Time is Money: The Value of Time Spent States Julia Prentice*
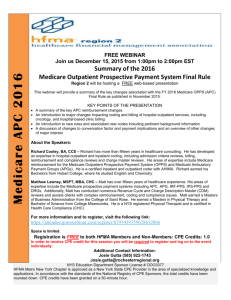
advertisement

Time is Money: The Value of Time Spent Waiting for Health Care in the United States Julia Prentice* Health Care Financing and Economics, Boston VA Healthcare System and Boston University School of Public Health Steve Pizer Health Care Financing and Economics, Boston VA and Boston University School of Public Health *Support was provided under Grant No. IAD 06-112 from the Department of Veteran Affairs, Health Services Research and Development Service and Grant No: 62967 from the Health Care Financing and Organization Program under the Robert Wood Johnson Foundation. Waiting is a Price • Number of days between appt. request and day appt. is scheduled • Reconciles gap between demand and supply when prices are too low • Outpatient waiting times have been low - Postpone Medicare reimbursement rate cuts • Proposed health reform may increase waits - Stimulate demand but no supply expansion Insurance Reform + Cost Control = Waiting Research Objective • Examine the time/cost tradeoff veterans make when choosing health care - How much more will veterans pay to avoid long waits? Choose Between Two Systems • VA - Low out of pocket cost to patients - Long waits • Medicare - Higher out of pocket cost to patients - Shorter waits Study Population • Veterans eligible for Medicare and VA - Respondents to the MCBS survey who served in armed forces - Non-institutionalized - MCBS 2001-2003 - n=1513 • Exclude respondents with employersponsored health insurance or Medicaid Data sources • MCBS 2001-2003 - Medicare insurance choice - FFS, HMO or Medigap - Medicare outpatient utilization • VA administrative/encounter data - VA facility level wait times - VA outpatient utilization • Medicare Personal Plan Finder/Insurer for HMO and Medigap plans - Annual premium Methodological Approach 1) Predict number of VA and Medicare outpatient visits - Accounting for VA wait time 2) Predict Medicare plan choice - Accounting for VA and Medicare outpatient utilization 3) Policy simulation - Increase VA wait time- what happens to Medigap market share? Methodological Approach 1) Predict number of VA and Medicare outpatient visits - Accounting for VA wait time 2) Predict Medicare plan choice - Accounting for VA and Medicare outpatient utilization 3) Policy simulation - Increase VA wait time- what happens to Medigap market share? First Stage Equation • Dependent variables - Number of VA visits in a year - Number of Medicare visits in a year • Main independent variable - VA facility level wait time averaged over the year - Average wait until next available appt. for new patients - Wait time at VA facility nearest to respondent • Zero-inflated negative binomial - Accounts for heaping at 0 -69% had no VA visits, 11% had no MCR visits Zero-Inflated Negative Binomials Predicting # of VA outpatient visits Independent Variables Facility average wait time in days β -0.0064 Robust P-Value Standard Error 0.0072 0.373 Predicting # of Medicare Outpatient Visits Facility average wait 0.0103 0.0049 time in days 0.034 *Model also includes non-VA health insurance options in county, VA priority status, distance to nearest VA facilities, year dummies, demographics (e.g. education, gender), lagged chronic conditions and hospital referral regions. First Stage Conclusion Longer VA wait time Higher Medicare utilization Methodological Approach 1) Predict number of VA and Medicare outpatient visits - Accounting for VA wait time 2) Predict Medicare plan choice - Accounting for VA and Medicare outpatient utilization 3) Policy simulation - Increase VA wait time- what happens to Medigap market share? Second Stage Equation Nested Logit Predicting Medicare Plan Choice FFS HMO 1-RX 2-RX 3-No RX Medigap 1-RX 2-No RX • Main independent variables - Annual premium of Medicare option - VA and Medicare outpatient utilization Nested Logit* Predicting Medicare plan chosen Top level- FFS, HMO or Medigap β Standard Error VA outpatient visits -0.1746 0.0348 <0.0001 Medicare outpatient visits -0.0658 0.0117 <0.0001 VA outpatient visits -0.2058 0.0282 <0.0001 Medicare outpatient visits 0.0414 0.0069 <0.0001 HMO P-Value Medigap Bottom level- Specific Plan Characteristics Annual premium -0.0007 0.00006 <0.0001 *Model also includes coverage, VA and Medicare outpatient utilization interacted with coverage and premium and the residual from the negative binomial equations in stage 1 in the top level and interacted with coverage and annual premium in the bottom level. First and Second Stage Conclusion Longer VA wait time Higher Medicare utilization Increased probability of choosing Medigap Methodological Approach 1) Predict number of VA and Medicare outpatient visits - Accounting for VA wait time 2) Predict Medicare plan choice - Accounting for VA and Medicare outpatient utilization 3) Policy simulation - Increase VA wait time- what happens to Medigap market share? Policy Simulation • Increase VA wait time by 1 standard deviation - Add 9.83 days • Predict expected number of VA and Medicare outpatient visits - Use increased wait time • Use this revised prediction in choice model -Predict change in probability of choosing Mgap • Decrease Mgap premium by 1 standard deviation - Subtract $615 - Predict change in choosing Mgap VA Wait Time Policy Simulation Results Increase VA Facility Wait time Baseline Simulation % Change VA wait time 42.27 52 23 Medigap market share 0.50 0.53 6 (probability) Elasticity Medigap market share/Wait: 6/23=0.26 Medigap Premium Policy Simulation Results Decrease Medigap premium Baseline Simulation % Change Medigap premium Medigap market share (probability) 2106 1491 29 0.50 0.59 15 Elasticity Medigap market share/Premium: 15/29=0.52 Conclusions Evidence of Time/Money Tradeoff Longer VA wait time Higher Medicare utilization Increased probability of choosing Medigap Conclusions ● Increase VA wait time Mgap market share - Elasticity=0.26 ● Decrease Mgap prem Mgap market share - Elasticity=0.52 ● Similar elasticities to previous research on health care choices ● Wait times influence health care choice Contact Information Julia Prentice* Health Care Financing and Economics Boston VA Healthcare System and Boston University School of Public Health Julia.Prentice@va.gov; jprentic@bu.edu Steve Pizer Health Care Financing and Economics, Boston VA and Boston University School of Public Health Steven.Pizer@va.gov, pizer@bu.edu