Health Care Transition and Youth with Autism Spectrum Disorders
advertisement
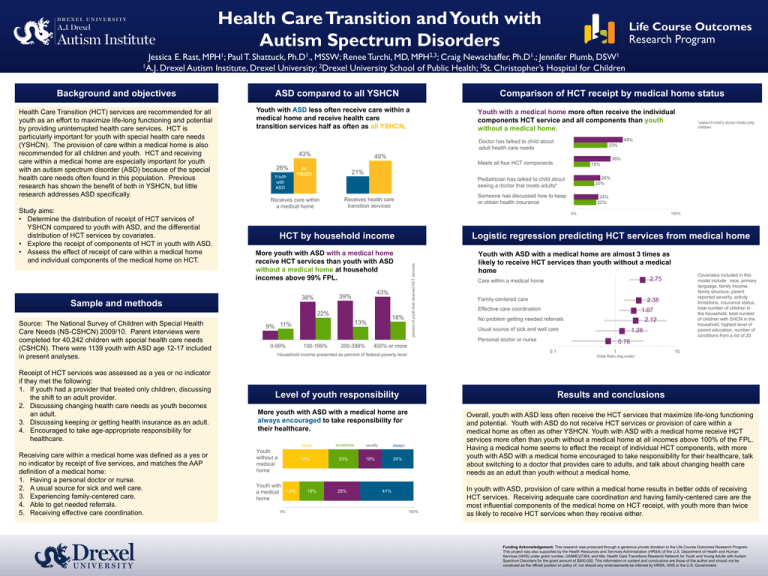
Health Care Transition and Youth with Autism Spectrum Disorders Jessica E. Rast, MPH1; Paul T. Shattuck, Ph.D1., MSSW; Renee Turchi, MD, MPH2,3; Craig Newschaffer, Ph.D1.; Jennifer Plumb, DSW1 1A.J. Drexel Autism Institute, Drexel University; 2Drexel University School of Public Health; 3St. Christopher’s Hospital for Children Health Care Transition (HCT) services are recommended for all youth as an effort to maximize life-long functioning and potential by providing uninterrupted health care services. HCT is particularly important for youth with special health care needs (YSHCN). The provision of care within a medical home is also recommended for all children and youth. HCT and receiving care within a medical home are especially important for youth with an autism spectrum disorder (ASD) because of the special health care needs often found in this population. Previous research has shown the benefit of both in YSHCN, but little research addresses ASD specifically. Study aims: • Determine the distribution of receipt of HCT services of YSHCN compared to youth with ASD, and the differential distribution of HCT services by covariates. • Explore the receipt of components of HCT in youth with ASD. • Assess the effect of receipt of care within a medical home and individual components of the medical home on HCT. ASD compared to all YSHCN Youth with ASD less often receive care within a medical home and receive health care transition services half as often as all YSHCN. 43% 26% Youth with ASD 36% 16% 21% Receives care within a medical home Receives health care transition services Pediatrician has talked to child about seeing a doctor that treats adults* 26% 20% Someone has discussed how to keep or obtain health insurance 24% 22% 0% HCT by household income More youth with ASD with a medical home receive HCT services than youth with ASD without a medical home at household incomes above 99% FPL. 43% 39% 38% 18% 13% 9% 11% 100% Logistic regression predicting HCT services from medical home Youth with ASD with a medical home are almost 3 times as likely to receive HCT services than youth without a medical home 0-99% 100-199% 200-399% Family-centered care 2.38 Effective care coordination 1.97 No problem getting needed referrals 2.12 Usual source of sick and well care 1.28 0.1 Youth without a medical home 35% Youth with a medical home 0% 13% 19% 23% 28% always 18% 24% 10 Results and conclusions More youth with ASD with a medical home are always encouraged to take responsibility for their healthcare. usually 1 Odds Ratio (log scale) Level of youth responsibility sometimes 0.76 400% or more Household income presented as percent of federal poverty level Covariates included in this model include: race, primary language, family income, family structure, parent reported severity, activity limitations, insurance status, total number of children in the household, total number of children with SHCN in the household, highest level of parent education, number of conditions from a list of 20. 2.75 Care within a medical home Personal doctor or nurse never Receiving care within a medical home was defined as a yes or no indicator by receipt of five services, and matches the AAP definition of a medical home: 1. Having a personal doctor or nurse. 2. A usual source for sick and well care. 3. Experiencing family-centered care. 4. Able to get needed referrals. 5. Receiving effective care coordination. 33% Meets all four HCT components All YSHCN *asked if child’s doctor treats only children 48% 40% 22% Receipt of HCT services was assessed as a yes or no indicator if they met the following: 1. If youth had a provider that treated only children, discussing the shift to an adult provider. 2. Discussing changing health care needs as youth becomes an adult. 3. Discussing keeping or getting health insurance as an adult. 4. Encouraged to take age-appropriate responsibility for healthcare. Youth with a medical home more often receive the individual components HCT service and all components than youth without a medical home. Doctor has talked to child about adult health care needs Sample and methods Source: The National Survey of Children with Special Health Care Needs (NS-CSHCN) 2009/10. Parent interviews were completed for 40,242 children with special health care needs (CSHCN). There were 1139 youth with ASD age 12-17 included in present analyses. Comparison of HCT receipt by medical home status percent of youth that received HCT services Background and objectives Overall, youth with ASD less often receive the HCT services that maximize life-long functioning and potential. Youth with ASD do not receive HCT services or provision of care within a medical home as often as other YSHCN. Youth with ASD with a medical home receive HCT services more often than youth without a medical home at all incomes above 100% of the FPL. Having a medical home seems to effect the receipt of individual HCT components, with more youth with ASD with a medical home encouraged to take responsibility for their healthcare, talk about switching to a doctor that provides care to adults, and talk about changing health care needs as an adult than youth without a medical home. 41% 100% In youth with ASD, provision of care within a medical home results in better odds of receiving HCT services. Receiving adequate care coordination and having family-centered care are the most influential components of the medical home on HCT receipt, with youth more than twice as likely to receive HCT services when they receive either. Funding Acknowledgement: This research was produced through a generous private donation to the Life Course Outcomes Research Program. This project was also supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number, UA6MC27364, and title, Health Care Transitions Research Network for Youth and Young Adults with Autism Spectrum Disorders for the grant amount of $900,000. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.