AUTHOR QUERY FORM
advertisement

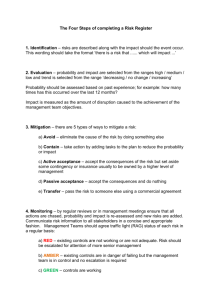
427770 BMO AUTHOR QUERY FORM Journal title: BMOD Article Number: 427770 Dear Author/Editor, Greetings, and thank you for publishing with SAGE. Your article has been copyedited, and we have a few queries for you. Please respond to these queries when you submit your changes to the Production Editor. Thank you for your time and effort. Please assist us by clarifying the following queries: No Query 1 Please check whether the inserted affiliations are correct. 2 Please provide complete reference details for “Lillis and colleagues, 2009” or allow us to delete the citation. 3 Please provide expansion for “SSI.” 4 Please provide expansion for “LEARN,” if required. 5 The sentence beginning “Items are rated on a 5-point Likert . . . ” seems little unclear. Please check. 6 Please provide complete reference details for “Juarascio, Forman, Timko, Butryn, & Goodwin, in press” or allow us to delete the citation. 7 Please provide complete reference details for “Butler, Furber, Phongsavan, Mark, & Bauman, 2009” and “Chang, Hendricks, Slawksy, &Locastro, 2004” or allow us to delete the citation. 8 Please confirm whether the given conflicts of interest statement is accurate and correct. 9 Please confirm whether the given funding statement is accurate and correct. 10 Please provide complete reference details for “Dunlop, Cortina, Vaslow, & Burke, 1996” or allow us to delete the citation. 11 Please provide place of publication for the reference “American Heart Association, 2009b.” 12 Please update the reference “Moitra et al., in press.” 13 Please provide publisher details for the reference “National Cancer Institute, 2010.” XXX10.1177/0145445511427770Goodwin et al.Behavior Modification A Pilot Study Examining the Initial Effectiveness of a Brief AcceptanceBased Behavior Therapy for Modifying Diet and Physical Activity Among Cardiac Patients Behavior Modification XX(X) 1–19 © The Author(s) 2011 Reprints and permission: sagepub.com/journalsPermissions.nav DOI: 10.1177/0145445511427770 http://bmo.sagepub.com Christina L. Goodwin1,2, Evan M. Forman1, James D. Herbert1, Meghan L. Butryn1, and Gary S. Ledley1 Abstract Approximately 90% of cardiac events are attributable to a small number of modifiable behavioral risk factors that, if changed, can greatly decrease morbidity and mortality. However, few at-risk individuals make recommended behavioral changes, including those who receive formal interventions designed to facilitate healthy behavior. Given evidence for the potential of specific psychological factors inherent in acceptance-based behavior therapy (ABBT; that is, intolerance of discomfort, mindfulness, and values clarity) to impact health behavior change, the authors evaluated the feasibility and 1 Drexel University, Philadelphia, PA, USA Ohio State University, Columbus, USA [AQ: 1] 2 Corresponding Author: Christina L. Goodwin, The Ohio State University, 169 Psychology Building, 1835 Neil Avenue, Columbus, OH 43210, USA Email: Christina.L.Goodwin@gmail.com 2 Behavior Modification XX(X) initial effectiveness of an ABBT pilot program designed to increase adherence to behavioral recommendations among cardiac patients. Participants (N ! 16) were enrolled in four, 90-min group sessions focused on developing mindfulness and distress tolerance skills, and strengthening commitment to health-related behavior change. Participants reported high treatment satisfaction and comprehension and made positive changes in diet and physical activity. This was the first evaluation of an ABBT program aimed at increasing heart-healthy behaviors among cardiac patients. Keywords acceptance-based, diet, physical activity, cardiac patients Cardiovascular disease (CVD) is the leading cause of death in the United States and costs Americans nearly US$276 billion annually in direct and indirect costs. CVD poses great risks in terms of morbidity and mortality; survivors of an acute heart attack have a risk of illness or death approximately 15 times higher than the general population (American Heart Association [AHA], 2009b; Cobb, Brown, & Davis, 2006). Importantly, the vast majority of heart disease patients have at least one modifiable physiologic (e.g., obesity, hypertension, hypercholesteremia) or behavioral (e.g., high-calorie, high-fat, and high-sodium diet; insufficient physical activity; and smoking) risk factor, which if changed results in markedly decreased mortality and morbidity (Cobb et al., 2006; Ornish et al., 1990; Ornish et al., 1998). However, relatively few individuals who have been diagnosed with CVD or experienced an acute cardiovascular event (e.g., a heart attack) make recommended behavioral changes (Cobb et al., 2006; Dorneleas, 2008). A number of cardiac lifestyle interventions have been developed in response to the difficulty in making and maintaining behavioral changes in diet, physical activity, and smoking. Unfortunately, these interventions tend to be minimally successful in the long-term modification of these behaviors (Bennett & Carroll, 1994; Bolman, de Vries, & van Breukelen, 2002; Dorneleas, Sampson, Gray, Waters, & Thompson, 2000; Hajek, Taylor, & Mills, 2002; Rigotti, McKool, & Shiffman, 1994). Programs that are more successful are also more likely to be time and resource intensive (e.g., involving the relocation of patients for