littered with examples of “medically unexplained” diseases being automatically redefined as “psychological illness” as discussed above. But stress reduction techniques and talk therapy didn’t cure stomach ulcers. Antibiotics did. Patients who have ME will not get better with talk therapy geared to convincing them that they are really not ill or with exercise to reverse their presumed deconditioning. ME patients will get better when there are therapies that effectively target the underlying neurological, immunological and energy production pathologies that wrack their bodies. It’s important to make one final note. In the wake of disputed findings that a retrovirus called XMRV was associated with this disease, there were reports that some researchers received death threats from patients or were attacked for researching psychological causes and treatments.236 It is unclear what the extent of the problem was but obviously death threats are never acceptable. However, there is understandably frustration and anger on the part of patients that they have had their lives so devastated while their disease is ignored, trivialized, denied or turned into a somatic disorder. And regarding death threats, the biggest death threat that I have seen is the threat of death that patients face at their own hand – the threat of suicide from being trapped in this Kafkaesque nightmare with no hope of escape. The View from the Outside The choices that have been made in how CFS has been defined affect more than just patients with ME. As a diagnostic entity, CFS has become a wastebin diagnosis that can be applied to anyone who goes to the doctor with a complaint of fatigue. For instance, one study found that over thirty percent of multiple sclerosis patients had first been misdiagnosed with CFS before being correctly diagnosed with multiple sclerosis.237 In Britain, a seventeen-year old patient, Sophie Coldwell,238 was diagnosed with “CFS” because of her fatigue. Ten days later, she died of leukemia. Patients with depression, sleep disorder and any number of other conditions can be easily misdiagnosed with CFS, which isn’t surprising given that the 2009 CDC study, noted above, said that depression, sleep disorders and obesity were key features of CFS.239 Then there are the patients diagnosed with CFS whose subsequent, serious illnesses are dismissed as not serious because they have a diagnosis of CFS. Toni Bernhardt shared the story of one May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 32 patient who was nearly released from the hospital with a potentially fatal case of pneumonia when the doctor dismissed him as not really sick because he had a “CFS” diagnosis.240 There’s a lesson to be learned here from somatic symptom disorder (SSD), another impossibly broad criteria that was discussed earlier. As noted above, Dr. Allen Frances has raised concerns about the potential for misuse of DSM-5’s somatic symptom disorder because it is so broad and poorly defined that it creates a serious risk of misdiagnosis.241 Dr. Diane O’Leary added to that point, stating, “there is an ethical imbalance inherent to any broad definition that needs to be considered carefully before any decisions are made.242 Speaking specifically of SSD, she states that defining SSD “too narrowly may obstruct access to mental health care, but defining it too broadly will create the opposite problem of obstructing access to needed medical diagnosis and care. Every time a doctor errs in using [SSD] to explain physical symptoms, a patient actually in need of medical care may be denied access to it.” As Dr. O’Leary further points out, such an overly broad definition becomes a real problem when doctors are advised to make early diagnosis of somatoform disorders in order to save time and reduce costs, based on the assumption that most complaints are somatoform in nature.243 How did SSD become so broadly and poorly defined when, as Dr. Frances says, “anyone with common sense” can immediately see that SSD is “impossibly broad and non-specific.”244 Dr. Frances suggests that at least part of the problem for SSD is that “experts always want to focus increased attention on their pet topic, want to expand its boundaries, and worry much more about missed than about mislabeled patients.” This is reminiscent of the concern Professor Peter White articulated in his 2009 editorial noted above when he called for widening the net to capture all who are “so chronically tired and unwell that they cant live their lives” to their potential.245There is likely also another factor at work in the case of somatic disorder – a different standard of scientific proof for some psychiatric diagnoses. Dr. Per Dalen, the Swedish psychiatrist, made this point, noting, “Many doctors would never let themselves be caught with woolly ideas about the possible causes of cancer, multiple sclerosis, or cardiovascular diseases. But just mention the word somatization, and they will feel free to engage in uncritical speculation.”246 Regardless of the reason, both influences have contorted the clinical entity called “CFS”. On the one hand, CFS has been defined so broadly and so imprecisely that it mistakenly capturing patients with other treatable illnesses, leaving them with inappropriate or no treatment while confounding the research, drug development and medical care for ME patients. At the same time, unproven disease theories like the biopsychosocial theory have contributed to the psychologicalization of “CFS”. The impact is predictable – ME patients are not being treated for the organic disease that they have. As Dr. Per Dalen noted for somatization, it is essential that we not accept the validity of the psychological theories that have been progressed without demanding the hard scientific proof that would justify it. It is equally essential that we demand hard scientific proof that justifies the creation of the overly broad CFS. 4. The Impact of Poorly Characterized Definitions It is clear that because of their non-specific fatigue-focused criteria and the failure to require hallmark symptoms like PEM, the “CFS” criteria – especially the Oxford, Fukuda and Empirical May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 33 definitions - are incapable of distinguishing ME from a variety of other unexplained fatiguing conditions that also meet the diverse “CFS” criteria but do not experience hallmark criteria like PEM. As a result, “CFS” is now a veritable Rorschach test, whose interpretation morphs depending on the person viewing it, the definition they employ, and the etiological theory they espouse. In one moment, we hear about studies claiming that “CFS” patients ‘recover’247 if they address their “unhelpful illness beliefs” and deconditioning with cognitive behavioral therapy (CBT) and graded exercise therapy (GET).248 Then, in the next moment, we hear that ME patients are having positive results with antivirals249 and drugs like Rituxan, which depletes B cells.250 That the concept of “CFS” varies so dramatically underscores the depth and breath of the problems that have resulted from how “CFS” has been defined as a clinical entity. The magnitude of the public health catastrophe that has resulted from this definitional chaos cannot be overstated. More than any other single factor, this is at the heart of our country’s tragic failure to address the ME crisis for the last thirty years. It has wasted precious dollars and time studying mixed patient cohorts that have no relationship to each other or to ME. It has polluted research, making it impossible to replicate findings across studies and casting doubt over all results. It has impeded the development of diagnostic biomarkers, leaving the diagnosis of this disease one of subjectivity and exclusion.251 It has virtually stalled drug development and made it almost impossible to attract private investment to the disease.252 It has resulted in flawed epidemiological studies and faulty, inflated prevalence numbers.253 As Dr. Vincent Racaniello pointed out in an article by David Tuller, it has generated such disdain and skepticism in the research community that researchers254 avoid the disease like early leprosy out of a fear that it could kill their careers. It has left clinicians confused on the very nature of this disease, ultimately viewing it as mental illness or a bogus disease. It has made it extremely difficult to get insurance reimbursement with most tests and treatments viewed as experimental. Worst of all, it has sentenced terribly disabled patients to abysmal clinical care and has dramatically altered the perception of ME by everyone, ensuring that neither the disease nor its victims are taken seriously and leaving its victims to perpetually rejustify both their disease and their debility.255 Dr. Bruce Carruthers summed up the situation simply when he said, “Patient sets that include people who do not have the disease [ME] lead to biased research findings, inappropriate treatments and waste scarce research funds.“256 Speaking of the web of confusion created by diverse CFS definitions, he further stated “We believe this is the foremost cause of diluted and inconsistent research findings, which hinders progress, fosters skepticism, and wastes limited research monies.”257 5. CFS as a Social and Political Creation It’s obvious from the history of “CFS” and the utterly irreconcilable views on the nature of the disease that the global concept of “CFS” today is not a reflection of the biology of the disease but is rather largely a product of social and political forces. Dr. H. James Wedner made exactly that point at the 1993 annual meeting of the Infectious Disease Society of America258 when he stated: CFS “is neither a disease nor a syndrome. It is a case definition based upon a list of definitional criteria developed by a committee… The criteria were constructed to accommodate not only clinical problems but also social and political ones.” May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 34 As noted above, Dr. Phillip Lee, U.S. Assistant Secretary of Health,259 made the same point when he said “Chronic Fatigue Syndrome is neither a disease nor a syndrome. It is a committee definition.” When myalgic encephalomyelitis achieved national attention as a result of the outbreaks in the 1980s, the disease had the unfortunate coincidence of being a complex, multi-system illness with a dizzying array of symptoms that primarily affects women. It fell in a no-man’s land between scientific disciplines with no discipline ‘owning’ it. Standard lab tests were all normal and the abnormalities that were found were ‘exotic’ or/and inconsistent. Early theories of a potential viral etiology lost what institutional support there might have been when the first antiviral treatment trial failed to deliver the expected efficacy. This made ME particularly vulnerable to the all too frequent tendency in the medical community for the failure to demonstrate organic disease to turn into proof of mental illness. ME has been particularly vulnerable to this because it primarily affects women and it didn’t have the “protection” that would have been conferred had it been “owned” from the onset by a particular scientific discipline. ME was truly an orphan disease, easy to ignore because the level of debility made patients invisible and treated as someone else’s problem by most of the mainstream medical societies. In such a vacuum, the players with the power and vested interest to do so – those within HHS responsible for this disease and a group of British psychiatrists – were the ones left to define the nature of this disease according to their own cognitive biases and with disregard for both ME patients and the small group of unaffiliated disease experts studying ME. And by at least 1987, these powerful players had decided that the disease seen in Incline Village was not an organic illness but rather non-specific chronic fatigue and/or a psychological problem. As Dr. Richman pointed out, this conceptual shift was paralleled by a significant shift in research that increasingly focused on psychiatric and psychosocial issues.260 But it wasn’t just that these groups were able to influence the evolution of disease criteria. They were able to exert influence in three additional ways. First, because these groups either had access to or controlled access to funds, a significant portion of the global money spent and studies done on CFS went to assessing psychological or behavioral problems in overly broad patient cohorts as opposed to the biological pathologies associated with ME. Examples include the studies on childhood trauma and personality disorders noted above and also the PACE trial noted above, which at 5.0 Million British Pounds was the largest and most expensive study ever done for this disease, costing more than NIH spends on this disease in one year. It should be no surprise that those recommendations – and the psychological theories behind them - are now making their way into medical education. The second factor was access to the media. When these studies were completed, these groups were able to broadcast the results to the world because of their ability to access the press while those who focused on biomedical research had much more limited access. For instance, in 2009, a number of news sources, including Science Daily, NewScientist and Medscape261 reported on a CDC Empirical definition study that found that childhood abuse was associated with a 6-fold increase in risk of CFS. In an article in Psychology Today, journalist Pamela Weintraub perceptively asked if the real issue was child abuse or abuse of research resulting from overly broad, ill-defined disease definitions.262 But her question was likely drowned out by the drumbeat of other publicity that reported the story as given to them, perverting the perceptions of doctors and the public alike about the nature of ME. Similarly, in 2013, PACE trial claims of recovery reverberated around the world, hitting major news outlets.263 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 35 Third, when ME patients inevitably objected to having their disease trivialized, and treated as a behavioral problem while the biological pathologies were ignored, these groups were able to leverage their access to media and the scientific literature to further delegitimatize patients by turning valid patient objections into proof that ME patients are irrational, anti-scientific or are so biased against psychiatry that they would rather stay sick than be helped.264 But when one steps back and really looks closely, there can be no question that the collective concept of CFS, as it has come to be defined today, is a political and social construct that has relatively little to do with the objectively observed biological pathophysiology of ME. So what motivated the creation of “CFS” to begin with and what has perpetuated the concept of “CFS” for thirty years? What social and political purposes were served that could have justified burying ME in this way? Why was the scientific and medical community so blind to the ample and long-standing evidence of the biological pathologies of ME and the hell of ME patients’ lives? Why have so many tolerated such definitional confusion and scientific sloppiness for so long without questioning the scientific validity of it? Was it simply the result of people’s conceptual and gender biases blinding them to the evidence of ME and the reality of ME patients? Did the kind of psychiatric expansionism noted in the DSM-5265 play a role? Was it because scientists were unwilling to criticize other scientists or else too busy in their own professional areas to pay attention? Did it serve a purpose as a diagnostic code for undiagnosable patients? Or did commercial interests somehow play a role?266 Dr. Straus’ letter to Dr. Fukuda makes it clear that part of the reason lies in a personal bias about the validity of this disease and a willingness to use one’s political power to make the disease “evaporate”. Beyond that, we can only speculate although it would be surprising if a number of these factors weren’t in play. But what we are certain of is that what has happened to ME patients is not only morally and ethically wrong but also scientifically wrong. One million Americans, seventeen million people worldwide, have been sentenced to a level of suffering, disability, abysmal medical care and disbelief that we could never have imagined until ME struck one of us, suddenly, arbitrarily and without any prior warning. We should all be incredulous that this situation came about to begin with. We should all be outraged that it has been allowed to thrive, virtually unchallenged, for three decades. We must demand that it stop now. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 36 7. Appendices and References Table 1: Summary of the primary CFS, ME/CFS and ME definitions The CDC CME “Diagnosis and Management of CFS” lists 5 definitions - Oxford, Fukuda, Canadian Consensus Criteria, ME-ICC and Pediatric. The Nice guidelines are used in Britain. Holmes is seldom if ever used today. Definition Label Key Symptoms in the Psychiatric Illness PEM ReComment Name Used (1) definition quired Holmes CFS 6 months chronic No Replaced by Fukuda. criteria fatigue eight symptoms Patients show more (1988)267 out of eleven signs of infectious process than Fukuda268 1991 Oxford CFS 6 months severe fatigue Schizophrenia, No PEM not recognized. 269 that affects mental or manic-depressive Myalgia, sleep, mood physical function. illness excluded. disturbance may be Anxiety, depression present – it &other allowed symptoms not required 1994 CDC CFS 6 months fatigue plus Major depressive & No PEM one of optional Fukuda270 any 4 of memory bipolar disorder, symptoms but not impairment, sore throat, schizophrenia required. Fukuda tender lymph nodes, excluded. Anxiety Includes more muscle pain, joint pain, somatoform & other depressed and less headaches of new type, types of psychiatric symptomatic patients 271 unrefreshing sleep, PEM disorder allowed than CCC 2003 ME/CFS PEM plus two Primary psychiatric Yes Requires PEM plus Canadian neurological/cognitive illness excluded combination of these Consensus plus 1 of autonomic, symptoms. 6 month Criteria immunological & wait (CCC)272 neuroendocrine symptoms 2005 CDC CFS Operationalization of Depression, anxiety, No Led to ten-fold Empirical Fukuda somatoform disorders prevalence increase. (Reeves) not exclusionary Jason has shown 38% Criteria 273 of patients with depression fit criteria.274 Pediatric ME/CFS 3 months of fatigue plus Schizophrenia, Yes 3 month waiting Case PEM, unrefreshing Bipolar, depressive period. Definition for sleep, neurocognitive, disorders ME & CFS pain plus one of exclusionary. May (2006) autonomic, have concomitant Jason et al 275 neuroendocrine, anxiety, depression, immune somatoform NICE CFS 4 months chronic Appears to allow Recommen Pain, cognitive and Clinical fatigue, PEM plus any primary psychiatric ds CFS be sleep difficulties Guideline one of 10 symptoms illness considered considered key. 276 (similar to Fukuda if PEM 3 months in child (2007) symptoms) exists 2011 ME ME PENE plus neurological, Primary psychiatric Yes Requires PENE plus International immunological, energy illness excluded combination of these Consensus metabolism /ion symptoms. No waiting Criteria (MEtransport, infections period ICC)277 1. Other less commonly used definitions can be found here: Brurberg, K., et al. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): a systematic review. BMJ Open 2014;4:e003973 doi:10.1136/bmjopen-2013-003973 http://bmjopen.bmj.com/content/4/2/e003973.long#T1 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 37 Table 2: Changing Prevalence Rates over time Prevalence estimates are suspect because of the varied “CFS” definitions, but the best estimates are that ME affects less than one million Americans of all ages, races, and socioeconomic groups and 17 million people worldwide. Prevalence estimates vary widely depending on the definition and methodology used. The following are the most of the major prevalence studies. The 2012 estimate is based on a U.S. census 278 population of 314M total population and 240M adults. Author Rate 2012 Reference estimate Gunn 1993 Modified Holmes For period 1989 to 1991 Price 1992 0.000073 2.0 to 7.3 per 100,000 6280 to 22,922 0.0074% (1 of 13,538) 23,236 Gunn, W.J., Connell, D.B., & Randall, B. (1993). Epidemiology of chronic fatigue syndrome: The Centers-for-Disease-Control study. In B.R. Bock & J. Whelan (Eds.), Chronic Fatigue Syndrome. (pp. 83-101). New York: John Wiley & Sons. http://www.ncbi.nlm.nih.gov/pubmed/8387910 Price RK, North CS, Wessely S, Fraser VJ (1992). Estimating the prevalence of chronic fatigue syndrome and associated symptoms in the community. Public Health Rep. 107: 514–522. need to confirm http://www.ncbi.nlm.nih.gov/pubmed/1329134 Wessely 2.2 /2.6% 6.908M for Wessely S, Chalder T, Hirsch S, Wallace P, Wright D (1997). The 1997 Oxford, prevalence and morbidity of chronic fatigue and chronic fatigue syndrome: a Oxford/ 0.7 /0.5% 8.164M for prospective primary care study. Am J Public Health. 87: 1449–1455. Fukuda when no Fukuda Multiple criteria were used. Oxford prevalence reported as 2.2% psych http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1380968/ Reyes 1997 0.00004 to 12,560 to Reyes, Gary, Dobbins, Randall, Steele, Fukuda, Holmes, Connell, Mawle, Holmes 0.000087 27,318 Schmid, Stewart, Schonberger, Gunn, & Reeves. Surveillance for chronic For period fatigue syndrome--four U.S. cities, September 1989 through August 1993. 1989-1993 MMWR CDC Surveill Summ. 1997 Feb 21;46(2):1-13. http://www.ncbi.nlm.nih.gov/pubmed/12412768 and http://www.cdc.gov/mmwr/preview/mmwrhtml/00046433.htm Jason – 0.0042 1,318,800 Jason, L.A., Richman, J.A., Rademaker, A.W., Jordan, K.M., Plioplys, A.V., 1999. (422 per Taylor, R., et al. (1999). A community-based study of chronic fatigue Fukuda 100000) syndrome. Archives of Internal Medicine. 159, 2129-2137. Survey of 28673 people in 1993 http://www.ncbi.nlm.nih.gov/pubmed/10527290 . Reyes 2003 0.0024 753,600 Reyes, Nisenbaum, Hoaglin, Unger, Emmons, Randall, Stewart, Abbey, Jones, Gantz, Minden, & Reeves Prevalence and incidence of chronic (235 per fatigue syndrome in Wichita, Kansas. Arch Intern Med. 2003 Jul 100000) 14;163(13):1530-6. http://archinte.jamanetwork.com/article.aspx?articleid=215827 Reeves 2007 0.0254 7,957,600 Reeves, W. C., Jones, J. J., Maloney, E., Heim, C., Hoaglin, D. C., Boneva, Empirical (6,096,000 R., et al. (2007). New study on the prevalence of CFS in metro, urban and – adults rural Georgia populations. Population Health Metrics, 5, Article 5. Available only) from http://www.pophealthmetrics.com/content/5/1/5 Nacul 2011 Nacul, L., Lacerda, E., Pheby, D., Campion, P., Molokhia, M., Fayyaz, S., Leite, J., Poland, F., Howe, A., Drachler, M. Prevalence of myalgic Canadian 0.0011 345,400 encephalomyelitis/chronic fatigue syndrome (ME/CFS) in three regions of England: a repeated cross-sectional study in primary care. BMC Medicine Fukuda 0.0019 596,600 2011, 9:91 doi:10.1186/1741-7015-9-91. http://www.biomedcentral.com/1741-7015/9/91 Vincent 2012 Vincent, A, Brimmer, D., Whipple, M., Jones, J., Boneva, R, Lahr, B., Fukuda 0.00071 222,940 Maloney, E., St. Sauver, J., Reeves, W. Prevalence, Incidence, and Classification of Chronic Fatigue Syndrome in Olmsted County, Minnesota, Fukuda w 0.00026 81,640 as Estimated Using the Rochester Epidemiology Project. Mayo Clinic PEM (36% of Proceedings Volume 87, Issue 12 , Pages 1145-1152 , December 2012 Fukuda) http://www.mayoclinicproceedings.org/article/S0025-6196(12)009238/references Fukuda with PEM called out under the working assumption is that this is an approximation for CCC. For more information, also see: Brurberg, K., Fønhus, A., Larun, L., Flottorp, S., Malterud, K. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): a systematic review. BMJ Open 2014;4:e003973 doi:10.1136/bmjopen-2013-003973 http://bmjopen.bmj.com/content/4/2/e003973.long#T1 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 38 Highlighted References Videos. 1. Story of two sisters with ME on German TV, "Menschen - das Magazin" (subtitled) Published on Apr 4, 2014 https://www.youtube.com/watch?v=fws-oAExvAs 2. 2011 “Voices from the Shadows” – Trailer http://www.youtube.com/watch?feature=player_embedded&v=fxZG4QVkO2k Web site http://voicesfromtheshadowsfilm.co.uk/ 3. Ben Di Pasquale May 2011 http://www.youtube.com/watch?feature=player_embedded&v=oeLal4nfrck 4. Laurel’s October 2009 CFSAC testimony - http://www.youtube.com/watch?v=LvweCk44WHs 5. Dr. David Bell discusses ME/CFS and a very severe 19-year-old patient. About 2010 http://vimeo.com/34099309 6. Kim Snyder, “I remember ME” released in 2000. http://www.youtube.com/watch?v=401--WCB5dc and http://en.wikipedia.org/wiki/I_Remember_Me 7. PrimeTime Live about 1996. Broadcast the same day as Hilary Johnson’s Osler’s Web was released. http://vimeo.com/13048135 and http://www.youtube.com/watch?v=AW0x9_Q8qbo. 8. 1993 Videos by CFIDS association. In the 20 years since these were made, the lack of change is disturbing a. http://www.youtube.com/watch?v=KGFVXacPuho b. http://www.youtube.com/watch?v=Q0EjR2yepHg c. http://www.youtube.com/watch?v=1stOT72UCQw d. http://www.youtube.com/watch?v=bGphVlRKovY e. http://www.youtube.com/watch?v=wD363vqG38U f. http://www.youtube.com/watch?v=ISteyLtnxOo 9. MacNeil Lehrer, Living Hell. Story about Tom Hennessey, 1992. https://www.youtube.com/watch?v=SyB49g_l9Sg 10. Nightline, 1987. Minute 7:20 http://www.youtube.com/watch?v=CqpvRC_YurY&feature=player_embedded Includes discussion over the nature of disease and whether its emotional, caused by stress, etc. 11. 20-20 program on CFS from 1985-86 - http://www.youtube.com/watch?v=4xdtVan0xko& Books and Articles 1. Jason, L. Principles of Social Change. Oxford University Presss, 2013. This book uses ME as the focus of some of its cases 2. Johnson, Hilary, March 2013, Chasing the Shadow Virus: Chronic Fatigue Syndrome and XMRV. Discover Magazine, http://discovermagazine.com/2013/march/17-shadow-virus#.Uc9q1utQ3es 3. 2012: Ranciello, Vincent, A tale of Two Viruses: Why AIDS was Pinned to HIV, but Chronic Fatigue Remains a Mystery. DIscover Magazine, January 2012. http://blogs.discovermagazine.com/crux/2012/01/12/hiv-in-xmrv-out-how-scientists-deduce-whatdoes-and-doesnt-cause-a-disease/ 4. 2011: Chronic Fatigue Syndrome and the CDC: A Long, Tangled Tale, David Tuller, November 23, 2011. http://www.virology.ws/2011/11/23/chronic-fatigue-syndrome-and-the-cdc-a-longtangled-tale/ 5. Laura Hillenbrand, Author and ME patient. Interview in 2011 http://well.blogs.nytimes.com/2011/02/04/an-author-escapes-from-chronic-fatigue-syndrome/ 6. Scott Jordan Harris review of Voices from the Shadows 2011 http://www.rogerebert.com/farflung-correspondents/a-howl-of-desperation-for-those-who-cannot-howl 7. Johnson, Hilary, Osler's Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic. Crown Publishing Group, New York. 1996. Extensively researched book that covers the handling of this disease both within and outside of the government from the start of the Incline Village outbreaks in 1984 until 1994. This also includes a discussion of the earlier outbreaks and a brief 2006 update. Available on Amazon. 8. Chronic Fatigue Syndrome, Newsweek, November 11, 1990. This article not only documents the early outbreaks but also gives a perspective on what was known at the time. http://www.thedailybeast.com/newsweek/1990/11/11/chronic-fatigue-syndrome.html May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 39 9. People Magazine, 1991 - Chronic Fatigue Victims Finally Get Some Respect—and Clues to the Cause of Their Misery. http://www.people.com/people/article/0,,20114907,00.html Summary of early ME epidemics (before 1980s) 1. http://www.meresearch.org.uk/wp-content/uploads/2012/11/ResearchPublications1934-1980.pdf Scientific Articles 1. Database of Research literature from 1956-2013 (as of June 2014). http://www.meresearch.org.uk/information/research-database/ Bibliography All references retrieved between January 2013 and May 2014. All translations done with Google Translate. 1 Dr. Malcolm Hooper wrote an article entitled “Magical Medicine: How to make a disease disappear.” Hooper’s writing has been very useful in the development of this document. The title echoes his title but also focuses on Dr. Straus’ hope that the idea of the disease would evaporate. • Hooper, Malcolm. “Magical Medicine: How To Make A Disease Disappear.” InvestInME. February 2010. http://www.investinme.org/Documents/Library/magical-­‐medicine.pdf 2 Straus, S., Komaroff, S., Wedner, H.J. Chronic Fatigue Syndrome: Point and Counterpoint. The Journal of Infectious Diseases. Vol 170, July 1994 http://www.jstor.org/stable/30133467 In 1993, Dr. Stephen Straus mediated a discussion at the annual meeting of the Infectious Disease Society of America. One of the speakers, Dr. H. James Wedner, Professor of Immunology and Allergy at Washington University and a clinician who had treated CFS patients, made the following statements: CFS “is neither a disease nor a syndrome. It is a case definition based upon a list of definitional criteria developed by a committee… The criteria were constructed to accommodate not only clinical problems but also social and political ones.” “…There has been a creeping movement to include other types of medical conditions under the rubric of CFS. For example, various forms of post-­‐infectious fatigue, fibromyalgia, and non-­‐psychiatric and depressive disorders were permitted by consensus of a National Institutes of Health (NIH) workshop. Somatoform disorders and panic disorder became part of what could be encompassed within the CFS case definition. This serves to broaden the scope of the clinical entity to the point at which it is no longer definable.” 3 The best descriptions of ME can be found in two case definitions and clinical guidelines. Definitions • Carruthers BM, van de Sande MI, De Meirleir KL, Klimas NG, Broderick G, Mitchell T, Staines D, Powles ACP, Speight N, Vallings R, Bateman L, Bell DS, Carlo-­‐Stella N, Chia J, Darragh A, Gerken A, Jo D, Lewis D, Light AR, Light K, Marshall-­‐ Gradisnik S, McLaren-­‐Howard J, Mena I, Miwa K, Murovska M, Steven S. Myalgic Encephalomyelitis International Consensus Primer for Medical Practitioners. 2012. http://www.hetalternatief.org/ICC primer 2012.pdf • Carruthers, B., et al Jain, A., De Meirleir, K., Peterson, D., Klimas, N., Lerner, M., Bested, A., Flor-­‐Henry, P., Joshi, P., Powles, A. , Sherkey, J., van de Sande, M. Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols. Journal of Chronic Fatigue Syndrome, Vol. 11(1) 2003. http://mefmaction.com/images/stories/Medical/ME-­‐CFS-­‐Consensus-­‐Document.pdf Primers • “ME/CFS: A Primer for Clinical Practitioners”. Published by IACFS/ME in 2012 and based on the Canadian Consensus Criteria. The IACFS/ME is an international organization of clinicians and researchers involved in the study of ME/CFS and the clinical care of patients with ME/CFS. http://www.iacfsme.org/Portals/0/PDF/PrimerFinal3.pdf • Carruthers BM, van de Sande MI, De Meirleir KL, Klimas NG, Broderick G, Mitchell T, Staines D, Powles ACP, Speight N, Vallings R, Bateman L, Bell DS, Carlo-­‐Stella N, Chia J, Darragh A, Gerken A, Jo D, Lewis D, Light AR, Light K, Marshall-­‐ Gradisnik S, McLaren-­‐Howard J, Mena I, Miwa K, Murovska M, Steven S. Myalgic Encephalomyelitis International Consensus Primer for Medical Practitioners. 