The Effect of Plan Design on Utilization: a
advertisement
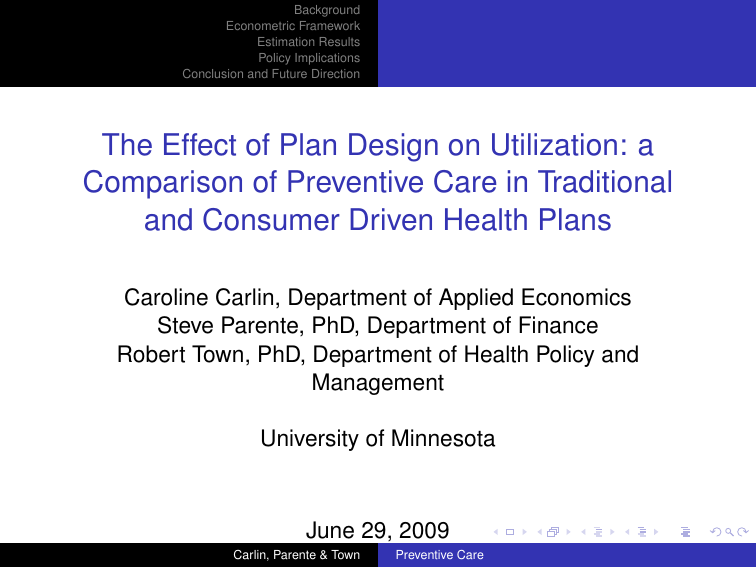
Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction The Effect of Plan Design on Utilization: a Comparison of Preventive Care in Traditional and Consumer Driven Health Plans Caroline Carlin, Department of Applied Economics Steve Parente, PhD, Department of Finance Robert Town, PhD, Department of Health Policy and Management University of Minnesota June 29, 2009 Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Outline Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction This is work in progress – comments are welcome! Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Background I Preventive care, particularly cancer screening, has been shown to improve mortality I There have been significant increases in patient copayments, especially through high-deductible consumer-driven health plans (CDHPs). There is concern that this patient cost sharing will discourage care (Dixon et al 2008) I I Even when preventive care is fully covered in a CDHP, there is concern that confusion on the part of the consumer leads to reduced preventive care. Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Background A number of studies have compared a CDHP group with traditional plan groups, where preventive services are fully covered, or have a minimal copayment, and found little difference in rates of preventive services. I Busch, et al (2006), took advantage of a natural experiment when Alcoa mandated high-deductible coverage for a subset of employees. I I I I Controls were union groups – unobserved differences? Rowe et al, 2008 found little difference in preventive care utilization after the first year. 89% of the CDHP population had another plan option – selection? Wilson et al (2009) compare CDHP to CMM enrollees with controls for observable characteristics. I No attempt to adjust for selection. Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Background Wharam, et al (2008), is one of the few studies that looks at the impact of a CDHP plan on preventive care use in a controlled setting. I Treatment group had employer-mandated CDHP coverage I Control group had HMO coverage with no CDHP option I Found little evidence of plan-induced change in rates of cancer screening. Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Background Wharam, et al (2008), is one of the few studies that looks at the impact of a CDHP plan on preventive care use in a controlled setting. I Treatment group had employer-mandated CDHP coverage I Control group had HMO coverage with no CDHP option I Found little evidence of plan-induced change in rates of cancer screening. May still be some selection impact at the employer level, or to coverage at the spouse’s employer. We add to the literature by explicitly controlling for selection. Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Study Setting I Our data come from a large Twin Cities-based employer. I Panel data include detailed claims and enrollments for 2002 through 2004. 9231 employees included I I Dependents excluded to avoid interfamily correlations I Employees choose between an HMO, two POS plans, and a CDHP. I Used CPT-4 code and ICD9 code information to identify preventive care. Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Study Setting Ad hoc changes in employer’s contribution philosophy provided exogenous variation in premiums across years, providing an instrument for the selection correction. 2002 2003 Annual Annual Share Share Premium Premium 2004 Annual Share Premium 2005 Annual Share Premium .622 $0 .688 $0 .688 $382 .686 $408 Tier 1 .077 $0 .044 $21 .040 $741 .047 $770 POS 1 Tier 2 .096 $242 .082 $247 .080 $1,064 .072 $1,074 Tier 3 .073 $522 .095 $512 .050 $1,474 .031 $1,721 POS 2 .090 $1,346 .060 $1,258 .064 $1,463 .086 $783 CDHP .041 $329 .061 $194 .074 $670 .073 $793 HMO Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Study Setting I All patients were assumed to be eligible for general preventive care visits I I preventive care visit (41% of 9231) Patients with prior history or ineligible age/gender were excluded for I I I Mammography (49% of 3447) Pap smear (18% of 4459) Colonoscopy (7.5% of 6428) Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Study Setting Predictive variables in the model include I Demographic information: age, gender, income I Diagnosis-based risk measure developed from the Johns Hopkins ACG software, a "concurrent weight" (CW) capturing health status as a relative measure of expected claims in the current year. I The office visit copay level (waived for preventive care) Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Selection Correction I I We estimated a joint choice and utilization model to facilitate adjustment for selection effects. Extending the methods used in Deb et al (2006) to a multinomial setting, we included the unobserved heterogeneity from the choice model utility equations as a covariate in the probit utilization equations. I This term was significant only in the cervical cancer screening equation. Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Choice Model Introduction The analysis uses a multinomial probit framework, with temporally correlated errors. Wijt = Uijt − Ui6t = xijt0 β + ijt for individual i = 1, ..., 3578 choice j = 1, ..., 5, and time t = 1, ..., 3 Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Choice Model Introduction The analysis uses a multinomial probit framework, with temporally correlated errors. Wijt = Uijt − Ui6t = xijt0 β + ijt for individual i = 1, ..., 3578 choice j = 1, ..., 5, and time t = 1, ..., 3 Where it = i1t . . . i5t ∼ MVN (0, Σ) Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Choice Model Introduction The analysis uses a multinomial probit framework, with temporally correlated errors. Wijt = Uijt − Ui6t = xijt0 β + ijt for individual i = 1, ..., 3578 choice j = 1, ..., 5, and time t = 1, ..., 3 Where it = i1t . . . i5t ∼ MVN (0, Σ) and AR(1) errors: ijt = ρj ij,t−1 + ηijt , with ηijt ∼ N(0, τj2 ) Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Choice Model The complexity of the model required estimation with Bayesian methods, rather than classical maximum likelihood methods. I A key component of Bayesian estimation of discrete choice models is the data augmentation process (Tanner & Wong 1987) I The latent utility is sampled from its posterior distribution, constrained by the observed choice pattern I This allows us to "observe" the latent utility, and thus compute the unobserved heterogeneity for inclusion in the preventive care model Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Preventive Care Utilization Model Probit equations were estimated for the four types of preventive services, with individual intercepts used to control for temporal correlation and capture correlation across equations. The latent variables for person i at time t enrolled in plan j had the form Vitjp = zitj0 βjp + bip + γ p itj + ωitjp Vitjcc = zitj0 βjcc + bicc + γ cc itj + ωitjcc Vitjco = zitj0 βjco + bico + γ co itj + ωitjco Vitjm = zitj0 βjm + bim + γ m itj + ωitjm The vector of individual intercepts, bi , is assumed to be N(0, D). The errors ωitj were assumed to be iid N(0, 1). Testing of a more complex covariance structure resulted in covariances that were statistically significant, but not meaningfully large. Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Choice Results - Mean parameters The parameters predicting the means of the plan utilities followed a logical pattern: I Those who are female and older prefer plans that have less tightly managed care I Typically-unobservable health status, measured by the CW, was also significant, with sicker individuals preferring less tightly managed plans I The impact of increasing premiums and the office visit copay was negative and highly significant Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Choice Results - Covariance Structure The estimated AR(1) coefficients are quite high, indicating significant "stickiness" in plan elections. The AR(1) coefficient for the HMO is 0.70, and greater than 0.90 for all other plans. We find a variance-covariance matrix with off-diagonal elements significantly different from zero, and strong evidence of heteroskedasticity. HMO POS 1, Tier 1 POS 1, Tier 2 POS 1, Tier 3 POS 2 HMO 1.0000 Across-Plan Variance-Covariance Matrix (std dev) POS 1, Tier 1 POS 1, Tier 2 POS 1, Tier 3 POS 2 0.2035 *** 0.2164 *** (0.0325) (0.0306) -0.0510 ** 0.0780 *** 0.1969 *** (0.0225) (0.0215) (0.0324) -0.0583 ** 0.0387 * 0.1407 *** 0.2509 *** (0.0317) (0.0225) (0.0299) (0.0402) 0.1817 *** -0.0061 -0.0007 0.0645 *** 0.2614 *** (0.0382) (0.0184) (0.0227) (0.0293) (0.0478) * 90% Bayesian Confidence Interval excludes zero ** 95% Bayesian Confidence Interval excludes zero *** 99% Bayesian Confidence Interval excludes zero Carlin, Parente & Town Preventive Care POS 1, Tier 1 0.2035 *** 0.2164 *** Background (0.0325) (0.0306) Econometric Framework Estimation POS 1, Tier 2 -0.0510 ** Results 0.0780 *** 0.1969 *** Policy Implications (0.0225) (0.0215) (0.0324) Conclusion and Future Direction POS 1, Tier 3 -0.0583 ** 0.0387 * 0.1407 *** 0.2509 *** (0.0317) (0.0225) (0.0299) (0.0402) POS 2 0.1817 *** -0.0061 -0.0007 0.0645 *** 0.2614 * (0.0382) (0.0184) (0.0227) (0.0293) (0.0478) Results - Covariance Structure 90% Bayesian Confidence Interval excludes zero It is***instructive to construct the implied correlations coefficients, 95% Bayesian Confidence Interval excludes zero several which exceed *** 99%of Bayesian Confidence Interval25%. excludesThis zero is strong evidence that the IIA assumption is not appropriate in this employer’s population. Implied Across-Plan Correlation Coefficients HMO POS 1, Tier 1 POS 1, Tier 2 POS 1, Tier 3 POS 1, Tier 1 0.4375 POS 1, Tier 2 -0.1150 0.3780 POS 1, Tier 3 -0.1164 0.1663 0.6331 POS 2 0.3555 -0.0256 -0.0032 0.2518 Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Preventive Care Results I The parameters on the utility errors were statistically significant only for the cervical cancer screening. I The Preventive Care model reproduced the actual visit patterns well. I A traditional random-effect probit model with the same covariate structure (excluding utility errors) was also estimated. I An intercept-only model was also estimated. Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Preventive Care Results We see better accuracy in prediction within the proposed model. Preventive Cerv Cancer Colonoscopy Mammography % Correctly Predicted Correlated Probit with Selection & Panel Probit Intercept Ind'l Effects w/ Rand Eff Only Model 81.9% 67.7% 51.5% 87.6% 78.6% 71.1% 93.0% 87.9% 86.0% 77.2% 63.0% 50.0% Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Preventive Care Results The proposed model reproduced the visit rates well within plan-visit type cells. The traditional model under-predicts pap smear rates. Actual Visit Rate Preventive Cerv Cancer Colonoscopy Mammography hmo 39.3% 8.9% 6.0% 49.1% pos 46.0% 33.7% 9.9% 51.4% cdhp 42.7% 24.7% 9.8% 51.2% total 41.3% 17.2% 7.4% 50.0% Preventive Cerv Cancer Colonoscopy Mammography Expected Visit Rate -- Bayesian Model hmo pos cdhp total 38.8% 45.1% 40.6% 40.6% 7.6% 34.4% 21.2% 16.3% 4.6% 8.2% 7.4% 5.9% 50.0% 50.5% 46.8% 50.0% Preventive Cerv Cancer Colonoscopy Mammography Expected Visit Rate -- Traditional Model hmo pos cdhp total 38.2% 45.2% 41.8% 40.4% 2.2% 22.5% 14.1% 8.9% 4.4% 8.2% 7.8% 5.8% 48.9% 50.3% 51.2% 49.5% Carlin, Parente & Town Preventive Care Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Predicted Visit Rates by Age We see very little differences in rates by age among the health plan types in three of the visit types, but we do see a difference in the cervical cancer screening rates. General Preventive Care Visit by Age Colonoscopy by Age 0.7 0.16 0.14 0.5 HMO 0.4 POS 0.3 CDHP 0.2 Prob(Visit) Prob(Visit) 0.6 0.1 0.12 0.1 0.08 HMO POS 0.06 0.04 0.02 0 CDHP 0 25 30 35 40 45 50 55 60 65 25 30 35 40 Age 50 55 60 65 Mammography by Age 0.45 0.4 0.35 0.3 0.25 0.2 0.15 0.1 0.05 0 0.7 0.6 HMO POS CDHP Prob(Visit) Prob(Visit) Cervical Cancer Screen by Age 45 Age 0.5 HMO 0.4 POS 0.3 CDHP 0 2 0.2 0.1 0 25 30 35 40 45 50 55 60 65 25 30 35 Age 40 45 Age Carlin, Parente & Town Preventive Care 50 55 60 65 Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Predicted Visit Rates by Health Status We see similar differences by health status. Colonoscopy by Health Status 0.16 0.14 0.12 HMO POS CDHP Prob(Visit) Prob(Visit) General Preventive Care Visit by Health Status 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 0.1 HMO 0.08 POS 0.06 CDHP 0.04 0.02 0 0 0.2 0.4 0.6 0.8 1 1.2 0 0.2 0.4 log(current health status) 0.8 1 1.2 Mammography by Health Status Cervical Cancer Screen by Health Status 0.7 0.45 0.4 0.35 0.3 0.25 0.2 0.15 0.1 0.05 0 0.6 HMO POS CDHP Prob(Visit) ob(Visit) Prob(Visit) ob(Visit) 0.6 log(current health status) 0.5 HMO 0.4 POS 0.3 CDHP 0.2 0.1 0 0 0.2 0.4 0.6 0.8 log(current health status) 1 1.2 Carlin, Parente & Town 0 0.2 Preventive Care 0.4 0.6 0.8 log(current health status) 1 1.2 Background Econometric Framework Estimation Results Policy Implications Conclusion and Future Direction Conclusion and Future Direction I We see that methods do matter – there is evidence of selection in at least one visit type, with a corresponding difference in predicted rates by method. I Leveling the financial playing field for preventive care, even within high-deductible plans, appears to be primarily a successful strategy – we need to look more closely at rates of cervical cancer screening. I We will look at drug compliance for those with chronic illnesses, where the deductibles impact the cost sharing, applying the same selection correction process. Carlin, Parente & Town Preventive Care