long periods of time; Billings, Scherwitz, Sullivan, & Sparler, 1996; Jiang, Sit, & Wong, 2007; Lisspers et al., 1999; Pischke, Scherwitz, Weidner, & Ornish, 2008; Sundin et al., 2003). In addition, the majority of interventions limit their focus to a single behavioral target, the most popular being exercise-based cardiac rehabilitation. Yet, most Goodwin et al. 3 cardiac patients have multiple behavioral risk factors (Cobb et al., 2006); therefore, even if these single-focus programs are successful (and they are not for most patients), they are not impacting other critical lifestyle behaviors that are important in cardiac rehabilitation. In addition, factors such as low socioeconomic status (SES) increase the likelihood that individuals will not adhere to healthy lifestyles. Smoking, obesity, and sedentariness are all more prevalent among lowSES (specifically low educated) individuals, and better health outcomes are reported for high-SES individuals with numerous health conditions (Cutler & Lleras-Muney, 2008; Illsley & Baker, 1991). While no single variable can explain the relationship between SES and health behaviors, it has been suggested that low-SES individuals are less likely to invest in their future health and are more focused on their present circumstances (Becker & Murphy, 1988; Cutler & Lleras-Muney, 2008). Psychological Explanations for Difficulty of Lifestyle Change On the whole, insufficient attention has been paid to the psychological factors that make it difficult to achieve and sustain a heart-healthy lifestyle. One construct that is increasingly invoked to explain maladaptive behavior, including health behavior, is distress tolerance. Distress tolerance, which is closely related to the construct of psychological acceptance, is defined as the extent to which individuals fully accept (vs. attempt to suppress or avoid) difficult internal experiences, that is, thoughts, emotions, physiological sensations, and urges (Forman & Herbert, 2009; Hayes, Strosahl, & Wilson, 1999). For example, difficulty giving up smoking and smoking cessation relapse, particularly, has been linked to lower levels of distress tolerance (Brown, Lejuez, Kahler, & Strong, 2002; Brown, Lejuez, Kahler, Strong, & Zvolensky, 2005). More recently, it has been proposed that adhering to a low-calorie diet and sustaining physical activity also requires the ability to psychologically accept difficult internal experiences such as food cravings, feelings of deprivation, and physical discomfort (Butryn, Forman, Hoffman, Shaw, & Juarascio, 2011; Falk, Bisogni, & Sobal, 2000; Forman, Butryn, Hoffman, & Herbert, 2009; Forman et al., 2010). Hayes and colleagues (Hayes et al., 1999; Hayes & Wilson, 1994) have argued that defusion (i.e., the ability to psychologically step back from thought and feelings and to see them for what they are) and values clarity (i.e., a clear and present awareness of one’s personal values) facilitate commitment to desired behaviors in the face of the aversive internal 4 Behavior Modification XX(X) experiences that they engender. The aforementioned constructs are found within acceptance-based behavioral treatments (ABBT). Promise of Acceptance-Based Health Behavior Interventions ABBT such as acceptance and commitment therapy (ACT; Hayes, Strosahl, & Wilson, 2002; Hayes & Wilson, 1994) focus on maximizing psychological flexibility, that is, the ability to choose one’s behaviors regardless of the internal distress they engender. These interventions may therefore be especially well suited to the challenge of health behavior change, including the adoption and maintenance of heart-healthy lifestyle behaviors. Unlike other psychological interventions that aim to modify or reduce negatively evaluated thoughts and feelings, ACT promotes mindful acceptance of one’s feelings and thoughts (e.g., discomfort felt while exercising) while engaging in activities in line with one’s values (e.g., increased physical activity). Various studies support the connection between these psychological constructs and health behavior change. For example, Lillis and colleagues (2009) [AQ: 2]reported that change in acceptance-based coping and psychological flexibility mediated the impact of an ACT workshop on weight maintenance among those who had completed a weight loss program. Moreover, Forman et al. (2009) reported that increases in acceptance-based psychological variables were associated with weight loss after the delivery of an open trial of ABBT for weight loss. Significant improvements in behavior have been observed in ABBT interventions for increasing physical activity (Butryn et al., 2011), increasing medical adherence in diabetes patients (Gregg, Callaghan, Hayes, & Glenn-Lawson, 2007), fostering adherence to highly active antiretroviral therapy in patients with HIV disease (Moitra, Herbert, & Forman, in press), and for smoking cessation (Gifford et al., 2004). Collectively, these ABBT studies demonstrate changes in important behaviors by increasing levels of mindfulness and distress tolerance among participants. Current Study Given preliminary evidence that ABBT programs have been shown to improve diet, physical activity level, and smoking, it seems that an acceptance-based intervention has high potential for improving adherence to hearthealthy living in a cardiac population. However, there are no previous studies