RADIOLOGICAL CASES SEPTEMBER 2013 PRESENTED BY:
advertisement

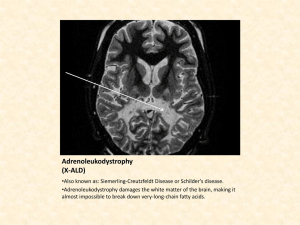
RADIOLOGICAL CASES SEPTEMBER 2013 PRESENTED BY: DR. PATRICK A. CHUI WAN CHEONG Jr. OSK DMRD FRCR CASE 1 • 38 year old female with sudden onset of altered consciousness, neurological deficit and headache. DIAGNOSIS? TUBERCULOSIS CNS manifestation of TB • TB incidence was in decline but has risen since 1986. • AIDS epidemic – 30 % of TB patients are HIV positive. Aetiology: Mycobacterium Tuberculosis. Other types eg Avium rarely affects the CNS. CNS involvement : 2 – 5% of all patients with TB. 10% of patient with AIDS related TB. Manifestations: i. Tuberculous granulomas (tuberculomas) - brain and spinal cord. ii. TB abscess. iii. Meningitis. iv. Epidural abscess from osteomyelitis or spondylodiscitis. Pathophysiology: Hematogenous spread from a pulmonary source – Grey white matter junction to form a granuloma. Abscess formation rare but more common in immunocompromised patients. TB meningitis can occur when i. A subependymal or subpial focus ruptures into the CSF. ii. Direct penetration of the walls of the meningeal vessels by hematogenous spread. Clinical presentation: Meningitis : Headache / Malaise / Low grade fever. Late complications : Neuropathy and hydrocephalus. Tuberculomas: Focal neurological deficits and seizures. CSF examination often shows striking low glucose levels in TB meningitis. Imaging findings: Tuberculoma – 4 Stages i. Cerebritis stage: Non-specific oedema. Ill-defined enhancement. ii. Solid granulomatous stage : Enhancing nodules +/- perilesional oedema. iii. Central caseation stage : Central hypointensity on MR T2 WI. iv. Involution stage: Shows calcified nodules on CT. Cerebritis Caseating tuberculoma. Axial T2W MR image(a) of brain shows profoundly hypointense lesion in left frontal lobe(black arrow) with marked perilesional oedema. The lesion demonstrates isointense core with slight hyperintense rim on T1W image(b), and thin peripheral ring enhancement on gadolinium‐enhanced image(c). Note similar lesion in left occipito‐parietal region(white arrow). Tuberculous abscess Usually larger than a tuberculoma – multiloculated – more perilesional oedema. May be undistinguishable from a typical bacterial abscess. Tubercular abscess in the right basal ganglia. A well‐defined hyperintense lesion is seen with a hypointense wall on axial T2‐weighted image (A). Lesion shows ring enhancement on post‐contrast T1‐weighted image (B). On axial T2‐weighted sequence, it has central hyperintense signal corresponding to the pus cavity and the characteristic surrounding T2 hypointense signal of the abscess capsule (white arrow). Local mass effect results in entrapment of the adjacent mildly dilated right temporal horn. Axial T1 postcontrast sequence demonstrates typical smooth ring enhancement of a mature abscess TB meningitis: i. Typically causes a thick basilar exudate associated with meningeal enhancement. ii. Communicating hydrocephalus and iii. Infarctions in the territories of the perforator vessels. WIDESPREAD GYRIFORM ENHANCEMENT Differential diagnosis: Infection – Viral, Bacterial, Tuberculous. Neoplasm – Primary or Secondary - more perilesional oedema. Sarcoidosis (rare). Focal gyriform enhancement – AVM, Infarction, Encephalitis, Glioma. Treatment for TB Multidrug treatment regime. Serial imaging is useful to assess response to therapy. Prognosis: Mortality up to 30 % in non HIV and up to 80% in HIV + CASE 2 16 year old girl with minor trauma to the elbow. DIAGNOSIS ? OSTEOPOIKILOSIS OSTEOPOIKILOSIS Sclerosing bony dysplasia with multiple enostoses. Rare inherited benign condition. Found incidentally on skeletal x rays. Correct diagnosis important. Not to be mistaken for pathology. OSTEOPOIKILOSIS Epidemiology The bone islands develop during childhood. They do not regress and hence seen in all age groups. No gender predilection. Autosomal dominant disorder. OSTEOPOIKILOSIS Clinical presentation Asymptomatic / Incidental finding. No malignant change. Bone strength is normal. RADIOGRAPHIC FEATURES Plain film and CT The bone islands of osteopoikilosis are typically clustered around joints and align themselves parallel to surrounding trabeculae (thus predominantly longitudinally in the metaphyses). Most lesions are found in the appendicular skeleton and pelvis. The axial skeleton is largely spared. The lesions vary in size, usually a 5 - 10mm, but ranging from only 1 2mm up to 1 - 2cm. MRI Appearances on MRI are the same as individual bone islands. Each lesion is small and dark on both T1 and T2 weighted images, as it is composed of mature dense bone. Bone scintigraphy Bone scan should not demonstrate any increase in uptake. Useful if metastatic disease is considered in the differential. Osteopoikilosis is one of the skeletal "DON’T TOUCH” lesions. Differential diagnosis: Appearances are characteristic. Few differentials. When only a few lesions are seen on an isolated film, the