Reimbursement Policy and Cancer Chemotherapy Treatment
advertisement

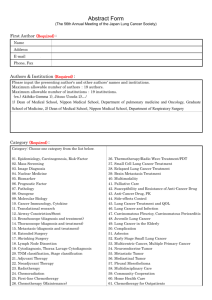
Reimbursement Policy and Cancer Chemotherapy Treatment Mireille Jacobson, RAND and NBER Craig C. Earle, MD, Cancer Care Ontario Mary Price, Kaiser Permanente Joseph P. Newhouse, Harvard and NBER Support from the Robert Wood Johnson Foundation HCFO Program g How do changes in reimbursement rates affect treatment? • Many studies find that non-clinical factors play an important role in physician decisions: – Training and local practice patterns – Reimbursements unrelated to quality-adj. costs • Medicare Modernization Act dramatically changed reimbursement methods for Part B drugs – Did this change affect cancer treatment? Important Institutional Detail • Chemotherapy typically provided in physician’s offices/clinics – Physicians Ph i i purchase h chemotherapy h th d drugs – Payers reimburse physicians for the drugs • Chemotherapy accounts for a large share of oncologist’s income • Ch Changing i reimbursement i b t rates t plausibly l ibl affect ff t ttreatment t t decisions How did the Medicare Modernization Act change reimbursement? • Prior to January 2005, rates based on list price (AWP) – AWP unrelated to transaction prices – Some chemotherapy agents were reimbursed at over 60% of wholesale transaction prices • Since January 2005, rates are based on wholesale prices (ASP) in the previous 2 quarters + 6% – Reimbursement rates for many drugs have declined dramatically since 1/2005 Change in Nominal Quarterly Reimbursement Rates Relative to the Payment Change Nomiinal Reimb bursement Per Mon nthly Dose 3500 3000 2500 2000 1500 1000 500 0 -10 -5 0 5 10 Quarter Relative to January 2005 Carboplatin p Paclitaxel Docetaxel Etoposide p Gemcitabine HCL 15 Potential Changes • Oncologists might turn away patients – refer them to hospitals for treatment • MMA could increase physician prescribing – Make up p for lost margins in volume ol me • Equalized 6% margin incentivizes use of higher priced agents – Potentially unintended effect of MMA Our Analytic Approach • Study lung cancer • Analyze regression-adjusted changes in: – Chemotherapy treatment rates overall – Chemotherapy treatment rates by setting – Use of different agents conditional on chemotherapy treatment • Look at treatment within 1 month of diagnosis – Analyze data 24 months prior to and 10 months after the implementation of the new payment regime Some comments about the approach • Currently just using a pre-post design: – Monumental shift in how chemotherapy is reimbursed – No other major changes to lung cancer treatment – Look for sharp changes in tx at time of change • Test stability of patient characteristics across regime change • In ongoing work, consider a control group: – Kaiser Permanente data for Northern California – Medicare pays a flat fee for enrollees Data sources • Rely exclusively on claims data – Received initial cohort of Medicare beneficiaries with g cancer-related claim,, 2003-2005 at least 1 lung (N=878,923) • ICD-9 codes: 162.0-162.9 • Have all 2002-2006 claims for these beneficiaries from the following files: – Carrier (physician data) – Outpatient – MedPAR M dPAR (inpatient (i ti t data) d t ) – Hospice Analytic Sample • Restrict R t i t to t Fee-for-service F f i patients ti t (95%) • Apply algorithm to “confirm” confirm a lung cancer dx. dx Require: – 2+ non-institutional claims separated by at least 28 days and no more than 365 with a lung cancer dx – 1 institutional claim with a lung cancer dx • Exclude those with more than one primary cancer • 222,478 beneficiaries with a “confirmed” lung cancer diagnosis between 2003 and 2005 Some Sample Characteristics Overall Pre Post Age at Dx 74.0 74.1 74.0 Share White 0.878 0.878 0.878 Share AfricanAmerican 0.089 0.090 0.088 Share male 0.516 0.519 0.511 Share with Metastasis at Dx 0.286 0.287 0.285 Analysis: What did we do? • Visual analysis of trends by month of dx in: – the probability of chemotherapy tx – the probability of receiving different agents among chemotherapy-treated • From visual analysis, specify a regression model to estimate change in probability of tx pre versus post MMA • Narrow the window around the pre versus post MMA periods to ensure estimates are driven by policy What did we find (I)? • Probability of chemotherapy increased about 2pp, off a base of 17% after the new payment regime took effect • Increase came entirely in physician office-setting not in hospital settings • Increase not driven by patent expiration of Carboplatin • Vi Visuall analysis l i off ttrends d suggests t th the paymentt regime i was likely the cause What did we find (II)? • A Among those th receiving i i chemotherapy h th ttreatment: t t – Patients less likely to get Paclitaxel & Carboplatin: 3 4 pp decline each or 14% and 5% respectively 3-4 • Previously reimbursed well above cost – Patients more likely to receive Docetaxel:1pp increase but 10% in relative terms! • Profit margin g changed g little with regime g change g • Higher priced agents favored by flat mark-up rate • Visual analysis of trends suggests some anticipation of the payment regime change Interpretation • Patient choice unlikely to play a role/works against effects ff we are finding fi di – With lower payment rates, physicians increasingly collect 20% coinsurance • Physicians increase volume to make up for lost income due to reduction in margins (PID) – Income effect > substitution effect • Some potential savings from the payment changes were offset ff t by b increases i in i use Summary • MMA’s reduction in payment rates for outpatient chemotherapy drugs: – Did not adversely affect access – Increased I d chemotherapy h th ttreatment t t for f lung l cancer – Changed the relative mix of agents – Implications p for health are unclear in this context Ongoing and Future Work Ongoing and Future Work • Quantify impact on spending: how much did increase in volume and change in drugs offset savings? • Analyze SEER data (confirmatory analysis) • E Expanding di analysis l i tto C Colorectal l t lC Cancer patients ti t – Preliminary results suggest a different response • Will analyze trends in treatment patterns for Kaiser Permanente, Northern California – Control group, Medicare pays a flat fee for enrollees • Will assess heterogeneity by race race, SES and geography