evaluating the ability of ABBT to effect change in a cardiac population. The Goodwin et al. 5 present pilot study aimed to test the feasibility, acceptability, and preliminary effectiveness of an ABBT program, delivered in a brief four-session intervention, to increase cardiac patients’ adherence to a heart-healthy lifestyle. In addition, we sought to gather preliminary evidence regarding potential mechanisms of action of this intervention, including mindfulness, distress tolerance, and values clarity. The current study was designed to evaluate the following hypotheses: Hypothesis 1: Participants would report the intervention to be satisfactory. Hypothesis 2: The intervention would increase levels of mindfulness, distress tolerance, and values clarity from pre- to postintervention. Hypothesis 3: The intervention would improve participant adherence to a heart-healthy lifestyle (increased physical activity; decreased caloric, fat, and sodium intake). Hypothesis 4: Change in psychological variables would be associated with change in outcome variables (caloric, sodium, and fat intake; physical activity; weight). Method Participants Patients (N ! 16) were recruited from the outpatient cardiac care unit of a major academic medical center in the Northeastern United States, which serves a predominately ethnic minority, low-SES population. Patients were referred by their cardiologists and/or were approached by study staff during clinic visits. Inclusion criteria reflected high risk for developing coronary artery disease and included (a) current diagnosis of acute coronary syndrome (ACS; that is, experienced a myocardial infarction or have unstable angina) or overweight (body mass index [BMI] "25) with a current diagnosis of hypertension or diabetes, (b) between the ages of 18 and 75, and (c) fluency in written and spoken English. Exclusion criteria were legally blind or deaf, or unable to fully participate in the group due to psychiatric (e.g., schizophrenia, delusions), cognitive (e.g., dementia), or substance abuse–related impairment. As shown in Table 1, the majority of participants were African American women, and a majority carried a diagnosis of hypertension or ACS. Only one participant reported current cigarette use. 6 Behavior Modification XX(X) Table 1. Demographic Data % Gender Male Female Ethnicity African American Asian Caucasian Haitian Hispanic Employment Full-time Part-time Occasional Disability/SSI No income Retired Relationship status Single (no current romantic partner) Divorced Widowed Married/living with partner Not living with current partner Cardiac risk factora Acute coronary syndrome Diabetes # obesity Hypertension # obesity High cholesterol # obesity 31.3 68.8 56.3 0.0 31.3 6.3 6.3 43.8 12.5 0.0 25.0 0.0 18.8 12.5 6.3 12.5 56.3 12.5 62.5 37.5 68.8 37.5 a Participants may have multiple risk factors. [AQ: 3] Procedure Eligible participants provided informed consent and were invited to participate in four, 90-min group therapy sessions. Participants received US$20 for completing all assessments. The interventionists were graduate students in clinical psychology and used a four-session intervention manual created by the authors to increase heart-healthy behaviors, as described below. Each group consisted of one to five group members and two interventionists. Goodwin et al. 7 The intervention manual was borrowed from (a) Brownell’s LEARN [AQ: 4]manual for weight loss (Brownell, 2000), (b) Forman and colleagues’ ABBT intervention for weight loss (Forman et al., 2010), and (c) educational material from the AHA (2009a). The aim of the intervention was increasing positive behavior change in diet and physical activity by enhancing psychological acceptance, values clarity, and ongoing commitment to engage in heart-healthy-related valued behavior even in the face of aversive internal experiences. The intervention was divided into three components, described below and outlined in Table 2. Psychoeducation. Psychoeducation involved teaching cardiac-specific nutritional, dietary, and physical activity information, and behavioral methods for modifying diet and physical activity levels. Participants were provided with specific behavioral techniques for adhering to a heart-healthy lifestyle (e.g., time management and assertiveness; brisk walking schedules; low-calorie, low-fat recipes; cooking methods to decrease calories). Cultural customization of lifestyle behaviors was considered and discussed as needed (e.g., modification of traditional foods, caregiver roles in multigenerational homes). In addition, group problem solving was used on a weekly basis to address difficulties in attaining assigned heart-healthy goals. Mindfulness and distress tolerance (willingness). Participants were asked to discuss previous methods for attaining weight loss and exercise goals. Experiences from their previous attempts to adopt a heart-healthy lifestyle were used to help participants identify control-based strategies (e.g., distraction from thoughts, attempts to change feelings about exercising) as ineffective, to provide them with motivation to try an acceptance-based approach. A rationale for accepting previously avoided internal experiences was presented through the use of metaphors and experiential exercises. In addition, participants monitored their weekly goals and their willingness to experience