2012. http://www.hetalternatief.org/ICC primer 2012.pdf A few additional notes and resources on ME • Although the etiology of ME is not yet known, much is known about the multi-­‐system dysfunction underlying these symptoms. University of Utah researchers Kathleen and Alan Light have objectively demonstrated dramatic changes in sensory, adrenergic and immune gene expression associated with post-­‐exertional malaise May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 40 • Staci Stevens, of Workwell Foundation, has used cardiopulmonary exercise testing to demonstrate the associated changes in energy utilization and anaerobic threshold that occur as a result of post-­‐exertional malaise. • In a 2011 review, Harvard researcher Anthony Komaroff reviewed the neurological abnormalities of the disease, including neurocognitive, sleep, autonomic, and sensory disturbances, cognitive impairments and pain along with changes in the brain that include hypoperfusion, reduced brain matter, and protein changes in the cerebral spinal fluid. • Beth Israel Deaconess Medical Center researcher Roy Freeman described the changes in sympathetic and parasympathetic functioning that underlie the orthostatic intolerance noted in ME patients. • ME researcher Nancy Klimas described immunological abnormalities that include chronic immune activation seen by elevated inflammatory cytokines; immune function defects seen in decreased natural killer (NK) cell function and viral reactivation. • Myhill described mitochondrial dysfunction as did Carruthers who also described oxidative stress, as well as cardiovascular impairment and abnormal thermoregulatory responses. • Given that ME, because of its association with “CFS”, has been conflated with depression, it is important to note that abnormalities like post-­‐exertional malaise, brain hypoperfusion and hypometabolism, joint and muscle pain, and headaches distinguish ME from depression. It is also worth considering the results of the Norwegian study of Rituxin in ME patients indicating the likelihood an autoimmune disease, given the effectiveness of B-­‐cell depleting drug in 67% of patients, for which all but patients but two in the placebo group met the Canadian Consensus Criteria as well as the Fukuda criteria. • Selected examples of peer-­‐reviewed articles that characterize this disease and the associated dysfunctions include the following: – Freeman, R. Komaroff, A. Does the chronic fatigue syndrome involve the autonomic nervous system? The American Journal of Medicine 1997:102:357-­‐364 http://www.ncbi.nlm.nih.gov/pubmed/9217617 – Komaroff AL, Cho TA. Role of infection and neurologic dysfunction in chronic fatigue syndrome. Semin Neurol. Epub 2011 Sep 30 http://www.ncbi.nlm.nih.gov/pubmed/21964849 – Light AR, White AT, Hughen RW, Light KC. Moderate exercise increases expression for sensory, adrenergic, and immune genes in chronic fatigue syndrome patients but not in normal subjects. J Pain. 2009 Oct;10(10):1099-­‐112. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2757484/?tool=pubmed – VanNess JM, Stevens SR, Bateman L, Stiles TL, Snell CR. Post-­‐exertional malaise in women with chronic fatigue syndrome. J Womens Health (Larchmt). 2010 Feb;19(2):239-­‐44. http://www.ncbi.nlm.nih.gov/pubmed/20095909 – Komaroff, A. Ten Discoveries about the Biology of CFS. 2008. http://www.cfids.org/about/10-­‐discoveries.pdf – Klimas NG, Koneru AO. Chronic fatigue syndrome: inflammation, immune function, and neuroendocrine interactions. Curr Rheumatol Rep. 2007 Dec;9(6):482-­‐7. http://cfids-­‐cab.org/cfs-­‐ inform/Reviewcfs/klimas.koneru07.pdf – Lange G, Streffner J, Cook D, Bly B, Christodoulou C, Liu W, Deluca J, Natelson BH. Objective evidence of cognitive complaints in chronic fatigue syndrome: A BOLD fMRI study of verbal working memory. NeuroImage 2005;26:513-­‐524. http://www.ncbi.nlm.nih.gov/pubmed/15907308 – Myhill, S. Booth,N., McLaren-­‐Howard, J. Chronic fatigue syndrome and mitochondrial dysfunction. Int J Clin Exp Med. 2009; 2(1): 1–16. Published online 2009 January 15. – Papanicolaou DA, Amsterdam JD, Levine S, McCann SM, Moore RC, Newbrand CH, Allen G, Nisenbaum R, Pfaff DW, Tsokos GC, Vgontzas AN, Kales A. Neuroendocrine aspects of chronic fatigue syndrome. Neuroimmunomodulation 2004;11(2):65-­‐74. http://www.ncbi.nlm.nih.gov/pubmed/14758052 – Fluge, O.; Bruland, O.: Risa, K.; Storstein, A.; Kristoffersen, E.; Sapkota, D.; Næss, H.; Dahl, O.; Nyland, H.; Mella, O. Benefit from B-­‐Lymphocyte Depletion Using the Anti-­‐CD20 Antibody Rituximab in Chronic Fatigue Syndrome. A Double-­‐Blind and Placebo-­‐Controlled Study. Plos One. Oct 2011. http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0026358 4 Presentation by Dr. Snell to CFSAC, October 12, 2010. Includes references to statements by various medical societies including the American Heart Association, about the use of CPET as a gold standard • Slides -­‐ http://www.hhs.gov/advcomcfs/meetings/presentations/presentation_10132010_snell-­‐ stevens.pdf • Video – starting at 4:38 -­‐ http://hhs.granicus.com/MediaPlayer.php?view_id=5&clip_id=99; http://media-­‐ 02.granicus.com:443/ondemand/hhs/hhs_b947e197-­‐a39c-­‐4c51-­‐8b89-­‐077723983c8c.mp3 5 Dr. Marc Loveless -­‐ (infectious disease specialist and head of the CFS and AIDS Clinic at Oregon Health Sciences University, in Congressional Testimony, CFS Awareness Day, May 12, 1995) "I have treated more than 2,000 AIDS and CFS patients in my career. And the CFS patients are MORE sick and MORE disabled every single day than my AIDS patients are, except for the last two months of life!" Also – “I Remember Me,” documentary in which Dr. Dan Peterson said that the disease can render the severely May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 41 affected as sick as AIDS patients in the last two months of their lives. – The CDC has said that the disease can be as debilitating as multiple sclerosis and congestive heart failure. 6 Jason, Chu Patient Survey in preparation for the FDA Stakeholder Workshop April 25,26, 2013. Summary of preliminary results -­‐ http://www.iacfsme.org/LinkClick.aspx?fileticket=pMB2%2bjKy7EQ%3d&tabid=36. Preliminary Raw data -­‐ http://www.iacfsme.org/LinkClick.aspx?fileticket=pMB2%2bjKy7EQ%3d&tabid=36 7 “ME/CFS: A Primer for Clinical Practitioners”. Published by IACFS/ME in 2012. Page 26 gives the 25% figure. http://www.iacfsme.org/Portals/0/PDF/PrimerFinal3.pdf Jason, Chu Patient Survey in preparation for the FDA Stakeholder Workshop April 25,26, 2013. Summary of preliminary results states that up to 60% of patients are bedridden on their worst days http://www.iacfsme.org/LinkClick.aspx?fileticket=pMB2%2bjKy7EQ%3d&tabid=36. Preliminary Raw data -­‐ http://www.iacfsme.org/LinkClick.aspx?fileticket=pMB2%2bjKy7EQ%3d&tabid=36 8 Examples of severe patients are discussed further in the section on medical care. These include • Harding, L. “She went into a hellhole': A mother's candid account of her daughter's battle with ME” http://www.dailymail.co.uk/home/you/article-­‐1277519/Criona-­‐Wilson-­‐recalls-­‐daughters-­‐losing-­‐battle-­‐ME-­‐ She-­‐went-­‐hellhole.html#ixzz2pHluAz8q. Also http://www.investinme.org/article-­‐ 050%20sophia%20mirza%2001.htm • Gammel, Carol. “Lynn Gilderdale: how a 14-­‐year-­‐old was condemned to a life lived from a bed.” The Telegraph, Jan 26, 2010. http://www.telegraph.co.uk/news/uknews/law-­‐and-­‐order/7074234/Lynn-­‐Gilderdale-­‐how-­‐a-­‐14-­‐ year-­‐old-­‐was-­‐condemned-­‐to-­‐a-­‐life-­‐lived-­‐from-­‐a-­‐bed.html • ”Trapped in bed for 14 years with chronic fatigue.” Daily Mail (London). 5 July 2006. by Gill Swain, Daily Mail, 5 July 2006. http://www.dailymail.co.uk/health/article-­‐393915/Trapped-­‐bed-­‐14-­‐years-­‐chronic-­‐fatigue.html 9 Few longitudinal studies have been done and to my knowledge, none have been done on patients characterized by the Canadian Consensus Criteria. The following sources provide information on prognosis. The 5-­‐10% is for fill recovery, not just improvement in some symptoms. • ME/CFS Primer for Clinical Practitioners (2014). www.iacfsme.org/Home/Primer.aspx • Cairns R1, Hotopf M. A systematic review describing the prognosis of chronic fatigue syndrome. Occup Med (Lond). 2005 Jan;55(1):20-­‐31. http://www.ncbi.nlm.nih.gov/pubmed/15699087 10 Jason, L. Corrdai, K. Gress, S. Williams, S. Torres-­‐Harding, S. “Causes of Death Among Patients With Chronic Fatigue Syndrome.” Health Care for Women International, 27:615–626, 2006 http://www.ncf-­‐ net.org/library/CausesOfDeath.pdf Chang CM, Warren JL, Engels EA.Chronic fatigue syndrome and subsequent risk of cancer among elderly US adults. Cancer. 2012 Dec 1;118(23):5929-­‐36. doi: 10.1002/cncr.27612. http://www.ncbi.nlm.nih.gov/pubmed/22648858 Discusses increased risk of non-­‐hodgkins lymphoma 11 In 2004, Reynolds reported a 54% reduction in labor force productivity and $20,000 in lost income per patient for a total of $9.1 billion across the U.S, which translates to a total population of 455,000 patients. In 2008, using prevalence estimates of 836,000 (rate of 422 per 100,000) from the 1999 Jason prevalence study and the $20,000 per person estimate from Reynolds, Jason reported estimated lost productivity at $17B. Jason also estimated direct medical costs at $2,342 per patient in a community based sample and $8,675 per patient for patients in a tertiary setting. Using the prevalence of 836,000 patients, he estimated direct medical costs ranging from $2B to $7B and an estimated total economic impact of $18B to $24B for lost productivity and direct medical costs. These estimates of economic burden are dependent on studies of disease burden and prevalence, which are biased by the definition used and also by estimates of unemployment and average wage. For instance, these estimates were based on a rate of 422 per 100,000 that Jason estimated using Fukuda. But Nacul estimated 110 in 100,000 for the Canadian Consensus Criteria and 190 per 100,000 for Fukuda which would bias the estimates lower. On the other hand, other factors have underestimated the economic impact. For instance, today’s estimates of unemployment range from 53% to as high as 87 %, the 2011 national average wage, as reported by the Social Security Administration was $42,980 and the 2012 U.S. population estimate of 314M. The prevalence rate of 422 per 100,000 reported by Jason was based on Fukuda while Nacul showed that the Canadian Consensus Criteria had 58% of the prevalence seen for Fukuda. Accounting for these factors, it could be estimated that the prevalence of Canadian Consensus Criteria patients in the U.S. today is 769,000 people and that between 407,000 and 669,000 of them are not working. This translates into lost income of between $17B and $28B not accounting for under-­‐employment. Combined with the direct costs of $2B to $7B, this translates to an economic impact of between $19B and $35B. • Reynolds, K., Vernon, S., Bouchery, E. and Reeves, W. The economic impact of chronic fatigue syndrome. Cost Effectiveness and Resource Allocation 2004, 2:4 doi:10.1186/1478-­‐7547-­‐2-­‐4 http://www.resource-­‐ allocation.com/content/2/1/4 • Jason, L.A., Richman, J.A., Rademaker, A.W., Jordan, K.M., Plioplys, A.V., Taylor, R., et al. (1999). A community-­‐ based study of chronic fatigue syndrome. Archives of Internal Medicine. 159, 2129-­‐2137. http://www.ncbi.nlm.nih.gov/pubmed/10527290 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 42 Jason, L., Benton, M., Valentine, L., Johnson, A., Torres-­‐Harding, S. The Economic impact of ME/CFS: Individual and societal costs. Dynamic Medicine 2008, 7:6 doi:10.1186/1476-­‐5918-­‐7-­‐6 http://www.dynamic-­‐ med.com/content/7/1/6 • CFIDS estimate of unemployment in CFS patients. http://www.cfids.org/resources/newly-­‐diagnosed-­‐faq.asp 12 CFSAC recommendation, November 2011. https://wayback.archive-­‐ it.org/3919/20140324192811/http://www.hhs.gov/advcomcfs/recommendations/11092011.html “This multi-­‐part recommendation pertains to classification of CFS in ICD classification systems: a) CFSAC considers CFS to be a multi-­‐system disease and rejects any proposal to classify CFS as a psychiatric condition in the U.S. disease classification systems.” 13 Outbreaks occurred in a number of countries, including the United States, United Kingdom, Iceland, and Australia, and were referred to by a number of different disease names, including Benign Myalgic Encephalomyelitis (ME), Iceland Disease, and Akureyri Disease. In the U.S., there was an outbreak in Los Angeles in 1934. In 1986, British physician Melvin Ramsay established a definition that described the essential features of the disease that he had observed at London’s Royal Free Hospital in the 1950s and termed ME. References include • Compilation of references related to epidemics reported between 1934 and 1980. Compiled by Dr. J. Gordon Parish. http://www.meresearch.org.uk/wp-­‐content/uploads/2012/11/ResearchPublications1934-­‐1980.pdf • Compilation of pre-­‐1990 references. Includes references with links for the ME outbreaks. http://phoenixrising.me/research-­‐2/defining-­‐chronic-­‐fatigue-­‐syndrome-­‐mecfs/me-­‐research-­‐a-­‐history-­‐pt-­‐i-­‐ citations Review papers • Henderson, D., Shelokov, A. Epidemic Neuromyasthenia — Clinical Syndrome? N Engl J Med 1959; 260:757-­‐ 764April 9, 1959DOI: 10.1056/NEJM195904092601506 http://www.nejm.org/doi/full/10.1056/NEJM195904092601506 • Acheson,E.D. (1959) The clinical syndrome variously called benign myalgic encephalomyelitis, Iceland disease and epidemic neurasthaenia. JAMA, 26, 569-­‐ 595. www.name-­‐ us.org/DefintionsPages/DefinitionsArticles/Acheson1959.pdf • Dr. J. Gordon Parish. Review of Acheson’s ‘The Clinical Syndrome Variously Called Benign Myalgic Encephalomyelitis, Iceland Disease and Epidemic Neuromyasthenia’. http://www.meresearch.org.uk/information/publications/acheson-­‐review/ 14 Royal Free Hospital information sources • Acheson,E.D. (1959) The clinical syndrome variously called benign myalgic encephalomyelitis, Iceland disease and epidemic neurasthaenia. JAMA, 26, 569-­‐ 595. www.name-­‐ us.org/DefintionsPages/DefinitionsArticles/Acheson1959.pdf • Compston, N. An outbreak of encephalomyelitis in the Royal Free Hospital Group, London,in 1955. Postgraduate Miedcal Journal, November 1987. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2425309/ • Wikipedia – Royal Free Hospital -­‐ http://en.wikipedia.org/wiki/Royal_Free_Hospital 15 Jason, L., Sunnquist, M., Brown, A., Evans, M., Newton, J. Are Myalgic Encephalomyelitis and chronic fatigue syndrome different illnesses? A preliminary analysis. Journal of Health Psychology 1–13 , 2014 The word “benign” was included because it was believed that the disease did not cause death 16 Review papers • Acheson,E.D. (1959) The clinical syndrome variously called benign myalgic encephalomyelitis, Iceland disease and epidemic neurasthaenia. JAMA, 26, 569-­‐ 595. www.name-­‐ us.org/DefintionsPages/DefinitionsArticles/Acheson1959.pdf • Dr. J. Gordon Parish. Review of Acheson’s ‘The Clinical Syndrome Variously Called Benign Myalgic Encephalomyelitis, Iceland Disease and Epidemic Neuromyasthenia’. http://www.meresearch.org.uk/information/publications/acheson-­‐review/ Other papers of interest • Index of papers and epidemics of ME from 1934-­‐1980 published by Dr. Gordon Parish. http://www.meresearch.org.uk/wp-­‐content/uploads/2012/11/ResearchPublications1934-­‐1980.pdf • 1978 Postgraduate Medical Journal 1978:54:637: 709-­‐771. Whole issue. • 1979 -­‐ Clinical and biochemical findings in ten patients with benign myalgic encephalomyelitis. AM Ramsay, A Rundle. Postgraduate Medical Journal 1979:856-­‐857 17 Henderson, D., Shelokov, A. Epidemic Neuromyasthenia — Clinical Syndrome? N Engl J Med 1959; 260:757-­‐764April 9, 1959DOI: 10.1056/NEJM195904092601506 http://www.nejm.org/doi/full/10.1056/NEJM195904092601506 18 Wikipedia -­‐ http://en.wikipedia.org/wiki/History_of_chronic_fatigue_syndrome 19 Ramsay, A.M., Dowsett, E. Dadswell, J., Lyle, W., Parish, J. Icelandic disease (benign myalgic encephalomyelitis or Royal Free disease). Br Med J. May 21, 1977; 1(6072): 1350. PMCID: PMC1607215 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1607215/?page=1 • May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 43 “Last year, a research group was formed to study the etiology and epidemiologygy of this syndrome. Our investigation so far indicates that the illness may accompany the more common viral infections and that the unique fatigue pattern may be due to mitochondrial damage. As objective manifestations of the disease can still be present over 30 years after the initial illness. The most characteristic resentation is profound fatigue and musculare weakness coming on during the day and increasing in severity with exercise, a diurnal rhythm contrary to that found with other forms of depression.” 20 Epidemic myalgic encephalomyelitis. British Medical Journal 3 JUNE 1978. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1604957/ The symposium proceedings were published in The Postgraduate Medical Journal later that same year. The attendees at the symposium stated • “the cardinal clinical features show that the disorder is an encephalomyelitis; "Iceland disease" is not specific enough; and "neuromyasthenia" suggests a relation to myasthenia gravis whereas the muscle fatigability is different, as are the electrophysiological findings. Indeed, the exhaustion and tiredness are similar to that described by patients with multiple sclerosis.9 From the patient's point of view the designation benign is also misleading, since the ilness may be devastating. Originally the term was used because no deaths had been recorded from myalgic encephalomyelitis. • “Some authors have attempted to dismiss this disease as hysterical, but the evidence now makes such a tenet unacceptable.” • Also see Hooper, M. Myalgic encephalomyelitis: a review with emphasis on key findings in biomedical research. J Clin Pathol. May 2007; 60(5): 466–471. doi: 10.1136/jcp.2006.042408. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1994528/ 21 Ramsay published the following in the early 1980s, in 1986 and in 1988. Some sources indicate that Ramsay published the definition in 1981 but I have not seen the source for that. • 1986 article -­‐ Myalgic Encephalomyelitis: A Baffling Syndrome With a Tragic Aftermath. Ramsay, M., Infectious Diseases Dept, Royal Free Hospital.. Published 1986. http://www.cfids-­‐me.org/ramsay86.html • Ramsay, M. Myalgic Encephalomyelitis and Postviral Fatigue States: The Saga of Royal Free Disease, Gower Publishing Corporation, London, 2nd ed., 1988. • Also see o Ramsay AM, Rundle A. Clinical and biochemical findings in ten patients with benign myalgic encephalomyelitis. Postgrad Med J 1979; 55: 856–7. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2425703/ o Ramsay, A. M., The clinical identity of the myalgic encephalomyelitis syndrome. Published in an article by ME Association in late 1980s or early 1990s. http://web.onetel.com/~kickback/THE%20CLINICAL%20IDENTITY%20OF%20ME.html Dr. Ramsay notes the confusion that arose because of the use of the term post-­‐viral fatigue states in the 1988 publication above and reinforced the hallmark symptoms of ME, which included “A unique form of muscle fatiguability whereby, even after a minor degree of physical effort, 3,4,5 days or longer elapse before full muscle power is restored.” “Muscle Phenomena The unique form of muscle fatiguability described above is virtually a sheet-­‐anchor in the diagnosis of Myalgic Encephalomyelitis and without it a diagnosis should not be made.” 22 Arnold DL, Bore PJ, Radda GK, Styles P, Taylor DJ. Excessive intracellular acidosis of skeletal muscle on exercise in a patient with a post-­‐viral exhaustion/fatigue syndrome. A 31P nuclear magnetic resonance study. Lancet. 1984 Jun 23;1(8391):1367-­‐9. • A patient with prolonged post-­‐viral exhaustion and excessive fatigue was examined by 31P nuclear magnetic resonance. During exercise, muscles of the forearm demonstrated abnormally early intracellular acidosis for the exercise performed. This was out of proportion to the associated changes in high-­‐energy phosphates. This may represent excessive lactic acid formation resulting from a disorder of metabolic regulation. • See “Mitochondrial Dysfunction, Post-­‐Exertional Malaise and CFS/ME” developed for the MassCFIDS organization by Dr. Lucy Dechene for a summary of mitochondrial dysfunction and PEM in ME. https://www.masscfids.org/resource-­‐library/13-­‐basic-­‐information/302-­‐mitochondrial-­‐dysfunction-­‐post-­‐ exertional-­‐malaise-­‐and-­‐cfsme 23 Besides for the sources listed here, other sources of information on the Incline Village Outbreak and the Lyndonvville Outbreak are listed in the Highlighted References, especially the early articles and videos. 24 Johnson, Hilary, Osler's Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic. Crown Publishing Group, New York. 1996. Available on Amazon. 25 Chronic Fatigue Syndrome: A Modern Medical Mystery, Newsweek Magazine, November 12, 1990, http://www.thedailybeast.com/newsweek/1990/11/11/chronic-­‐fatigue-­‐syndrome.html 26 PrimeTime Live 1996 Investigation -­‐ http://www.youtube.com/watch?v=AW0x9_Q8qbo. 27PrimeTime Live 1996 Investigation -­‐ http://www.youtube.com/watch?v=AW0x9_Q8qbo. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 44 28 PrimeTime Live 1996 Investigation -­‐ http://www.youtube.com/watch?v=AW0x9_Q8qbo. Minute 3:42 -­‐ Also Johnson, Hilary, Osler’s Web : Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic". 1996, 2005. Crown Publishing Group, New York. Author’s Guild Backprint.com. Page 43 -­‐ 44 29 PrimeTime Live 1986 Investigation. http://www.youtube.com/watch?v=AW0x9_Q8qbo • According to PrimeTime Live, Hilary Johnson said “The tone behind the scenes at the CDC was one of complete and utter ridicule. Employees at the CDC would make jokes about this disease. If anyone eve said I’m tired, they would be teased about having this fake, bogus disease.”(Minute 4:48) 30 PrimeTime Live 1986 Investigation -­‐ http://www.youtube.com/watch?v=AW0x9_Q8qbo 31 PrimeTime Live 1986 Investigation – Minute 3:50 -­‐ http://www.youtube.com/watch?v=AW0x9_Q8qbo 32 May 30 1986 Mortality and Morbidity Weekly Report -­‐ http://www.cdc.gov/mmwr/preview/mmwrhtml/00000740.htm CDC also published a paper in the Journal of the American Medical Association in May of 1987 which was dismissive of the Incline Village patients -­‐ Holmes GP, Kaplan JE, Stewart JA, Hunt B, Pinsky PF, Schonberger LB. “A Cluster of Patients with a Chronic Mononucleosis-­‐like Syndrome: Is Epstein-­‐Barr Virus the Cause?” JAMA 257, not 18, May 1, 1987;2297-­‐ 302 http://www.ncbi.nlm.nih.gov/pubmed/3033337 33 PrimeTime Live 1986 Investigation. http://www.youtube.com/watch?v=AW0x9_Q8qbo • Regarding the 1986 report, Dr. Cheney said “the overall message, the tone of the paper was that this did not appear to be anything -­‐ at all”(Minute 5:05) 34 Straus, S., Dale, J., Tobi, M. Lawley, T. Preble, O. Blaese, M., Hallahan, C. , Henle, W. Acyclovir Treatment of the Chronic Fatigue Syndrome. N Engl J Med 1988; 319:1692-­‐1698 December 29, 1988 DOI: 10.1056/NEJM198812293192602 http://www.nejm.org/doi/full/10.1056/NEJM198812293192602 35 Richman, J., Jason, L., Taylor, R., Jahn, S. Feminist Perspectives On The Social Construction Of Chronic Fatigue Syndrome, Health Care for Women International, 21:3, 173-­‐185, DOI: Oct. 2000. http://dx.doi.org/10.1080/073993300245249 36 Nightline, 1987. Minute 7:20 -­‐ http://www.youtube.com/watch?v=CqpvRC_YurY&feature=player_embedded 37 Jane Brody, Health, Personal Health, 1988. Reporting on Chronic Fatigue Syndrome. NY Times. Includes quotes by Stephen Straus. -­‐ http://www.nytimes.com/1988/07/28/us/health-­‐personal-­‐health.html?src=pm&pagewanted=2 “Dr. Straus said his colleagues at the National Institutes of Health had demonstrated that many patients were psychologically ''different'' long before they developed the syndrome. He described some patients as having been anxious and depressed with various neurotic symptoms for years before becoming ill. In other cases, patients were motivated, dynamic, driven individuals who were functioning at peak levels when stricken. Some may be under an undue amount of stress trying to maintain busy lives.” 38 Straus SE, Dale JK, Wright R, Metcalfe DD. "Allergy and the Chronic Fatigue Syndrome" in the Journal of Allergy and Clinical Immunology. May 1988. • The following quote was listed on a patient blog but I have not been able to access the full article to confirm: http://www.mecfsforums.com/wiki/ME/CFS_Timeline • "The demography of this syndrome reflects an excessive risk for educated adult white women. This may reflect either a bias toward the cohort of sufferers who can best afford a sophisticated medical evaluation or some unique constitutional frailty of such individuals. Most patients with this syndrome report excellent prior health. Some had engaged in competitive sports or at least aggressively maintained physical conditioning. A less casual appraisal, however, often uncovers histories of unachievable ambition, poor coping skills, and somatic complaints…It is difficult and at times unpleasant to address the demands of such patients or to test hypotheses as to the etiology of their woes.” 39 Racaniello, V. A Tale of Two Viruses: Why AIDS Was Pinned to HIV, but Chronic Fatigue Remains a Mystery, Vincent Racaniello, January 12, 2012 http://blogs.discovermagazine.com/crux/2012/01/12/hiv-­‐in-­‐xmrv-­‐out-­‐how-­‐scientists-­‐ deduce-­‐what-­‐does-­‐and-­‐doesnt-­‐cause-­‐a-­‐disease/#.Ucx055Wyu5d Dr. Racaniello states: “In its 1988 paper on the illness, a CDC-­‐led team of researchers cast doubt on the Epstein-­‐Barr hypothesis and rechristened the phenomenon “chronic fatigue syndrome” to discourage unproven assumptions about viral origins.” 40 Holmes, G., Kaplan, J., Gantz, N., Komaroff, A., Schonberger, L., Straus, S. Jones, J., Dubois, R. Cunningham-­‐Rundles, C., Pahwa, S. Tosato, G., Zegans, L., Purtilo, D., Brown, N., Schooley, R. Brus, I. Chronic Fatigue Syndrome: A Working Case Definition. Holmes GP et.al. Annals of Internal Medicine. 1988 http://annals.org/article.aspx?articleid=701163, http://www.ncf-­‐net.org/patents/pdf/Holmes_Definition.pdf. The introduction states: “The chronic Epstein-­‐Barr virus syndrome is a poorly defined symptom complex characterized primarily by chronic or recurrent debilitating fatigue and various combinations of other symptoms, including sore throat, lymph node pain and tenderness, headache, myalgia, and arthralgias. Although the syndrome has received recent attention, and has been diagnosed in many patients, the chronic Epstein-­‐Barr virus syndrome has not been defined consistently. Despite the name of the syndrome, both the diagnostic value of Epstein-­‐Barr virus serologic tests and the proposed causal relationship between Epstein-­‐Barr virus infection and patients who have been diagnosed with the chronic Epstein-­‐Barr virus syndrome remain doubtful. We propose a new name for the chronic Epstein-­‐Barr virus syndrome—the chronic fatigue syndrome—that more accurately describes this symptom complex as a syndrome of unknown cause characterized primarily by chronic fatigue. We also present a working definition for the chronic May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 45 fatigue syndrome designed to improve the comparability and reproducibility of clinical research and epidemiologic studies, and to provide a rational basis for evaluating patients who have chronic fatigue of undetermined cause.” Note that the term CFS was first used in an article: Buchwald D, Sullivan JL, Komaroff AL. Frequency of 'chronic active Epstein-­‐Barr virus infection' in a general medical practice. JAMA. 1987 May 1;257(17):2303-­‐7. http://www.ncbi.nlm.nih.gov/pubmed/3033338 41 Jason, L., Richman, J. How Science Can Stigmatize: The Case of Chronic Fatigue Syndrome Journal of Chronic Fatigue Syndrome, Vol. 14(4),2007 http://cfids-­‐cab.org/cfs-­‐inform/CFS.case.def/jason.richman.07.txt 42 The Holmes definition was discussed at a roundtable discussion after a symposium, called the First International Symposium on the Immunobiolgy and Pathogenesis of Persistent Virus Infections held by CDC in April 1987. • This conference and the position taken by Drs. Parish and Shelokov was also discussed in: o Hyde, B. A Brief History of Myalgic Encephalomyelitis and an Irreverent History of Chronic Fatigue Syndrome. presented at the London Conference of May 12, 2006. Page 19, 22. www.imet.ie/imet_documents/BYRON_HYDE_little_red_book.pdf Dr. Hyde states that he also attended the meeting but left when Drs. Parish and Shelokov did. This article gives an extensive review of the problems with the Holmes definition o Johnson, Hilary, Osler’s Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic". 1996, 2005. Crown Publishing Group, New York. Author’s Guild Backprint.com. Page 205 o Marshall, E. Williams, M. Hooper, M. What is ME? What is CFS? Information for Clinicians and Lawyers. December 2001. http://www.investinme.org/Article-­‐020 What is ME What is CFS.htm and http://www.meactionuk.org.uk/What_Is_ME_What_Is_CFS.htm 43 Marshall, E.P. Williams, M. Hooper, M. What is ME? What is CFS? Information for Clinicians and Lawyers. December 2001. http://www.investinme.org/Article-­‐020 What is ME What is CFS.htm and http://www.meactionuk.org.uk/What_Is_ME_What_Is_CFS.htm 44 Schwartz RB, Komaroff AL, Garada BM, et al. SPECT imaging of the brain: comparison of findings in patients with chronic fatigue syndrome, AIDS dementia complex, and major unipolar depression. AJR Am J Roentgenol 1994; 162(4):943–951 http://www.ncbi.nlm.nih.gov/pubmed/8141022 • The [midcerebral Uptake Index], however, was significantly lower in patients with CFS and [AIDS Dementia Complex] than in patients with major unipolar depression on the healthy comparison group. By this objective standard, the pathophysiologic process in the CNS of patients with CFS would seem more similar to that in patients with ADC than that in patients with unipolar depression. • Although neuropathologic data in patients with CFS are unavailable, the findings in CFS are consistent with hypothesis that CFS also results from viral infection of neurons, glia, on vasculature. • In summary, this study indicates that SPECT may help in distinguishing patients with CFS from healthy subjects and depressed patients. 45 Jason, L, Torres-­‐Harding, S, Jurgens, A, Helgerson, J. “Comparing the Fukuda et al. Criteria and the Canadian Case Definition for Chronic Fatigue Syndrome, Journal of Chronic Fatigue Syndrome, Vol 12, 2004 http://www.cfids-­‐ cab.org/cfs-­‐inform/CFS.case.def/jason.etal04.pdf “However, problems emerged in doing research with this case definition, Katon et al. found that patients with CFS were indistinguishable from those with chronic fatigue who did not meet the 1988 Holmes et al. criteria (4). Another concern with the original CFS criteria was that the requirement of eight or more minor symptoms could inadvertently select for individuals with psychiatric problems.” Katon paper that as referenced is here. Katon WJ1, Buchwald DS, Simon GE, Russo JE, Mease PJ. Psychiatric illness in patients with chronic fatigue and those with rheumatoid arthritis. J Gen Intern Med. 1991 Jul-­‐Aug;6(4):277-­‐85. -­‐ http://www.ncbi.nlm.nih.gov/pubmed/1890495 46 In the early 1990s, researchers and clinicians were reporting a variety of immune abnormalities, neurological issues and evidence of viral infection. There were even reports of B-­‐ cell abnormalities at that time. (Klimas) • Williams, Margaret (from the U.K.) has compiled documentation about the early research studies. o Part 1 – 1956-­‐1990 http://www.investinme.org/Article422%20Grey%20Information%20About%20ME-­‐CFS.htm o Part 2 1991 -­‐ 1993http://www.investinme.org/Article422-­‐ 2%20Grey%20Information%20about%20ME%20CFS%20Part%20II.htm o Part 3 1994 http://www.investinme.org/Article422-­‐ 3%20Grey%20Information%20about%20ME%20CFS%20Part%20III.htm • Tuller, David. Chronic Fatigue Syndrome and the CDC: A Long, Tangled Tale, November 23, 2011. http://www.virology.ws/2011/11/23/chronic-­‐fatigue-­‐syndrome-­‐and-­‐the-­‐cdc-­‐a-­‐long-­‐tangled-­‐tale/ • Klimas NG, Salvato FR, Morgan R, Fletcher MA. Immunologic abnormalities in chronic fatigue syndrome. J Clin Microbiol. 