Lipids have a wide variety ... consequence of their chemical and ... Introduction to Lipid Metabolism Roles of Lipids
advertisement

Introduction to Lipid Metabolism
Roles of Lipids
Lipids have a wide variety of roles in biological systems. These roles are a
consequence of their chemical and physical properties. Fatty acids and their
derivatives (especially triacylglycerols) can act as highly concentrated energy
storage molecules. The high energy density (i.e. the relatively large amount of
energy released per unit of mass) of fat stores is due to three main factors. 1) The
completely reduced carbons of fatty acids have a higher energy content than the
partially oxidized carbons of carbohydrates and proteins. 2) The fortuitous fact that
the reduced carbons have covalent bonds to light atoms (hydrogen rather than to
the heavier oxygen) means that the fully reduced hydrocarbon compounds are
lighter than the partially oxidized carbohydrates. 3) Lipids are hydrophobic
molecules and therefore fat stores tend to exclude water, which would add to the
weight of the molecules without adding to the energy content.
Because layers of lipids are good insulators, and because adipose tissue has
limited metabolic activity, fat stores can reduce the exchange of heat between an
organism and its environment. This insulation is important for mammals living in
cold climates, and is especially important for marine mammals, which would
otherwise rapidly lose their body heat to the much cooler surrounding water.
As we have already seen, membranes are composed of fatty acid derivatives. These
compounds form hydrophobic barriers that separate cells from their surroundings
and which subdivide cells into multiple compartments that allow more finely tuned
control of metabolism. Lipids are also used as signaling molecules, such as
prostaglandins and steroids, and as enzyme cofactors.
Digestion of lipids
The majority of lipids in a normal diet are present in the form of triacylglycerols.
Digestion of these compounds begins in the stomach, which contains acid-stable
lipases that release some free fatty acids from dietary triacylglycerols. However, the
stomach is not capable of efficiently cleaving triacylglycerols, because these
hydrophobic molecules tend to aggregate, and the lipases are only capable of
hydrolyzing the triacylglycerols at the surface of the aggregates. In addition, the
stomach has a small surface area to volume ratio, and therefore many of the
triacylglycerols are not accessible to the enzymes.
The small intestine has mechanisms for emulsifying lipids. The process begins by
dispersing the lipid aggregates mechanically as a result of the muscles of the small
intestine forcing the partially digested material through the relatively small spaces
of the intestinal lumen. In addition, the intestine contains bile acids and bile salts,
detergents that break up the lipid aggregates into smaller micelles.
OH
Examples
of bile
acids
O
OH
OH
O
OH
OH
O
NH
O
S OH
HO
OH
Cholic acid
Copyright © 2000-2013 Mark Brandt, Ph.D.
Deoxycholic acid
HO
1
HO
O
OH Taurocholic acid
Finally, the small intestine also contains a variety of digestive enzymes produced in
the pancreas. These enzymes include pancreatic cholesteryl ester hydrolase,
which releases free cholesterol from cholesteryl esters, pancreatic lipase, which
releases free fatty acids from the 1- and 3-positions of triacylglycerols, and several
phospholipases, which release free fatty acids from phospholipids. The
monoacylglycerols, partially hydrolyzed phospholipids, and free fatty acids act as
additional detergents and assist in further disrupting the larger lipid aggregates.
O
C
Triacylglycerol O
CH2 CH CH2
O
C
O
O
C
O
H2O
Free
fatty
acid
1,2-Diacylglycerol
OH
H2O
Free
fatty
acid
CH2 CH CH2
O
Pancreatic
lipase
C
O
O
C
O
2-Monoacylglyerol
OH
CH2 CH CH2
Pancreatic
lipase
O
C
OH
O
Absorption of fatty acids
Once the micelles of free fatty acids, 2-monoacylglycerols, and bile acids become
small enough, they can be absorbed from the intestinal lumen into the intestinal
cells. In the intestinal cells, the fatty acids are esterified to re-form triacylglycerols.