distressing thoughts and feelings related to lifestyle changes. To increase distress tolerance, participants were encouraged to recognize that distress associated with physical activity and healthy eating (e.g., physical and mental discomfort, urges to stop exercising) is normal, and often cannot readily be suppressed or controlled without producing even more distress. In addition, strategies to promote defusion (i.e., distancing from unhelpful thoughts, feelings, or beliefs) were used to promote contact with the present moment. Participants were taught to use defusion to increase their ability to experience thoughts, feelings, and sensations in the context of their individual goal-/value-driven behaviors. Participants were taught that increasing their willingness to experience distressing internal states increases their ability to engage in difficult behavior change (such as adopting heart-healthy behaviors). 8 Behavior Modification XX(X) Table 2. Summary of Treatment Components Session 1 2 3 Behavioral components Introductions Problems with living healthily Heart-healthy living (calories, serving sizes, fat grams, sodium, physical activity) Relationship between goals and cardiac health Barriers to being active How to keep food record Home assignment Review of nutritional information and concepts discussed last week Review of behavioral home assignment Continue nutritional information Healthy eating out and eating in Eating and activity cues Home assignment Review of home assignment and concepts discussed last week Discussion of “How you eat” Strategies to slow down eating Home assignment 4 Review of home assignment and concepts discussed last week Urge surfing Lapse and relapse prevention Closing of the program ABBT components Creative hopelessness Limitations of control strategies Acceptance as an alternative to control Willingness Willingness cues Values and goals Relating values to ACT-themes Continued acceptance and willingness Defusion to increase willingness Mindless eating Mindful eating strategies Distress tolerance Note: ABBT ! acceptance-based behavioral treatments; ACT ! acceptance and commitment therapy. Committed action/values and goals. Interventionists helped participants clarify their values and define their goals. Participants listed 10 reasons why they value living heart-healthily to facilitate a discussion of value-driven behaviors. Goodwin et al. 9 Potential barriers (psychological and environmental) to reaching individual goals and living consistently with values were also discussed. Treatment Fidelity To increase treatment fidelity and consistency, the intervention followed a highly structured treatment manual, which included the timing and duration of each intervention subcomponent. Interventionists were supervised by licensed clinical psychologists (M.L.B., E.M.F., and J.D.H.) and were provided with immediate feedback about any potential deviations from the intended intervention. Measures Participants completed all assessments before Session 1 and after Session 4, with the exception of the acceptability and comprehension questionnaires, which were completed only at posttreatment. Demographics and a brief medical history were also completed by participants. In addition, height and weight were assessed using a stadiometer and a medical-grade scale. Physical activity and diet. Participants were instructed to track their diet and physical activity levels using self-report measures. Physical activity was assessed using the International Physical Activity Questionnaire, which measures physical activity across several life domains. The automated selfadministered 24-hr dietary recall (ASA-24) was used to assist patients in reporting dietary intake on two weekdays and one weekend day. The ASA-24 was designed by the National Cancer Institute and is based on the Automated Multiple Pass Method, which is reported to result in less food intake underreporting than other methods as well as high validity and reliability (National Cancer Institute, 2010).The ASA-24 enables self-administered, interactive, 24-hr dietary recalls. Mindful awareness and psychological acceptance. The Philadelphia Mindfulness Scale (PHLMS; Cardaciotto, Herbert, Forman, Moitra, & Farrow, 2008) is a self-report measure of mindfulness, consisting of Mindful Awareness and Psychological Acceptance subscales. Items are rated on a 5-point Likert-type scale according to the frequency each item was experienced during the past week [AQ: 5]. Very good internal consistency has been demonstrated (awareness subscale α ! .85; acceptance subscale α ! .87). Higher scores indicate greater mindfulness (Cardaciotto et al., 2008). Physical activity– specific and food-specific psychological acceptance questionnaires were also used. The Physical Activity Acceptance and Action Questionnaire 10 Behavior Modification XX(X) (PA-AAQ) measures the degree to which a person avoids exercise-related internal experiences and has a Cronbach’s alpha of .79 (Forman et al., 2009). The Food Acceptance and Action Questionnaire (FAAQ) measures the degree to which a person avoids food-related internal experiences and has a Cronbach’s alpha of .68 (Juarascio, Forman, Timko, Butryn, & Goodwin, in press).