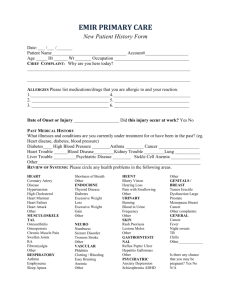
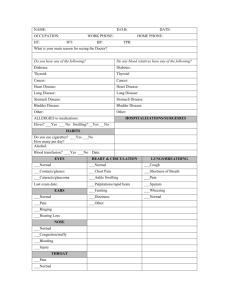
Nursing/Teaching Exam Medical History form --- Current medications: ___________________________________________________________
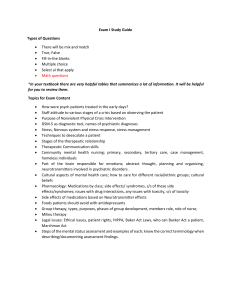
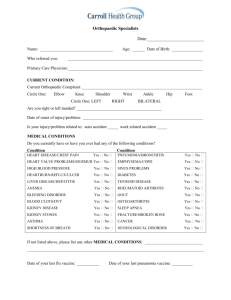
advertisement

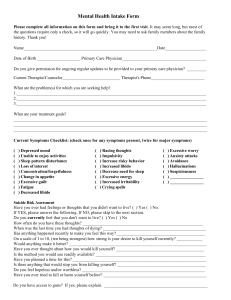
Nursing/Teaching Exam Medical History form --- to be completed by student Age: _____ Sex: M F Allergies to medications: _____________________________ Current medications: ___________________________________________________________ Current medical illness being treated: _____________________________________________ Do you have any concerns about your ability to function in clinical nursing/teaching? Y N Past hospitalizations (year/reason) _______________________________________________ Past treatment for illnesses (diabetes, thyroid, heart murmur, depression, eating disorder, other______________________________________________________________________ Social History Do you smoke cigarettes? Y N Packs per day: Use other tobacco products? Y N Do you drink alcohol? Y N Drinks/week average: Do you use recreational drugs? Y N Do you ever drink and drive or ride with people who drink and drive? Y N Do you wear seat belts? Y N Do you exercise? Y N Number sessions/week: Family History: Have immediate relatives (parents, brothers, sisters) had? Y N Relationship Y N Relationship Type High Blood Pressure Stroke Heart Attack age <50 Diabetes Cancer Thyroid disease Blood clotting disorder Psychiatric illness REVIEW OF SYSTEMS: Have you had during the last year: (CIRCLE any that apply) General: unexplained weight changes, unusual fatigue, fever, chills, sweats at night Skin: changes in existing moles, new moles, poorly healing wounds, rashes Eyes/Ears: blurred vision, double vision, loss of hearing Cardiac: chest pain, racing or irregular heart beat Lungs: cough, wheezing, shortness of breath with activity Gastrointestinal: diarrhea, constipation, change in bowel habits, blood in stool, dark black stools, abdominal pain Genitourinary: pain with urination, blood in urine, frequent bladder infections abnormal vaginal bleeding or discharge Last period _______________ Breasts: breast lump, nipple discharge, pain in breast Musculoskeletal: unusual muscle or joint pain, anything that limits your activity Neurologic: frequent headaches, fainting, blackouts, seizures, weakness, tingling, tremors Psychiatric: depression, unusual anxiety, history of taking psychiatric medications (name of meds with approximate dates taken) Student signature _____________________________________Date _______________ 5/04