These triacylglycerols combine with apolipoproteins synthesized by the intestines to
produce chylomicrons, which act as serum transport particles for triacylglycerols.
Lipid transport
Lipid transport is a continuously varying process. During the absorption of
nutrients from the diet, lipids must be transported to the tissues for use. When
lipids are not being absorbed, they must be transported from adipose stores to
maintain metabolism. Finally, cholesterol redistribution from one tissue to another
requires movement of cholesterol through the blood stream.
Lipids are hydrophobic and exhibit very limited solubility in aqueous media such as
the blood. Analysis of blood indicates that plasma contains triacylglycerol,
phospholipids, cholesterol, and free fatty acids.
Free fatty acid levels in the blood are usually quite low (less than 5% of the total
plasma lipids). The levels of free fatty acids depend on the rate of their release by
adipose tissue. Most free fatty acids are actually bound to serum albumin; the total
concentration of “free fatty acid” may approach 2 mM, with the vast majority of
these compounds present bound to serum proteins; the millimolar concentrations
observed in most individuals represent a ~1000-fold increase over the maximum
concentration that could exist without forming micelles in the absence of the carrier
proteins.
The stereoview figure below shows human serum albumin bound to stearic acid
(from PDB ID 1E7I). About seven fatty acid molecules were observed to be bound
Copyright © 2000-2013 Mark Brandt, Ph.D.
2
this experimentally determined structure, with four additional sites thought to
allow binding of shorter chain fatty acids; the binding sites appear to vary
significantly in affinity, with many of the sites being capable of binding other nonpolar molecules.
A family of sodium-dependent active transporters (fatty acid transport proteins,
FATP) mediates transport of the free fatty acids into cells. In spite of the pump
proteins, however, uptake of fatty acids is largely a function of fatty acid
concentration in plasma. The fate of the free fatty acids inside cells depend on the
status of the cell; the energy balance of the cell determines the rate of β-oxidation to
acetyl-CoA relative to the rate of esterification to form triacylglycerols or
phospholipids.
Transport and use of lipids other than free fatty acids requires specialized
mechanisms to overcome their insolubility. One option would be to allow these
compounds to simply form micelles, and allow these micelles to move freely.
However, most lipids are insufficiently soluble to allow favorable micelle formation.
In addition, actual lipid transport requires a greater degree of control than would
result from release of individual lipid molecules. Actual lipid transport involves
specialized particles (lipoproteins) in which the lipids and specific proteins for
structures that allow the control of lipid movement. Lipoproteins are discussed
further in a later section.
Nutrient storage
Fatty acids are stored in adipose tissue in the form of triacylglycerols, while
cholesterol is stored in the form of cholesteryl esters in a variety of tissues. These
molecules are essentially entirely hydrophobic, and therefore tend to remain
present as aggregates (called lipid droplets) within tissues.
Different tissues contain different amounts of fuel available for use during fasting.1
The fuel is present in three major forms: carbohydrate, protein, and fat. The table
below summarizes the distribution of this fuel among the tissues of the body.
1Fasting is a technical term that applies both to the few hours between meals and to a prolonged
period without food.
Copyright © 2000-2013 Mark Brandt, Ph.D.
3
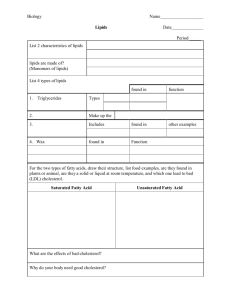
Fuel reserves of “typical” 70 kg individual
Glucose or
glycogen
Available energy (kcal)
Triacylglycerols Degradable Protein
Organ
Brain
8
0
0
Blood
60
45
0
Liver
400
450
400
Muscle
1200
450
24,000
Adipose tissue
80
135,000
40
(modified from Stryer (1995) Biochemistry, 4th Ed.)