[AQ: 6] Defusion from negative experiences. The Drexel Defusion Scale (DDS) is a 10-item scale that assesses the degree of psychological distance from various negative thoughts and feelings. Higher scores indicate greater ability to defuse from internal experiences (Cronbach’s α ! .83; Forman, Herbert, Moitra, Yoemans, & Geller, 2007). Values and goals clarity. As existing measures tapped strength of values for various life domains, and not values clarity, a values and goals clarity measure was created for this study. Participants provided a definition of a “value” and were asked to respond in writing to the open-ended question, “What are the values by which you live your life?” Responses (de-identified) were scored by two interventionists. Responses were coded as 0 (no defined goals/ values or a single-word answer such as “God” or “Retire”), 1 (broad goals or values, for example, further education), 2 (specific goals or values but also listed items that were not goals/values), or 3 (well-defined goals or values). Interrater reliability of this measure was 92.9%. Treatment satisfaction and comprehensibility. Participants answered the following two satisfaction questions on a 5-point Likert-type scale (1 ! not at all, 5 ! very): “How helpful did you find the strategies (e.g., acceptance, willingness, and defusion) for responding to urges or desires pushing you to make unhealthy choices regarding diet, physical activity, and smoking?” and “How satisfied were you with the approach we used to help you make changes in your diet, physical activity level, and smoking behavior?”. Self-reported comprehensibility was measured using a 5-point Likert-type scale (1 ! very difficult and 5 ! not at all difficult) rating how difficult they felt it was to comprehend the constructs of acceptance, mindfulness, willingness, defusion, and values individually. Higher scores indicate less difficulty/greater comprehension. A posttreatment quiz measured comprehension more objectively. Participants were presented five treatment concepts (acceptance, mindfulness, willingness, defusion, and values) and asked to explain each of them in their own words. Responses were graded (blindly) by an interventionist on a 0 (no correct content) to 20 (fully correct response) scale with specific anchor points (e.g., 10 ! described metaphors used in session without a construct definition). Goodwin et al. 11 Statistics Given the pilot nature of the data and the low statistical power, effect sizes1 are reported for all statistics. Results Participants Participant ages ranged from 32 to 73 years (M ! 56.42, SD ! 12.72). Overall, participants reported an unhealthy lifestyle at baseline, with nontreatment completers reporting less healthy lifestyles; see Table 3 for descriptive statistics of baseline measures. Retention, Acceptability, and Comprehension All analyses are computed for treatment completers (n ! 12). Due to the lack of posttreatment data for noncompleters (n ! 4) and the small sample size, treatment completers are defined as having attended all four sessions. Based on inspection of descriptive data, the four participants who discontinued treatment had a higher mean BMI, had a less healthy lifestyle, and were less psychologically minded than those who completed treatment. Participants judged the program strategies to be highly satisfactory, based on their high ratings of treatment helpfulness (M ! 4.17, SD ! 1.27) and treatment satisfaction (M ! 4.33, SD ! 1.23) on a 5-point Likert-type scale. On the self-reported assessment of comprehension, participants rated the concepts of acceptance (M ! 4.17, SD ! 0.72), willingness (M ! 4.08, SD ! 1.16), mindfulness (M ! 4.42, SD ! 1.16), and defusion (M ! 4.25, SD ! 0.97) to be fairly easy to comprehend. However, on the objective assessment of comprehension, participants demonstrated variable levels of construct comprehension, scoring from 58.4% (11.67/20 points) correct on willingness, defusion, and values to 83.3% (16.67/20 points) correct on mindfulness. Intervention Effects Participants made large improvements from pre- to posttreatment in calorie (d ! 1.03; $523.0 calories/day), fat gram (d ! 1.15; $32.37 g/day), and sodium intake (d ! 1.63; $1509 mg/day), as well as substantial reductions in absolute weight and BMI (d ! $0.13; $2.2 kg; $.77 kg/m2), and moderate 12 Behavior Modification XX(X) Table 3. Means, Standard Deviations, Change Scores, and Effect Sizes Measure M Psychological variables (n ! 12) DDS Pretreatment 24.58 Posttreatment 26.33 PHLMS (acceptance) Pretreatment 33.83 Posttreatment 33.00 PHLMS (awareness) Pretreatment 34.75 Posttreatment 37.75 FAAQ Pretreatment 47.83 Posttreatment 54.50 PA-AAQ Pretreatment 25.08 Posttreatment 28.42 Values/goals clarity Pretreatment 1.85 Posttreatment 2.54 Behavioral Variables (n ! 