1990 Jun;28(6):1403-­‐10. 47 Tuller, David that describes the study: Chronic Fatigue Syndrome and the CDC: A Long, Tangled Tale, November 23, 2011. http://www.virology.ws/2011/11/23/chronic-­‐fatigue-­‐syndrome-­‐and-­‐the-­‐cdc-­‐a-­‐long-­‐tangled-­‐tale/. The quotes are from the Tuller article which references the following study: Buchwald D, Cheney PR, Peterson DL, Henry B, May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 46 Wormsley SB, Geiger A, Ablashi DV, Salahuddin SZ, Saxinger C, Biddle R, et al. A chronic illness characterized by fatigue, neurologic and immunologic disorders, and active human herpesvirus type 6 infection. Ann Intern Med. 1992 Jan 15;116(2):103-­‐13. http://www.ncbi.nlm.nih.gov/pubmed/1309285 “Neurologic symptoms, MRI findings, and lymphocyte phenotyping studies suggest that the patients may have been experiencing a chronic, immunologically mediated inflammatory process of the central nervous system. The active replication of HHV-­‐6 most likely represents reactivation of latent infection, perhaps due to immunologic dysfunction. Our study did not directly address whether HHV-­‐6, a lymphotropic and gliotropic virus, plays a role in producing the symptoms or the immunologic and neurologic dysfunction seen in this illness. Whether the findings in our patients, who came from a relatively small geographic area, will be generalizable to other patients with a similar syndrome remains to be seen.” 48 Lusso, P., Ensoli, B., Markham, P., Ablashi, D., Salahuddin, S. Z., Tschachler, E. Wong-­‐Staal, F., Gallo, R. Productive dual infection of human CD4+ T lymphocytes by HIV-­‐1 and HHV-­‐6 Nature 337, 370 -­‐ 373 (26 January 1989); doi:10.1038/337370a0 http://www.nature.com/nature/journal/v337/n6205/pdf/337370a0.pdf “Although infection by HIV-­‐1 has been implicated as the primary cause of AIDS and related disorders3,4, cofactorial mechanisms may be involved in the pathogenesis of the disease. For example, several viruses commonly detected in AIDS patients and capable of transactivating the long terminal repeat of HIV-­‐1, such as herpesviruses, papovaviruses7, adenoviruses8 and HTLV-­‐I, have been suggested as potential cofactors.” “Here we demonstrate that HHV-­‐6 and HIV-­‐1 can productively co-­‐infect individual human CD4+ T lymphocytes, resulting in accelerated HIV-­‐1 expression and cellular death. We also present evidence that HHV-­‐6 transactivates the HIV-­‐1 long terminal repeat (LTR). These observations indicate that HHV-­‐6 might contribute directly or indirectly to the depletion of CD4+ T cells in AIDS.” 49 Reeves, W. Pellett, P. Gary, H. The Chronic Fatigue Syndrome Controversy http://annals.org/article.aspx?articleid=705746 As reported by • Tuller, David, Chronic Fatigue Syndrome and the CDC: A Long, Tangled Tale, November 23, 2011. http://www.virology.ws/2011/11/23/chronic-­‐fatigue-­‐syndrome-­‐and-­‐the-­‐cdc-­‐a-­‐long-­‐tangled-­‐tale/ In a letter to the journal listing more than a dozen purported methodological flaws, the CDC—with Dr. Reeves as the lead author—dismissed the Harvard study and its findings in unusually blunt terms. “We conclude that the disease…described is not the chronic fatigue syndrome or any other clinical entity and that they showed no association with active HHV-­‐6 replication,” wrote Dr. Reeves and his colleagues. Other sources that have discussed this letter include: • ME/CFS Forum – Patient advocacy forum http://www.mecfsforums.com/wiki/ME/CFS_Timeline "To the Editors: Buchwald and colleagues conclude that the chronic fatigue observed in their patients may reflect an immunologically mediated inflammatory process of the central nervous system and may be associated with human herpesvirus 6 (HHV-­‐6). The authors, however, failed to consider organic causes of chronic fatigue for analysis as a separate category and referred to neurologic symptoms without specifying diagnostic criteria. The study also lacked appropriate controls; this was not a cohort study with matched controls, as stated in the abstract, but a case series with variously selected nonmatched controls..." "We conclude that the disease Buchwald and co-­‐workers described is not chronic fatigue syndrome or any other clinical entity, and that they showed no association with active HHV-­‐6 replication." • Johnson, Hilary, Osler’s Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic". 1996, 2005. Crown Publishing Group, New York. Author’s Guild Backprint.com. Osler’s Web also discusses this study and CDC’s rejection 50 Sam Donaldson and Nancy Snyderman, Primetime report on Incline Village and Chronic Fatigue Syndrome 1996, http://www.youtube.com/watch?v=AW0x9_Q8qbo Minute 10:15 • Its worth noting that the same report interviews Dr. Phillip Lee, Assistant Secretary of Health who states that he does believe that Lake Tahoe represented a cluster of the disease and that not everyone agreed with CDC’s conclusions. Unfortunately, that did not change what CDC did. 51 CFSAC Recommendations – October 3-­‐4, 2012 Recommendation: “Allocating specific funds to study patients with ME/CFS from past cluster outbreaks” http://www.hhs.gov/advcomcfs/recommendations/10032012.html HHS response (Dr. Koh): “Studying CFS clusters or outbreaks, if they are detected, is a worthwhile project. To date, CDC has not been able to confirm the occurrence of outbreaks of CFS. Studies of potential outbreaks or clusters would greatly benefit from better understanding the different spectrums of CFS and clearly defining what constitutes an outbreak or a cluster.” http://www.hhs.gov/advcomcfs/recommendations/response-­‐from-­‐ash-­‐10-­‐2012.pdf 52 As reported by Dr. Byron Hyde, B. A Brief History of Myalgic Encephalomyelitis and an Irreverent History of Chronic Fatigue Syndrome. Presented at the London Conference, 2006. Page 12. www.imet.ie/imet_documents/BYRON_HYDE_little_red_book.pdf 53McEvedy, C., Beard, A.Royal Free Epidemic of 1955: A Reconsideration. Br Med J. 1970 January 3; 1(5687): 7–11. PMCID: PMC1700894. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1700894/ May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 47 “From a re-­‐analysis of the case notes of patients with Royal Free disease it is concluded that there is little evidence of an organic disease affecting the central nervous system and that epidemic hysteria is a much more likely explanation. The data which support this hypothesis are the high attack rate in females compared with males; the intensity of the malaise compared with the slight pyrexia; the presence of subjective features similar to those seen in a previous epidemic of hysterical overbreathing [sic]; the glove-­‐and-­‐stocking distribution of the anaesthesia [sic]; and the normal findings in special investigations.” McEvedy, C., Beard, A. Concept of Benign Myalgic Encephalomyelitis, 3rd January 1970. Br Med J. 1970 January 3; 1(5687): 11–15. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1700895/ “We believe that a lot of these epidemics were psychosocial phenomena caused by one of two mechanisms, either mass hysteria on the part of the patients or altered medical perception of the community.” Selected correspondence in response to McEvedy and Beard 54 Scott B (January 1970). “Epidemic malaise”. Br Med J 1 (5689): http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1699088/?page=1 • Compston, N., Dimsdale, H., Ramsay, A., Richardson, A. (February 1970). “Epidemic malaise”. Br Med J http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1699022/?page=1 • E. D. Acheson (February 1970). “Epidemic malaise”. Br Med J http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1698971/?page=1 • Galpine JF (February 1970). “Epidemic malaise”. Br Med J 1 (5694): 501. PMC 1699416. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1699416/?tool=pmcentrez&forumid=331851 • Poskanzer DC (May 1970). “Epidemic malaise”. Br Med J 2 (5706): 420–1. PMC 1700311. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1700311/?page=1 • Parish JG (July 1970). “Epidemic malaise”. Br Med J 3 (5713): 47–8. PMC 1700986. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1700986/?page=2 55 Abbey SE, Garfinkel PE. Neurasthenia and chronic fatigue syndrome: the role of culture in the making of a diagnosis. Am J Psychiatry. 1991 Dec;148(12):1638-­‐46. “Chronic fatigue syndrome is an increasingly popular diagnosis consisting of multiple psychiatric and somatic symptoms. It bears a striking resemblance to the nineteenth-­‐century diagnosis of neurasthenia. Both disorders arose during periods characterized by a preoccupation with commerce and material success and major changes in the role of women. They illustrate the role of culture in the development of a new diagnosis that emphasizes a "medical" rather than "psychiatric" etiology. The authors argue that chronic fatigue syndrome will meet the same fate as neurasthenia-­‐-­‐a decline in social value as it is demonstrated that the majority of its sufferers are experiencing primary psychiatric disorders or psychophysiological reactions and that the disorder is often a culturally sanctioned form of illness behavior.” Letters in response to this article can be seen here: http://ajp.psychiatryonline.org/article.aspx?articleID=169098 and here http://www.docstoc.com/docs/69274336/I-­‐Am-­‐Psychiatry-­‐December-­‐Dr-­‐Abbey-­‐and-­‐Dr-­‐-­‐neurasthenia 56 While the quotes here are from the 1980s, this is not an old view, no longer held. Here is an example of a more recent paper presenting the same approach. • Harvey, S. Wessely, S. Chronic fatigue syndrome: identifying zebras amongst the horses BMC Med. 2009; 7: 58. Published online Oct 12, 2009. doi: 10.1186/1741-­‐7015-­‐7-­‐58 PMCID: PMC2766380. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2766380/ • Maes M, Twisk F. Chronic fatigue syndrome: Harvey and Wessely's (bio)psychosocial model versus a bio(psychosocial) model based on inflammatory and oxidative and nitrosative stress pathways. BMC Med. 2010 Jun 15;8:35. doi: 10.1186/1741-­‐7015-­‐8-­‐35. http://www.ncbi.nlm.nih.gov/pubmed/20550693. 57 Wessely, S., David, A. Butler, S., Chalder, T. Management of chronic (post-­‐viral) fatigue syndrome. J R Coll Gen Pract. 1989 January; 39(318): 26–29. PMCID: PMC1711569 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1711569/ “A model is outlined of an acute illness giving way to a chronic fatigue state in which symptoms are perpetuated by a cycle of inactivity, deterioration in exercise tolerance and further symptoms. This is compounded by the depressive illness that is often part of the syndrome. The result is a self-­‐perpetuating cycle of exercise avoidance….Cognitive behavioural therapy… helps the patient understand how genuine symptoms arise from the frequent combination of physical inactivity and depression, rather than continuing infection, while a behavioural approach enables the treatment of avoidance behaviour and a gradual return to normal physical activity.” 58 One example includes the following study by Professor Wessely. Wessely, S., Powell, R. Fatigue syndromes: a comparison of chronic "postviral" fatigue with neuromuscular and affective disorders. Journal of Neurology, Neurosurgery, and Psychiatry 1989; 52:940-­‐948 http://jnnp.bmj.com/content/52/8/940. In a highly cited 1989 article by Professor Wessely, found that CFS patients more closely resembled patients with psychiatric disorders than patients with neuromuscular disorders associated with peripheral fatigue.”Peripheral fatigue neuromuscular disease included myasthenia gravis, myopathies, Guillan-­‐Barre syndrome and a variety of rare genetic or metabolic muscle disorders. Neurological disorders with central involvement, such as multiple sclerosis, were excluded.” May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 48 59 Wessely, S. (1990). Old wine in new bottles: Neurasthenia and 'me'. Psychological Medicine, 20, 35-­‐53. http://www.ncbi.nlm.nih.gov/pubmed/2181519 Richman, J. Jason, L. Gender Biases Underlying the Social Construction of Illness States: The Case of Chronic Fatigue Syndrome http://csi.sagepub.com/content/49/3/15.abstract 60 Wessely, S., David, A., Butler, S., Chalder, T. Management of chronic fatigue (post-­‐viral) syndrome. Journal of the Royal College of General Practitioners, January 1989 http://www.simonwessely.com/Downloads/Publications/CFS/4.pdf http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1371151/ “The development and persistence of chronic fatigue syndrome can be understood using a cognitive-­‐behavioral model. This is used to explain the observed progression from the avoidance of most forms of activity during the initial acute illness which is both necessary and adaptive to chronic avoidance behaviors which are maladaptive.” Wessely, S. Chronic fatigue and myalgia syndromes. In: Psychological Disorders in General Medical Settings. eds: N Sartorius et al pub: Hogrefe & Huber 1990 “Most CFS patients fulfil diagnostic criteria for psychiatric disorder. Symptoms include muscle pain and many somatic symptoms, especially cardiac, gastrointestinal and neurological. Do any of these symptoms possess diagnostic significance? The answer is basically negative. It is of interest that the ‘germ theory’ is gaining popularity at the expense of a decline in the acceptance of personal responsibility for illness. Such attribution conveys certain benefits, in other words, there is avoidance of guilt and blame. It is this author’s belief that the interactions of the attributional, behavioural and affective factors is responsible for both the initial presentation to a physician and for the poor prognosis”. Sourced from http://www.meactionuk.org.uk/select_cttee_final_version.htm 61 There is a group of doctors in England and another group in Netherlands that promote a biopsychosocial or psychosocial approach to the disease. The following two articles discuss this theory. The work of Wessely is referred to as the biopsychosocial approach where the work of Vercoulen was described by Maes as a psychosocial approach. • Harvey, S. Wessely, S. Chronic fatigue syndrome: identifying zebras amongst the horses BMC Med. 2009; 7: 58. Published online Oct 12, 2009. doi: 10.1186/1741-­‐7015-­‐7-­‐58 PMCID: PMC2766380. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2766380/ • Vercoulen JH, Swanink CM, Galama JM, Fennis JF, Jongen PJ, Hommes OR, van der Meer JW, Bleijenberg G. The persistence of fatigue in chronic fatigue syndrome and multiple sclerosis: development of a model. J Psychosom Res. 1998;45:507–517. doi: 10.1016/S0022-­‐3999(98)00023-­‐3. 62 This proposed protocol for a review of exercise in CFS contains the following description of the Biopsychosocial model for CFS. Larun L, Odgaard-­‐Jensen J, Brurberg KG, Chalder T, Dybwad M, Moss-­‐Morris RE, Sharpe M, Wallman K, Wearden A, White PD, Glasziou PP. Exercise therapy for chronic fatigue syndrome (individual patient data). Cochrane Database of Systematic Reviews 2014, Issue 4. Art. No.: CD011040. DOI: 10.1002/14651858.CD011040. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD011040/abstract “The multifactorial biopsychosocial model (Moss-­‐Morris 2012) distinguishes between precipitating and maintaining factors. Precipitating factors may include acute infective illness and/or excessive stress, while the illness is maintained by the interaction of behavior, thoughts, emotions and physiology. For example, after a severe infection or other illness, attempts to get back to normal life may result in bursts of activity punctuated by the need to rest up to recover, known as all-­‐or-­‐nothing behaviour (Moss-­‐Morris 2010; Spence 2005). These periodic bursts of activity may exacerbate symptoms and result in failure, which further reinforces sufferers’ belief that they have a serious, ongoing illness. As time goes by, efforts to meet previous standards of achievement are abandoned and patients become increasingly inactive and distressed by their ongoing symptoms. Inactivity in turn leads to physiological changes such as cardiovascular and muscular deconditioning, dysregulation of the hypothalamic-­‐ pituitary-­‐adrenal axis and disrupted circadian rhythms. In this deconditioned state, any activity is liable to produce symptoms, the experience of which reinforces the fearful beliefs and hence reinforces the avoidance of activity (fear avoidance).” 63 Regarding the biopsychosocial approach, Dr. Michael Maes pointed out that both the biopsychosocial approach as described by Professor Wessely and the similar psychosocial approach described by Dr. J. Vercoulen focused either entirely or almost entirely on psychosocial factors and ignored the existing biological evidence, particularly that for immune activation, inflammation, oxidative stress and persistent or reactivating infections and the fact that exercise intensifies the biology pathophysiology • Maes M, Twisk F. Chronic fatigue syndrome: Harvey and Wessely's (bio)psychosocial model versus a bio(psychosocial) model based on inflammatory and oxidative and nitrosative stress pathways. BMC Med. 2010 Jun 15;8:35. doi: 10.1186/1741-­‐7015-­‐8-­‐35. http://www.ncbi.nlm.nih.gov/pubmed/20550693. Dr. Maes was responding in part to this article: Harvey, S. Wessely, S. Chronic fatigue syndrome: identifying zebras amongst the horses BMC Med. 2009; 7: 58. Published online Oct 12, 2009. doi: 10.1186/1741-­‐7015-­‐7-­‐58 PMCID: PMC2766380. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2766380/ • Vercoulen JH, Swanink CM, Galama JM, Fennis JF, Jongen PJ, Hommes OR, van der Meer JW, Bleijenberg G. The persistence of fatigue in chronic fatigue syndrome and multiple sclerosis: development of a model. J Psychosom Res. 1998;45:507–517. doi: 10.1016/S0022-­‐3999(98)00023-­‐3. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 49 64 The IOM report on the definition of Gulf War Illness maed the following statement about mind-­‐body in CFS. Given that the GWI IOM was not charged with studying CFS, they were not in a position to make such a statement. Given that, one must question whether the statement was politically motivated o “Like CMI and many other symptom-­‐based illnesses, ME/CFS is not without controversy, particularly regarding whether they are mental disorders or physical health disorders (IACFSME, 2012). The committee notes that this either–or approach is not useful, for several reasons. The distinction between mental and physical disorders is often arbitrary, and most patients' experiences of any illness are influenced by biologic, psychologic, and social factors. Either–or thinking leads too often to a presumption that medically unexplained symptoms must be psychogenic. In addition, psychiatric symptoms may not be fully evaluated if a patient’ssymptoms are psychogenic. Although physical and psychologic stress can exacerbate many chronic conditions—including chronic pain, headache, respiratory, and gastrointestinal symptoms—there is an inherent risk in assuming that medically unexplained symptoms assume a “stress-­‐induced” etiology. Nearly one-­‐third of physical symptoms presenting in primary care are psychiatric or medically unexplained (Kroenke and Price, 1993). There has been a tendency to dismiss medically unexplained symptoms, but they are disabling and associated with poor quality of life (Ismail and Lewis, 2006). 65 PACE trial -­‐ Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomised trial. The Lancet -­‐ 5 March 2011 ( Vol. 377, Issue 9768, Pages 823-­‐836 ) http://www.thelancet.com/journals/lancet/article/PIIS0140-­‐6736(11)60096-­‐2/fulltext. The PACE trial, done in patients that met the Oxford definition, tested cognitive behavioral therapy (CBT) and graded exercise therapy (GET) which were used “on the basis of the fear avoidance theory of chronic fatigue syndrome” that “assume that the syndrome is perpetuated by reversible physiological changes of deconditioning and avoidance of activity.” Comments on the PACE trial outcome measures and how recovery was defined are found in a number of places including the following which lists letters to the journal on the paper -­‐ • http://www.meassociation.org.uk/2013/07/pace-­‐trial-­‐letters-­‐and-­‐reply-­‐journal-­‐of-­‐psychological-­‐medicine-­‐ august-­‐2013/ • http://www.meassociation.org.uk/2013/02/me-­‐association-­‐response-­‐to-­‐pace-­‐trial-­‐recovery-­‐paper-­‐15-­‐february-­‐ 2013/ 66 Dr. Wessely’s theory of activity avoidance is behind the large PACE trial. White, P., et al, Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomised trial. The Lancet -­‐ 5 March 2011 ( Vol. 377, Issue 9768, Pages 823-­‐836 ) http://www.thelancet.com/journals/lancet/article/PIIS0140-­‐6736(11)60096-­‐2/fulltext. The PACE trial, done in patients that met the Oxford definition, tested cognitive behavioral therapy (CBT) and graded exercise therapy (GET) which were used “on the basis of the fear avoidance theory of chronic fatigue syndrome” that “assume that the syndrome is perpetuated by reversible physiological changes of deconditioning and avoidance of activity.” The theory underlying CBT is often described as “false illness beliefs”. 67 Examples of CFS being referred to as SOmatorm illness. • Overview -­‐ Slide presentation [PDF format] Somatoform disorders – functional somatic syndromes – Bodily distress syndrome. Need for care and organisation of care in an international perspective – EACLPP Lecture, Prof. Per Fink, MD, Ph.D, Dr.Med.Sc. www.functionaldisorders.dk • Michael B. First, M.D., DSM Somatic Presentations of Mental Disorders (September 6-­‐8, 2006). American Psychiatric Association. http://www.dsm5.org/research/pages/somaticpresentationsofmentaldisorders(september6-­‐8,2006).aspx “Simon Wessely, MD (London, UK) presented on the association between the various functional somatic syndromes seen across medical specialties (e.g., irritable bowel syndrome, fibromyalgia, atypical chest pain, tension headache, etc.). Overall, unexplained medical symptoms are common in primary care settings (occurring in more than 50% of patients in one study).” 68 This article from Dr. Maes’ article includes additional explanation of the biopsychosocial model as does the PACE trial itself • Maes M, Twisk F. Chronic fatigue syndrome: Harvey and Wessely's (bio)psychosocial model versus a bio(psychosocial) model based on inflammatory and oxidative and nitrosative stress pathways. BMC Med. 2010 Jun 15;8:35. doi: 10.1186/1741-­‐7015-­‐8-­‐35. http://www.ncbi.nlm.nih.gov/pubmed/20550693. • White, P., Goldsmith, K., Johnson,A., Potts, L., Walwyn, R., DeCesare, J., Baber, H., Burgess, M., Clark, L., Cox, D., Bavinton, J., Angus, B., Murphy, G., Murphy, M., O’Dowd, H., Wilks, D., McCrone, P., Chalder, T., Sharpe, M. “Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomised trial.” The Lancet -­‐ 5 March 2011 ( Vol. 377, Issue 9768, Pages 823-­‐836 ) 1. PACE subscribes to the “fear avoidance theory of chronic fatigue syndrome” that “assume that the syndrome is perpetuated by reversible physiological changes of deconditioning and avoidance of activity.” May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 50 2. Study Publication -­‐ http://www.thelancet.com/journals/lancet/article/PIIS0140-­‐6736(11)60096-­‐ 2/fulltext 3. PACE Trial information -­‐ http://www.pacetrial.org/trialinfo/ § CBT Manual -­‐ http://www.pacetrial.org/docs/cbt-­‐therapist-­‐manual.pdf • Page 81 -­‐ “It is important to include the precipitating factors, e.g., illness, life-­‐events, working excessively hard, perfectionist personality etc. It is also important to discuss the maintaining factors, e.g., erratic or reduced activities, disturbed sleep patterns, unhelpful illness beliefs and any other unhelpful cognitions etc.” § GET Manual -­‐ http://www.pacetrial.org/docs/get-­‐therapist-­‐manual.pdf 69 Dr. Per Dalen “Somatic medicine abuses psychiatry — and neglects causal research” -­‐ http://www.art-­‐ bin.com/art/dalen_en.html 70 Yancey, J, Thomas, S. Chronic Fatigue Syndrome: Diagnosis and Treatment. American Family Physician, October 15, 2012. http://www.aafp.org/afp/2012/1015/p741.html “Patients with poor social adjustment, a strong belief in an organic cause for fatigue, or some sort of sickness benefit (i.e., financial incentive) tend to have worse responses to [cognitive behavioral] therapy.” • For patient reaction to this article see -­‐ Tony Bernhardt, Psychology Today. Another Blow to Chronic Fatigue Syndrome Sufferers, Nov 2, 2012. The misnomer “Chronic Fatigue Syndrome” once again leads to misinformation. Ms. Bernhard discusses patient concerns with the Yancey article and the position taken by the American Academy of Family Physicians. http://www.psychologytoday.com/blog/turning-­‐straw-­‐gold/201211/another-­‐blow-­‐ chronic-­‐fatigue-­‐syndrome-­‐sufferers 71 Schluederberg, A. Straus, S., Peterson, P., Blumenthal, S., Komaroff, A., Spring, S., Landay, A., Buchwald, D. Chronic Fatigue Syndrome Research Definition and Medical Outcome Assessment. Annals of Internal Medicine. August 1992. Abstract -­‐ http://annals.org/article.aspx?articleid=705740 Full text -­‐ http://annals.org/data/Journals/AIM/19757/AIME199208150-­‐00010.pdf “One recommended modification was that patients with certain psychiatric disorders be included regardless of the time of symptom onset, provided that they otherwise meet the case definition (see Table 1). The working definition had been made deliberately restrictive to reduce heterogeneity among cases under study (8); however, it now seems prudent to make the definition less exclusionary. To ensure that studies are replicable and interpretable, such cases must be carefully delineated and their data handled separately in analyses. Study of well-­‐characterized subgroups will foster an integrative approach that gives consideration to issues relating to comorbidity and possible common pathogenic pathways in patients with CFS and psychic stress. Such an approach should lead to a better understanding of factors underlying CFS (9)” Other key points • The report noted considerable discussion on how to best include psychiatric patients and on “techniques for quantifying and qualifying the degree of psychiatric suffering.” • Regarding medical testing, the report stated, “A main point of consensus was that no currently existing laboratory tests can be used to confirm the diagnosis of CFS. It was also agreed that, for clinical purposes, diagnostic testing in patients with suspected CFS should be done solely to exclude other diagnoses. An economical but comprehensive battery of laboratory tests, specified in Table 1, should be sufficient for this purpose when used in conjunction with a carefully ob-­‐ tained patient medical history and physical examination.” • This bullet makes the case that these psychiatric cases are included in the definition but separated for analysis. But in practice, most of the scientific papers I have seen treat them as a single group and do not stratify patients. o “The following disorders are included in the case definition but are identified clearly for separate analysis: major depressive episodes (not including those with psychotic features), panic disorder (with or without ag-­‐ oraphobia), generalized anxiety disorder, and somatoform disorder. These psychiatric disorders should be further distinguished by the timing of the onset of the disorder (for example, one discrete and self-­‐limited ep-­‐ isode well before the onset of chronic fatigue; chronic and recurring episodes well before the onset of chronic fatigue; active at the time of onset of chronic fatigue; clearly beginning after the onset of chronic fatigue) and by the response (if any) of the disorder to therapy (that is, does the psychiatric disorder improve, and do the chronic fatigue and associated somatic symptoms im-­‐ prove?).” • Acknowledged contributors included Susan E. Abbey, MD; Michael A. Caligiuri, MD; Chun C. Chao, PhD; Paul R. Cheney, PhD, MD; Patricia K. Coyle, MD; Mark A. Demitrack, MD; Robert Fekety, MD; Don L. Goldenberg, MD; Walter Gunn, PhD; Wayne J. Katon, MD; Andrew R. Lloyd, MB BS; Nicole Lurie, PhD; Peter Manu, MD; Anita Stewart, PhD; Warren Strober, Robert J. Suhadolnik, PhD; and Simon Wessely, MRC Psych. According to the text, the participants were involved in the creation of Holmes, Oxford or the Australian definition. 72 NIH has held a number of conferences on CFS. As far as I can tell, These include May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 51 1985 First NIH conference on CFS Held by NIAID Second NIH Conference on CFS -­‐ March 1991 Held by NIAID. And National Institute of Mental Health Feb 2000 Internal Science Consultation Held by NIAID Key issue, as reported in the report for the second conference was “In 1985 at the first NIAID workshop, it was agreed that the greatest obstacle to CFS research was the lack of an objective case definition.” Purpose was to review the collective experience of investigators in the United States who have been using the CDC criteria for case definition in their research and, if necessary, to make recommendations concerning further modification and 2) to discuss approaches to assessment of illness severity for studies of natural history and intervention. -­‐ Report http://annals.org/article.aspx?articleid=705740. -­‐ Held in response to CFSCC recommendation but planned without CFSAC input -­‐ Purpose to improve the quality, direction and extent of CFS research supported by NIH -­‐ Attendees -­‐ Originally planned to only include Simon Wessely, Michael Sharpe, Mark Demitrack and Stephen Straus. The revised meeting was attended by group of 11 people, including Gail Cassell (chair), Margaret Chesney, Mark Demitrack, Charles Engel, Helen Mayberg, Kevin McCully, William Reeves, Joan Shaver, Michael Sharpe, Simon Wessely, Stephen Straus, Lon White, Barry Wilson, Nancy Klimas. Patient Kathy Rabin. It is unclear who of these individuals were given the opportunity to speak and who wrote the final report. -­‐ Produced report and led to 2001 AHRQ evidence based review noted elsewhere -­‐ Report -­‐ http://webharvest.gov/peth04/20041027092632/www.niaid.nih.gov/dmid/meetings/cfsreport.h tm -­‐ CAA report -­‐ http://www.co-­‐cure.org/infoact2.htm, http://www.cfids.org/archives/2000/2000-­‐ 1-­‐article02.asp -­‐ Purpose -­‐ focus on CFS research areas in which information is both mature and exciting; summarize current knowledge and identify important gaps in knowledge; garner the perspective of expert investigators not currently working on the problem of CFS; and identify expert investigators who might be attracted to study CFS as a clinical problem. -­‐ Topics -­‐ neuroendocrinology; cognition; chronic pain; sleep; immunology; orthostatic intolerance/neurally mediated hypotension; and fatigue, functional status, and disability. -­‐ Sponsorship – according to the report, this was organized by the CFSCC with financial support from CDC and NIH -­‐ report -­‐ www.co-­‐cure.org/SOS.pdf . Issued by CFSCC -­‐ CAA Summary -­‐ http://www.cfids.org/archives/2000/2000-­‐2-­‐dcd.asp -­‐ Craig Maupin summary -­‐ http://www.cfidsreport.com/Articles/NIH/NIH_CFS_2.htm October 2000 State of the Science workshop Organized by CFSCC, not NIH as the other conferences in this list were. June 12-­‐13 -­‐ Report has a focus on stress and allostatic load. 2003 -­‐ Sponsored by NIH Office on Women’s Health and Trans-­‐NIH Working Group on Research on CFS Neuroimmun Report -­‐ e Mechanisms https://web.archive.org/web/20060930202459/http://orwh.od.nih.gov/pubs/cfs_june03report.p and chronic df fatigue syndrome held by NIH April 2011 Report -­‐ orwh.od.nih.gov/research/me-­‐cfs/pdfs/ORWH_SKW_Report.pdf NIH State of Knowledge Conference held by Trans-­‐NIH Working Group May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 52 73 Straus, Stephen. Defining the Chronic Fatigue Syndrome. Editorial. Arch Intern Med, August 1992. http://archinte.jamanetwork.com/article.aspx?articleid=616488 “A workship convened jointly last year in Bethesda, Md, by the National Institute of Allergy and Infectious Diseases and the National Institute of Mental Health and organized to review the status of the CDC case definition in research, ascertained that most investigators, including those conducting the ongoing CDC prevalence study of chronic fatigue syndrome in four US cities, accept a concurrent diagnosis of depression or anxiety disorder. Still others accept such problems when they predate chronic fatigue but were not active when the fatigue itself began. Until prospectively acquired data reveal whether either of these is a reasonable strategy, the suggestion made was that investigators document psychiatric problems and stratify for them in data analysis.” 