The carbohydrate stores, predominately glycogen with small amounts of circulating
glucose, contain sufficient energy to support metabolism for about one day. In
principle, the various protein stores could provide fuel for a prolonged fast (one to
two weeks); in practice, most of the proteins involved have functional roles (in the
form of enzymes, contractile proteins, and structural molecules). However, some
protein degradation is often necessary to support gluconeogenesis, since acetyl-CoA,
the main product of lipid breakdown, cannot be used as substrate for glucose
synthesis. (Note that the brain and blood do not contain “degradable protein”; these
tissues obviously contain protein, but in general this protein is exempt from
degradation for fuel.) The fat stores of adipose tissue provide the major energy
reservoir for the animal.
As mentioned above, triacylglycerol has a much higher energy density than protein
or carbohydrate. The standard figures quoted for dietary calculations (i.e. fat
yielding ~9 kcal/g and protein or carbohydrate yielding ~4 kcal/g), apply to the dry
weight of the compounds. In vivo, metabolism of protein or carbohydrate yields only
about 1 kcal/g of stored substrate due to the large amount of water associated with
these compounds. In contrast, triacylglycerol is hydrophobic, and therefore little
water is associated with fat stores; metabolism of the fat stored in adipose tissue
yields nearly the full 9 kcal/g. This is good news for individuals attempting to carry
their energy stores with them: the weight of glycogen equivalent in energy to the
normal fat stores of a 70 kg man would be about 100 kg! On the other hand, in
contemplating weight loss, each kilogram corresponds to about 7000 kcal, enough
energy to maintain normal metabolism for several days.
Side note: calories, Calories, and joules
The SI unit for energy is the joule, and joules (and kilojoules) are the energy unit used in most of the
modern biochemical literature. For many types of calculations joules have advantages. However,
when discussing the energy content of food, many sources use “Calories”. The terminology used is
that a “Calorie” (i.e. written with a capital “C”) is a kilocalorie. The distinction is important: one
calorie is the amount of energy required to raise the temperature of 1 gram of water by 1°C, while
one kcal is the energy required to raise the temperature of 1 kilogram of water by 1°C.
Misunderstanding of the difference between calories and Calories has led some people to proclaim
that drinking a soda should result in weight loss. A typical (non-diet) soda has 180 Calories, while
Copyright © 2000-2013 Mark Brandt, Ph.D.
4
the energy required to raise the temperature of 355 ml of the liquid from its initial temperature of
4°C to body temperature of 37°C is 11,715 calories. Naively comparing 11,715 calories to 180
Calories presents the appearance of an energy deficit.
To avoid this potential problem, the Table above explicitly uses “kcal”, rather than the equivalent
potentially misleading term “Calories”. To convert calories to joules, multiply by 4.184 (the ratio of
the gas constants 8.3145 joules•mol–1•K–1 and 1.9872 cal•mol–1•K–1).
Utilization of lipid stores
The first step in the metabolism of fat stores is the release of free fatty acids from
the adipose tissue. This release is a regulated process, with three major stimulators
(epinephrine, cortisol, and growth hormone), and one major inhibitor (insulin). Each
of the four hormones alters the activity of the hormone-sensitive lipase, the enzyme
that hydrolyzes triacylglycerol from the lipid droplets to release the free fatty acids
and glycerol into circulation. (The mechanism for the growth hormone effect is
poorly understood, and may be confined to decreasing the effect of insulin.)
"!
"!
%&'()&*+'()
&'()*+*),-.
/*.*012)
"!
B!C.
!"
