Impact of Expansion of Specialty Consultation Practice Medicaid High Risk Pregnancies
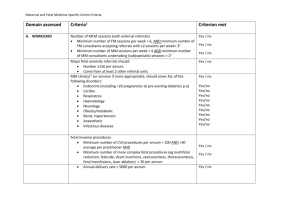
advertisement
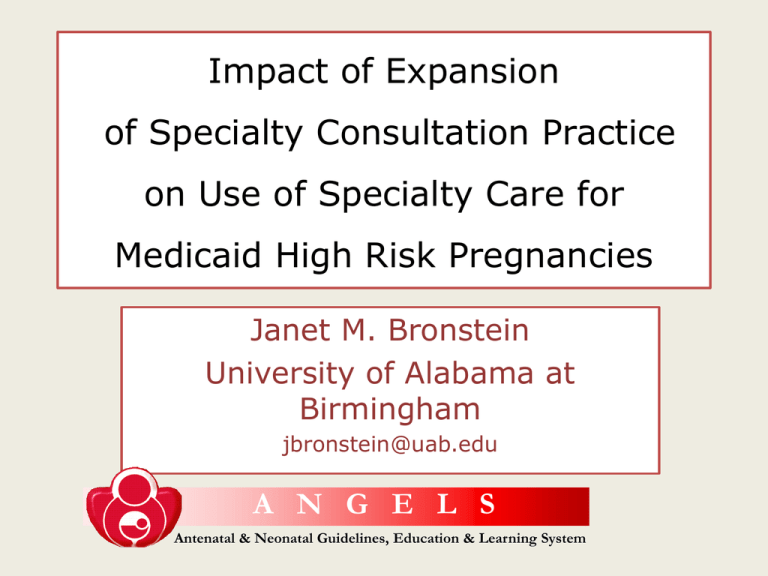
Impact of Expansion of Specialty Consultation Practice on Use of Specialty Care for Medicaid High Risk Pregnancies Janet M. Bronstein University of Alabama at Birmingham jbronstein@uab.edu A N G E L S Antenatal & Neonatal Guidelines, Education & Learning System A N G E L S Antenatal & Neonatal Guidelines, Education & Learning System • Co-authors at the University of Arkansas for Medical Sciences – – – – Songthip T. Ounpraseuth, Ph.D. Jeffrey Jonkman, Ph.D. David Fletcher, M.B.A Curtis Lowery, M.D. • Co-authors at the State of Arkansas – Judith McGhee, M.D. (Medicaid Agency) – Richard Nugent, M.D., M.P.H. (Department of Public Health) Medicaid covers a large portion of U.S. pregnancies – many are high risk ANGELS – Arkansas Medicaid supported expansion of UAMS MFM consulting service Case Management Education & Support for OB Providers Evidence Based Guidelines Clinical Research 24/7 Consultation Call Center Expansion of Telemedicine Network & Clinics Evaluation of ANGELS (Phase one, 20012005, intervention started April 2003) • Did ANGELS increase the proportion of – Maternal Fetal Medicine (MFM) consults for targeted diagnoses? – MFM consults for other reasons? – Deliveries of infants younger than 35 weeks at neonatology-staffed NICU? Consults and NICU deliveries are special cases of physician referral behavior • Making the Referral • Norms for referral (boundaries of expertise), professional networks, pressures to retain patients – ANGELS and health care market factors • Completing the Referral • Enabling characteristics, awareness of pregnancy risk, relationship with primary provider – Demographics and care factors Consults and NICU deliveries are special cases of physician referral behavior • ANGELS and health care market factors – Guidelines, calls to call center, site for MD tele-rounds, remote patient consult site – Presence of OB or GP or no maternity, beds and MDs per capita, sites claiming to do high risk OB and have NICUs • Demographics and care factors – Education, age, race, parity, ethnicity, partner status, county poverty level, % Black, rural, distance – Adequacy of prenatal care, initial care in health dept, gestation at delivery, any MFM consult (for delivery at NICU) Methodology Data • Medicaid claims for pregnancy 2001-2005, clustered into episodes, linked to birth certificates. Total 91,902 live births. • County ARF and AHA data for residence and contiguous counties linked to the episodes. • MFM analysis excludes Little Rock. NICU analysis includes only births < 35 weeks gestation. Statistical Approach • Time series logistic regression with standard errors corrected for