differential includes: incidental bone islands (enostoses) other sclerosing bony dysplasias sclerotic metastases osteosarcoma lymphoma osteoid osteoma: only rarely multiple chronic multifocal sclerosing osteomyelitis CASE 3 • 14 year old boy with progressive paraparesis and gradual decline in intellectual function. ADRENOLEUKODYSTROPHY SPECTRUM OF WHITE MATTER DISEASES (LEUKODYSTROPHIES) Caused by pathology of myelin and/or oligodendrocyte. Either inherited (demyelination). (dysmyelination) or acquired WHITE MATTER DISEASES Dysmyelination - Formation of intrinsically abnormal myelin, resulting in poor myelination or early myelin degeneration. Demyelination - Destruction of normal myelin with relative axonal preservation. ACQUIRED LEUKODYSTROPHIES INFLAMMATORY Multiple sclerosis and variants Acute disseminated encephalomyelitis (ADEM) Acute hemorrhagic encephalomyelitis INFECTIONS Progressive Multifocal Leukoencephalopathy (PML) Lyme disease ‐ tick borne disease AIDS encephalopathy Creutzfeldt‐Jakob disease METABOLIC Central pontine myelinolysis Malnutrition Vitamin B12 deficiency VASCULAR Ageing changes affecting the white matter Hypertensive encephalopathy Hypoxic‐ischemic edema TRAUMA HEREDITARY LEUKODYSTROPHIES LYSOSOMAL DISORDERS Metachromatic leukodystrophy Krabbe’s leukodystrophy PEROXISOMAL DISORDERS Adrenoleukodystrophy Zellweger cerebrohepatorenal syndrome Alpers’ disease AMINO‐ACID AND ORGANIC ACID METABOLIC DISORDERS Canavan disease Maple syrup urine disease WHITE MATTER DISEASE OF UNKNOWN METABOLIC DEFECT Pelizaeus‐Merzbacher disease Alexander’s disease Congenital muscular dystrophy. ADRENOLEUKODYSTROPHY Encompasses two genetic disorders causing varying degrees of malfunction of the adrenal cortex and CNS myelin. Characterized by elevated levels of very long chain fatty acids. Uncommon and exclusively in males. Characterized by dysmyelination in the CNS. Hallmark is impaired Beta oxidation of the VLCFA’s. ADRENOLEUKODYSTROPHY Diagnosis: Typical clinical presentation. Presence of elevated blood levels of the VLCFA’s. Aetiology Defect in a peroxisomal enzyme involved in the breakdown of the VLCFA’s in the CNS, adrenal cortex and testes. Gene for this disorder has been mapped to Xq28. ADRENOLEUKODYSTROPHY Clinical findings: Typically presents between ages 5 to 10. Gait disturbances. Intellectual impairment. Adrenal insufficiency is present in 90% of cases. There may be a delayed presentation with onset of symptoms in adolescence and adulthood – referred to as adrenomyeloneuropathy (AMN). Adult type: Progressive paraparesis and sphincter disturbances and 66% have adrenal insufficiency. MALE ALD PHENOTYPE DESCRIPTION ONSET RELATIVE FREQUENCY Childhood cerebral Progressive neurodegenerative decline, leading to vegetative state without treatment. 3-10 years 31-35 % Adolescent Similar to childhood cerebral, slower onset 11-21 years 4-7 % Adrenomyeloneuropathy (AMN) Progressive neuropathy, Paraparesis, about 40 % progress to cerebral involvement. 21-37 years 40-46 % Adult cerebral Dementia, behavioural disturbances Adulthood 1-2 % Asymptomatic No clinical presentation. Further studies may reveal subclinical adrenal insufficiency. Most common < 4 years Addison Disease only Adrenal insufficiency <7.5 yrs Up to 50 % in childhood. Varies with age. ADRENOLEUKODYSTROPHY Complications: Hypotonia Seizures Visual changes Dysphagia Deafness Progressive dementia Death occurs 1 to 10 years from onset of symptoms ADRENOLEUKODYSTROPHY CT low attenuation in the occipital white matter with involvement of the splenium of the corpus callosum. +/- dystrophic calcification. ADRENOLEUKODYSTROPHY MRI Symmetric prolongation of T1 and T2 WI in the occipital white matter and splenium. Involvement of the retrolenticular portion of the posterior limb of the internal capsule is often contiguous. Involvement of the frontal white matter as disease progresses. T2 prolongation involving the corticospinal tracts in the pons and medulla. Auditory pathways involved. Post Gd – enhancement of the leading edge of active demyelination. Inferior colliculus involvement Lateral lemniscus involvement ADRENOLEUKODYSTROPHY Treatment: Immunosuppression to modify the inflammatory response. Dietary therapy with specific fatty acids but is controversial. Bone marrow transplantation may arrest progression of disease. Adrenal hormone replacement therapy usually required. Prognosis: Classic X-linked ALD – poor prognosis with relentless progression to death. Adrenomyeloneuropathy has a much more favorable prognosis. CASES 4 CAUSES OF PSOAS MUSCLE ABSCESSES Primary cause: As a result of hematogenous spread of an infectious process. Primary psoas muscle abscess can occur in patients with: Diabetes mellitus IVDA AIDS renal failure Immunosuppression Secondary cause: Spread of infection from gastrointestinal disease (e.g. appendicitis, diverticulitis, Crohn’s disease or perforated colon carcinoma). Renal disease is the second most common source. THANK YOU