Implementation and use of HIT in primary care settings
advertisement
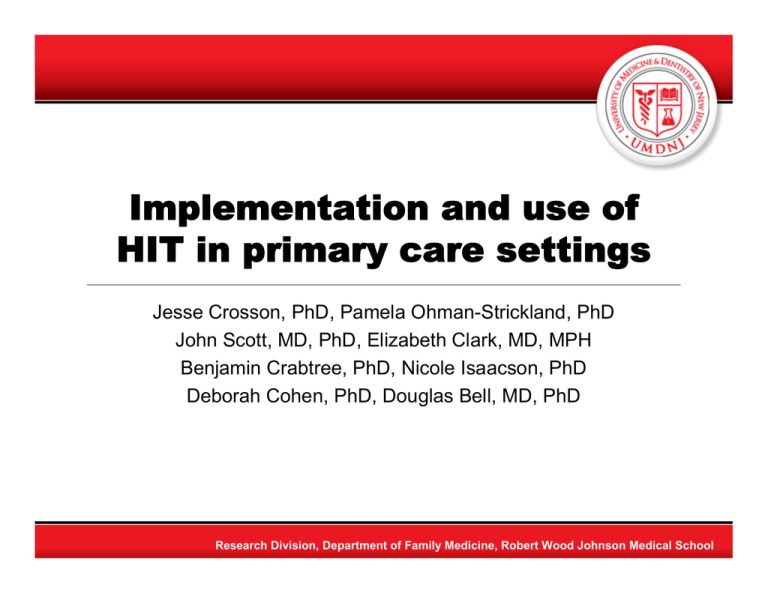
Implementation and use of HIT in primary care settings Jesse Crosson, PhD, Pamela Ohman-Strickland, PhD John Scott, MD, PhD, Elizabeth Clark, MD, MPH Benjamin Crabtree, PhD, Nicole Isaacson, PhD Deborah Cohen, PhD, Douglas Bell, MD, PhD Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Introduction • HIT recommended for error reduction, quality improvement, and cost reduction • Translation to typical primary care practices is needed Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Funders Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Methods • Synthesis of findings from five multimethod studies of implementation and use of HIT in primary care Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Multiple Methods • Qualitative data collection and analysis – Participant observation in 69 primary care practices – Key informant interviews – In-depth interviews with over 128 primary care physicians and their staff – Template organizing and grounded theory analysis of text data • Medical record review – 927 patient records across 50 practices – Hierarchical logistic regression Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Findings – comparative case study • Successful practices (n=5) – Anticipated workflow change and disruption – Had informed and prepared support staff – Physicians expected practice-level efficiency gains • Less successful practices (n=7) – Had little or no advance knowledge – Expected only minimal disruption: “anything you start new, it’s going to cause problems up front, but, I’m sure … within two weeks that will all be sorted out.” – Physicians thought e-prescribing would be faster JC Crosson, N Isaacson, et.al. Variation in electronic prescribing implementation among twelve ambulatory practices. JGIM, 2008, 4:364-71 Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Findings – case study • Reminders were disabled because lab values were scanned into the record. • “Our clinicians know what to do.” • High levels of interpersonal conflicts negatively affected communication • The practice was described by the senior owner as a “dictatorship” JC Crosson, C Stroebel, et. al. Implementing an electronic medical record in a family medicine practice: communication, decision-making, and conflict. AnnFamMed, 2005; 3:307-311. Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Quantitative assessment of care quality and EMR use • Chart audits of 927 randomly selected patients with diabetes in 50 family medicine practices in 2003-2004 • Hierarchical logistic regression to examine adherence to guidelines JC Crosson, PA Ohman-Strickland, et. al. Use of electronic medical records and diabetes quality of care: results from a sample of family medicine practices. AnnFamMed, 2007; 5: 209-215. Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Results • Mean practice-level rates of adherence to clinical guidelines were higher in non-EHR practices • The odds of patients in non-EHR practices meeting three targets (A1c, LDL, BP) was 2.68 times that of patients in EHR practices. Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Medication Adherence Alerting • Alert sent after 60 day gap between prescription and fill – 1918 messages sent, May – Nov 2008 • Qualitative evaluation in 6 primary care practices – Pre: no awareness of ability to track fill status – Post: no reported usage of messages – Discontinuation of e-prescribing • Quantitative assessment – Analysis of prescribing and claims data – ongoing Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Developing an e-Prescribing Implementation Toolset • Develop a strong pharmacy relationship • Delegate work through protocols • E-prescribing eliminates some errors but creates the opportunity for new ones • Pay attention to staff turnover issues • Accessible IT support Research Division, Department of Family Medicine, Robert Wood Johnson Medical School Policy Implications • Primary care practices need: – Ongoing technical support for both implementation and effective use of HIT – Training in population health concepts in order to realize HIT benefits – Quality incentives to reward the results of appropriate use • Regulations needed to ensure – Technologies are capable of achieving health quality improvements Research Division, Department of Family Medicine, Robert Wood Johnson Medical School