!%$
"
"
.'3$
.'3$
2/3145)&)(6)(7
1+87)'(9:'(;<)
=-+7.1-9*>
!"#$%&'(')*')+
$,-+'.)/0.)12'
3)(,-.#4
$
-+
-0
)-5
!5<.2.2)1-.2-(
/*.*012)
0+
%)-7.45,54.*)25"
$*
-+
-0
=-0-(>#)205*1
$*)-5-0-+
$
$*)-5-0-+
012*31),)*#
012*31),)*#
-5-
)-5
$
5-,6-)'
7')2.+.8'/9.(12'
3)(,-.#4
!8+?8()
#)(<'7'@)9A'&;<)
=-+7.1-9*>
$
5-,6-)'
7')2.+.8'/9.(12'
3)(,-.#4
$*
)
$*
)-5
-0
-+
$*
42562$#78#$*-,-.#
9-3)*#:;#$#:<5)$*(5-3,-2$
"
?)**>@7114>7.-("
A>,54.*)25
.'3$
/01
!
"
!
"
!
"
!
"
"
-+
$
$
.
!
"
!
"
!
"
!
"
!
"
$
$
!"#$%&%&
'%(&)*#
+!(,-.#/
BC02)1
"
!
"
!#$
#
#
!
"
!"
!
"
!
"
!
"
"
!
"
!
"
!
"
!
"
!
"
'(*+4545
64.57"*
8-+7.1-9*:
!
"
!,-
!
"
!
"
!
"
!
"
!
"
!
"
!
"
!
"
!
"
"
?)**>@7114>7.-("
A>,54.*)25
%)-7.45,54.*)25"
G+))
2*8F)<7)+8F
1)+'&*)+;F
/&8&+87)'(
!"
"
"
"
-
"
"
"
"
"
-
"
"
-
"
"
"
-
"
"
-
!"
-*8F)<7)+HF
)<7)+<
Copyright © 2000-2013 Mark Brandt, Ph.D.
5
"
D(7)E+;F
/&8&+87)'(
)-5
-+
9-32352,#-$
9-3)*#
$*
-0
!
"
"
!
"
;D02)1
!
"
!
"
"
!
"
!
"
!
"
!
"
!
"
"
)-5
?)**>@7114>7.-("
$*
;+"<5-+
/*.*012)
-0
%)-7.45,54.*)25"
<5-)(%&=&%(#52&
*%$,1#*-*
$*
)-5
-+
-0
-+
-0
)-5
$*)-5-0-+
$*
Hormone-sensitive lipase activity is increased by phosphorylation. Epinephrine
increases cAMP production, which in turn increases phosphorylation of the enzyme,
and therefore increases the activity of the enzyme. Cortisol acts by increasing the
transcription of the hormone-sensitive lipase; cortisol and epinephrine thus act via
different mechanisms to increase triacylglycerol breakdown.
Insulin inhibits triacylglycerol breakdown by increasing the activity of a protein
phosphatase that reverses the cAMP-dependent phosphorylation of the hormonesensitive lipase. Insulin also decreases cAMP levels, and decreases hormonesensitive lipase gene transcription. Adenosine seems to also inhibit triacylglycerol
breakdown, probably by decreasing cAMP production.
Caffeine and thyroid hormone both indirectly stimulate triacylglycerol breakdown.
Caffeine inhibits cAMP phosphodiesterase, and therefore increases the half-life of
cAMP, and also acts as an adenosine antagonist. Thyroid hormone makes the cell
more sensitive to the effects of epinephrine, and may have other actions also.
In addition to the effects on the hormone-sensitive lipase, increased cAMPdependent protein kinase activity results in phosphorylation of the perilipin
proteins. The phosphorylated perilipin proteins increase access of the hormonesensitive lipase to the lipid droplet interior, and probably increase activity of other
triacylglycerol lipases as well. The control of adipose tissue lipolysis is still an active
area of research, and is not fully understood.2
2
The recent discovery of a perilipin gene mutation has aided in the understanding of the role of the
perilipin gene products in humans. See Gandotra, et al., (2011) “Perilipin Deficiency and Autosomal
Dominant Partial Lipodystrophy” N. Engl. J. Med. 364, 740-748.
Copyright © 2000-2013 Mark Brandt, Ph.D.
6