Consumer-Directed Health Plans and the Chronically Ill Stephen T. Parente, Ph.D.
advertisement

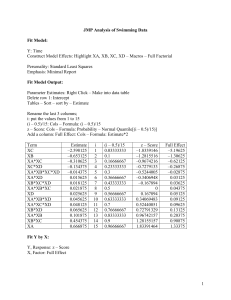
Consumer-Directed Health Plans and the Chronically Ill h Stephen T. Parente, Ph.D. Jon Christianson, Ph.D. Roger Feldman, Ph.D. University of Minnesota Sponsored by the Health Care Financing Organization of the Robert Wood Johnson Foundation Academy Health, June 29, 2009 Questions to Address How are Chronically ill CDHP-enrollees different than non-CDHP enrollees? How does CDHP enrollee expenditures change with respect to a chronic illness? Is there a different story for the chronically ill when they face a CDHP full replacement? Study Population from University of Minnesota Employees, 2003 (AD) HealthPartners Classic Patient Choice Cost Group I Patient Choice Cost Group II Patient Choice Cost Group III PreferredOne National Definity Health Option 1 Definity Health Option 2 Employee-only Coverage Less UM Total Cost Contribution $131.00 $131.00 $131.80 $131.00 $140.50 $131.00 $150.70 $131.00 $179.40 $131.00 $141.20 $131.00 $131.00 $131.00 HealthPartners Classic Patient Choice Cost Group I Patient Choice Cost Group II Patient Choice Cost Group III PreferredOne National Definity Health Option 1 Definity Health Option 2 Family Coverage Total Cost Less UM Contribution $327.50 $307.80 $329.60 $307.80 $351.30 $307.80 $376.80 $307.80 $448.40 $307.80 $353.00 $307.80 $327.50 $307.80 Employee Contribution Enrollment $ 0.00 5,069 $ 0.80 326 $ 9.50 533 $ 19.70 564 $ 48.40 375 $ 10.20 291 $ 0.00 182 Total 7,340 Employee Contribution Enrollment $ 19.70 4,179 $ 21.80 354 $ 43.50 718 $ 69.00 747 $140.60 335 $ 45.20 318 $ 19.70 138 Total 6,789 Single & Family Total 14,129 Plan Attributes from University of Minnesota 2003 Choices PLAN CHARACTERISTIC CDHP HMO and PPOs Employer HRA contribution $750 single option $1,500 family option Not applicable Deductible $1,250 single option #1 None $2,500 family option #1 $2,000 single option #2 $4,000 family option #2 None $10-20 office visit co-pay $200 inpatient co-pay (PPO) $0 inpatient co-pay HMO Same as other covered $10 generic services $20 formulary brand $30 non-formulary brand 100% covered 100% covered None, covered under $400 person (HMO) deductible structure. $800 family (HMO) $500 person (PPO) $1,000 family (PPO) Coinsurance/Co-pay Rx coverage Preventive Care Stop-loss limit Chronic Illness Enrollee Attributes by Plan Choice Variable Mean Values Chronic Illness All Enrollees CDHP Enrollees Age in years** No C hronic Illness Enrollees in Other Plans 50.96 52.81 48.8 45.34 0.52 0.42 0.65 0.56 $61.76 $74.38 $47.02 $52.03 Type of contract (family=1, else=0)** 0.56 0.57 0.54 0.44 Number of dependents** 2.28 2.25 2.31 1.78 Number of observations 362 195 167 659 Gender (female=1, male=0) Salary (in ,000s of $)** CDHP Chronic Illness Enrollee Experience with Out of Pocket Cost Sharing – Single Contracts Single Contract Enrollees with Annual Spending Exceeding Deductible Prescription Drugs** Physician Services* Hospital Enrollees with Annual Spending in the Donut Hole Prescription Drugs Physician Services Hospital Enrollees with Annual Spending within Savings Account Limit Prescription Drugs Physician Services Hospital * p<.05; ** p<.01, *** p<.001 Chronic Illness No Chronic Illness (n=62) $2,638 $3,973 $2,621 (n=90) $1,233 $2,865 $2,398 (n=11) $ 484 $1,228 $ 190 (n=41) $ 283 $ 758 $ 250 (n=9) $ 83 $ 99 $ 32 (n=88) $ 62 $ 167 $ 66 CDHP Chronic Illness Enrollee Experience with Out of Pocket Cost Sharing – Family Contracts Family Contract Enrollees with Annual Spending Exceeding Deductible Prescription Drugs** Physician Services Hospital Enrollees with Annual Spending in the Donut Hole Prescription Drugs Physician Services Hospital Enrollees with Annual Spending within Savings Account Limit Prescription Drugs** Physician Services Hospital * p<.05; ** p<.01, *** p<.001 Chronic Illness No Chronic Illness (n=84) $4,364 $6,648 $4,827 (n=63) $1,895 $5,947 $6,963 (n=18) $ 656 $1,447 $ 578 (n=45) $571 $1,535 $559 (n=4) $548 $328 $123 (n=36) $117 $458 $78 Full Replace Impact on Total $$ Total Expenditures Intercept Age (years) Female=1, else 0 Baseline Chronic/Illness Count Catastrophic Shock=1, else 0 Year 2=1, else Year 1 Later Sample=1, else 0 Firm 2=1, else 0 Firm 3=1, else 0 Firm 4=1, else 0 Firm 2 & Year 2 interaction Firm 3 & Year 2 interaction Firm 4 & Year 2 interaction Enrollee is spouse=1, else 0 Enrollee is dependent=1, else 0 Second Year Impact Firm 1 Firm 2 Firm 3 Firm 4 Adjusted R-Square Coefficients 5.2453 0.0160 0.1351 0.3117 0.5976 0.0128 -0.0398 -0.2587 0.0753 -0.0674 -0.0539 0.0229 -0.0222 0.0617 -0.1523 T-Stat 273.76 38.89 16.66 175.66 62.68 1.39 -0.54 -19.61 0.97 -1.18 -2.91 0.28 -0.33 5.66 -10.03 Pr > |t| <.0001 <.0001 <.0001 <.0001 <.0001 0.1657 0.5874 <.0001 0.3343 0.2369 0.0036 0.7815 0.7434 <.0001 <.0001 1.28% -4.11% 3.57% -0.94% 0.384 $$$ are logged for 2006 expenditures from 2005-2006 difference GLM Full Replace Impact on Rx $$ Total Pharmacy Expenditures Intercept Age (years) Female=1, else 0 Baseline Chronic / Illness Count Catastrophic Shock=1, else 0 Year 2=1, else Year 1 Later Sample=1, else 0 Firm 2=1, else 0 Firm 3=1, else 0 Firm 4=1, else 0 Firm 2 & Year 2 interaction Firm 3 & Year 2 interaction Firm 4 & Year 2 interaction Enrollee is spouse=1, else 0 Enrollee is dependent=1, else 0 Second Year Impact Firm 1 Firm 2 Firm 3 Firm 4 Adjusted R-Square Coefficients 3.3627 0.0376 0.0459 0.2296 -0.0966 0.0979 -0.1814 -0.4840 0.5472 -0.1162 -0.0580 -0.2972 -0.1121 -0.0091 0.2454 T-Stat 131.73 70.17 4.18 99.41 -7.69 7.97 -1.84 -26.94 5.24 -1.52 -2.29 -2.70 -1.23 -0.63 12.10 Pr > |t| <.0001 <.0001 <.0001 <.0001 <.0001 <.0001 0.0658 <.0001 <.0001 0.1291 0.022 0.0069 0.2174 0.5257 <.0001 9.79% 3.99% -19.93% -1.42% 0.256 $$$ are logged for 2006 expenditures from 2005-2006 difference GLM Summary How are Chronically ill CDHP-enrollees different than nonCDHP enrollees? Younger, wealthier with larger family size. How does CDHP enrollee expenditures change with respect to a chronic illness? Significantly higher, usually by a factor of 2. Is there a different story for the chronically ill when they face a CDHP full replacement? No. Just are higher for this group as well. Chronically ill patients have higher costs in CDHPs, regardless of plan choice. Outcomes impact needs more study. CDHPs, Chronic Illness & Health Reform Needs a new paradigm (like I need a new sweater) A. Rewards in premium reduction for active management. B. Consumers/providers get the data to make via web with results in near real time. C. Most majority reform proposals hint ‘the experiment is over.’