74 JACOBSON, D. Science / Medicine : Chronic Fatigue Debate Still Going Strong : Research: Thousands who suffer from the syndrome, and their doctors, claim it's caused by a virus. But researchers say the syndrome is rare, if it exists at all, and psychological. The Hartford Courant. Dec 35, 1989. http://articles.latimes.com/1989-­‐12-­‐25/local/me-­‐ 751_1_chronic-­‐fatigue-­‐syndrome “…the University of Connecticut researchers [which included Dr. Manu], say people with CFS symptoms start with a history of recurrent mental illness, including depression, panic attacks and other disorders. Their physical symptoms then emerge from patients' unspoken "psycho-­‐emotional conflicts." 75 Hyde B M, Goldstein J, Levine P. The clinical and scientific basis of myalgic encephalomyelitis/chronic fatigue syndrome. Ottawa: Nightingale Research Foundation, 1992. 76 A Summary of Chronic Fatigue Syndrome and Its Classification in the International Classification of Diseases. Prepared by the Centers for Disease Control and Prevention, National Center for Health Statistics, Office of the Center Director, Data Policy and Standards March 2001 http://www.co-­‐cure.org/ICD_code.pdf 77 A Summary of Chronic Fatigue Syndrome and Its Classification in the International Classification of Diseases. Prepared by the Centers for Disease Control and Prevention, National Center for Health Statistics, Office of the Center Director, Data Policy and Standards March 2001 http://www.co-­‐cure.org/ICD_code.pdf “WHO published ICD-­‐10 in 1992 and included many modifications, among them relocation of some diagnoses to different chapters within the classification. WHO created a new category G93, Other disorders of brain, in Chapter VI, Diseases of the Nervous System, and created a new code G93.3, Postviral fatigue syndrome, a condition which was previously in the symptom chapter of ICD-­‐9. WHO also moved benign myalgic encephalomyelitis to the new code G93.3. The alphabetic index contains other terms, such as chronic fatigue syndrome, that WHO considers synonymous or clinically similar.” Note that the ICD-­‐10 has a tabular listing that lays out the primary categories and terms of ICD. It also has an alphabetical index which indexes additional terms back to the terms of the tabular index. ME is in the tabular index at G93.3 and CFS is in the alphabetical index at G93.3 78 Straus, S., Komaroff, S., Wedner, H.J. Chronic Fatigue Syndrome: Point and Counterpoint. The Journal of Infectious Diseases. Vol 170, July 1994 http://www.jstor.org/stable/30133467 Reporting on the 1993 annual meeting of the Infectious Disease Society of America. In 1993, Dr. Stephen Straus mediated a discussion at the annual meeting of the Infectious Disease Society of America. One of the speakers, Dr. H. James Wedner, Professor of Immunology and Allergy at Washington University and a clinician who had treated CFS patients, made the following statements: “…There has been a creeping movement to include other types of medical conditions under the rubric of CFS. For example, various forms of post-­‐infectious fatigue, fibromyalgia, and non-­‐psychiatric and depressive disorders were permitted by consensus of a National Institutes of Health (NIH) workshop. Somatoform disorders and panic disorder became part of what could be encompassed within the CFS case definition. This serves to broaden the scope of the clinical entity to the point at which it is no longer definable. 79 Lloyd A,Hickie I,Boughton R,Spencer,O. Wakefield D.Prevalence of chronic fatigue syndrome in an Australian population. Med JAust. 1990;153:522-­‐528. 80 Sharpe M, Archard L, Banatvala J., Borysiewicz, L., Clare, A., David, A., Edwards, R., Hawton, K., Lambert, H., Lane, R., McDonald, E., Mowbray, J., Pearson, D., Peto, T., Preedy, V., Smith, A., Smith, D., Taylor, D., Tyrrell, A., Wessely, S., White, P. A report—chronic fatigue syndrome. J Roy Soc Med 1991; 84: 118-­‐121. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1293107/ The criteria for Oxford CFS are: 1. A syndrome characterized by fatigue as the principal symptom 2. A syndrome of definite onset that is not life long 3. The fatigue is severe, disabling and affects physical and mental functioning the symptom of fatigue should have been present for a minimum of 6 months during which it was present for more than 50% of the time 4. Other symptoms may be present, particularly myalgia, mood and sleep disturbance Fatigue is described as follows: “When used to describe a symptom this is a subjective sensation and has a number of synonyms including, tiredness and weariness. A clear description of the relationship of fatigue to activity is preferred to the term fatiguability…The symptom of fatigue should not be confused with impairment of performance as measured by physiological or psychological testing. The physiological definition of fatigue is of a failure to sustain muscle force May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 53 or power output. 81 Fukuda K, et al Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med 1994;121:953-­‐9. http://www.ncf-­‐net.org/patents/pdf/Fukuda_Definition.pdf 82 Jason discusses the impact of how a disease is conceptualized. Jason, L., Richman, J., Friedberg, F., Wagner, L., Taylor, R., Jordan, K. Politics science and the emergence of a new disease. September 1997, American Psychologist. Vol. 52, No. 9, 973-­‐983 http://www.ncbi.nlm.nih.gov/pubmed/9301342 83 M. Sharpe was one of the authors and Professor Simon Wessely was on the International Chronic Fatigue Study Group, which included authors of the Oxford, Holmes and I believe the Australian definition. 84 The Fukuda definition lists the following psychiatric exclusions: Any past or current diagnosis of a major depressive disorder with psychotic or melancholic features; bipolar affective disorders; schizophrenia of any subtype; delu-­‐ sional disorders of any subtype; dementias of any subtype; anorexia nervosa; or bulimia nervosa. Other psychiatric disorders are not listed. 85 Jason, L., Richman, J., Friedberg, F., Wagner, L., Taylor, R., Jordan, K. Politics science and the emergence of a new disease. September 1997, American Psychologist. Vol. 52, No. 9, 973-­‐983 http://www.ncbi.nlm.nih.gov/pubmed/9301342 86 Jason, L. “Defining CFS: Diagnostic Criteria and Case Definition”. CFIDS association webinar, April 2010. www.cfids.org/webinar/jason-­‐slides041410.pdf slide 10, 12. Jason’s presentation discusses the fact that Fukuda does not require core symptoms and that depressed patients can have fatigue plus 4 of the Fukuda symptoms -­‐ unrefreshing sleep, joint pain, muscle pain and impairment in concentration. Oxford is even broader than Fukuda and specifically allows the inclusion of psychiatric patients. 87 Komaroff AL, Cho TA. Role of infection and neurologic dysfunction in chronic fatigue syndrome. Semin Neurol. Epub 2011 Sep 30 http://www.ncbi.nlm.nih.gov/pubmed/21964849 Examples include • Multiple studies have demonstrated hypofunction of corticotropin-­‐releasing (CRH) neurons in the hypothalamus, and hypocortisolism (distinct from Addison dis-­‐ ease). This downregulation of the hypothalamic– pituitary–adrenal (HPA) axis in CFS stands in contrast to the upregulation seen in major depression. • Neuropsychological testing of cognition has revealed abnormalities in patients with CFS, abnormalities not explained by a coexisting depression. 88 Fukuda K, et al Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med 1994;121:953-­‐9. http://www.ncf-­‐net.org/patents/pdf/Fukuda_Definition.pdf • “The complexities of the chronic fatigue syndrome and the methodologic problems associated with its study indicate the need for a comprehensive, systematic, and integrated approach to the evaluation, classification, and study of persons with this condition and other fatiguing illnesses. We propose a conceptual framework and a set of guidelines that provide such an approach. Our guidelines include recommendations for the clinical evaluation of fatigued persons, a revised case definition of the chronic fatigue syndrome, and a strategy for subgrouping fatigued persons in formal investigations.” • “We propose a conceptual framework (Figure 1) to guide the development of studies relevant to the chronic fatigue syndrome. In this framework, in which the chronic fatigue syndrome is considered a subset of prolonged fatigue (>1 month), epidemiologic studies of populations defined by prolonged or chronic fatigue can be used to search for illness patterns consistent with the chronic fatigue syndrome. Such studies, which differ from case-­‐ control and cohort studies based on predetermined criteria for the chronic fatigue syndrome, will also produce much-­‐needed clinical and laboratory background information.” 89 Fukuda K, et al Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med 1994;121:953-­‐9. http://www.ncf-­‐net.org/patents/pdf/Fukuda_Definition.pdf • “In formal studies, cases of the chronic fatigue syndrome and idiopathic chronic fatigue should be subgrouped be-­‐ fore analysis or stratified during analysis by the presence or absence of essential variables, which should be rou-­‐ tinely established in all studies.” 90 Wessely S, Chalder T, Hirsch S, Wallace P, Wright D (1997). The prevalence and morbidity of chronic fatigue and chronic fatigue syndrome: a prospective primary care study. Am J Public Health. 87: 1449–1455. Multiple criteria were used. Oxford prevalence reported as 2.2% http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1380968/ 91 Harvey, S. Wessely, S. Chronic fatigue syndrome: identifying zebras amongst the horses BMC Med. 2009; 7: 58. Published online Oct 12, 2009. doi: 10.1186/1741-­‐7015-­‐7-­‐58 PMCID: PMC2766380. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2766380/ “Thus, current recommendations advising a range of simple investigations (Appendix) for those with persistent fatigue seem well placed. Jones et al. did find some 'zebras' but, as expected, these were relatively rare. A simple mental state examination appears to remain the most productive single investigation in any new person presenting with unexplained fatigue.” 92 Examples include May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 54 Nijs J, Roussel N, Van Oosterwijck J, De Kooning M, Ickmans K, Struyf F, Meeus M, Lundberg M. Fear of movement and avoidance behaviour toward physical activity in chronic-­‐fatigue syndrome and fibromyalgia: state of the art and implications for clinical practice. Clin Rheumatol. 2013 May 3. http://www.ncbi.nlm.nih.gov/pubmed/23639990 • Pariante, C. In his 2012 review of “Should Myalgic Encephalomyelitis and chronic fatigue syndrome (ME/cfs) be regarded as prolonged sickness behavior?”, Pariante states “For many, including this reviewer, CFS/ME is predominantly a condition triggered by excessive rest in predisposed individuals following acute triggers, and its interpretation requite a psychosocial and psychiatric framework.” http://www.biomedcentral.com/1741-­‐ 7015/11/64/prepub • Over the years, a number of authors have characterized chronic fatigue syndrome as a classic example of a somatic/somatoform disorder. One example is the following 2013 presentation on the Royal College. http://www.rcpsych.ac.uk/pdf/C%20Feinmann%20Slides.pdf. 93 Jason, L., Najar, N., Porter, N., Reh, C. Evaluating the Centers for Disease Control’s Empirical Chronic Fatigue Syndrome Case Definition. Journal of Disability Policy Studies Oct 2008, http://www.co-­‐cure.org/Jason-­‐7.pdf • The comments here were made relative to the Empirical definition but are general to the comments that Dr. Jason has made about how the approaches used to assess cases of “CFS” could increase the percentage of “CFS” patients that had psychiatric illness or other conditions while failing to require that patients had the hallmark criteria of ME such as PEM. He also raised the concern that these assessment approaches and criteria might lead to the conclusion that only “distress and unwellness characterize CFS, thus inappropriately supporting a unitary hypothetical construct called ‘functional somatic syndrome’.” Collectively, these factors would result in more patients, including more patients with primary psychiatric illness, being diagnosed as having “CFS” and also result in CFS itself being equated to psychiatric illness. 94 Letter from Dr. Stephen Straus at NIH to Dr. Keiji Fukuda at CDC. The letter, which is undated, was written about the time of the publication of Fukuda in 1994. The letter was obtained by Craig Maupin of CFIDSReport.com by FIOA and released in March of 2014. FOIA Number No.38767, presumably from NIH https://dl.dropboxusercontent.com/u/89158245/Straus%20to%20Fukuda%20letter%201994.docx Further information is available on Craig Maupin’s site. http://www.cfidsreport.com/News/14_Chronic_Fatigue_Syndrome_Definition_IOM_Straus.html 95 1996 report of the Joint Working Group of the Royal Colleges of Physicians, Psychiatrists and General Practitioners on Chronic Fatigue Syndrome. www.theoneclickgroup.co.uk/documents/ME-­‐CFS_docs/Royal Colleges Report-­‐CFS.doc, http://books.google.com/books/about/Chronic_Fatigue_Syndrome.html?id=RRId4npKxDsC 96 Lancet, Editors of the Lancet, Frustrating Survey of Chronic Fatigue, Vol. 348, issue 9033, p. 971, October 12 1996, doi:10.1016/S0140-­‐6736(05)64917-­‐3. http://www.thelancet.com/journals/lancet/article/PIIS0140-­‐ 6736%2805%2964917-­‐3/fulltext “Psychiatry has won the day for now. A decade hence, when an organic cause for at least some cases of CFS may have emerged, it would be tempting to ask the committee to reconvene. We believe that the report was haphazardly set-­‐up, biased, and inconclusive, and is of little help to patients or their physicians. Or as the Department of Health weakly put it, the report will “provide a further contribution to the ongoing debate”. Incidentally, the Department still talks about CFS/ME. 97 Stephen Straus, NIH National Institute of Allergy and Infectious Diseases, Editorial, Chronic fatigue syndrome. Biopsychosocial approach may be difficult in practice. BMJ October 1996; 313:831 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2359057/pdf/bmj00562-­‐0007.pdf 98 Dr. Phillip Lee, Assistant Secretary of Health. Acceptance Speech, Rudy Perpich Award. 1998 Bi-­‐Annual Research Conference of the American Association for Chronic Fatigue Syndrome. http://www.cfids-­‐me.org/mpwc/lee.html His comments include the following • Chronic Fatigue Syndrome, Wedner tells us, is neither a disease nor a syndrome. It is a committee definition. • “The approach to CFS is now dominated by the biopsychosocial approach that gives excessive emphasis to the social, behavioral, and emotional factors in the presentation and perpetuation of symptoms. The "bio" seems to be missing. While I believe in the psychosocial determinants of health paradigm, this approach to CFS has gone too far. “ • “The problem is evidence in the proposed ICD-­‐9 codes for CFS, and the 1996 report of the Joint Working Group of the Royal Colleges of Physicians, Psychiatrists and General Practitioners on Chronic Fatigue Syndrome in the United Kingdom. The Royal Colleges convened a working group after a request from the UK's Chief Medical Officer. The group recommended that the term encephalomyelitis be dropped in the UK and that it be replaced by CFS.” • Third, the current approaches to CFS, except in a few hands, do not take sufficient cognizance of the research on brain positron emission tomography, cognitive function, possible biomarkers, electron microscopy, the evidence from past outbreaks, or a number of the studies presented here. • Finally, the overlap of symptoms with Gulf War Syndrome, fibromyalgia, and multiple chemical sensitivities merit a thorough re-­‐examination and the development of a comprehensive strategic plan for research. • May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 55 • “Dr. Stephen Straus of the NIH had a very different view and one that I strongly disagree with.” 99 National Institutes of Health. Chronic Fatigue Syndrome State-­‐of-­‐the-­‐Science Consultation. February 6-­‐7, 2000. http://webharvest.gov/peth04/20041027092632/www.niaid.nih.gov/dmid/meetings/cfsreport.htm Following an uproar from the community, NIH modified the meeting to include 11 people, including Gail Cassell (chair), Margaret Chesney, Mark Demitrack, Charles Engel, Helen Mayberg, Kevin McCully, William Reeves, Joan Shaver, Michael Sharpe, Simon Wessely, Stephen Straus, Lon White, Barry Wilson, Nancy Klimas. Patient Kathy Rabin. It is unclear who of these individuals were given the opportunity to speak and who wrote the final report. This meeting generated considerable controversy in the community. A few of the contemporary sources include: • CFIDS Association report on discussion with NIH prior to the meeting -­‐ http://www.co-­‐ cure.org/infoact2.htm, http://www.cfids.org/archives/2000/2000-­‐1-­‐article02.asp • CFIDS Association report post meeting -­‐ http://www.cfids.org/archives/2000/2000-­‐1-­‐article02.asp • Report by advocate Mary Schweitzer -­‐ http://www.cfids-­‐me.org/marys/nihprobs.html • Summary of events -­‐ After two months of requests by Kim Kenney (McCleary) of the CFIDS Association, Dr. David Morens, the CFS Program Officer at NIH finally stated “the purpose of this conference was to help guide NIH's CFS research priorities” and there were four attendees -­‐ Professor Simon Wessely, Professor Michael Sharpe, Dr. Mark Demitrack and Dr. Stephen Straus. The first three were psychiatrists and Wessely, Sharpe and Straus had promoted or endorsed the biopsychosocial view of this disease. Dr. Morens further said that CFSCC had not been involved in planning the conference even though CFSCC had recommended the meeting. As a result of vocal patient opposition, Dr. Klimas, Dr. Komaroff and Dr. Rowe, members of CFSCC were invited to attend at short notice. Dr. Komaroff was not able to attend. Seven others also attended but the others were reported to not be expert in this disease. The resultant report discounted the importance of infectious agents. The report noted a higher prevalence of depression, generalized anxiety disorder, and panic in CFS and that the majority of CFS patients may have diagnosable psychiatric illnesses. It discussed chronic life stresses and the need to distinguish between predisposing, precipitating and perpetuating factors. Finally, the report stated “beliefs about illness should be explored as an aspect of CFS” and stated that CBT had been successfully used. 100 Chronic Fatigue Syndrome. State of the Science Conference Oct 22-­‐23, 2000. Published by the HHS CFS Coordinating Committee http://www.co-­‐cure.org/SOS.pdf “The goals of the meeting were to focus on CFS research areas in which information is both mature and exciting; summarize current knowledge and identify important gaps in knowledge; garner the perspective of expert investigators not currently working on the problem of CFS; and identify expert investigators who might be attracted to study CFS as a clinical problem.” “Seven topic areas of medical research were identified: neuroendocrinology; cognition; chronic pain; sleep; immunology; orthostatic intolerance/neurally mediated hypotension; and fatigue, functional status, and disability. For each topic, a clinical scientist studying CFS (CFS expert) was asked to present the most provocative aspects of current knowledge; then scientists working in that same research area, but not studying CFS (subject experts), were asked to provide additional information and insights from that discipline that could enhance understanding of CFS.” Its worth noting that psychiatric issues were not discussed except to discount their importance as an explanation for cognitive issues. Rather than psychiatric issues and dysregulation of thought and belief, the October 2000 report found that a majority had viral-­‐like illnesses preceding the onset of CFS and discussed dysregulation of biological control systems. Rather looking for clues in mood disorders, this report discussed the potential relevance of multiple sclerosis research 101 National Institutes of Health. Chronic Fatigue Syndrome State-­‐of-­‐the-­‐Science Consultation. February 6-­‐7, 2000. http://webharvest.gov/peth04/20041027092632/www.niaid.nih.gov/dmid/meetings/cfsreport.htm The report language echoed the later focus on chronic unwellness and on a broader case definition based on empirical analysis of populations. This was played out in the Empirical definition (see below). • “It is important to distinguish between the research case definition that is intended to help design research studies and the identification of individual patients at the community and clinical level. The case definition was developed by physicians who see patients and by the characteristics of those patients who are seen by physicians. They are therefore likely to be highly selected and unrepresentative of the true spectrum of illness.” • “Empirical case definitions using information from people in population surveys may be derived from factor analysis, e.g., data from persons studied in population surveys. Factor analysis may be a useful exploratory tool for further refining the case definition.” • “It is a cardinal premise of epidemiology that case-­‐control studies should enroll incident cases. With CFS this is difficult to do, as many patients have already had the disease for quite a while and are from tertiary medical care. In any event, the case definition requires at least six months of fatigue.” • “In persons with chronic unwellness, there seem to be two categories of predominant symptom patterns that can be broadly classified as cognitive and inflammatory (although there is no definitive evidence of inflammation).” May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 56 Yet remarkably, the report also states that requiring fatigue first may be approaching the issue backwards but then goes on to compare CFS to PTSD and burnout. The report also calls out the importance of subgrouping, something that doesn’t appear to have been done. • “Fatigue and sleep disorders may be the result of the two predominant symptom patterns, cognitive and inflammatory. Thus, requiring fatigue first could be approaching the issue backwards.” • “Stress reactions and immune regulation are more sensitive in women than in men. Women's physiology is more cyclical in nature. These factors need to be taken into account in study design.” • “The idea of a chronic stress activation pattern may be worthy of pursuit. There is much evidence for a stress component to CFS. Additionally, a range of conditions associated with stress or trauma has been related to hypocortisol. Thus, there is considerable symptom overlap in PTSD, nurses and "burnout," teachers who report living under chronic stress, CFS, FMS, and idiopathic chronic pain.” • “Predisposing factors, precipitating factors, and perpetuating factors need to be distinguished and studied. Understanding perpetuating factors and factors predicting recovery are important issues. Iatrogenic factors, such as medical treatment, involved in perpetuation or recovery need also to be considered.” • “Research and clinical experience suggests a higher prevalence in CFS of depression, generalized anxiety disorder, and panic disorders than in other ill groups.” 102 2000 GAO report on CFS. Key findings included lack of coordination, inadequate communication, CDC misuse of funds • GAO report, June, 2000. http://www.gao.gov/products/HEHS-­‐00-­‐98 • http://www.gao.gov/new.items/he00098.pdf • Reuters. GAO Critiilizes CDC, NIH Handling of Chronic Fatigue Research. 2000. http://www.ncf-­‐ net.org/library/GAOCriticizesCDC.htm • CFIDS Association -­‐ http://www.cfids.org/advocacy/cdc-­‐scandal.asp 103 July 2006 CFSAC discussion with Dr. Hanna. http://www.hhs.gov/advcomcfs/meetings/minutes/cfsac060717_min.html 104 As reported in other parts of this paper, Dr. Straus has made numerous statements about his views of this disease. This statement is one that he made in 2001, about the same time this decision was made. Dreifus, C. A CONVERSATION WITH: STEPHEN STRAUS; Separating Remedies From Snake Oil. April 2001 http://www.nytimes.com/2001/04/03/health/a-­‐conversation-­‐with-­‐stephen-­‐straus-­‐separating-­‐remedies-­‐from-­‐snake-­‐ oil.html?pagewanted=all&src=pm Dr. Straus stated that many people get over CFS. He added that individuals who have it for years lose hope and “They then take on a series of maladaptive behaviors which sustain their illness because they become so focused and so phobic: they avoid exercise, disrupt their sleep patterns. It gets harder and harder for them to regain normalcy." 105 Insight into another potential driver behind this change comes from an interview between patient advocate Craig Maupin and HHS’ Donna Dean. Dr. Donna Dean reportedly stated that the responsibility she had been given was “the function of trying to straighten out, as much as I could, the mess that the NIH had gotten into with CFS (and the mess that DHHS had gotten into).” She further added “It was important to get the NIH CFS program leadership somewhere where people were focusing on scientific kinds of issues, on a scientific approach to medical conditions, without the encumbrances and biases of the past.” Craig Maupin. “The CFS program at the NIH – Past, present, and future” September, 2005. http://www.cfidsreport.com/Articles/NIH/NIH_CFS_2.htm I have not been able to find another source for this information. 106 CDC held three closed meetings/working groups between 2000 and 2002 to discuss the issues with Fukuda and its usage. These included • May 2000 meeting -­‐ http://www.cdc.gov/cfs/meetings/case_def_05_2000.html o “Participants at the first workshop (May 2000) agreed that the 1994 International CFS Research Case Definition was not optimal, that it should be revised, and that future revisions should be based on empirically derived data (if possible from defined populations). Three groups were formed to discuss the following issues: how a case definition should be used for research; how population groups should be identified for studies and how classification instruments should be standardized.” • May 2001 meeting -­‐ http://www.cdc.gov/cfs/meetings/case_def_05_2001.html o “The second meeting (June 2001) focused on ambiguities of the 1994 case definition and on what instruments would provide the best objective measures of the major dimensions of CFS. We agreed to prepare a review article critiquing the 1994 case definition. We also agreed that CDC would take the lead in facilitating communication about the CFS case definition and in forming an International Collaborative Group to test standard instruments and collect data that could be used to propose an empiric data-­‐based revision to the case definition.” • May 2002 meeting -­‐ http://www.cdc.gov/cfs/meetings/case_def_05_2002.html o “The overall objective of the third meeting was to maintain the momentum of the International Collaborative Group and continue the work to more precisely define CFS. The specific aim was to discuss how standard instruments measuring the major symptom domains of CFS could be used May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 57 internationally in clinical research settings. During the meeting, three working groups sought to develop strategies” to a) uniformly apply standardized instruments, b) optimally measure fatigue and other symptoms and psychiatric comorbidity and c) identify procedures to identify “symptom dimensions among persons with CFS and other unexplained chronically fatiguing illnesses.” CDC’s conclusions on the May 2002 meeting link conveyed their overwhelming focus on chronic fatigue – they planned a study to “identify symptom dimensions among persons with unexplained chronic fatigue; determine the variability of symptom dimensions across the sites; measure the associations between symptom dimensions and other health constructs; and determine the feasibility of conducting an international multicenter study of unexplained chronic fatigue.” 107 Reeves, W., Lloyd, A., Vernon, S., Klimas, N., Jason, L., Bleijenberg, G., Evengard, B., White, P. Nisenbaum, R., Unger, E. and the International Chronic Fatigue Syndrome Study Group. Identification of ambiguities in the 1994 chronic fatigue syndrome research case definition and recommendations for resolution BMC Health Services Research 2003, 3:25 http://www.biomedcentral.com/1472-­‐6963/3/25 Other information • The International Chronic Fatigue Research Group members included: Susan Abbey (University of Toronto, Toronto, Canada), Catherine Campbell (Centers for Disease Control and Prevention, Atlanta, GA), Dedra Buchwald (University of Washington, Seattle, WA), Anthony Cleare (Institute of Psychiatry, Guy's, King's, and St. Thomas School of Medicine, London, UK), Nelson Gantz (Pinnacle Health System, Harrisburg, PA), Ron Glaser (Ohio State University, Columbus, OH), Christine Heim (Emory University, Atlanta, GA), Ian Hickie (University of New South Wales, Sydney, Australia), Gail Ironson University of Miami, Miami, FL), Ann-­‐Britt Jones (Centers for Disease Control and Prevention, Atlanta, GA), James Jones (National Jewish Medical Center, Denver, CO), Kevin Karem (Centers for Disease Control and Prevention, Atlanta, GA), K. Kimberly Kenney (CFIDS Association of America, Charlotte, NC), Hirohiko Kuratsune (Osaka University, Osaka, Japan), Gudrun Lange (New Jersey Medical School, Newark, NJ), Kathleen McCormick (SRA, Rockville, MD), Andrew Miller (Emory University, Atlanta, GA), Harvey Moldofsky (Centre for Sleep and Chronobiology, Toronto, Canada), Benjamin Natelson (New Jersey Medical School, East Orange, NJ), Thomas J. O'Laughlin (Physical Medicine, Rehabilitation & Electromyography, Fresno, CA), Dimitris A. Papanicolaou (Emory University, Atlanta, GA), Mangalathu Rajeevan (Centers for Disease Control and Prevention, Atlanta, GA), John Stewart (Centers for Disease Control and Prevention, Atlanta, GA), Eng Tan (Scripps Institute), Vicki Walker (CFIDS Association of America, Charlotte, NC). • The recommended instruments included (1) the Medical Outcomes Survey Short Form-­‐36 (SF-­‐36), to measure functional impairment; (2) a comprehensive instrument, such as the Checklist Individual Strength (CIS) or the Multidimensional Fatigue Inventory (MFI), to obtain reproducible quantifiable measures of fatigue,; and (3) the CDC Symptom Inventory to document the occurrence, duration and severity of the symptom complex Note: The recommendations for instruments included the use of the Composite International Diagnostic Instrument to assess psychiatric illness. The Structured Clinical Interview for DSM-­‐IV Axis 1 was suggested as an alternative but the report states that this requires trained individuals to administer the test. The report acknowledges that these two tools produce different results but states that the differences should be handled by stating clearly which instrument was used and discussing the resultant issues. 