county clustering. • Time trend, distance to specialist and distance to closest NICU hospital controlled Trends in Outcome Measures 2001 2002 2003 Angels began 2004 Angels 2005 Angels MFM with 28.7% targeted DX (n=30,364) 30.4% 27.5% 25.6% 24.3% 17.8% MFM no targeted DX (n=47,410) 18.4% 16.0% 12.2% 12.3% 40.3% 40.5% 45.3% 45.0% 43.6% NICU delivery (n=4,531) Impact of ANGELS measures on care delivery (O.R., 95% C.I., p value) MFM for targeted DX MFM for other DX Delivery at NICU Guidelines in active draft 0.99 (0.99,1.00) 1.00 (0.99,1.01) 1.02 (1.01,1.04)** Cumulative guidelines completed 0.98 (0.98,0.99)*** 0.98 (0.98,0.99)*** 1.00 (0.99, 1.01) MD calls from county 0.91 (0.74,1.13) 0.71 (0.54,0.93)* 1.22 (0.94,1.57) PT calls from county 1.68 (1.33,2.11)*** 2.59 1.60 (1.82, 3.69)*** (1.13,2.27)** Teleconference site 1.03 (0.71,1.48) 1.16 (0.80, 0.70) 0.29 (0.18,0.45)*** Clinical remote site 1.26 (0.90,1.77) 1.36 (0.80,2.32) 1.88 (1.22,2.89)** * P < .05, ** p<.01, *** p< .001 Impact of Health Care Market measures on care delivery (sign, p value) MFM for targeted DX MFM for other DX Delivery at NICU Other MD vs OB - (p=.06) -*** +*** No maternity vs OB +* +* +*** Reports NICU (no (ns) (ns) -*** in cty +*** contig cty Reports high risk OB (no MFM) (ns) - (p=.05) -** MDs per capita -* - (p=.07) +** in cty, -*** contig cty Beds per capita +*** +*** +*** neonatologist) * P < .05, ** p < .01, *** p < .001 Impact of individual demographic measures on care delivery (sign, p value) MFM for targeted DX MFM for other DX Delivery at NICU Black/other vs white (ns) (ns) (ns) Hispanic vs not -*** -* +* Education (ns) + low (p=.07) - High ** -low* + high*** Age (ns) - >34 *** -Teen* Partner status vs married + without* + without*** (ns) % cnty Black +* +* +* % cnty < FPL -*** -** -*** (ns) -** +*** Rural county * P < .05, ** p < .01, *** p < .001 Impact of individual care measures on care delivery (sign, p value) MFM for targeted DX Multiple birth MFM for other DX Delivery at NICU +** + p=.05 (ns) + 25 -31wks** + 32-33 wks p=.06 (ns) +*** (most common for 25-27 wks) (ns) + high parity* + first birth*** Adequacy of Prenatal care + intensive*** + intensive*** -Intermed.*** + inadeq.*** Initial care in Health Dept +*** +*** -*** Health Dept X time -*** -*** +*** MFM visit ------ ----- +*** Gestational age at delivery vs oldest Parity * P < .05, ** p < .01, *** p <.001 Conclusions • Medicaid-supported expansion of academic MFM consulting service is altering delivery of maternity care in Arkansas – Increasing local expertise, decreasing specialty visits – Increasing use of neonatology-staffed NICU for preterm deliveries • Local expertise competes with more distant specialists, may lead to less appropriate care. Thank You A N G E L S Antenatal & Neonatal Guidelines, Education & Learning System