Oxford Molecular Genetics Laboratory
advertisement

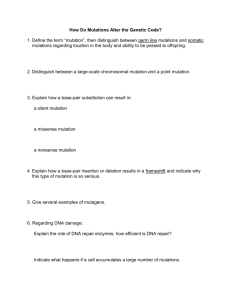
Oxford Molecular Genetics Laboratory Genetics Laboratories, Churchill Hospital, Old Road, Headington, Oxford, OX3 7LE www.ouh.nhs.uk/geneticslab Juvenile Polyposis Syndrome – OMIM 174900, 600993 (SMAD4), 601299 (BMPR1A) INTRODUCTION Juvenile polyposis syndrome (JPS) is a hereditary (autosomal dominant) predisposition to juvenile polyps in the gastrointestinal tract. The majority of the polyps are benign, however approximately 20% of them undergo malignant transformation and become cancerous. Individuals with JPS are also at an elevated risk of developing pancreatic tumours. The age of onset and severity of disease is highly variable, but the overall penetrance of disease in mutation carriers is estimated to be ~90%. Two JPS causative genes have been identified to date; BMPR1A and SMAD4. Mutations in both genes cause JPS but mutations in SMAD4 are specifically associated with a combination of juvenile polyposis and hereditary hemorrhagic telangiectasia (HHT). TESTING AND REFERRALS Diagnostic: o Clinically affected patients. o UK referrals must be made through Clinical Genetics departments. Presymptomatic/confirmation test for a familial mutation: o Individuals at risk of inheriting a pathogenic mutation in SMAD4 or BMPR1A. o Referrals from Clinical Genetics only. o Requests for presymptomatic testing should either be accompanied by details of the known pathogenic mutation in the family or discussed with the laboratory in advance. Prenatal: o Prenatal testing is not usually requested. o Prenatal requests would only be accepted from Clinical Genetics and must be discussed with the laboratory and arranged in advance. STRATEGY & TECHNICAL INFORMATION o Mutation screening in diagnostic referrals is undertaken by fluorescent sequencing analysis of exons 3-13 of BMPR1A and exons 3-13 of SMAD4 (including exon/intron boundaries). o Dosage analysis by multiplex ligation-dependant probe amplification (MLPA) analysis for large scale rearrangements of BMPR1A and SMAD4. o When a pathogenic mutation has been identified in an individual, subsequent testing of family members (presymptomatic or diagnostic confirmation) involves testing for the familial mutation only. TARGET REPORTING TIMES Diagnostic test (2 gene screen): Presymptomatic/Familial Mutation test: Prenatal testing (includes maternal contamination check): 40 working days 10 working days 3 working days CLINICAL SENSITIVITY JPS: Germline mutations in SMAD4 and BMPR1A account for ~15-20% and ~25-40% of mutations respectively in patients with a clinical diagnosis of JPS syndrome; (Howe et al. Science 280 (5366): 1086-8, 1998; Howe et al. Nat Genet 28 (2): 184-7, 2001; Zhou et al.: Am J Hum Genet 69 (4): 704-11, 2001). JPS/HHT: Germline Mutations in SMAD4 have been detected in approximately 2% of patients with HHT and cause HHT and juvenile polyposis (JP/HHT) syndrome. Gallione et al, Lancet 2004, 363(9412):852-9. N.B. Details are correct for the Contact date of printing Details: only – last updated 11/06/2015 Duty Scientist Oxford Regional Molecular Genetics Laboratory, Churchill Hospital, Old Road, Headington, Oxford, OX3 7LE Tel: 01865 225594 Fax: 01865 225363 oxford.dnalab@nhs.net http://www.ouh.nhs.uk/geneticslab