108 Reeves, W., Wagner, D., Nisenbaum, R., Jones, J., Gurbaxani, B., Solomon, L., Papanicolaou, D., Unger, E., Vernon, S., Heim, C. Chronic Fatigue Syndrome – A clinically empirical approach to its definition and study. BMC Medicine 2005, 3:19 http://www.biomedcentral.com/1741-­‐7015/3/19. • The Empirical definition was based on the feedback the above series of CDC workshops between 2000 to 2002 to identify issues with the Fukuda definition and then on a December 2002 to July 2003 study conducted by the CDC to empirically establish the definition. The 2002 study included patients that had been previously identified in the CDC’s Witchita CFS Surveillance study • The 2005 report states that when the case definition used in the Witchita surveillance study to “classify subjects when they entered this clinical study only 16 had a current classification of CFS, 76 of ISF, 48 were not fatigued controls, and remission was identified in 24 recruited as CFS/ISF who no longer reported fatigue. Most (87%) of the 46 subjects enrolled because they were considered CFS during surveillance did not meet the same case definition criteria at the time of the clinical study: most (58.7%) were classified as ISF and 10.9% were in remission.” 109 Reeves, W., Wagner, D., Nisenbaum, R., Jones, J., Gurbaxani, B., Solomon, L., Papanicolaou, D., Unger, E., Vernon, S., Heim, C. Chronic Fatigue Syndrome – A clinically empirical approach to its definition and study. BMC Medicine 2005, 3:19 http://www.biomedcentral.com/1741-­‐7015/3/19. • “This study showed scant stability of CFS over time, when diagnosed by the usual algorithm (based on patients' subjective responses to direct questions as to whether they feel fatigued, if they perceive their fatigue causes substantial reduction in daily activities, and whether at least 4 case defining symptoms are present). There was poor correlation between illness classification during surveillance (recruitment classification) and classification by the same criteria during the clinical study. While this might reflect fluctuation in illness over time, illness categories May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 58 (CFS, ISF, Remission, non-­‐fatigued) defined by this surveillance classification scheme were not consistent with respect to overall illness severity.” 110 Jason, L., Richman, J. How Science Can Stigmatize: The Case of Chronic Fatigue Syndrome Journal of Chronic Fatigue Syndrome, Vol. 14(4),2007 http://cfids-­‐cab.org/cfs-­‐inform/CFS.case.def/jason.richman.07.txt “Clearly, this newly developed empirical system diagnoses additional people with CFS. It is very possible that this new empirical classification does identify a group of individuals with high levels of fatigue, impairment, and symptoms, but it might also be identifying a group with high chronic distress and illness, rather than CFS as a unique disorder.” 111 Reeves, W. C., Jones, J. J., Maloney, E., Heim, C., Hoaglin, D. C., Boneva, R., et al. (2007). New study on the prevalence of CFS in metro, urban and rural Georgia populations. Population Health Metrics, 5, Article 5. Available from http://www.pophealthmetrics.com/content/5/1/5 This paper reports a prevalence rate of 0.0254 versus 0.0024 in the 2003 Reyes study (Prevalence and incidence of chronic fatigue syndrome in Wichita, Kansas). 112 White PD How common is chronic fatigue syndrome; how long is a piece of string? Population Health Metrics 5:6, 2007. http://www.pophealthmetrics.com/content/5/1/6 113 Jones, J., Lin, J., Maloney, E., Boneva, R., Nater, U., Unger, E., Reeves, W. An evaluation of exclusionary medical/psychiatric conditions in the definition of chronic fatigue syndrome. BMC Med. 2009; 7: 57. Published online Oct 12, 2009. doi: 10.1186/1741-­‐7015-­‐7-­‐57 PMCID: PMC2768736 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2768736/ This article looks at the health status of patients that meet Empirical criteria and those who would meet it except for exclusionary diagnoses. The conclusion is that those who fail to meet CFS criteria because of exclusionary conditions also need care. “As those with CFS suffer from personal, social, workplace and observed financial losses, should not all individuals fulfilling CFS inclusion criteria, with or without exclusionary diagnoses, be considered in future public health planning? For instance, would both groups benefit from prevention and intervention efforts such as cognitive behavioral therapy and graded exercise therapy? A similar question could be asked of those who are unwell but who do not reach the diagnostic threshold.” 114 Aslakson E, Vollmer-­‐Conna U, Reeves WC, White PD. "Replication of an Empirical Approach to Delineate the Heterogeneity of Chronic Unexplained Fatigue" Population Health Metrics. October 2009, 7:17 doi:10.1186/1478-­‐ 7954-­‐7-­‐17 http://www.pophealthmetrics.com/content/7/1/17 o “The broadening of the concept of CFS to include patients with fewer symptoms but similar disability is supported by this replication.” o "Conclusion: These data support the hypothesis that chronic medically unexplained fatigue is heterogeneous. The data do not support the current perception that CFS represents a unique homogeneous disease and suggests broader criteria may be more explanatory. o “What are the clinical implications of this work?... Future research studies should now examine for moderators of outcome that include obesity, metabolic syndrome, sleep problems, depression, and having multiple symptoms.” Note that the study reported that these were the factors associated with CFS. 115 Jason, L., Richman, J. How Science Can Stigmatize: The Case of Chronic Fatigue Syndrome Journal of Chronic Fatigue Syndrome, Vol. 14(4),2007 http://cfids-­‐cab.org/cfs-­‐inform/CFS.case.def/jason.richman.07.txt for comments on a number of these studies. 116 Reported by Jason in: Jason, L., Richman, J. How Science Can Stigmatize: The Case of Chronic Fatigue Syndrome Journal of Chronic Fatigue Syndrome, Vol. 14(4),2007 http://cfids-­‐cab.org/cfs-­‐inform/CFS.case.def/jason.richman.07.txt 117 Reported by Jason in: Jason, L., Richman, J. How Science Can Stigmatize: The Case of Chronic Fatigue Syndrome Journal of Chronic Fatigue Syndrome, Vol. 14(4),2007 http://cfids-­‐cab.org/cfs-­‐inform/CFS.case.def/jason.richman.07.txt “Gurbaxani, Jones, Goertzel, and Maloney (2006) found that the depression score was the most effective variable discriminating between CFS cases and controls, whereas 20 biological variables only achieved classification accuracy slightly better than chance.” The study that he is referring to is: Gurbaxani, B. M., Jones, J. F., Goertzel, B., & Maloney, E.M. (2006). Linear data mining the Wichita clinical matrix suggests sleep and allostatic load involvement in chronic fatigue syndrome. Pharmacogenomics, 7(3), 455465. 118 Press release “Results of the study confirm that childhood trauma, particularly emotional maltreatment and sexual abuse, is associated with a six-­‐fold increased risk for CFS.” Emory University, January 7, 2009 http://shared.web.emory.edu/emory/news/releases/2009/01/childhood-­‐trauma-­‐chronic-­‐fatigue-­‐syndrome-­‐risk-­‐ linked.html#.UscXy_aE4YQ Study being reported: Heim C, Nater UM, Maloney E, Boneva R, Jones JF, Reeves WC. "Childhood Trauma and Risk for Chronic Fatigue Syndrome" January 2009 Archives of General Psychiatry. http://archpsyc.ama-­‐assn.org/cgi/content/full/66/1/72 119 Nater UM, Jones JF, Lina JS, Maloneya E, Reeves WC, Heim C. "Personality Features and Personality Disorders in Chronic Fatigue Syndrome: A Population-­‐Based Study" in Psychotherapy and Psychosomatics. July 2010 "Our results suggest that CFS is associated with an increased prevalence of maladaptive personality features and personality disorders. This might be associated with being noncompliant with treatment suggestions, displaying unhealthy behavioral strategies and lacking a stable social environment. Since maladaptive personality is not specific to CFS, it might be associated with illness per se rather than with a specific condition." May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 59 http://content.karger.com/ProdukteDB/produkte.asp?Aktion=ShowAbstract&ArtikelNr=319312&Ausgabe=254424& ProduktNr=223864 120 CDC authors published a study on maladaptive coping styles in CFS in 2012 that was used the empirical definition. Reference: Nater, U., Maloneya, E., Linb, J., Heimc, C., Reeves, W. “Coping Styles in Chronic Fatigue Syndrome: Findings from a Population-­‐Based Study”. Psychother Psychosom 2012;81:127–129. • Publication: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3701445/ • News release: http://www.alphagalileo.org/ViewItem.aspx?ItemId=121978&CultureCode=en 121 Professor Emeritus Hooper makes this point in Magical Medicine Page 43 www.investinme.org/Documents/Library/magical-­‐medicine.pdf 122 Jason, L., Najar, N., Porter, N., Reh, C. Evaluating the Centers for Disease Control’s Empirical Chronic Fatigue Syndrome Case Definition. Journal of Disability Policy Studies Oct 2008, http://www.co-­‐cure.org/Jason-­‐7.pdf “In conclusion, this study suggests that the Reeves et al. (2005) empirical case definition has broadened the criteria such that some individuals with a purely psychiatric ill-­‐ ness will be inappropriately diagnosed as having CFS. The Reeves et al. empirical case definition used specific instruments (such as the Medical Outcomes Survey Short-­‐ Form-­‐36) to make diagnostic decisions but included dimensions within them such as role emotional functioning that were not specific for this illness…assessment and criteria that fail to capture the unique characteristics of these illnesses might inaccurately conclude that only distress and unwellness characterize CFS, thus inappropriately supporting a unitary hypothetical construct called “functional somatic syndrome.” Additional useful information can be found at: • Jason, L., Richman, J. How Science Can Stigmatize: The Case of Chronic Fatigue Syndrome Journal of Chronic Fatigue Syndrome, Vol. 14(4),2007 http://cfids-­‐cab.org/cfs-­‐inform/CFS.case.def/jason.richman.07.txt “The issues that he called out were a) how patients were screened (not just fatigue but also pain, concentration, unrefreshing sleep) which accounted for a 13% increase b) the use of the standardized criteria of the Empirical definition – this resulted in 3 times as many cases c) a symptom severity and frequency scoring mechanism that led to a diagnosis even if just 2 symptoms, one moderate and one severe at the same time d) symptoms only had to be experienced for the last month, not the past 6 as specified in Fukuda e) patients diagnosed as CFS even if they only had role emotional score on SF-­‐36 at a level that almost all clinically depressed patients would meet. If patients were not diagnosed based on the role emotional factor alone, many of the depressed patients would not be diagnosed as having CFS. The Medical Outcomes SF-­‐36 is an instrument that assesses functional health and well being 123 Taylor RR, Jason LA. Sexual abuse, physical abuse, chronic fatigue, and chronic fatigue syndrome: a community-­‐based study. J Nerv Ment Dis. 2001 Oct;189(10):709-­‐15. http://www.ncbi.nlm.nih.gov/pubmed/11708672 124 Taylor RR, Jason LA. Chronic fatigue, abuse-­‐related traumatization, and psychiatric disorders in a community-­‐based sample. Soc Sci Med. 2002 Jul;55(2):247-­‐56. http://www.ncbi.nlm.nih.gov/pubmed/12144139 • “These findings suggest that a history of abuse, particularly during childhood, may play a role in the development and perpetuation of a wide range of disorders involving chronic fatigue. Among individuals with chronic fatigue, PTSD and other anxiety disorders appear to demonstrate the strongest association with abuse history. The implications of these findings are discussed.” 125 One example -­‐ CDC CME “Diagnosis and Management of Chronic Fatigue Syndrome” http://www.cdc.gov/cfs/education/diagnosis/index.html Page 1-­‐9. Page 5, which describes the Fukuda definition includes reference to the recommendations to add standardized measures to the case definition in 2003. These recommendations are related to the Empirical definition. 126 This was done by the PACE trial as noted above and also in the following report on CFS prevalence studies which reported the 2005 prevalence study as a Fukuda study. Brurberg, K., Fønhus, A., Larun, L., Flottorp, S., Malterud, K. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): a systematic review. BMJ Open 2014;4:e003973 doi:10.1136/bmjopen-­‐2013-­‐003973 http://bmjopen.bmj.com/content/4/2/e003973.long#T1 127 The higher prevalence estimate of 4 million resulted from an Empirical definition study. This estimate is listed on various HHS websites and is often quoted in medical education material from a variety of secondary sources. One HHS website is: Voice of the Patient Report from the FDA Patient Focused Drug Development Initiative Meeting in April 2013. http://www.fda.gov/downloads/ForIndustry/UserFees/PrescriptionDrugUserFee/UCM368806.pdf At the FDA Advisory Committee meeting for Ampligen, this upper limit of 4 million was mentioned in the context of determining what size safety studies were needed 128 Regarding Dr. Unger’s statement on the Empirical definition. In a November 9, 2011 CFSAC meeting minutes exchange between Dr. Jason and Dr. Unger. Dr. Jason asked about the continued publication of Empirical study results (the 2005 Empirical definition has been discredited) and how the CDC intended to evolve the criteria? Dr. Unger’s response that they had done a study comparing “the standardized approach to applying the Fukuda definition [Empirical definition] and the approach that we had used in the past in the Wichita studies. Everyone will find it very reassuring that the patient populations are quite comparable.” A study was to have been published in early 2012 but so far that study does not appear to be available. http://www.hhs.gov/advcomcfs/meetings/minutes/cfsac_min-­‐11092011.pdf -­‐ page 24 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 60 129 NICE guidelines -­‐ http://guidance.nice.org.uk/CG53 Comments by Invest In ME on NICE guidelines -­‐ http://www.investinme.org/iime%20campaigning-­‐nice-­‐ guidelines%20iime%20response.htm • Comments by Dr. an Gibson on NICE guidelines -­‐ http://www.investinme.org/Article-­‐ 301%20Ian%20Gibson%20NICE%20Guideline%20Witness%20Statement.htm “NICE claims that both CBT and graded exercise therapy are supported by an adequate evidence base, however, the GDG relied on a very small number of controversial randomised control trials (RCTs). The patient selection criteria for participating in the trials were too wide and therefore allowed non-­‐ME/CFS suffers to participate. It is also misleading to refer to CBT & GET as `treatments' of `choice'. They cannot properly be described as treatments, since, as NICE admits, they do not address the core pathology of ME.” “That NICE did not adequately take into account the general international biomedical evidence base was highlighted by the GSRME committee of senior parliamentarians I chaired in 2005-­‐6 who were concerned with both the psychiatric dominance in the current UK ME research programmes and patient selection criteria they use. I am therefore disappointed that the NICE GDG did not adopt or endorse high quality internationally recognised patient selection and diagnostic criteria such as the Canadian Criteria even though the latter were mentioned in the Guideline.” “The NICE GDG also failed to endorse the World Health Organisation definition of ME/CFS as a neurological disorder despite the fact the Department of Health and Government Ministers have repeatedly confirmed that they do agree with this classification. I do not believe that the NICE CFS/ME Guidelines are fit for purpose.” 130 NICE guidelines Appendix A, which includes the Evidence Based Review used in NICE: Bagnall, A., Hempel, S., Chambers, D., Orton, V., Forbes, C. The diagnosis, treatment and management of chronic fatigue syndrome (CFS) / myalgic encephalomyelitis (ME) in adults and children. Centre for Reviews and Dissemination University of York. October 2005. www.nice.org.uk/nicemedia/live/11630/34188/34188.pdf 131 NICE guidelines static list including comments from stakeholders on the decision to place a disease on the static list. http://www.nice.org.uk/guidance/cg/published/ListStaticClinicalGuidelines.jsp 132 Dowsett EG, Goudsmit E, Macintyre A, Shepherd CB. Report from The National Task Force on Chronic Fatigue Syndrome (CFS), Post Viral Fatigue Syndrome (PVFS), Myalgic Encephalomyelitis (ME). Westcare, 1994. pp. 96-­‐98. http://www.meassociation.org.uk/2011/02/london-­‐criteria-­‐for-­‐m-­‐e/ • “The London Criteria was produced at a time when clinicians, researchers and scientific journals were becoming increasingly reluctant to use the term ME in a research context – preferring the term CFS instead. Consequently, there was very little research into ME taking place. The London Criteria, which were designed for research purposes, are based on Dr Melvin Ramsay’s clinical description of ME as can be found on pages 30 – 31 of the second edition of his book Postviral fatigue syndrome – The saga of Royal Free disease (re-­‐published by and available from The ME Association). Dr Ramsay was not involved in the process to develop the London Criteria because he died in 1990. • The London Criteria was published in 1994 in the Task Force Report and was subsequently made use of in a small number of research studies – the most important one being the research carried out by Costa et al which demonstrated brain stem hypoperfusion. (ref: Costa D et al. Brainstem perfusion is impaired in patients with myalgic encephalomyelitis/chronic fatigue syndrome. Quarterly Journal of Medicine, 1995, 88, 767 – 773.” 133 Carruthers, B., et al Jain, A., De Meirleir, K., Peterson, D., Klimas, N., Lerner, M., Bested, A., Flor-­‐Henry, P., Joshi, P., Powles, A. , Sherkey, J., van de Sande, M. Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols. Journal of Chronic Fatigue Syndrome, Vol. 11(1) 2003 Page 18. http://mefmaction.com/images/stories/Medical/ME-­‐CFS-­‐Consensus-­‐Document.pdf • The 2003 Canadian Consensus Criteria for ME/CFS was developed by an expert consensus panel at the request of Health Canada and with the intent of developing a clinical definition that addressed the pathogenesis of the disease and provided diagnostic and treatment protocols. • In marked contrast to the definitions discussed above, the CCC was the first definition since Ramsay’s 1988 definition to put the focus on post-­‐exertional fatigability and the other characteristic immune, neurological, and endocrine abnormalities by which ME experts identify patients. In recognition of the fact that U.S. patients frequently refer to ME as “CFS,” while patients abroad largely refer to the disease as ME, the CCC used the label “ME/CFS.” While a logical decision, the use of “ME/CFS,” “CFS/ME,” “CFS,” and even chronic fatigue “CF” as alternative names for ME has ultimately compounded confusion about the nature of the disease produced by the use of overbroad and overlapping case definitions, because people are using the same terms and meaning very different things. 134 Nacul, L., Lacerda, E., Pheby, D., Campion, P., Molokhia, M., Fayyaz, S., Leite, J., Poland, F., Howe, A., Drachler, M. Prevalence of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) in three regions of England: a repeated cross-­‐sectional study in primary care. BMC Medicine 2011, 9:91 doi:10.1186/1741-­‐7015-­‐9-­‐91. http://www.biomedcentral.com/1741-­‐7015/9/91 135 Chronic fatigue syndrome/myalgic encephalomyelitis. A primer for clinical practitioners. International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (IACFS/ME). Chicago (IL): International Association for • May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 61 Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (IACFS/ME); 2012. 41 p. [121 references] http://www.guideline.gov/content.aspx?id=38316 Also see 2014 version, released in May 2014 -­‐ http://www.iacfsme.org/Home/Primer.aspx 136 Harvey, S. Wessely, S. Chronic fatigue syndrome: identifying zebras amongst the horses BMC Med. 2009; 7: 58. Published online Oct 12, 2009. doi: 10.1186/1741-­‐7015-­‐7-­‐58 PMCID: PMC2766380. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2766380/ 137 Jason L, Jordan K, Miike T, Bell DS, Lapp C, Torres-­‐Harding S., Rowe, K., Gurwitt, A., DeMeirleir, K., Van Hoof, E. A Pediatric Case Definition for Myalgic Encephalomyelitis and Chronic Fatigue Syndrome. J Chronic Fatigue Syndr. 2006 13: 1-­‐44 http://www.cfids-­‐cab.org/MESA/Jason-­‐1a.pdf 138 Carruthers, B., van de Sande, M., De Meirleir, K., Klimas, K., Broderick, G., Mitchell, T., Staines, D., Powles, A., Speight, N., Vallings, R., Bateman, L., Baumgarten-­‐Austrheim, B., Bell, D., Carlo-­‐Stella, N., Chia, J., Darragh, A., Jo, D., Lewis, D., Light. A., Marshall-­‐Gradisbik, S., Mena, I., Mikovits, J., Miwa, K., Murovska, M., Pall, M., Stevens, S. Myalgic encephalomyelitis: International Consensus Criteria. Journal of Internal Medicine. Volume 270, Issue 4, pages 327–338, October 2011. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-­‐2796.2011.02428.x/full • To address what they described as a “web of confusion” created by the overly broad CFS definitions and the mixing and matching of names, twenty-­‐six researchers and clinicians from thirteen countries published the Myalgic Encephalomyelitis International Consensus Criteria (ME-­‐ICC) in 2011. Although it used the CCC as a starting point, requiring post-­‐exertional neuroimmune exhaustion and symptoms reflecting neurological, immunological/gastrointestinal/genitourinary, and energy production/transportation impairments, the ME-­‐ICC did not include the CCC definition’s requirement that doctors wait six months before diagnosing the disease. Significantly, the ME-­‐ICC called for patients meeting the ME-­‐ICC criteria to be removed from the NICE criteria and the Reeves Empirical criteria. Further, the companion ME International Consensus Primer for Medical Practitioners, published in 2012, called for patients meeting the ME-­‐ICC criteria to be removed from the broader CFS or CFS/ME criteria, including the Oxford, Reeves (Empirical), Fukuda, and CCC case definitions. • The requirement for 6 months prior to diagnosis is not required in other diseases and was dropped in this definition. 139 The ME-­‐ICC, referenced in the last footnote, describes the difference between fatigue and fatigability as follows “Fatigue in other conditions is usually proportional to effort or duration with a quick recovery and will recur to the same extent with the same effort or duration that same or next day. The pathological low threshold of fatigability of ME de-­‐ scribed in the following criteria often occurs with minimal physical or mental exertion and with reduced ability to undertake the same activity within the same or several days.” 140 Myalgic Encephalomyelitis: International Consensus Criteria for Medical Practitioners published by the International Consensus Criteria that developed the ME-­‐ICC sacfs.asn.au/download/me_international_consensus_primer_for_medical_practitioners.pdf 141 Scottish Public Health Network -­‐ Health Care Needs Assessment of Services for people living with ME/CFS http://www.scotphn.net/pdf/Final_report_web_version_271110.pdf Page 36 states that NICE is used for CFS and CCC for ME. This statement was not seen in the following document. Also found here -­‐ http://www.scotphn.net/projects/previous_projects/care_needs_for_those_experiencing_me_cfs www.show.scot.nhs.uk/App_Shared/docs/MainDoc.pdf also states that CCC is used for ME. • “The Scottish Parliament Cross Party Group on M.E. is also strongly supportive of the Canadian Consensus Document definition. It has been adopted for general use in Australia and New Zealand. The Gibson Inquiry (2006) recently reviewed diagnostic criteria and concluded that the Canadian Consensus Document definition was a useful contribution to defining the clinical condition of ME-­‐ CFS. Reflecting the lack of accord, the Scottish Public Health Care Network’s Health Care Needs Assessment of Services for people living with ME-­‐CFS, has recommended the ‘pragmatic use’ of the Canadian Consensus Document for the clinical, symptomatic definition of ME.” 142 Unity of Opposites? Chronic fatigue syndrome and the challenge of divergent perspectives in guideline development” J Neurol Neurosurg Psychiatry 2014;85:214-­‐219 doi:10.1136/jnnp-­‐2012-­‐303208. First published online Nov 17, 2012 http://jnnp.bmj.com/content/85/2/214.full, http://jnnp.bmj.com/content/early/2012/11/16/jnnp-­‐2012-­‐303208.abstract 143 Euromut is a Belgian Health Insurance company. It recommends the use of the CCC for diagnosis of patients http://www.euromut.be/cs/ContentServer?packedargs=typeSubAsset2%3DM509_Article&c=M509_Dossier&childpa gename=Mut509%2FLayout&p=1239006699187&pagename=Mut509_Wrapper&cid=1255618087871 All translations by Google Translate • “CFS is a complex disease in which the immune system is disturbed and that above all characterized by a disproportionate increase in complaints by a small effort. This occurs in 100% of the patients, and is the hallmark of CFS.” • http://www.euromut.be/ContentServer/particulier/Dossiers/dossier.syndrome-­‐de-­‐fatigue-­‐chronique-­‐SFC-­‐ fr/article.sfc-­‐les-­‐causes o “The biopsychosocial model: In the search for causes of disease, the biopsychosocial model is oriented towards the biological, psychological and social. The origin is sought in the patient's personality and May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 62 vulnerability factors such as stress , depression , biological factors and personality characteristics. Nowadays , this assumption is increasingly challenged, as it offers no explanation for the physical pain. Unlike the biopsychosocial model, the discussion within the biomedical model shows visible irregularities and anomalies. More than 400 scientific studies provide evidence of biomedical nature of the disease . CFS usually occurs after a viral infection or a severe weakening of the immune system as a result of physical or emotional overload . CFS is often related to different viruses and different bacterial infections. This results in a chain reaction of physical abnormalities , which explain the typical symptoms of CFS.” • http://www.euromut.be/ContentServer/particulier/Dossiers/dossier.syndrome-­‐de-­‐fatigue-­‐chronique-­‐SFC-­‐ fr/article.sfc-­‐le-­‐diagnostic o “A correct diagnosis of CFS is benefited by the handling of the Canadian criteria , with post-­‐exertional malaise is a mandatory criterion.” o “Tests as diagnostic aids: For a correct diagnosis, a blood test is an asset. Regular blood tests generally do not reveal much, unlike specialized targeted tests. Respiratory and blood tests are tracking intolerances to foods. A stress test or a bike , preferably a double test test clearly demonstrates the unique feature of exercise intolerance . Most CFS patients get abnormal neurological examination . A SPECT scan shows reduced irrigation in the brain , the tilt test shows orthostatic intolerance. Neuropsychological tests are an overview of problems with memory and concentration.” 144 Public Health Agency of Canada -­‐ http://www.phac-­‐aspc.gc.ca/cd-­‐mc/az-­‐index-­‐eng.php 145 Norwegian Health Directorate draft guidelines were issued in 2012 that recommended ME-­‐ICC for ME and Fukuda for CFS. • Consultation document -­‐ http://www.helsedirektoratet.no/Om/hoyringar/Documents/cfs-­‐ me/horingsutkast.pdf • Reaction to Norwegian Health Directorate guidelines by the Norwegian Society of General Practice http://translate.googleusercontent.com/translate_c?depth=1&hl=en&rurl=translate.google.com&sl=no&tl=en&t wu=1&u=http://legeforeningen.no/Fagmed/Norsk-­‐forening-­‐for-­‐allmennmedisin/Horingsuttalelser/Horing-­‐-­‐ utkast-­‐til-­‐rundskriv-­‐om-­‐CFSME-­‐/&usg=ALkJrhhCx_dx7bilY_tG5JDBputAC0F5Zg • Nov 17, 2012 Norwegian ME Story conveying GPs reaction: http://translate.google.com/translate?hl=en&sl=no&tl=en&u=http%3A%2F%2Fme-­‐ foreningen.com%2Fmeforeningen%2F%3Fp%3D4450 • Health Directorate Site -­‐ http://www.helsedirektoratet.no/helse-­‐og-­‐omsorgstjenester/cfs-­‐ me/Sider/default.aspx 146 National Plan -­‐ Patients with CFS / ME: Assessment, diagnosis, treatment, rehabilitation and care, Directorate of Health. http://www.helsedirektoratet.no/publikasjoner/pasienter-­‐med-­‐cfsme-­‐utredning-­‐diagnostikk-­‐behandling-­‐ pleie-­‐og-­‐omsorg/Sider/default.aspx 147 The Rituxin story and the Norwegian apology: Story -­‐ http://debortgjemte.com/2012/06/07/the-­‐drug/ Apology -­‐ http://www.euro-­‐me.org/news-­‐Q42011-­‐003.htm Apology in Norwegian. http://www.tv2.no/nyheter/innenriks/helsedirektoratet-­‐vi-­‐har-­‐ikke-­‐gode-­‐nok-­‐helsetjenester-­‐for-­‐mesyke-­‐ 3618296.html 148 Bernhard, Toni. “The Stigma of Chronic Fatigue Syndrome”. Psychology Today. April 10, 2011. http://www.psychologytoday.com/blog/turning-­‐straw-­‐gold/201104/the-­‐stigma-­‐chronic-­‐fatigue-­‐syndrome 149 Craig Maupin. The NIH and CFS: The CFS Community’s Concerns http://www.cfidsreport.com/Articles/NIH/NIH_CFS_4.htm 150 Jason, L., Richman, J. How Science Can Stigmatize: The Case of Chronic Fatigue Syndrome Journal of Chronic Fatigue Syndrome, Vol. 14(4),2007 http://cfids-­‐cab.org/cfs-­‐inform/CFS.case.def/jason.richman.07.txt He performed two studies, one in medical trainees and the other in college undergraduates to assess perception based on the name. 151 Dec 2003 response by CFSAC to the Name Change recommendation http://www.cfids.org/advocacy/cfsac-­‐ statement.asp Sept 2003 CFSAC Meeting minutes -­‐ http://www.hhs.gov/advcomcfs/meetings/minutes/csfac_mins_2003.09.29r_pdf.pdf 152 ME is rarely if ever given as a diagnosis according to participants at a 2011 National Center for Health Statistics ICD meeting (http://www.cdc.gov/nchs/icd/icd9cm_maintenance.htm) 153 The ICD-­‐10 has a tabular listing that lays out the primary categories and terms of ICD. It also has an alphabetical index which indexes additional terms back to the terms of the tabular index. ME is in the tabular index at G93.3 and CFS is in the alphabetical index at G93.3 154 Background sources include • CFIDS report on the 2000 CFS Coordinating Committee, http://www.cfids.org/archives/2000/2000-­‐1-­‐ article02.asp "The Centers for Disease Control and Prevention (CDC) announced that in 2002 the U.S. diagnostic code for CFS will be moved from "General symptoms-­‐Malaise and fatigue" (780.71) [the code in ICD-­‐9-­‐CM] to "Other disorders of the brain" (G93.], which is the code the World Health Organization (WHO) established in ICD-­‐10 in 1992 for CFS, post-­‐viral fatigue syndrome and benign myalgic encephalomyelitis. In 1998 the U.S. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 63 created a separate code (distinct from the WHO code) for CFS. Dr. Klimas, Kim [McCleary] and I [Vicky Walker] worked closely with the National Center for Health Statistics over the past 18 months to provide scientific evidence supporting our position that the U.S. should adopt the WHO designation, providing worldwide consistency in CFS classification and a more scientifically appropriate code for CFS. Hopefully this coding change will have a positive impact on insurance reimbursement and validation of CFS." • A Summary of Chronic Fatigue Syndrome and Its Classification in the International Classification of Diseases. Prepared by the Centers for Disease Control and Prevention, National Center for Health Statistics, Office of the Center Director, Data Policy and Standards March 2001 http://www.co-­‐cure.org/ICD_code.pdf “In keeping with the placement in the ICD-­‐10, chronic fatigue syndrome (and its synonymous terms) will remain at G93.3 in ICD-­‐10-­‐CM.” 155 The current version of the ICD-­‐10-­‐CM, which is intended to be rolled out in October, 2015 can be found here ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Publications/ICD10CM/2014/ 156 Placing CFS in the Symptoms chapter does not align with WHO standards and goes against recommendations by CFSAC, a recommendation by the International Association of CFS/ME and two formal requests by patient advocates to have CFS put back into the neurological chapter. The U.S. will categorize “CFS” as a subcategory of chronic fatigue when it rolls out the ICD-­‐10-­‐CM in October 2015. • A Summary of Chronic Fatigue Syndrome and Its Classification in the International Classification of Diseases. Prepared by the Centers for Disease Control and Prevention, National Center for Health Statistics, Office of the Center Director, Data Policy and Standards March 2001 http://www.co-­‐cure.org/ICD_code.pdf • Requests to the NCHS to reclassify CFS back to the neurological chapter o Sept 2011 -­‐ http://www.cdc.gov/nchs/data/icd/TopicpacketforSept2011a.pdf o Sept 2012 -­‐ http://www.cdc.gov/nchs/data/icd/Topic_packet_for_September_19_2012.pdf • Patient advocates emailed to Dr. Daulaire, the U.S. member of the Executive Board of the World Health Organization, to intervene and abide by WHO standards was unsuccessful in getting CFS reclassified to the neurological chapter. https://dl.dropboxusercontent.com/u/89158245/ICD-­‐10-­‐ CM%20letter%20to%20Daulaire%20May%202013.docx o In his June 28, 2013 response, he stated: “Thank you for your letter and apologies for my delayed reply. Thank you also for your continued advocacy around this disease which remains a challenge to the health community and a devastating disease for patients. We continue to strive to improve our knowledge of its etiology in order to better serve patients both in diagnosis and treatment… I welcome your continued input to the Coordination and Maintenance Committee during future meetings as reaching consensus in this process will be critical moving forward. The issue of determining the appropriate classification of CFS is important and I agree that we must strive to achieve a placement of the disease that is understood within the medical community and can advance our knowledge of this serious and complex syndrome.” 157 http://www.cms.gov/Medicare/Coding/ICD10/index.html “U.S. Department of Health and Human Services expects to release an interim final rule in the near future that will include a new compliance date that would require the use of ICD-­‐10 beginning October 1, 2015.” 158 WHO Guide to Mental Health In Primary Care” published by the WHO collaborating Center at Kings College. It is not clear exactly when this was first published but it is on the 2001 version of this page. http://web.archive.org/web/20010709061548/http://cebmh.warne.ox.ac.uk/cebmh/whoguidemhpcuk/disorders/f 48-­‐0.html 159 This article by Prins had even stated that “During the past few years, the UK collaborating centre of the WHO Guide to Mental Health in Primary Care unified CFS and ME in a single psychiatric code.” Prins, J. van der Meer, J., Bleijenberg, G. Chronic fatigue Syndrome. The Lancet, Volume 367, Pages 346 -­‐ 355, 28 January 2006 doi:10.1016/S0140-­‐6736(06)68073-­‐2 http://www.thelancet.com/journals/lancet/article/PIIS0140673606680732/fulltext#bib97 160 Correspondence from Andre L’Hours, Technical Officer at the WHO. A similar situation arose in England in 2001 when CFS was listed under both Mental and Behavioral Disorders/Neurasthenia and Nervous System Disorders. In a June 2001 press release reported by the CFIDS and numerous other organizations at the time, “Andre L’Hours, the Technical Officer at the WHO headquarters in Geneva who is responsible for the ICD, confirmed that it was "unacceptable" if the same disorder had been included in two places in the ICD-­‐10 and that the same disorder could not be differently categorized under the one WHO banner.” Multiple organizations reported at the time. • CFIDS -­‐ http://www.cfids-­‐cab.org/cfs-­‐inform/CFS.case.def/who.classification.me.cfs04.txt • The Gibson Report -­‐ www.erythos.com/gibsonenquiry/Docs/ME_Inquiry_Report.pdf and http://www.erythos.com/gibsonenquiry/Docs/Press_Release_26Nov06.rtf May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 64 Professor Emeritus Malcom Hooper’s Magical Medicine -­‐ www.investinme.org/Documents/Library/magical-­‐ medicine.pdf WHO January 23, 2004 response -­‐ “According to the taxonomic principles governing ICD-­‐10, it is not permitted for the same condition to be classified to more than one rubric”. 161 According to Suzy Chapman (http://dxrevisionwatch.com/), an advocate who has closely tracked ICD and DSM, the single chapter concept applies to ICD-­‐10 but in ICD-­‐11, terms can be dual listed. For instance, In ICD-­‐11, the Dementias and Alzheimer are primarily coded for in the Neurological chapter but they are secondary listed under Mental and behavioural disorders, under Neurocognitive disorders. This potential for dual listing could have important implications for this disease. This WHO document gives a similar example -­‐ www.who.int/classifications/icd/revision/icd11betaknownconcerns.pdf • “In the Beta browser participants may see more detail in “the foundation component” and this may be perceived as clutter. In fact this is a design feature, where a category may have multiple parents: e.g. a skin tumor is both a skin disease and a neoplasm.” 162 American Psychiatric Association Somatic symptom disorder Fact Sheet www.dsm5.org/Documents/Somatic Symptom Disorder Fact Sheet.pdf Highlights include: • “Somatic symptom disorder (SSD) is characterized by somatic symptoms that are either very distressing or result in significant disruption of functioning, as well as excessive and disproportionate thoughts, feelings and behaviors regarding those symptoms.” • “To be diagnosed with SSD, the individual must be persistently symptomatic (typically at least for 6 months)” • “The DSM-­‐IV diagnosis of somatization disorder required a specific number of complaints from among four symptom groups. The SSD criteria no longer have such a requirement; however, somatic symptoms must be significantly distressing or disruptive to daily life and must be accompanied by excessive thoughts, feelings, or behaviors.” • “Another key change in the DSM-­‐5 criteria is that while medically unexplained symptoms were a key feature for many of the disorders in DSM-­‐IV, an SSD diagnosis does not require that the somatic symptoms are medically unexplained” • “This change in emphasis removes the mind-­‐body separation implied in DSM-­‐IV and encourages clinicians to make a comprehensive assessment and use clinical judgment rather than a check list that may arbitrarily disqualify many people who are suffering with both SSD and another medical diagnosis from getting the help they need.” 163 All patients, even those with well-­‐known physical diseases like cancer, can be given a bolt-­‐on mental illness diagnosis if their medical provider decides that the patient is too concerned with his illness or health. But ME patients are at risk of having this be the sole diagnosis that they receive. And in fact, in spite of being classified as a neurological disease in the ICD-­‐10, in the U.K. today, CBT and GET are the only treatments offered to many patients in the UK, via NHS clinics and according to NICE G53 Guideline for CFS/ME. 164 Examples of CFS being referred to as Somatorm illness. • Overview -­‐ Slide presentation [PDF format] Somatoform disorders – functional somatic syndromes – Bodily distress syndrome. Need for care and organisation of care in an international perspective – EACLPP Lecture, Prof. Per Fink, MD, Ph.D, Dr.Med.Sc. www.functionaldisorders.dk • Michael B. First, M.D., DSM Somatic Presentations of Mental Disorders (September 6-­‐8, 2006). American Psychiatric Association. http://www.dsm5.org/research/pages/somaticpresentationsofmentaldisorders(september6-­‐8,2006).aspx • Gulf War and Health Volume 9: Treatment for Chronic Multisymptom Illness. Jan 23, 2013 www.iom.edu/Reports/2013/Gulf-­‐War-­‐and-­‐HealthTreatment-­‐for-­‐Chronic-­‐Multisymptom-­‐Illness/Report-­‐ Brief012313.aspx. This report states that it calls medically unexplained symptoms chronic multi-­‐symptom illness. It also uses the term MUPS for medically unexplained physical symptoms. While it doesn’t specifically state that It states that CFS, 165 Wessely, S., Nimnuan, C., Sharpe, M. Functional somatic syndromes: one or many? Lancet 1999; 354: 936–39 www.researchgate.net/publication/12810185_Functional_somatic_syndromes_one_or_many/file/79e415149530814 c3c.pdf • “Functional somatic symptoms and syndromes are a major health issue. They are common and may be persistent, disabling, and costly. Most of the current literature pertains to specific syndromes defined by medical subspecialties. We have put forward the hypothesis that the acceptance of distinct syndromes as defined in the medical literature should be challenged. We contend that the patients so defined actually have much in common. 166 Michael B. First, M.D., DSM Somatic Presentations of Mental Disorders (September 6-­‐8, 2006). American Psychiatric Association. http://www.dsm5.org/research/pages/somaticpresentationsofmentaldisorders(september6-­‐ 8,2006).aspx This document states: “Simon Wessely, MD (London, UK) presented on the association between the various functional somatic syndromes seen across medical specialties (e.g., irritable bowel syndrome, fibromyalgia, atypical chest pain, tension headache, etc.). Overall, unexplained medical symptoms are common in primary care settings (occurring in more than 50% of patients in one study). There is tremendous overlap among the symptoms included in the definitions of • May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 65 the various functional syndromes so that the more symptoms you have that are characteristic of one syndrome, the more likely one is to have symptoms characteristic of the other syndromes as well. …A latent class analysis of functional somatic symptoms in the community suggests the presence of five classes: a chronic fatigue-­‐like entity, a pan/myalgia-­‐like entity, an irritable bowel syndrome-­‐like entity, a depression entity, and an anxiety entity. Dr Wessely concluded that we should accept the existence of a concept of functional somatic symptoms/syndromes that differ from anxiety and depression, and that within this broad category we still need to respect the integrity of fibromyalgia, irritable bowel syndrome, chronic fatigue syndrome, and their cultural variants.” 167 The inclusion of SSD in the DSM-­‐5 has created significant concern for patients with ME because of this association of CFS with somatic disorder. Dr. Allen Frances has discussed this issue and the impact on patients whose diseases have been labeled as a somatic disorder. http://www.psychologytoday.com/blog/dsm5-­‐in-­‐distress/201212/mislabeling-­‐ medical-­‐illness-­‐mental-­‐disorder See also Diagnostic Ethics: Harms vs Benefits of Somatic Symptom Disorder Huffington Post, Den 16, 2013 http://www.huffingtonpost.com/allen-­‐frances/diagnostic-­‐ethics-­‐harms-­‐v_b_4450653.html Dr. Frances discusses the guidelines by the American Association of Family Physicians which urges doctors to make early diagnoses of somatoform disorders in order to save time and to reduce costs. 168 Diagnostic Ethics: Harms vs Benefits of Somatic Symptom Disorder Huffington Post, Den 16, 2013 http://www.huffingtonpost.com/allen-­‐frances/diagnostic-­‐ethics-­‐harms-­‐v_b_4450653.html Diagnostic Rights web site -­‐ http://www.diagnosticrights.org/the-­‐coalition/ 169 Dr. Allen Frances. Bad News: DSM 5 Refuses to Correct Somatic Symptom Disorder, January 16, 2013, Psychology Today. http://www.psychologytoday.com/blog/dsm5-­‐in-­‐distress/201301/bad-­‐news-­‐dsm-­‐5-­‐refuses-­‐correct-­‐somatic-­‐ symptom-­‐disorder 170 Wilcken, Hugo, DSM Criteria useless in Fibromyalgia: experts. February 21, 2014. Rheumatology Update. http://www.rheumatologyupdate.com.au/latest-­‐news/dsm-­‐5-­‐criteria-­‐useless-­‐in-­‐fibromyalgia-­‐experts. The authors were quoted as stating ““We are dubious that the DSM-­‐5 approach can distinguish validly and reliably which fibromyalgia patients are and which are not mentally ill, particularly in clinical care settings where diagnosis will come most often from generalists,” they concluded.” 171 Swidey, N. and Wen, P. “No release for Conn. teen caught in hospital dispute”, Boston Globe, Dec 21, 2013 http://www.bostonglobe.com/lifestyle/health-­‐wellness/2013/12/21/state-­‐retains-­‐custody-­‐teen-­‐limbo-­‐children-­‐ hospital-­‐for-­‐months/5TGcy5X8IxQusdtXgRmXdK/story.html 172 Story of Karina Hansen – Voices of the Shadows website. http://voicesfromtheshadowsfilm.co.uk/2013/karina-­‐ hansen-­‐is-­‐a-­‐severely-­‐ill-­‐danish-­‐patient-­‐who-­‐was-­‐forcibly-­‐taken-­‐from-­‐her-­‐home-­‐update-­‐may-­‐2013-­‐9th/ Letter by Karina’s parents to members of Parliament on March 19, 2014. In Danish. Use Google translate http://www.ft.dk/samling/20131/almdel/suu/bilag/311/1347104/index.htm Letter from Dr. Diane O’Leary from Diagnostic Rights to the Danish Minister of Health http://www.diagnosticrights.org/the-­‐coalitions-­‐letter-­‐to-­‐the-­‐danish-­‐minister-­‐of-­‐health-­‐on-­‐karina-­‐hansens-­‐behalf/ 173 Dr. Richard Fox, New Disease Discovery Could Be the Answer to “Mystery Illness”. January 9, 2013. Doctor’s Health Press. http://www.doctorshealthpress.com/pain-­‐articles/new-­‐disease-­‐discovery-­‐could-­‐be-­‐the-­‐answer-­‐to-­‐mystery-­‐ illness -­‐ based on work of Dr. Per Fink referenced above Also see the website for The Research Clinic for Functional Disorders and Psychosomatics at Aarhus University Hospital. http://funktionellelidelser.dk/en/about/treatment/ Also see Fink, Per, Somatoform disorders – functional somatic syndromes – Bodily distress syndrome. Need for care and organisation of care in an international perspective -­‐ EACLPP Lecture. Slides – www.eapm.eu.com/tl_files/content/Presentations/EACLPP_Per Fink_Somatoform Disorders.pdf or Google 174 It is difficult to state definitely what is being considered for ICD-­‐11 at this time. It appears that there are two different types of options being considered: • Bodily stress syndrome – Based on a 2012 article, the approach being considered by the Primary Care Consultation Group (PCCG) at that time. The concept drew heavily on Per Fink’s model, but also has some psychobehavioral criteria that are more reflective of DSM-­‐5’s concept of SSD. See reference below for Lam. • P Lam; D P Goldberg; A C Dowell; S Fortes; J K Mbatia; F A Minhas; M S Klinkman: Proposed new diagnoses of anxious depression and bodily stress syndrome in ICD-­‐11-­‐PHC: an international focus group study. Family Practice 2012; doi: 10.1093/fampra/cms037 o http://fampra.oxfordjournals.org/content/early/2012/07/20/fampra.cms037.long • Bodily distress disorder (BDD) – the concept being advanced by the Expert Working Group on Somatic Distress and Dissociative Disorders and the term entered into the Beta draft. The current Beta draft definition for BDD is based on wording from the work group's 2012 emerging proposals paper [ref] which had described a disorder that appeared to be a bolt-­‐on diagnosis for any disease, with a disorder model close to DSM-­‐5's Somatic symptom disorder References: • For more information on what is being done in the DSM and ICD, see http://dxrevisionwatch.com/ May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 66 Fink, Per, Somatoform disorders – functional somatic syndromes – Bodily distress syndrome. Need for care and organisation of care in an international perspective -­‐ EACLPP Lecture. • Slides – www.eapm.eu.com/tl_files/content/Presentations/EACLPP_Per Fink_Somatoform Disorders.pdf or Google for “Bodily distress syndrome. Need for care and organisation of care in an international perspective“ • Dr. Fink’s Clinic -­‐ http://funktionellelidelser.dk/en/about/bds/ • Lam et al “Proposed new diagnoses of anxious depression and bodily stress syndrome in ICD-­‐11-­‐PHC: an international focus group study”. Family Practice. July 2012. http://fampra.oxfordjournals.org/content/30/1/76.long. Also see this article that suggests a model like Per Fink’s. o Psychol Assess. 2013 Dec 2. [Epub ahead of print] Bifactor Analysis and Construct Validity of the HADS: A Cross-­‐Sectional and Longitudinal Study in Fibromyalgia Patients. Luciano JV, Barrada JR, Aguado J, Osma J, García-­‐Campayo J. http://www.uam.es/becarios/jbarrada/papers/hads.pdf “[...] In the upcoming primary healthcare version of the ICD-­‐11 (ICD-­‐11-­‐PHC), FM will be classified as part of bodily stress syndrome (BSS; Lam et al., 2013). This new diagnosis will group patients who might have previously been considered different (e.g., those with FM, chronic fatigue syndrome, irritable bowel syndrome, and so on) 175 ICD-­‐11 http://apps.who.int/classifications/icd11/browse/f/en#/http://id.who.int/icd/entity/1296093776 176 ICD-­‐11 Beta Bodily distress disorder Entry: “Bodily distress disorder is characterized by high levels of preoccupation regarding bodily symptoms, unusually frequent or persistent medical help-­‐seeking, and avoidance of normal activities for fear of damaging the body. These features are sufficiently persistent and distressing to lead to impairment in personal, family, social, educational, occupational or other important areas of functioning. The most common symptoms include pain (including musculoskeletal and chest pains, backache, headaches), fatigue, gastrointestinal symptoms, and respiratory symptoms, although patients may be preoccupied with any bodily symptoms. Bodily distress disorder most commonly involves multiple bodily symptoms, though some cases involve a single very bothersome symptom (usually pain or fatigue). http://apps.who.int/classifications/icd11/browse/l-­‐ m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f1472866636 177 October 2012 CFSAC recommendations -­‐ http://www.hhs.gov/advcomcfs/recommendations/10032012.html 178 Institute of Medicine Initiative to define new consensus clinical diagnostic criteria for ME and CFS – http://www.iom.edu/Activities/Disease/DiagnosisMyalgicEncephalomyelitisChronicFatigueSyndrome.aspx 179 Summary of patient concerns with the IOM and the handling of the GWI. https://dl.dropboxusercontent.com/u/89158245/MECFS%20Action%20Alert%20Background%20Sept%2025%202 013.pdf 180 IOM Chronic Multisymptom Illness in Gulf War Veterans: Case Definitions Reexamined. March 2014 http://www.iom.edu/Reports/2014/Chronic-­‐Multisymptom-­‐Illness-­‐in-­‐Gulf-­‐War-­‐Veterans-­‐Case-­‐Definitions-­‐ Reexamined.aspx Ruiz, Rebecca Experts Can't Decide On Definition For Mysterious Gulf War Illness. Forbes, March 12, 2014 http://www.forbes.com/sites/rebeccaruiz/2014/03/12/experts-­‐cant-­‐decide-­‐on-­‐definition-­‐for-­‐gulf-­‐war-­‐illness/ 181 Letter to Secretary Sebelius from 50 ME/CFS experts. Originally sent on 9/23 and resent on 10/25. https://dl.dropboxusercontent.com/u/89158245/Case%20Definition%20Letter%20Sept%2023%202013.pdf “We strongly urge the Department of Health and Human Services (HHS) to follow our lead by using the CCC as the sole case definition for ME/CFS in all of the Department’s activities related to this disease. In addition, we strongly urge you to abandon efforts to reach out to groups such as the Institute of Medicine (IOM) that lack the needed expertise to develop “clinical diagnostic criteria” for ME/CFS. Since the expert ME/CFS scientific and medical community has developed and adopted a case definition for research and clinical purposes, this effort is unnecessary and would waste scarce taxpayer funds that would be much better directed toward funding research on this disease. Worse, this effort threatens to move ME/CFS science backward by engaging non-­‐ experts in the development of a case definition for a complex disease about which they are not knowledgeable.” 182 Letter from Secretary Sebelius to Dr. Chris Snell in response to the letter from the 50 experts https://dl.dropboxusercontent.com/u/89158245/Nov%2012%202013%20Secretary%27s%20Response%20to%20 MECFS%20experts.pdf 183 FAQ from HHS on the OM contract. https://dl.dropboxusercontent.com/u/89158245/HHS%20FAQs%20on%20contract%20with%20the%20IOM%20to %20recommend%20clinical%20diagnostic%20criteria%20for%20ME_CFS%20%7C%20HHS.gov.html or http://www.hhs.gov/advcomcfs/notices/faqs-­‐iom.html 184 CFSAC May 2013 meeting. Exchange between Dr. Unger and CFSAC members. Minutes 25-­‐45. https://www.youtube.com/watch?v=VJ7VqYJTsWI&list=PLrl7E8KABz1FGfzllYcomOoI9agz8-­‐6QL&index=12 Putting a sharp point on patient concerns is the exchange from the May 2013 CFSAC in which CDC’s Dr. Unger questioned the importance of PEM as a symptom rhetorically asked the question “If a patient doesn’t have [post-­‐ exertional malaise], would you not manage them as a CFS patient?” • May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 67 185 Institute of Medicine Study for Diagnostic Criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Activity Description http://www.iom.edu/Activities/Disease/DiagnosisMyalgicEncephalomyelitisChronicFatigueSyndrome.aspx § “An Institute of Medicine (IOM) committee will comprehensively evaluate the current criteria for the diagnosis of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). The committee will consider the various existing definitions and recommend clinical diagnostic criteria for the disorder to address the needs of health providers, patients, and their caregivers.” § “The committee will also distinguish between disease subgroups, develop a plan for updating the new criteria, and make recommendations for its implementation. Any recommendations made by the committee will consider unique diagnostic issues facing people with ME/CFS, specifically related to: gender, across the lifespan, and specific subgroups with substantial disability.” § “Specifically the IOM will: – Conduct a study to identify the evidence for various diagnostic clinical criteria of ME/CFS using a process with stakeholder input, including practicing clinicians and patients; – Develop evidence-­‐based clinical diagnostic criteria for ME/CFS for use by clinicians, using a consensus-­‐building methodology; – Recommend whether new terminology for ME/CFS should be adopted; – Develop an outreach strategy to disseminate the definition nationwide to health professionals.” Regarding the choice of a consensus based methodology, CFSAC Discussions –June 2012 Page 41. www.hhs.gov/advcomcfs/meetings/minutes/cfsac20120514.pdf § HHS has previously stated that new definitions should be data driven so its unclear why they have chosen a consensus approach for this. Dr. Belay of CDC stated “My second point is that I think the definitions should be data-­‐driven. We should not be creating a case definition in a vacuum. It has to be supported by data.” 186 Both the Statement of Task (SOT) on the IOM website and the Statement of Work (SOW) provided by HHS are vague on this issue. The SOT uses the term “ME/CFS” without defining what is meant by it. The SOW does define the term “ME/CFS”, stating that: ME/CFS shall be used to refer to Myalgic Encephalomyelitis (ME), Chronic Fatigue Syndrome (CFS), Chronic Fatigue and Immune Dysfunction Syndrome (CFIDS), Neuroendocrine Immune Disorder, and other terminologies in use for this illness. https://dl.dropboxusercontent.com/u/57025850/MECFS%20IOM%20SOW.pdf It is important to ask what these terms really mean. Is the term “ME” referring to the disease described by the Canadian Consensus Criteria? Does CFS include Oxford, Fukuda without PEM? 187 Prior to the IOM meeting, both Kate Meck of IOM and Dr. Nancy Lee of HHS stated in personal emails to the author that this had not been decided yet. But when asked more specifically how ME would be handled, Dr. Lee referenced the SOT statement about the creation of subgroups and indicated that ME would become a subgroup or part of a spectrum of the broader “CFS” illnesses. She also stated that for the sake of the target audience -­‐ primary care physicians -­‐ it was better to start broader and then define subgroups. Dr. Lee’s charge to the IOM panel did not provide any further direction on this issue. 188 CDC Multi-­‐site study -­‐ http://www.cdc.gov/cfs/programs/clinical-­‐assessment/ Further notes:. CDC has decided against using the replicated CPET to objectively measure the hallmark post-­‐ exertional malaise and instead is using a mechanism to detect the presence of this most critical symptom that to my knowledge has not been replicated or validated. Finally, because of issues with study design, the participants are largely white, female, with insurance, highly educated and not the most severe. As pointed out by an IOM panel member at the first IOM public meeting, these patients do not represent the demographic of ME. Regarding inclusion and exclusion -­‐ “The study started in 2012 and aims to enroll 450 patients. Any patient (aged 18 – 70 years) that is managed or diagnosed with CFS, post-­‐infective fatigue (PIF) or myalgic encephalomyelitis (ME) at any of seven participating clinical sites is eligible for participating in this study. Study exclusions include illness onset at age older than 62 years, HIV infection, current pregnancy, or dementia.” 189 Post-­‐infective fatigue is an ill-­‐defined term. The closest case definition that I am aware of is post-­‐infectious fatigue syndrome, which is a subcategory of the Oxford definition described as “a subtype of CFS which either follows an infection or is associated with a current infection”. This would be a very broad category of illness given that the only other criteria is 6 months of chronic fatigue. Given that different clinicians may include different types of illness under these cases, its important to ask whether they would collectively agree on who has the disease but it does not appear that cross-­‐site validation is being done. At the first public IOM meeting on ME/CFS, Dr. Lily Chu and Dr. Unger of CDC had an exchange on this issue. http://www.youtube.com/watch?v=U9D59TU-­‐JUY Dr. Chu asked “I can understand why you are asking clinicians to come up with their own idea of who fits the CFS diagnosis. And I wondered if there was any thought given to see if there were any patients where three or two different physicians, they might not examine them but looking at the data we think this patient have CFS.” May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 68 Dr. Unger replied: “The clinicians involved in the study have not exchanged data so to speak in terms of that. We would have to let them decide if they wanted to undergo that exercise but I think they are confident in their diagnostic skills.” At the same meeting, Dr. Klmas also asked whether there would be any effort to compare the diagnosis to the various definitions. Dr. Jason has developed a tool that allows this comparison to be made by using the questions from the DePaul inventory. It was not clear if this would be done. 190 Exchange with CDC on CPET • Letter from Patient advocates to CDC requesting the incorporation of 2 day CPET -­‐ https://dl.dropboxusercontent.com/u/89158245/Advocates%20letter%20to%20CDC%20on%20CEPT%20Jul y%202013.doc • Dr. Unger response to patient request to use CPET -­‐ https://dl.dropboxusercontent.com/u/89158245/Dr.%20Unger%20Response%20to%20CPET%20letter%20J uly%202013.pdf 191 Pathways to Prevention Process links • NIH P2P site -­‐ https://prevention.nih.gov/programs-­‐events/pathways-­‐to-­‐prevention • OccupyCFS explanation of the process -­‐ http://www.occupycfs.com/tag/p2p/ and http://www.occupycfs.com/2014/01/06/behind-­‐closed-­‐doors/ • On the use for controversial areas -­‐ “P2P workshops are designed for topics that have incomplete or underdeveloped research, difficulty producing a report synthesizing published literature, and are generally not controversial.” 