12) Calories (kcal) Pretreatment 1778.21 Posttreatment 1255.21 Fat (grams) Pretreatment 77.81 Posttreatment 45.44 Sodium (mg) Pretreatment 3378.24 Posttreatment 1869.24 IPAQ (METS/min per week) Pretreatment 3946.29 Posttreatment 12397.79 Weight (lbs) Pretreatment 223.34 Posttreatment 218.48 BMI (kg/m2) Pretreatment 35.61 Posttreatment 34.87 SD Mchange SDchange p ES (d) 7.56 7.82 1.75 10.65 .58 0.23 6.41 7.31 $0.83 4.26 .51 $0.12 6.27 7.56 3.00 4.05 .03 0.43 12.65 8.32 6.67 10.92 .06 0.62 5.30 2.68 3.33 5.26 .05 0.80 1.14 0.82 0.44 1.33 .02 0.33 580.02 421.05 $523.00 335.85 .00 1.03 23.05 23.68 $32.37 23.13 .00 1.15 1087.18 729.12 $1509.00 886.78 .00 1.63 7025.97 20899.86 8451.5 22341.33 .22 0.54 39.59 37.80 $4.85 4.64 .00 $0.13 7.84 7.73 $0.74 $0.11 .10 $0.05 Note: ES ! effect size; PHLMS ! Philadelphia Mindfulness Scale; DDS ! Drexel Defusion Scale; FAAQ ! Food Craving Acceptance and Action Questionnaire; PA-AAQ ! Physical Activity Acceptance and Action Questionnaire; IPAQ ! International Physical Activity Questionnaire; METS ! metabolic equivalents; BMI ! body mass index 13 Goodwin et al. Table 4. Correlation Coefficients of Residualized Change Scores (Pretreatment to Posttreatment) of Behavioral Variables and Psychological Variables. Calories (kcal) Fat (g) Sodium (mg) IPAQ total (METS) Weight (lbs) $.18 .18 .41a .42a — $.12 $.38a .35a .14 .58*a — .09 .00 .29a .42a .64*a — $.04 $.165 — $.42a .09 .15 .78*a .09 — $.12 $.14 $.18 $.05 DDS FAAQ PHLMS–acceptance PHLMS–awareness PA-AAQ Values/goals clarity Note: IPAQ ! International Physical Activity Questionnaire; METS ! metabolic equivalents; DDS ! Drexel Defusion Scale; FAAQ ! Food Craving Acceptance and Action Questionnaire; PHLMS ! Philadelphia Mindfulness Scale; PA-AAQ ! Physical Activity Acceptance and Action Questionnaire. a Medium-large effect sizes. *p % .05. increases in physical activity (d ! 0.54; 8451.5 metabolic equivalents [METS]/day; Table 3). Mechanism of Action Comparisons of pre- and posttreatment scores indicated medium-sized, significant (or trending significant) improvements on most psychological measures, including psychological acceptance, awareness, and defusion (Table 3). Moreover, (residualized) gains in these psychological variables were associated with (residualized) gains in outcome variables (Table 4). Considering the study’s limited power to detect bivariate associations, the pattern of results is consistent with our mediation hypotheses. Discussion This pilot study evaluated the feasibility, acceptability, and initial effectiveness of implementing ABBT inpatients with, or at high risk for, CVD. The program was viewed as helpful to participants, was feasible to deliver, and maintained a moderately high retention rate. Despite the low program intensity (6 hr), analyses revealed moderate to large pretreatment to posttreatment improvements in patient adherence to a heart-healthy lifestyle (improvements in weight, physical activity, and calorie, saturated fat, and sodium intake). For example, participants lost an average of 2.2% of their baseline 14 Behavior Modification XX(X) body weight (0.73%/week), which compares favorably with standard exercisebased cardiac rehabilitation programs, which report a 0% to 2% reduction in body weight at 3 months (Brochu et al., 2000). Weight loss among participants is consistent with previous research on the impact of diet and physical activity on weight loss (Donnelly, Jacobsen, Snyder Heelan, Seip, & Smith, 2000; Garrow & Summerbell, 1995). The current study reported large (42%) reductions in fat gram intake, although not as large as some of the more time- and resource-intensive interventions such as the Lifestyle Heart Trial, which achieved an 80% reduction while using a vegetarian diet and a week-long hotel retreat followed by 4 hr of group meetings twice a week (Ornish et al., 1998). In support of the theorized mechanisms of action, increases in nearly all process variables were also observed, and these changes were associated with improvement in outcome variables. The general acceptance score was essentially unchanged (d ! $0.12). However, as predicted, food-specific and physical activity–specific acceptance increased from pre- to postintervention. The intervention (unlike others we and others have implemented) was short term in nature and specifically targeted foodspecific and physical activity–specific acceptance skills, which could explain the lack of change in general acceptance. Although the absence of a control group limits conclusions, the changes in the very psychological variables targeted by the intervention in combination with the associations observed between gains in psychological variables and outcomes support the contention that the intervention (and not another factor) was responsible for the participants’ health gains. There are several important limitations to this study. First, as noted, this was a small pilot investigation that lacked a control group and long-term assessments. Second, several constructs were collected by self-report, including calorie intake, physical activity, and distress tolerance. Self-reports of calorie intake and physical activity have only moderate reliability (Jakicic, Polley, & Wing, 1998), and self-reports of distress tolerance show very low associations with behavioral measures (e.g., cold-pressor-induced pain; Schloss & Haaga, 2011).Third, travel, frequent doctor appointments, and inclement weather impacted participant retention rates. Nevertheless, retention rates were comparable with previous cardiac rehabilitation programs and other behavioral interventions (Butler, Furber, Phongsavan, Mark, & Bauman, 2009; Chang, Hendricks, Slawksy, & Locastro, 2004) [AQ: 7]. Fourth, the low literacy observed in this group (evidenced by poor spelling, poor grammar, inappropriate word usage, and incomplete sentences in openended written questionnaires) may have compromised several aspects of the intervention, such as comprehension of concepts, written supplementary Goodwin et al. 15 material, and self-report measures. Finally, therapist adherence and patient adherence to homework assignments were not captured. Overall, the intervention was feasible and rated as very helpful by participants, and preliminary results support theorized psychological processes (e.g., mindfulness, defusion) and their role in heart-health behavior change. The current intervention was the first study to our knowledge to test an acceptance-based behavioral intervention to increase adherence to hearthealthy behaviors in a cardiac patient population. The intervention was successful at delivering a novel intervention to cardiac patients and increasing adherence to a heart-healthy lifestyle. Future studies should increase intensity and add active controls to formally address mediational pathways to adherence. Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.[AQ: 8] Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.[AQ: 9] Note 1. Effect sizes can be calculated using Cohen’s d ! (M1 $ M2)/σpooled or using a formula that accounts for the correlation between the two time points (Dunlop, Cortina, Vaslow, & Burke, 1996)[AQ: 10]. We chose the former because it provides more conservative estimates. References American Heart Association. (2009a). Getting healthy. Retrieved from http://www .heart.org/HEARTORG/GettingHealthy/GettingHealthy_UCM_001078_Sub HomePage.jsp American Heart Association. (2009b). Heart disease and stroke statistics–2009 update. Author.[AQ: 11] Becker, G., & Murphy, K. (1988). A theory of rational addiction. Journal of Political Economy, 96, 675-700. Bennett, P., & Carroll, D. (1994). Cognitive-behavioural interventions in cardiac rehabilitation. Journal of Psychosomatic Research, 38, 169-182. Billings, J., Scherwitz, L., Sullivan, R., & Sparler, S. (Eds.). (1996). The lifestyle heart trial: Comprehensive treatment and group support therapy. Washington, DC: American Psychological Association. 16 Behavior Modification XX(X) Bolman, C., de Vries, H., & van Breukelen, G. (2002). A minimal-contact intervention for cardiac inpatients: Long-term effects on smoking cessation. Preventive Medicine, 35, 181-192. doi:10.1006/pmed.2002.1036 Brochu, M., Poehlman, E. T., Savage, P., Fragnoli-Munn, K., Ross, S., & Ades, P. (2000). Modest effects of exercise training alone on coronary risk factors and body composition in coronary patients. Journal of Cardiopulmonary Rehabilitation, 20, 180-188. Brown, R., Lejuez, C., Kahler, C., & Strong, D. (2002). Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology, 111, 180-185. Brown, R., Lejuez, C., Kahler, C., Strong, D., & Zvolensky, M. (2005). Distress tolerance and early smoking lapse. Clinical Psychology Review, 25, 713-733. Brownell, K. (2000). The LEARN program from weight management. Dallas, TX: American Health. Butryn, M. L., Forman, E., Hoffman, K., Shaw, J. A., & Juarascio, A. S. (2011). A pilot study of acceptance and commitment therapy for promotion of physical activity. Journal of Physical Activity & Health, 8, 516-522. Cardaciotto, L., Herbert, J., Forman, E., Moitra, E., & Farrow, V. (2008). The assessment of present-moment awareness and acceptance: The Philadelphia mindfulness scale. Assessment, 15, 204-223. Cobb, S. L., Brown, D., & Davis, L. L. (2006). Effective interventions for lifestyle change after myocardial infarction or coronary artery revascularization. Journal of the American Academy of Nurse Practitioners, 18, 31-39. Cutler, D., & Lleras-Muney, A. (2008). Education and health: Evaluating theories and evidence. In R. Schoeni, J. House, G. Kaplan, & H. Pollack (Eds.), Making Americans healthier: Social and economic policy as health policy (pp. 29-60). New York, NY: Russell Sage. Donnelly, J., Jacobsen, D., Snyder Heelan, K., Seip, R., & Smith S. (2000). The effects of 18 months of intermittent vs continuous exercise on aerobic capacity, body weight and composition, and metabolic fitness in previously sedentary, moderately obese females. International Journal of Obesity and Related Metabolic Disorders, 24, 566-572. Dorneleas, E. (2008). Psychotherapy with cardiac patients: Behavioral cardiology in practice. Washington, DC: American Psychological Association. Dorneleas, E., Sampson, R. A., Gray, J. F., Waters, D., & Thompson, P. D. (2000). A randomized controlled trial of smoking cessation counseling after myocardial infarction. Preventive Medicine, 30, 261-268. Falk, L., Bisogni, C., & Sobal, J. (2000). Personal, social, and situational influences associated with dietary experiences of participants in an intensive heart program. Journal of Nutrition Education, 32, 251-260. Goodwin et al. 17 Forman, E., Butryn, M. L., Hoffman, K., & Herbert, J. D. (2009). An open trial of an acceptance-based behavioral treatment for weight loss. Cognitive and Behavioral Practice, 16, 223-235. Forman, E., Butryn, M. L., Shaw, J. A., Glassman, L. H., Clark, V. L., Belmont, A., & Herbert, J. D. (2010, November). Preliminary outcomes in the mind your health project: A randomized controlled trial comparing standard behavioral and acceptance-based behavioral interventions for obesity. In J.Arch (Chair), Acceptancebased therapies for anxiety disorders and obesity. Paper to be presented at the 44th annual convention of the Association for Behavioral and Cognitive Therapies, San Francisco, CA. Forman, E., & Herbert, J. (2009). New directions in cognitive behavior therapy: Acceptance-based therapies. Hoboken, NJ: Wiley. Forman, E., Herbert, J., Moitra, E., Yoemans, P., & Geller, P. (2007). A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior Modification, 31, 772-799. Garrow, J., & Summerbell, C. (1995). Meta-analysis: Effect of exercise, with or without dieting, on the body composition of overweight subjects. European Journal of Clinical Nutrition, 49, 1-10. Gifford, E., Kohlenberg, B., Hayes, S., Antonuccio, D., Piasecki, M., Rasmussen-Hall, M., & Palm, K. M. (2004). Acceptance-based treatment for smoking cessation. Behavior Therapy, 35, 689-705. Gregg, J., Callaghan, G., Hayes, S., & Glenn-Lawson, J. (2007). Improving diabetes self-management through acceptance, mindfulness, and values: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 75, 336-343. Hajek, P., Taylor, T., & Mills, P. (2002). Brief intervention during hospital admission to help patients to give up smoking after myocardial infarction and bypass surgery: Randomised controlled trial. British Medical Journal, 324, 87-89. Hayes, S., Strosahl, K., & Wilson, K. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford. Hayes, S., Strosahl, K., & Wilson, K. (2002). Acceptance and commitment therapy: An experimental approach to behavior change. Child & Family Behavior Therapy, 24, 51-57. Hayes, S., & Wilson, K. (1994). Acceptance and commitment therapy: Altering the verbal support for experiential avoidance. Behavior Analyst, 17, 289-303. Illsley, R., & Baker, D. (1991). Contextual variations in the meaning of health inequality. Social Science & Medicine, 32, 359-365. Jakicic, J., Polley, B., & Wing, R. (1998). Accuracy of self-reported exercise and the relationship with weight loss in overweight women. Medicine & Science in Sports & Exercise, 30, 634-638. 18 Behavior Modification XX(X) Jiang, A., Sit, J., & Wong, T. K. S. (2007). A nurse-led cardiac rehabilitation programme improves health behaviors and cardiac psychological risk parameters: Evidence from Chengdu, China. Journal of Clinical Nursing, 16, 1886-1897. Lisspers, J., Sundin, O., Hofman-Bang, C., Nordlander, R., Nygren, A., Ryden, L., & Ohman, A. (1999). Behavioral effects of a comprehensive, multifactorial program for lifestyle change after percutaneous transluminal coronary angioplasty: A prospective, randomized, controlled study. Journal of Psychosomatic Research, 46, 143-154. Moitra, E., Herbert, J., & Forman, E. (in press). Acceptance-based behavior therapy to promote HIV medication adherence. AIDS Care.[AQ: 12] National Cancer Institute. (2010). The automated self-administered 24-hour dietary recall (ASA24).[AQ: 13] Ornish, D., Brown, S., Scherwitz, L., Billings, J., Armstrong, W., Ports, T., . . . Gould, K. L. (1990). Can lifestyle changes reverse coronary heart disease? The lifestyle heart trial. Lancet, 336, 129-133. Ornish, D., Scherwitz, L. W., Billings, J. H., Brown, S. E., Gould, K. L., Merritt, T. A., . . . Brand, R. J.(1998). Intensive lifestyle changes for reversal of coronary heart disease. Journal of American Medical Association, 280, 2001-2007. Pischke, C. R., Scherwitz, L., Weidner, G., & Ornish, D. (2008). Long-term effects of lifestyle changes on well-being and cardiac variables among coronary heart disease patients. Health Psychology, 27, 584-592. Rigotti, N. A., McKool, K. M., & Shiffman, S. (1994). Predictors of smoking cessation after coronary artery bypass graft surgery. Results of a randomized trial with 5-year follow-up. Annals of Internal Medicine, 120, 287-293. Schloss, H. M., & Haaga, D. A. F. (2011). Interrelating behavioral measures of distress tolerance with self-reported experiential avoidance. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 29, 53-63. Sundin, O., Lisspers, J., Hofman-Bang, C., Nygren, A., Ryden, L., & Ohman, A. (2003). Comparing multifactorial lifestyle interventions and stress management in coronary risk reduction. International Journal of Behavioral Medicine, 10, 191-204. Bios Christina L. Goodwin, MS, is a doctoral student in clinical psychology at the Ohio State University. Her research interests include developing interventions to improve cardiovascular health and promote healthy behaviors. Evan M. Forman, PhD, is an associate professor of psychology at Drexel University where he is the director of the doctoral program in clinical psychology. His research interests include the development and evaluation of acceptance-based behavioral Goodwin et al. 19 interventions for mood, anxiety, and health-related behavior change; mediators of psychotherapy outcome; and posttraumatic stress disorder. James D. Herbert, PhD, is professor of psychology and director of the Anxiety Treatment and Research Program at Drexel University, where he also serves as associate dean of the College of Arts and Sciences. His research interests include cognitive behavior therapy, clinical behavioral analysis, psychological acceptance, and remote treatment delivery. Meghan L. Butryn, PhD, is an assistant research professor in the Department of Psychology at Drexel University. She conducts research on the prevention and treatment of obesity and eating disorders. Gary S. Ledley, MD, is board certified in cardiovascular disease, internal medicine, and interventional cardiology. He has been the principle investigator for a number of National Institutes of Health–funded research studies and has published extensively in the cardiology field.