192 Pathways to Prevention website http://prevention.nih.gov/p2p/default.aspx. The NIH Pathways to Prevention Initiative was originally called the Evidence based Methodology Workshop. HHS provided the following description of P2P, originally called the Evidence based ethodology Workshop process -­‐ hhs.gov/advcomcfs/recommendations/response-­‐from-­‐ash-­‐10-­‐2012.pdf § October 12, 2012 CFSAC recommendation for the case definition meeting o Recommendation 1: CFSAC recommends that you will promptly convene (by 12/31/12 or as soon as possible thereafter) at least one stakeholders' (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) experts, patients, advocates) workshop in consultation with CFSAC members to reach a consensus for a case definition usefiul for research, diagnosis and treatment o fME/CFS beginning with the 2003 Canadian Consensus Definition for discussion purposes. § HHS Response o The National Institutes o f Health (NIH) is convening an Evidence-­‐based Methodology Workshop process (outlined in recommendation 3b) to address the issue of case definitions appropriate for ME/CFS research. However, it will not cover in detail a clinical case definition. The Office of the Assistant Secretary for Health, Department of Health and Human Services, is actively pursuing options for a separate effort that would work in coordination with the NIH process, but result in a case definition useful for clinicians who see patients with symptoms that may be ME/CFS. 193 P2P protocol from AHRG. http://www.effectivehealthcare.ahrq.gov/ehc/products/586/1906/chronic-­‐fatigue-­‐ protocol-­‐140501.pdf “An examination of the comparative effectiveness and harms of treatments for ME/CFS is important to guide clinical practice, which underscores the need for a systematic review on this topic. This report focuses on the clinical outcomes surrounding the attributes of fatigue, especially post-­‐exertional malaise and persistent fatigue, and its impact on overall function and quality of life because these are unifying features of ME/CFS that impact patients.” Key Questions include: • What methods are available to clinicians to diagnose ME/CFS and how do the use of these methods vary by patient subgroups? • What are the (a) benefits and (b) harms of therapeutic interventions for patients with ME/CFS and how do they vary by patient subgroups? PICOTS (Population, Intervention, Comparators, Outcomes, Timing, Setting • Population(s) Include: For KQ 1: Symptomatic adults (aged 18 years or older) with fatigue For KQ 2: Adults aged 18 years or older, with ME/CFS, without other underlying diagnosis Exclude: Children and adolescents Patients with other underlying diagnosis o Interventions • For KQ1: Case definitions: e.g., Fukada/CDC, Canadian, International and others • For KQ2: Forms of counseling and behavior therapy, graded exercise programs, complementary and alternative medicine (acupuncture, relaxation, massage, other), and symptom-­‐based medication May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 69 management (immune modulators, beta blockers, antidepressants, anxiolytics, stimulants, other) Setting o Include – Clinical Setting 194 In the May 2013 CFSAC, Dr. Maier described the P2P as follows:. http://www.hhs.gov/advcomcfs/meetings/minutes/cfsacmay23_final_508.pdf § Page 6 -­‐ Dr. Maier of the NIH has stated that the purpose of this workshop is to “identify methodological and scientific weaknesses in a scientific area and move the field forward through the unbiased and evidence-­‐based assessment of a very complex clinical issue” § Page 9 -­‐ The purpose of the workshop is to evaluate the research evidence surrounding the multiple case definitions and to address the validity, reliability, and ability of the current case definitions to identify individuals with the illness, identify individuals within the subgroups with the illness who can be differentiated by a case definition, and/or to identify responders or non-­‐responders based on some element of the case definition as informed by the evidence. This is all used to advance the research. It’s really an analysis of the science that supports the case definitions in the sense that the outcomes are telling us something or the outcomes are not telling us something. Where are the gaps? Where does the evidence show up? Where does it not? § Page 11 -­‐ The goal of the evidence-­‐based methodology workshop is to understand and identify how the evidence shows up for case definitions, for outcomes, for interventions, and for treatments. If it turns out that some interventions have more impact or a more positive outcome for post-­‐exertional malaise, then we’re going to know that post-­‐ exertional malaise in a case definition is probably going to be a good thing to do. The workshop is not advocating any specific case definition. It is simply a method to review it, to understand where the evidence shows up, where the gaps are, and where we need to move forward 195 Summary of concerns with P2P by Jennie Spotila http://www.occupycfs.com/2014/01/06/behind-­‐closed-­‐doors/ http://www.occupycfs.com/2014/01/13/more-­‐on-­‐p2p/ http://www.occupycfs.com/2014/05/02/protocol-­‐for-­‐disaster/ http://www.occupycfs.com/2014/05/19/will-­‐the-­‐real-­‐p2p-­‐please-­‐stand-­‐up/#comments http://www.occupycfs.com/2014/05/22/p2p-­‐agenda-­‐fatigue/ This post discusses a systemic review of the 20 ME/CFS definitions and the conclusions that were drawn http://www.occupycfs.com/2014/03/06/systematic-­‐overreaching/ Regarding the focus on diagnostics and treatment, the IOM contract states that P2P will provide input but the timelines of IOM and P2P do not appear to be aligned in a way that will allow that to happen. 196 Reeves et al. "Chronic Fatigue Syndrome – A Clinically Empirical Approach to Its Definition and Study" in BMC Medicine. 2005, December 15. http://www.biomedcentral.com/1741-­‐7015/3/19/ • “most studies of CFS merely note that they used the 1994 case definition and they do not generally specify how disability, fatigue and symptom occurrence were elucidated. Thus, it is difficult to assess the validity of their diagnostic criteria and essentially impossible to compare results between studies critically." 197 Larun L, Odgaard-­‐Jensen J, Brurberg KG, Chalder T, Dybwad M, Moss-­‐Morris RE, Sharpe M, Wallman K, Wearden A, White PD, Glasziou PP. Exercise therapy for chronic fatigue syndrome (individual patient data). Cochrane Database of Systematic Reviews 2014, Issue 4. Art. No.: CD011040. DOI: 10.1002/14651858.CD011040. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD011040/abstract The study specifies that the following participants will be included: “We will include male and female participants over the age of 17, irrespective of culture and setting. As several sets of criteria are currently used to diagnose CFS (Sharpe 1991; Fukuda 1994; Carruthers 2011) we will include trials given that the patients fulfill the following diagnostic criteria for CFS: • Fatigue or a synonym is a prominent symptom; • Fatigue is medically unexplained (i.e. other diagnosis known to cause fatigue such as psychiatric disorders and cancer should be excluded); • Fatigue is sufficiently severe to significantly disable or distress the patient; and • Fatigue has persisted for at least six months. We will include trials which include patients with disorders other than CFS as long as more than 90% of the patients had a primary CFS diagnosis according to the criteria above. Trials in which less than 90% of participants had a primary diagnosis of CFS will only be included in the analysis of this review if data for CFS are reported separately.” 198 Brurberg, K., Fønhus, A., Larun, L., Flottorp, S., Malterud, K. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): a systematic review. BMJ Open 2014;4:e003973 doi:10.1136/bmjopen-­‐2013-­‐003973 http://bmjopen.bmj.com/content/4/2/e003973.long#T1 199 CFSAC May 2013 meeting. Exchange between Dr. Unger and CFSAC members. Minutes 25-­‐45. https://www.youtube.com/watch?v=VJ7VqYJTsWI&list=PLrl7E8KABz1FGfzllYcomOoI9agz8-­‐6QL&index=12 Putting a sharp point on patient concerns is the exchange from the May 2013 CFSAC in which CDC’s Dr. Unger questioned the importance of PEM as a symptom rhetorically asked the question “If a patient doesn’t have [post-­‐ o May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 70 exertional malaise], would you not manage them as a CFS patient?” Adding to this is the response to the joint patient request to adopt the Canadian Consensus Criteria in which Dr. Unger stated that CDC is committed to studying “CFS and other similar medically unexplained chronically fatiguing illnesses such as ME, fibromyalgia syndrome, neurasthenia…”199 The ambiguity around the importance of PEM, the apparent continued focus on “CFS” regardless of the symptom of PEM and the focus on medically unexplained chronically fatiguing illnesses that include neurasthenia, a mental illness, amplifies the concerns that HHS’ definitional efforts are not focused on a definition for ME. 200 The IOM public file for the initiative to develop new clinical diagnostic criteria contains the following document which was reportedly submitted to IOM by CDC. https://dl.dropboxusercontent.com/u/89158245/IOM%20submission%20from%20CDC%20CFS%20Case%20Defini tion%20Issues%20with%20Appendices%201_28_14-­‐under%20NCEZID%20review.docx 201 Examples include • Nijs J, Roussel N, Van Oosterwijck J, De Kooning M, Ickmans K, Struyf F, Meeus M, Lundberg M. Fear of movement and avoidance behaviour toward physical activity in chronic-­‐fatigue syndrome and fibromyalgia: state of the art and implications for clinical practice. Clin Rheumatol. 2013 May 3. http://www.ncbi.nlm.nih.gov/pubmed/23639990 • Pariante, C. In his 2012 review of “Should Myalgic Encephalomyelitis and chronic fatigue syndrome (ME/cfs) be regarded as prolonged sickness behavior?”, Pariante states “For many, including this reviewer, CFS/ME is predominantly a condition triggered by excessive rest in predisposed individuals following acute triggers, and its interpretation requite a psychosocial and psychiatric framework.” http://www.biomedcentral.com/1741-­‐ 7015/11/64/prepub • Over the years, a number of authors have characterized chronic fatigue syndrome as a classic example of a somatic/somatoform disorder. One example is the following 2013 presentation on the Royal College. http://www.rcpsych.ac.uk/pdf/C%20Feinmann%20Slides.pdf. 202 CDC CME “Diagnosis and Management of Chronic Fatigue Syndrome” http://www.cdc.gov/cfs/education/diagnosis/index.html Page 1-­‐9. Page 5 includes reference to the recommendations to add standardized measures to the case definition in 2003. These are the Empirical definition changes. • Interestingly, CDC has not always taken this position. In October 2009, the CDC CFS website described ME as a separate illness http://web.archive.org/web/20091026164234/http://cdc.gov/cfs/cfsbasicfacts.htm o “Similar Medical Conditions: A number of illnesses have been described that have a similar spectrum of symptoms to CFS. These include fibromyalgia syndrome, myalgic encephalomyelitis, neurasthenia, multiple chemical sensitivities, and chronic mononucleosis. Although these illnesses may present with a primary symptom other than fatigue, chronic fatigue is commonly associated with all of them.” • Also the following article stated that Canadian and Fukuda were different patient groups. Switzer WM, Jia H, Hohn O, Zheng HQ, Tang S, Shankar A, Bannert N, Simmons G, Hendry RM, Falkenberg VR, Reeves WC, Heneine W. "Absence of Evidence of Xenotropic Murine Leukemia Virus-­‐related Virus Infection in Persons with Chronic Fatigue Syndrome and Healthy Controls in the United States." in Retrovirology. 2010, July 1: o “The 1994 International CFS case definition and the Canadian Consensus Criteria are different and do not necessarily identify similar groups of ill persons... The physical findings in persons meeting the Canadian definition may signal the presence of a neurologic condition considered exclusionary for CFS. 203 Regarding Dr. Unger’s statement on the Empirical definition. In a November 9, 2011 CFSAC meeting minutes exchange between Dr. Jason and Dr. Unger. Dr. Jason asked about the continued publication of Empirical study results (the 2005 Empirical definition has been discredited) and how the CDC intended to evolve the criteria? Dr. Unger’s response that they had done a study comparing “the standardized approach to applying the Fukuda definition [Empirical definition] and the approach that we had used in the past in the Wichita studies. Everyone will find it very reassuring that the patient populations are quite comparable.” A study was to have been published in early 2012 but so far that study does not appear to be available. http://www.hhs.gov/advcomcfs/meetings/minutes/cfsac_min-­‐11092011.pdf -­‐ page 24 204 The CDC CFS Toolkit states that one set of clinical guidelines is suitable for CFS patients and even for “CFS-­‐like” illness (6 months of fatigue but does not meet the rest of the symptom requirements for CFS). Other documents, like the 2012 CDC “Diagnosis and Management CFS” CME referenced above also give a single set of guidelines for all 5 definitions. http://www.cdc.gov/cfs/toolkit/index.html 205 Kindlon, T. Reporting of Harms Associated with Graded Exercise Therapy and Cognitive Behavioural Therapy in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, Bulletin of the IACFS/ME, Fall 2011 http://www.iacfsme.org/BULLETINFALL2011/Fall2011KindlonHarmsPaperABSTRACT/tabid/501/Default.aspx 206 The American College of Physicians and MedPageToday’s KevinMD takes a similar positon http://www.kevinmd.com/blog/2014/02/mksap-­‐32yearold-­‐woman-­‐chronic-­‐fatigue-­‐syndrome.html This site provides information on CFS as part of the Medical Knowledge Self Assessment program produced by the American College of Physicians -­‐ https://mksap16.acponline.org/ Section on General issues states May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 71 a. CBT in this setting is targeted in part at breaking the cycle of effort avoidance, decline in physical conditioning, and increase in fatigue and can work well in combination with graded exercise in this regard. CBT reduces fatigue and improves functional status. Another site is Cleveland CLinic http://www.clevelandclinicmeded.com/online/casebased/decisionmaking/chronic-­‐fatigue/ • This site provides a footnote that says that the disease is also called ME but says that there is a separate case definition for ME. • Question 3 – “ Another diagnostic term, myalgic encephalomyelitis (ME) is frequently used for CFS outside the US and also implies a known pathophysiology, but ME has its own case definition, separate from CFS.(4) “ The reference given is Prins JB, van der Meer JW, Bleijenberg G. Chronic fatigue syndrome. Lancet. 2006; 367:346-­‐55. • Question 8 on graded exercise – [CBT’s] goal is to help the patient gradually return to their normal physical activities. Other interventions such as antidepressants may help with associated mood disorders but have not been demonstrated to be beneficial in treating the core symptoms of CFS in those without depression. • Question 9 on CBT: Cognitive behavioral therapy (CBT) aims to change the cognitive responses that are thought to perpetuate CFS, such as fears about symptoms or activity, and social and emotional obstacles 207 One example is the review behind the NICE guidelines Bagnall, A., Hempel, S., Chambers, D., Orton, V., Forbes, C. The diagnosis, treatment and management of chronic fatigue syndrome (CFS) / myalgic encephalomyelitis (ME) in adults and children. Centre for Reviews and Dissemination University of York. October 2005. www.nice.org.uk/nicemedia/live/11630/34188/34188.pdf Another example is the 2001 review -­‐ Mulrow CD, Ramirez G, Cornell JE, Allsup K. Defining and managing chronic fatigue syndrome. Evidence Report: Technology Assessment (Summary) 2001:1-­‐4. http://www.ncbi.nlm.nih.gov/books/NBK11946/ 208 Larun L, Odgaard-­‐Jensen J, Brurberg KG, Chalder T, Dybwad M, Moss-­‐Morris RE, Sharpe M, Wallman K, Wearden A, White PD, Glasziou PP. Exercise therapy for chronic fatigue syndrome (individual patient data). Cochrane Database of Systematic Reviews 2014, Issue 4. Art. No.: CD011040. DOI: 10.1002/14651858.CD011040. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD011040/abstract The study specifies that the following participants will be included: “We will include male and female participants over the age of 17, irrespective of culture and setting. As several sets of criteria are currently used to diagnose CFS (Sharpe 1991; Fukuda 1994; Carruthers 2011) we will include trials given that the patients fulfill the following diagnostic criteria for CFS: • Fatigue or a synonym is a prominent symptom; • Fatigue is medically unexplained (i.e. other diagnosis known to cause fatigue such as psychiatric disorders and cancer should be excluded); • Fatigue is sufficiently severe to significantly disable or distress the patient; and • Fatigue has persisted for at least six months. We will include trials which include patients with disorders other than CFS as long as more than 90% of the patients had a primary CFS diagnosis according to the criteria above. Trials in which less than 90% of participants had a primary diagnosis of CFS will only be included in the analysis of this review if data for CFS are reported separately.” 209 Price JR, Mitchell E, Tidy E, Hunot V. Cognitive behaviour therapy for chronic fatigue syndrome in adults. Cochrane Database of Systematic Reviews 2008, Issue 3. Art. No.: CD001027. DOI: 10.1002/14651858.CD001027.pub2. http://www.ncbi.nlm.nih.gov/pubmed/18646067, http://www.cfids-­‐cab.org/rc/Price.pdf. • "All studies specified inclusion criteria requiring that participants had fatigue as their main or major complaint, the minimum duration of fatigue being six months in 12 studies, at least four months in one study, and at least three months in the two remaining studies. There was heterogeneity of other recruitment criteria between studies. Seven studies used the ’CDC’ (’Fukuda’) criteria for inclusion. One of these studies waived the requirement of four of eight additional symptoms included in the CDC criteria to be present. Three studies used the ’Oxford’ criteria for participant inclusion. The sample in Deale fulfilled CDC as well as Oxford criteria. Two studies used the ’Australian’ criteria. Three studies did not use standard CFS criteria. Two of these studies used a score of at least 4 on the Chalder fatigue scale as the basis for inclusion. The remaining study included subjects who scored 35 or more on the Dutch Checklist Individual Strength and who had been completely absent from work for 6-­‐26 weeks on health grounds. These studies thus had samples suffering from chronic fatigue, of which a sub-­‐sample met CDC chronic fatigue syndrome criteria. 210 White PD, Goldsmith K, Johnson AL, Chalder T, Sharpe M; PACE Trial Management Group. Recovery from chronic fatigue syndrome after treatments given in the PACE trial. Psychol Med. 2013 Jan 31:1-­‐9. [Epub ahead of print] http://journals.cambridge.org/action/displayFulltext?type=1&fid=8826663&jid=PSM&volumeId=-­‐1&issueId=-­‐ 1&aid=8826661 • The recent publication from PACE states that they analyzed the data using ME criteria and the International (CDC) criteria. The International criteria was referenced as the Reeves 2003 publication “Identification of ambiguities in the 1994 chronic fatigue syndrome research case definition and recommendations for resolution” This is one of the May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 72 publications that led to the Empirical definition. Further, they only required that patients had the symptoms for 1 week prior to assessment, not 6 months, to qualify for a diagnosis of CFS. Regarding the ME criteria, they used a 1994 report from Westcare for the ME diagnosis. It is not clear why they did not use Fukuda, why they only required 1 week and why they did not use the much more widely accepted Canadian Consensus Criteria or the newer ME International Consensus Criteria. • Regarding assessment for the CDC criteria -­‐ “The research assessor used participant ratings to judge whether participants met the International (CDC) criteria for CFS at 52 weeks (Reeves et al. 2003), … For the purposes of this study, the four or more symptoms needed to be present within the previous week of the assessment date, rather than the previous 6 months (Reeves et al. 2003). Reeves 2003 was when the approach was first described. 2005 is when the first study using the approach was published. • In addition to using modified versions of criteria that were either largely abandoned or seldom used to begin with, the PACE trial also used measures of recovery that are broadly disputed by the patient community. It remains to be seen how the research community will respond to the latest PACE paper but it is important to note that PACE style CBT and GET have been rejected by a number of researchers and clinicians as well as by the IACFS/ME Primer (http://www.iacfsme.org/Portals/0/PDF/PrimerFinal3.pdf -­‐ p23 for CBT comments.) 211 Jason, L., Brown, A., Evans, M., Sunnquist, M., Newton, J. Contrasting chronic fatigue syndrome versus myalgic encephalomyelitis/chronic fatigue syndrome. Biomedicine, Health & Behavior, DOI:10.1080/21641846.2013.774556. http://dx.doi.org/10.1080/21641846.2013.774556 Also see • Jason, L., Brown, A. Clyne, E. Bartgis, L, Evans, M., Brown, M. Contrasting Case Definitions for Chronic Fatigue Syndrome, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Myalgic Encephalomyelitis Eval Health Prof published online 7 December 2011 http://ehp.sagepub.com/content/early/2011/10/18/0163278711424281 • Brown, A.; Jason, L.; Evans, M.; Flores, S. Contrasting Case Definitions: The ME International Consensus Criteria vs. the Fukuda et Al. CFS Criteria. North American Journal of Psychology, Vol. 15, No. 1, March 2013. http://www.questia.com/library/1G1-­‐322563471/contrasting-­‐case-­‐definitions-­‐the-­‐me-­‐international. Brown et al examined the ME-­‐ICC and the Fukuda and found that the ME-­‐ICC identified a much tighter group of patients (39 compared to 113 for Fukuda) with more functional impairments and physical, mental and cognitive problems than in those patients meeting the Fukuda criteria. The paper also raised a concern that ME-­‐ICC included more psychiatric co-­‐morbidities than Fukuda because of the number of symptoms required and concluded that a focus on a smaller number of hallmark symptoms like post-­‐exertional malaise would be critical. Finally, the paper acknowledges the need for more study because this study used a questionnaire designed for Fukuda CFS, that they were unable to assess one of the key ME-­‐ICC criteria because of the available data and the study did not look at homebound or bedbound patients. Such study will help to refine the CCC over time. 212 Jason, L., Sunnquist, M., Brown, A., Evans, M., Newton, J. Are Myalgic Encephalomyelitis and chronic fatigue syndrome different illnesses? A preliminary analysis. Journal of Health Psychology 1–13 , 2014 213 Jason, L. “Defining CFS: Diagnostic Criteria and Case Definition”. CFIDS association webinar, April 2010. www.cfids.org/webinar/jason-­‐slides041410.pdf slide 12 214 Jason, L. “Defining CFS: Diagnostic Criteria and Case Definition”. CFIDS association webinar, April 2010. www.cfids.org/webinar/jason-­‐slides041410.pdf slide 10, 12. Jason’s presentation discusses the fact that Fukuda does not require core symptoms and that depressed patients have the same symptoms as one combination of Fukuda symptoms. Oxford is even broader than Fukuda and specifically allows the inclusion of psychiatric patients. 215 Jason, L., Richman, J., Friedberg, F., Wagner, L., Taylor, R., Jordan, K. Politics science and the emergence of a new disease. September 1997, American Psychologist. Vol. 52, No. 9, 973-­‐983 http://www.ncbi.nlm.nih.gov/pubmed/9301342 “Over the past ten years, a series of key decisions were made concerning the criteria for CFS diagnosis and the selection of psychiatric instruments, which scored CFS symptoms as medical or psychiatric problems. At least some of these decisions may have been formulated within a societal and political context in which CFS was assumed to be a psychologically determined problem.” 216 Dr. Jason has made the point in numerous publications, noted in this document that the researchers conceptualization of the disease affects their decisions about the choice of instruments used to apply the definition and how they ascertain cases of CFS. One example is: Jason, L., Richman, J., Friedberg, F., Wagner, L., Taylor, R., Jordan, K. Politics science and the emergence of a new disease. September 1997, American Psychologist. Vol. 52, No. 9, 973-­‐983 http://www.ncbi.nlm.nih.gov/pubmed/9301342 “Over the past ten years, a series of key decisions were made concerning the criteria for CFS diagnosis and the selection of psychiatric instruments, which scored CFS symptoms as medical or psychiatric problems. At least some of these decisions may have been formulated within a societal and political context in which CFS was assumed to be a psychologically determined problem.” 217 Reeves et al. "Chronic Fatigue Syndrome – A Clinically Empirical Approach to Its Definition and Study" in BMC Medicine. 2005, December 15. http://www.biomedcentral.com/1741-­‐7015/3/19/ May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 73 “most studies of CFS merely note that they used the 1994 case definition and they do not generally specify how disability, fatigue and symptom occurrence were elucidated. Thus, it is difficult to assess the validity of their diagnostic criteria and essentially impossible to compare results between studies critically." 218 Jason, L., Richman, J., Friedberg, F., Wagner, L., Taylor, R., Jordan, K. Politics science and the emergence of a new disease. September 1997, American Psychologist. Vol. 52, No. 9, 973-­‐983 http://www.ncbi.nlm.nih.gov/pubmed/9301342 “Over the past ten years, a series of key decisions were made concerning the criteria for CFS diagnosis and the selection of psychiatric instruments, which scored CFS symptoms as medical or psychiatric problems. At least some of these decisions may have been formulated within a societal and political context in which CFS was assumed to be a psychologically determined problem.” 219 De Becker P, McGregor N, De Meirleir K. A definition-­‐based analysis of symptoms in a large cohort of patients with chronic fatigue syndrome. J Intern Med. 2001 Sep;250(3):234-­‐40. http://www.ncbi.nlm.nih.gov/pubmed/11555128 “Comparison of Holmes and Fukuda – “The CFS patients fulfilling the Holmes criteria have an increased symptom prevalence and severity of many symptoms. Patients fulfilling the Fukuda criteria were less severely affected patients which leads to an increase in clinical heterogeneity. Addition of certain symptoms and removal of others would strengthen the ability to select CFS patients.” 220 Kennedy, G., Abbot, N., Spence, V., Underwood, C., Belch, J. The Specificity of the CDC-­‐1994 Criteria for Chronic Fatigue Syndrome: Comparison Of Health Status in Three Groups of Patients Who Fulfill the Criteria. Ann Epidemiol 2004;14:95–100. cfids-­‐cab.org/cfs-­‐inform/Subgroups/kennedy.etal04.pdf 221 Nacul, L., Lacerda, E., Pheby, D., Campion, P., Molokhia, M., Fayyaz, S., Leite, J., Poland, F., Howe, A., Drachler, M. Prevalence of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) in three regions of England: a repeated cross-­‐sectional study in primary care. BMC Medicine 2011, 9:91 doi:10.1186/1741-­‐7015-­‐9-­‐91. http://www.biomedcentral.com/1741-­‐7015/9/91 222 Maes, M., et al., Myalgic Encephalomyelitis (ME), Chronic Fatigue Syndrome (CFS), and Chronic Fatigue (CF) are distinguished accurately: Results of supervised.... Psychiatry Research (2012), http://dx.doi.org/10.1016/j.psychres.2012.03.031 http://www.ncbi.nlm.nih.gov/pubmed/22521895 223 Brenu EW, Johnston S, Hardcastle SL, Huth TK, Fuller K, et al. (2013) Immune Abnormalities in Patients Meeting New Diagnostic Criteria for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. J Mol Biomark Diagn 4: 152. doi:10.4172/2155-­‐9929.1000152 http://www.omicsonline.org/immune-­‐abnormalities-­‐in-­‐patients-­‐meeting-­‐new-­‐ diagnostic-­‐criteria-­‐for-­‐chronic-­‐fatigue-­‐syndromemyalgic-­‐encephalomyelitis-­‐2155-­‐9929.1000152.pdf?aid=20654 Note that this was a study of patients pulled from a clinic that treats “ME/CFS” patients. It is reasonable to expect that their application of Fukuda is stricter than the general research community at large. 224 Johnston, S., Brenu, E., Staines, D., Marshall-­‐Gradisnik, S. The role of clinical guidelines for chronic fatigue syndrome/myalgic encephalomyelitis in research settings, Fatigue: Biomedicine, Health & Behavior (2013): DOI: 10.1080/21641846.2013.860779 . http://www.tandfonline.com/doi/abs/10.1080/21641846.2013.860779#preview This study compared three primers – the Centers for Disease Control and Prevention (CDC) Toolkit; the International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (IACFS/ME) Primer; and the International Consensus Primer. The purpose of this review is to evaluate the differences and similarities among three sets of guidelines and their definitional criteria. “It has been argued that the 1994 CDC criteria are broadly inclusive and, thus, more likely to select widely heterogeneous patient groups.[26,27] This heterogeneity has been demonstrated among distinct patient sets that all fulfill the definition, but are based on widely different clinical measures.[28] In contrast, the CCC and ICC have been shown to select cases with more severe impairments in physical and social functioning.[29–31]” 225 The report of the Group on Scientific Research into ME (The Gibson Report): www.erythos.com/gibsonenquiry/Docs/ME_Inquiry_Report.pdf http://www.erythos.com/gibsonenquiry/Docs/Press_Release_26Nov06.rtf “The Group on Scientific Research into ME has been established to assess the progress of scientific research on ME since the publication of the Chief Medical Officer's Working Group Report into CFS/ME in 2002. In particular the Group has been established to – o increase public understanding of scientific research into ME/CFS o evaluate progress in the development of a full program of research into ME/CFS o identify research and funding requirements in establishing the cause of ME/CFS? In 2005, Dr. Gibson chaired a cross-­‐party ME/CFS science inquiry with members from both Houses of Parliament, The Group on the Scientific Research into ME (GSRME). The report was issued in November 2006; The GSRME was a NICE Stakeholder. “NICE claims that both CBT and graded exercise therapy are supported by an adequate evidence base, however, the GDG relied on a very small number of controversial randomised control trials (RCTs). The patient selection criteria for participating in the trials were too wide and therefore allowed non-­‐ME/CFS suffers to participate. It is also misleading to refer to CBT & GET as `treatments' of `choice'. They cannot properly be described as treatments, since, as NICE admits, they do not address the core pathology of ME.” • May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 74 Additional statement by Dr. an Gibson on NICE guidelines -­‐ http://www.investinme.org/Article-­‐ 301%20Ian%20Gibson%20NICE%20Guideline%20Witness%20Statement.htm 226 There are a number of studies that show a difference between patients with ME and patients with psychiatric illness. For instance, • For instance, patients have reduced gray matter volume and blood flow in the brain along with abnormal proteins in the spinal fluid and increased lactate levels. Komaroff AL, Cho TA. Role of infection and neurologic dysfunction in chronic fatigue syndrome. Semin Neurol. Epub 2011 Sep 30 http://www.ncbi.nlm.nih.gov/pubmed/21964849 • There are changes in EEG that are consistent with brain dysregulation. Zinn, Mark, Zinn, Marcia. Report on qEEG and LORETTA at the March 2014 IACFE/ME conference. They reported “decreased Peak Alpha Frequency (PAF) across 58% of the entire cortex compared to controls” and stated “these findings are consistent with reduced efficiency of thalamo-­‐cortical connections in CFS participants.”. They also reported ‘evidence of widespread cortical hypoactivation in CFS patients as demonstrated by increased delta and decreased beta2 sources” and stated that ‘the findings provide objective quantification of central nervous system dysregulation in CFS sufferers.” They showed how the symptoms of ME/CFS are seen in executive function disorders that include diseases like Alzheimer and Parkinson. • There are demonstrable visual disturbances that include foggy/shadowed vision, difficulty in tracking objects and problems with eye movement. o Hutchinson CV, Badham SP. Patterns of abnormal visual attention in myalgic encephalomyelitis. Optom Vis Sci. 2013 Jun;90(6):607-­‐14. doi: 10.1097/OPX.0b013e318294c232. http://www.ncbi.nlm.nih.gov/pubmed/23689679 o Hutchinson, CV. Letter Br J Ophthalmol 2014;98:144-­‐145 doi:10.1136/bjophthalmol-­‐2013-­‐304439 http://bjo.bmj.com/content/98/1/144.extract o Badham SP1, Hutchinson CV. Characterising eye movement dysfunction in myalgic encephalomyelitis/chronic fatigue syndrome. Graefes Arch Clin Exp Ophthalmol. 2013 Dec;251(12):2769-­‐76. doi: 10.1007/s00417-­‐013-­‐2431-­‐3. Epub 2013 Aug 6. http://www.ncbi.nlm.nih.gov/pubmed/23918092 o Review article http://www.everydayhealth.com/chronic-­‐fatigue-­‐syndrome/vision-­‐problems.aspx • There are altered sleep waves and cognitive dysfunctions that cause decreased processing speeds and lead to mental confusion and impairment of memory. Blood pressure and heart rate regulation is not working properly and heart rates can rise dramatically simply from standing or even just sitting up • Energy production impairment -­‐ Presentation by Dr. Snell to CFSAC, October 12, 2010. Includes references to statements by various medical societies including the American Heart Association, about the use of CPET as a gold standard o Slides -­‐ http://www.hhs.gov/advcomcfs/meetings/presentations/presentation_10132010_snell-­‐ stevens.pdf o Video – starting at 4:38 -­‐ http://hhs.granicus.com/MediaPlayer.php?view_id=5&clip_id=99; http://media-­‐02.granicus.com:443/ondemand/hhs/hhs_b947e197-­‐a39c-­‐4c51-­‐8b89-­‐ 077723983c8c.mp3 227 Carruthers, B., van de Sande, M., De Meirleir, K., Klimas, K., Broderick, G., Mitchell, T., Staines, D., Powles, A., Speight, N., Vallings, R., Bateman, L., Baumgarten-­‐Austrheim, B., Bell, D., Carlo-­‐Stella, N., Chia, J., Darragh, A., Jo, D., Lewis, D., Light. A., Marshall-­‐Gradisbik, S., Mena, I., Mikovits, J., Miwa, K., Murovska, M., Pall, M., Stevens, S. Myalgic encephalomyelitis: International Consensus Criteria. Journal of Internal Medicine. Volume 270, Issue 4, pages 327–338, October 2011. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-­‐2796.2011.02428.x/full 228 Prins, J. van der Meer, J., Bleijenberg, G. Chronic fatigue syndrome. The Lancet, Volume 367, Issue 9507, Pages 346 -­‐ 355, 28 January 2006. doi:10.1016/S0140-­‐6736(06)68073-­‐2 Prins also stated “Although they differ, all case definitions select severely fatigued groups of patients.” http://www.ncbi.nlm.nih.gov/pubmed/16443043 229 Stephen Straus, NIH National Institute of Allergy and Infectious Diseases, Editorial, Chronic fatigue syndrome. Biopsychosocial approach may be difficult in practice. BMJ October 1996; 313:831 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2359057/pdf/bmj00562-­‐0007.pdf • In essence, it [Fukuda] classifies a constellation of prolonged and debilitating symptoms as worthy of medical attention and study…. Related case criteria were developed by consensus at Oxford in 1991.Neither the American (Fukuda] nor the Oxford criteria assume the syndrome to be a single nosological entity 230 Prins, J. van der Meer, J., Bleijenberg, G. Chronic fatigue syndrome. The Lancet, Volume 367, Issue 9507, Pages 346 -­‐ 355, 28 January 2006. doi:10.1016/S0140-­‐6736(06)68073-­‐2 Prins also stated “the main purpose of a case definition is to identify patients who are at the tail end of the dimension fatiguing illness.” And also said “Although they differ, all case definitions select severely fatigued groups of patients.” http://www.ncbi.nlm.nih.gov/pubmed/16443043 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 75 231 CDC CFS website 2009 – “A number of illnesses have been described that have a similar spectrum of symptoms to CFS. These include fibromyalgia syndrome, myalgic encephalomyelitis, neurasthenia, multiple chemical sensitivities, and chronic mononucleosis. Although these illnesses may present with a primary symptom other than fatigue, chronic fatigue is commonly associated with all of them.” http://web.archive.org/web/20090501222433/http://www.cdc.gov/cfs/cfsbasicfacts.htm 232 Switzer WM, Jia H, Hohn O, Zheng HQ, Tang S, Shankar A, Bannert N, Simmons G, Hendry RM, Falkenberg VR, Reeves WC, Heneine W. "Absence of Evidence of Xenotropic Murine Leukemia Virus-­‐related Virus Infection in Persons with Chronic Fatigue Syndrome and Healthy Controls in the United States." in Retrovirology. 2010, July 1: http://www.retrovirology.com/content/7/1/57 233 Voice of the Patient Report from the Patient Focused Drug Development Initiative http://www.fda.gov/ForIndustry/UserFees/PrescriptionDrugUserFee/ucm368342.htm 234 Wessely S. Neurasthenia and chronic fatigue syndrome: theory and practice. Transcultural Psychiatric Review 1994;31:173-­‐209. http://www.simonwessely.com/Downloads/Publications/CFS/43.pdf 235 Brurberg, K., Fønhus, A., Larun, L., Flottorp, S., Malterud, K. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): a systematic review. BMJ Open 2014;4:e003973 doi:10.1136/bmjopen-­‐2013-­‐003973 http://bmjopen.bmj.com/content/4/2/e003973.long#T1 236 McKie, Robin. Chronic Fatigue Syndrome researchers face death threats from militants. The Guardian. August 20, 2011 http://www.theguardian.com/society/2011/aug/21/chronic-­‐fatigue-­‐syndrome-­‐myalgic-­‐encephalomyelitis This article presents the perspective of Professor Wessely but does not include the patient perspective or discussion of the justified concerns that patients have that only psychological research is being funded in Britain. For another article that includes the patient perspective see: ME Researchers “receive death threats from sufferers”, The Telegraph, July 29, 2011. http://www.telegraph.co.uk/health/healthnews/8669893/ME-­‐researchers-­‐receive-­‐death-­‐threats-­‐from-­‐ sufferers.html 237 Misdiagnosis of MS patients -­‐ http://www.prohealth.com/me-­‐cfs/library/showArticle.cfm?libid=17900&site=research Berger JR, Pocoski J, Preblick R, Boklage S. Fatigue heralding multiple sclerosis. Mult Scler. 2013 Oct;19(11):1526-­‐32. doi: 10.1177/1352458513477924. Epub 2013 Feb 25. http://www.ncbi.nlm.nih.gov/pubmed/23439577 238 Sophie Coldwell -­‐ http://swns.com/news/girl-­‐17-­‐died-­‐leukaemia-­‐10-­‐days-­‐nhs-­‐doctors-­‐dismissed-­‐illness-­‐tiredness-­‐ 33956/ and http://www.birminghammail.co.uk/lifestyle/health/tragic-­‐solihull-­‐teenager-­‐died-­‐rare-­‐2583629 239 Aslakson E, Vollmer-­‐Conna U, Reeves WC, White PD. "Replication of an Empirical Approach to Delineate the Heterogeneity of Chronic Unexplained Fatigue" Population Health Metrics. October 2009, 7:17 doi:10.1186/1478-­‐ 7954-­‐7-­‐17 http://www.pophealthmetrics.com/content/7/1/17 o “The broadening of the concept of CFS to include patients with fewer symptoms but similar disability is supported by this replication.” o "Conclusion: These data support the hypothesis that chronic medically unexplained fatigue is heterogeneous. The data do not support the current perception that CFS represents a unique homogeneous disease and suggests broader criteria may be more explanatory. o “What are the clinical implications of this work?... Future research studies should now examine for moderators of outcome that include obesity, metabolic syndrome, sleep problems, depression, and having multiple symptoms.” Note that the study reported that these were the factors associated with CFS. 240 Bernhard, T. The Stigma of Chronic Fatigue Syndrome II: Readers Respond. May 6, 2011 http://www.psychologytoday.com/blog/turning-­‐straw-­‐gold/201105/the-­‐stigma-­‐chronic-­‐fatigue-­‐ syndrome-­‐ii-­‐ readers-­‐respond Ms. Tony Bernhardt described a patient who went to the hospital because severe breathing problems. When the doctor saw the diagnosis of CFS, he rolled his eyes, ran a few tests and told him he could go home and sleep it off. When the man’s wife strenuously objected, the doctor finally agreed to do an xray, although he seemed most concerned with the expense of it. The xray showed that his lungs were full of pneuomina and he would have died if he had gone home. But that doctor saw “CFS” and decided that the patient couldn’t really be sick. 241 Dr. Allen Frances. Bad News: DSM 5 Refuses to Correct Somatic Symptom Disorder, January 16, 2013, Psychology Today. http://www.psychologytoday.com/blog/dsm5-­‐in-­‐distress/201301/bad-­‐news-­‐dsm-­‐5-­‐refuses-­‐correct-­‐somatic-­‐ symptom-­‐disorder 242 Diagnostic Ethics: Harms vs Benefits of Somatic Symptom Disorder Huffington Post, Den 16, 2013 http://www.huffingtonpost.com/allen-­‐frances/diagnostic-­‐ethics-­‐harms-­‐v_b_4450653.html Diagnostic Rights web site -­‐ http://www.diagnosticrights.org/the-­‐coalition/ 243 Diagnostic Ethics: Harms vs Benefits of Somatic Symptom Disorder Huffington Post, Den 16, 2013 http://www.huffingtonpost.com/allen-­‐frances/diagnostic-­‐ethics-­‐harms-­‐v_b_4450653.html Dr. O’Leary points out that advice from the American Association of Family Physicians “urges doctors to make early diagnoses of somatoform disorders in order to save time and to reduce costs” based on the assumption that most complaints are somatoform in nature. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 76 244 Dr. Allen Frances. Bad News: DSM 5 Refuses to Correct Somatic Symptom Disorder, January 16, 2013, Psychology Today. http://www.psychologytoday.com/blog/dsm5-­‐in-­‐distress/201301/bad-­‐news-­‐dsm-­‐5-­‐refuses-­‐correct-­‐somatic-­‐ symptom-­‐disorder • “The question naturally arises-­‐ How could DSM 5 get SSD so wrong and why is ICD 11 so likely to fall into the very same trap? It gains poignancy from the fact that the experts working on DSM 5 and ICD 11 are all very smart, highly experienced, and well meaning. The road to hell is paved with good intentions and bad unintended consequences…. “Experts always want to focus increased attention on their pet topic, want to expand its boundaries, and worry much more about missed than about mislabelled patients…. “Anyone with common sense immediately recognises that the DSM 5 and the likely ICD 11 definitions of SSD are impossibly broad and nonspecific. Such excess could be offered only by otherwise sensible experts who have lost their common sense when it comes to their own field.” 245 White PD How common is chronic fatigue syndrome; how long is a piece of string? Population Health Metrics 5:6, 2007. http://www.pophealthmetrics.com/content/5/1/6 “Our current criteria for diagnosing CFS are arbitrary, and we need to widen the net to capture all those people who become so chronically tired and unwell that they can't live their lives to their full potential.”245 246 Dr. Per Dalen “Somatic medicine abuses psychiatry — and neglects causal research” -­‐ http://www.art-­‐ bin.com/art/dalen_en.html 247 Comments on the PACE trial outcome measures and how recovery was defined are found in a number of places including the following which lists letters to the journal on the paper -­‐ • http://www.meassociation.org.uk/2013/07/pace-­‐trial-­‐letters-­‐and-­‐reply-­‐journal-­‐of-­‐psychological-­‐medicine-­‐ august-­‐2013/ • http://www.meassociation.org.uk/2013/02/me-­‐association-­‐response-­‐to-­‐pace-­‐trial-­‐recovery-­‐paper-­‐15-­‐february-­‐ 2013/ • The simplest explanation of the recovery controversy is found in this video, which reports for instance, that one of the entry criteria was 65 on the SF-­‐36 health survey scale, a scale that goes from 0 to 100 where 100 is full health. The entry criteria for the PACE trial was reported as 65, a level that is defined as abnormal. Recovery was originally slated at 85 on the SF-­‐36 scale. But the definition of recovery was changed during the trial to be 60, a level that was below the entry criteria for the trial. http://www.youtube.com/watch?v=d_7J5ELjArU&feature=youtu.be 248 White, P., Goldsmith, K., Johnson,A., Potts, L., Walwyn, R., DeCesare, J., Baber, H., Burgess, M., Clark, L., Cox, D., Bavinton, J., Angus, B., Murphy, G., Murphy, M., O’Dowd, H., Wilks, D., McCrone, P., Chalder, T., Sharpe, M. “Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomised trial.” The Lancet -­‐ 5 March 2011 ( Vol. 377, Issue 9768, Pages 823-­‐836 ) 4. PACE subscribes to the “fear avoidance theory of chronic fatigue syndrome” that “assume that the syndrome is perpetuated by reversible physiological changes of deconditioning and avoidance of activity.” 5. Study Publication -­‐ http://www.thelancet.com/journals/lancet/article/PIIS0140-­‐6736(11)60096-­‐ 2/fulltext 6. PACE Trial information -­‐ http://www.pacetrial.org/trialinfo/ § CBT Manual -­‐ http://www.pacetrial.org/docs/cbt-­‐therapist-­‐manual.pdf • Page 81 -­‐ “It is important to include the precipitating factors, e.g., illness, life-­‐events, working excessively hard, perfectionist personality etc. It is also important to discuss the maintaining factors, e.g., erratic or reduced activities, disturbed sleep patterns, unhelpful illness beliefs and any other unhelpful cognitions etc.” § GET Manual -­‐ http://www.pacetrial.org/docs/get-­‐therapist-­‐manual.pdf 249 Petersen, D. “Peterson Reports Antiviral (Vistide) Effective in Treating Herpesvirus Infected Chronic Fatigue Syndrome (ME/CFS) Patients.” April 2013. http://simmaronresearch.com/2013/04/peterson-­‐conference-­‐presentation-­‐reports-­‐ vistide-­‐cidofovir-­‐effective-­‐in-­‐treating-­‐chronic-­‐fatigue-­‐syndrome-­‐mecfs-­‐patients-­‐with-­‐hhv6-­‐and-­‐hcmv-­‐infections/ 250 Fluge and Mella have done two studies on Rituxin in CFS • Fluge, O. Mella, O. Clinical impact of B-­‐cell depletion with the anti-­‐CD20 antibody rituximab in chronic fatigue syndrome: a preliminary case series. BMC Neurology 2009, 9:28 http://www.biomedcentral.com/1471-­‐ 2377/9/28 • Fluge, O.; Bruland, O.: Risa, K.; Storstein, A.; Kristoffersen, E.; Sapkota, D.; Næss, H.; Dahl, O.; Nyland, H.; Mella, O. Benefit from B-­‐Lymphocyte Depletion Using the Anti-­‐CD20 Antibody Rituximab in Chronic Fatigue Syndrome. A Double-­‐Blind and Placebo-­‐Controlled Study. Plos One. Oct 2011. http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0026358 251 Jason, L., Najar, N., Porter, N., Reh, C. Evaluating the Centers for Disease Control’s Empirical Chronic Fatigue Syndrome Case Definition. Journal of Disability Policy Studies Oct 2008, http://dps.sagepub.com/content/20/2/93.abstract, http://www.co-­‐cure.org/Jason-­‐7.pdf • Jason noted that this “blurring of diagnostic categories” makes it harder to identify biological markers. 252 The primary clinical trials for disease modifying treatments for this disease have been on Ampligen in the U.S., Rituxan in Norway. Most of the other trials have been for behavioral treatments or for supplements. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 77 253 Jason, L., Richman, J. How Science Can Stigmatize: The Case of Chronic Fatigue Syndrome Journal of Chronic Fatigue Syndrome, Vol. 14(4),2007 http://cfids-­‐cab.org/cfs-­‐inform/CFS.case.def/jason.richman.07.txt 254 Tuller, David, Chronic Fatigue Syndrome and the CDC: A Long, Tangled Tale, November 23, 2011. http://www.virology.ws/2011/11/23/chronic-­‐fatigue-­‐syndrome-­‐and-­‐the-­‐cdc-­‐a-­‐long-­‐tangled-­‐tale/. In this article, Dr. Racaniello, Higgins Professor of Microbiology & Immunology, Mt. Sinai School of Medicine of CUNY “said that when he used to question colleagues about chronic fatigue syndrome, they would argue that it was an imaginary illness. ‘Every time I asked someone about it, they would say it doesn’t exist, it isn’t a real disease, even as recently as the past year,’ he said. ‘But once you start paying attention and reading papers, this looks like a chronic or hyper-­‐immune activation. These patients have a lot of signs that their immune systems are firing almost constantly.’” Tuller also has a second useful article on case definition. Defining an Illness Is Fodder for Debate -­‐ The New York Times www.nytimes.com/2011/03/08/health/research/08fatigue.html 255 Jason, L, Torres-­‐Harding, S, Jurgens, A, Helgerson, J. “Comparing the Fukuda et al. Criteria and the Canadian Case Definition for Chronic Fatigue Syndrome, Journal of Chronic Fatigue Syndrome, Vol 12, 2004 http://www.cfids-­‐ cab.org/cfs-­‐inform/CFS.case.def/jason.etal04.pdf • Dr. Jason of DePaul University notes that the definitional criteria has major implications for which individuals are diagnosed with CFS and how seriously the illness is viewed.” 256 Carruthers, B., van de Sande, M., De Meirleir, K., Klimas, K., Broderick, G., Mitchell, T., Staines, D., Powles, A., Speight, N., Vallings, R., Bateman, L., Baumgarten-­‐Austrheim, B., Bell, D., Carlo-­‐Stella, N., Chia, J., Darragh, A., Jo, D., Lewis, D., Light. A., Marshall-­‐Gradisbik, S., Mena, I., Mikovits, J., Miwa, K., Murovska, M., Pall, M., Stevens, S. Myalgic encephalomyelitis: International Consensus Criteria. Journal of Internal Medicine. Volume 270, Issue 4, pages 327–338, October 2011. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-­‐2796.2011.02428.x/full 257 Carruthers BM, van de Sande MI, De Meirleir KL, Klimas NG, Broderick G, Mitchell T, Staines D, Powles ACP, Speight N, Vallings R, Bateman L, Bell DS, Carlo-­‐Stella N, Chia J, Darragh A, Gerken A, Jo D, Lewis D, Light AR, Light K, Marshall-­‐ Gradisnik S, McLaren-­‐Howard J, Mena I, Miwa K, Murovska M, Steven S. Myalgic Encephalomyelitis International Consensus Primer for Medical Practitioners. 2012. http://www.hetalternatief.org/ICC primer 2012.pdf “There is a poignant need to untangle the web of confusion caused by mixing diverse and often overly inclusive patient populations in one heterogeneous, multi-­‐rubric pot called ‘chronic fatigue syndrome’. We believe this is the foremost cause of diluted and inconsistent research findings, which hinders progress, fosters skepticism, and wastes limited research monies” 258 Straus, S., Komaroff, S., Wedner, H.J. Chronic Fatigue Syndrome: Point and Counterpoint. The Journal of Infectious Diseases. Vol 170, July 1994 http://www.jstor.org/stable/30133467 “…There has been a creeping movement to include other types of medical conditions under the rubric of CFS. For example, various forms of post-­‐infectious fatigue, fibromyalgia, and non-­‐psychiatric and depressive disorders were permitted by consensus of a National Institutes of Health (NIH) workshop. Somatoform disorders and panic disorder became part of what could be encompassed within the CFS case definition. This serves to broaden the scope of the clinical entity to the point at which it is no longer definable. 259 Dr. Phillip Lee, Assistant Secretary of Health. Acceptance Speech, Rudy Perpich Award. 1998 Bi-­‐Annual Research Conference of the American Association for Chronic Fatigue Syndrome. http://www.cfids-­‐me.org/mpwc/lee.html His comments include the following • Chronic Fatigue Syndrome, Wedner tells us, is neither a disease nor a syndrome. It is a committee definition. • “The approach to CFS is now dominated by the biopsychosocial approach that gives excessive emphasis to the social, behavioral, and emotional factors in the presentation and perpetuation of symptoms. The "bio" seems to be missing. While I believe in the psychosocial determinants of health paradigm, this approach to CFS has gone too far. “ • “The problem is evidence in the proposed ICD-­‐9 codes for CFS, and the 1996 report of the Joint Working Group of the Royal Colleges of Physicians, Psychiatrists and General Practitioners on Chronic Fatigue Syndrome in the United Kingdom. The Royal Colleges convened a working group after a request from the UK's Chief Medical Officer. The group recommended that the term encephalomyelitis be dropped in the UK and that it be replaced by CFS.” • Third, the current approaches to CFS, except in a few hands, do not take sufficient cognizance of the research on brain positron emission tomography, cognitive function, possible biomarkers, electron microscopy, the evidence from past outbreaks, or a number of the studies presented here. • Finally, the overlap of symptoms with Gulf War Syndrome, fibromyalgia, and multiple chemical sensitivities merit a thorough re-­‐examination and the development of a comprehensive strategic plan for research. • “Dr. Stephen Straus of the NIH had a very different view and one that I strongly disagree with.” 260 Richman, J., Jason, L., Taylor, R., Jahn, S. Feminist Perspectives On The Social Construction Of Chronic Fatigue Syndrome, Health Care for Women International, 21:3, 173-­‐185, DOI: Oct. 2000. http://dx.doi.org/10.1080/073993300245249 261 Stress, Childhood Trauma Linked To Chronic Fatigue Syndrome In Adults, Science Daily, Nov 7, 2006. http://www.sciencedaily.com/releases/2006/11/061107082833.htm Khamsi, R. Chronic fatigue syndrome linked to stressful childhood, Nov 6, 2006 May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 78 www.newscientist.com/article/dn10454-­‐chronic-­‐fatigue-­‐syndrome-­‐linked-­‐to-­‐stressful-­‐childhood.html#. Barclay, Laurie, Childhood Trauma, Stress Linked to Adult Chronic Fatigue Syndrome. Medscape, Nov 10, 2006. http://www.medscape.org/viewarticle/547583 262 Weintraub, P. Chronic fatigue syndrome & child abuse: Disordered patients or disordered research? Are chronic fatigue patients victims of child abuse or research abuse? Psychology Today, January 13, 2009 http://www.psychologytoday.com/blog/emerging-­‐diseases/200901/chronic-­‐fatigue-­‐syndrome-­‐child-­‐abuse-­‐ disordered-­‐patients-­‐or-­‐disordered 263 Example includes http://www.abc.net.au/radionational/programs/healthreport/comparison-­‐of-­‐treatments-­‐for-­‐ chronic-­‐fatigue/2993296 http://www.psychologytoday.com/blog/sleep-­‐newzzz/201303/exercise-­‐and-­‐cbt-­‐can-­‐help-­‐chronic-­‐ fatigue/comments 264 Unity of Opposites? Chronic fatigue syndrome and the challenge of divergent perspectives in guideline development” J Neurol Neurosurg Psychiatry 2014;85:214-­‐219 doi:10.1136/jnnp-­‐2012-­‐303208. First published online Nov 17, 2012 http://jnnp.bmj.com/content/85/2/214.full, http://jnnp.bmj.com/content/early/2012/11/16/jnnp-­‐2012-­‐303208.abstract Professor Wessely is responding to the recommendation of the Scottish Health Network to adopt the Canadian Consensus Criteria for ME patients and NICE guidelines for CFS while questioning the effectiveness of CBT and GET • Professor Wessely questioned this situation as reflecting irreconcilable differences in views between objectiveness and evidence-­‐based medicine on the one hand and the subjectiveness and individual accounts of patients pointing the opposite. He stated that the Canadian Criteria had been developed in response to “patient pressure” and further went on to state: “Attempting to synthesize patient views into the discourse regarding which criteria should be used to identify patients clinically has led to dangerous criteria being adopted.” • Regarding the fact that Scotland had not endorsed CBT for ME patients, Professor Wessely stated “Again the discussion appears to refer extensively to the survey of patient groups, which are inevitably biased against those who have improved, contain heterogeneous groups of people probably with a wide variety of diagnoses, and a bias as in all self-­‐help groups towards those with poor prognosis.” • Professor Wessely asks what lies behind the failure to adopt CBT and GET and states “We cannot know this conclusively, or find out from any publicly available document. It strikes us, however, that internet searches of patient group websites and forums reveal a stream of antipsychiatry views, not only rejecting psychiatry in relation to ME/CFS, but also conducting personal attacks on those professionals who are involved in scientific research and review that come to opposing conclusions that are not aligned with these antipsychiatry views.” • Finally he states “In conclusion, these are examples of a less than helpful interaction between politics and science, and one in which the former has outweighed the latter. The issue is important; it is not an example of patients versus doctors—far from it. It is about the challenge of accurately reflecting and giving due weight to patient views in the discourse, when there is no consensus among those either. The programme of evidence-­‐based medicine is based on the premise that it is possible through reason, logic and debate to take what at first sight seems to be discordant views within the medical literature, and to follow a transparent and reproducible process seeking to understand the causes of the discrepancies, and resolve them via this methodology to arrive at conclusions. However, there seems to be no equivalent process for the other side of the process, to blend this with the views of patients, their narratives, perspectives and insights.” Dr. Malcolm Hooper has provided other examples, some of which are listed below. A longer list is available in A briefing prepared for the House of Commons Select Health Committee, Britain, December 2003. http://www.meactionuk.org.uk/SELECT_CTTEE_FINAL_VERSION.htm • Chronic fatigue syndrome: a practical guide to assessment and management. Sharpe M, Chalder T, Wessely S et al General Hospital Psychiatry 1997:19:3:185-­‐199. “Many patients receive financial benefits and payment which may be contingent upon their remaining unwell. Gradual recovery may therefore pose a threat of financial loss.” • Chronic fatigue syndrome: Symptom and Syndrome. Wessely S. Annals of Internal Medicine 2001:134: 9S:838-­‐843 “Some of the modern impetus to ‘allow’ a specific chronic fatigue syndrome arises from the various compensation and social insurance schemes operating in developed countries.”. • Doctors’Diagnoses and Patients’ Perceptions: Lessons from Chronic Fatigue Syndrome Editorial Michael Sharpe. Gen Hosp Psychiat 1998:20:335-­‐338 “The application of (a psychiatric diagnosis) may give the physician the satisfaction of having applied a label of which most of his peers would approve. The problem is that many patients not only fail to accept this diagnosis but respond to it with frank hostility.” 265 Numerous articles have criticized the DSM-­‐5 which has turned everyday experience, like bereavement into a mental health issue. Dr. Allen Frances, char of DSM-­‐IV stated “Way too much treatment is given to the normal 'worried well' who are harmed by it; far too little help is available for those who are really ill and desperately need it," Dr. Allen Frances writes in "Saving Normal." He is a retired Duke University professor who headed the psychiatry group's task force that worked on the previous handbook. May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 79 He says the new version adds new diagnoses "that would turn everyday anxiety, eccentricity, forgetting and bad eating habits into mental disorders." http://www.nydailynews.com/life-­‐style/health/shrinks-­‐critics-­‐face-­‐new-­‐psychiatric-­‐manual-­‐article-­‐ 1.1344935#ixzz2uYpU2ath 266 The report of the Group on Scientific Research into ME (The Gibson Report): www.erythos.com/gibsonenquiry/Docs/ME_Inquiry_Report.pdf The Gibson Report stated “There have been numerous cases where advisors to the DWP have also had consultancy roles in medical insurance companies. Particularly the Company UNUMProvident. Given the vested interest private medical insurance companies have in ensuring CFS/ME remain classified as a psychosocial illness there is blatant conflict of interest here. The Group find this to be an area for serious concern and recommends a full investigation of this possibility by the appropriate standards body.” It is not currently clear if that was done or what the results were. This is an area that needs additional investigation. 267 Holmes, G., Kaplan, J., Gantz, N., Komaroff, A., Schonberger, L., Straus, S. Jones, J., Dubois, R. Cunningham-­‐Rundles, C., Pahwa, S. Tosato, G., Zegans, L., Purtilo, D., Brown, N., Schooley, R. Brus, I. Chronic Fatigue Syndrome: A Working Case Definition. Holmes GP et.al. Annals of Internal Medicine. http://annals.org/article.aspx?articleid=701163, http://www.ncf-­‐net.org/patents/pdf/Holmes_Definition.pdf 268 Arpino C, Carrieri MP, Valesini G, Pizzigallo E, Rovere P, Tirelli U, Conti F, Dialmi P, Barberio A, Rusconi N, Bosco O, Lazzarin A, Saracco A, Moro ML, Vlahov D. Idiopathic chronic fatigue and chronic fatigue syndrome: a comparison of two case-­‐definitions. Ann Ist Super Sanita. 1999;35(3):435-­‐41. http://www.ncbi.nlm.nih.gov/pubmed/10721210?dopt=Abstract “In conclusion, the 1994 criteria increased the number of patients classified as CFS (compared to Holmes); however, those who fit only the 1994 criteria were less likely to have an acute symptomatic onset and signs and symptoms suggestive of an infectious process.” 269 Sharpe M, Archard L, Banatvala J., Borysiewicz, L., Clare, A., David, A., Edwards, R., Hawton, K., Lambert, H., Lane, R., McDonald, E., Mowbray, J., Pearson, D., Peto, T., Preedy, V., Smith, A., Smith, D., Taylor, D., Tyrrell, A., Wessely, S., White, P. A report—chronic fatigue syndrome. J Roy Soc Med 1991; 84: 118-­‐121. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1293107/. The criteria for the Oxford CFS are: 5. A syndrome characterized by fatigue as the principal symptom 6. A syndrome of definite onset that is not life long 7. The fatigue is severe, disabling and affects physical and mental functioning the symptom of fatigue should have been present for a minimum of 6 months during which it was present for more than 50% of the time 8. Other symptoms may be present, particularly myalgia, mood and sleep disturbance 270 Fukuda K, et al Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med 1994;121:953-­‐9. http://www.ncf-­‐net.org/patents/pdf/Fukuda_Definition.pdf 271 Jason, L, Torres-­‐Harding, S, Jurgens, A, Helgerson, J. Comparing the Fukuda et al. Criteria and the Canadian Case Definition for Chronic Fatigue Syndrome, Journal of Chronic Fatigue Syndrome, Vol 12, 2004 http://www.cfids-­‐ cab.org/cfs-­‐inform/CFS.case.def/jason.etal04.pdf. Also Jason, L. “Defining CFS: Diagnostic Criteria and Case Definition”. CFIDS association webinar, April 2010. www.cfids.org/webinar/jason-­‐slides041410.pdf slide 12 where he describes how fatigue plus 4 Fukuda symptoms are equivalent to the symptoms of depressed patients 272 Carruthers, B., et al Jain, A., De Meirleir, K., Peterson, D., Klimas, N., Lerner, M., Bested, A., Flor-­‐Henry, P., Joshi, P., Powles, A. , Sherkey, J., van de Sande, M. Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols. Journal of Chronic Fatigue Syndrome, Vol. 11(1) 2003. http://mefmaction.com/images/stories/Medical/ME-­‐CFS-­‐Consensus-­‐Document.pdf 273 Reeves, W., Wagner, D., Nisenbaum, R., Jones, J., Gurbaxani, B., Solomon, L., Papanicolaou, D., Unger, E., Vernon, S., Heim, C. Chronic Fatigue Syndrome – A clinically empirical approach to its definition and study. BMC Medicine 2005, 3:19 http://www.biomedcentral.com/1741-­‐7015/3/19 274 Jason, L., Najar, N., Porter, N., Reh, C. Evaluating the Centers for Disease Control’s Empirical Chronic Fatigue Syndrome Case Definition. Journal of Disability Policy Studies Oct 2008 http://www.co-­‐cure.org/Jason-­‐7.pdf 275 Jason L, Jordan K, Miike T, Bell DS, Lapp C, Torres-­‐Harding S., Rowe, K., Gurwitt, A., DeMeirleir, K., Van Hoof, E. A Pediatric Case Definition for Myalgic Encephalomyelitis and Chronic Fatigue Syndrome. J Chronic Fatigue Syndr. 2006 13: 1-­‐44 http://www.cfids-­‐cab.org/MESA/Jason-­‐1a.pdf 276 Chronic fatigue syndrome / Myalgic encephalomyelitis (or encephalopathy); diagnosis and management. National Institute for Health and Clinical Excellence. 2007. http://www.nice.org.uk/CG53 277 Carruthers, B., van de Sande, M., De Meirleir, K., Klimas, N., Broderick, G. Mitchell, T., Staines, D., Powles, P., Speight, N., Vallings, R., Bateman, L., Baumgarten-­‐Austrheim, B., Bell, D., Carlo-­‐Stella, N., Chia, J., Darragh, A., Jo, D., Lewis, D., Light, A., Marshall-­‐Gradisbik, S., Mena, I., Mikovits, J., Miwa, K., Murovska, M., Pall, M., Stevens, S. Myalgic encephalomyelitis: May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 80 International Consensus Criteria. Journal of Internal Medicine. Volume 270, Issue 4, pages 327–338, October 2011. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-­‐2796.2011.02428.x/full 278 U.S. Census quick facts, 2012. http://quickfacts.census.gov/qfd/states/00000.html May 12, 2014 Chronic Fatigue Syndrome: How to Make a Disease Evaporate Page 81