The Aging of the Rural Dentist and g g
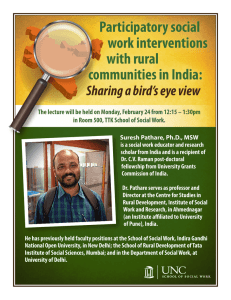
advertisement

The Aging g g of the Rural Dentist and Primary Care Physician Workforce: Are Some Locations More Vulnerable than Others? Mark Doescher, MD, MSPH, Director Meredith Fordyce, PhD, Research Scientist Susan Skillman, MS, Deputy Director WWAMI Rural Health Research Center University of Washington Acknowledgments This University of Washington WWAMI Rural H lth R Health Research hC Center t study t d was ffunded d db by th the Office of Rural Health Policy, Health Resources and Services Administration Administration, Department of Health and Human Services Why is This Study Important? Why is this Study Important? • Large numbers of “baby boomer” dentists and physicians are approaching traditional retirement ti t age. • This is occurring at a time in which: – ffewer new dentists d ti t and d physicians h i i are choosing h i the generalist specialties that form backbone of the rural p physician y workforce. – the aging U.S. population requires more dentist and physician services. Why is this Study Important? • As the baby-boom generation advances into old age, the need for complicated dental and medical di l services i will ill iincrease. • For example, elderly people are much more likely to retain their teeth than a generation ago, so they will require much more care than in the past past. Why is this Study Important? • Familyy p physicians y have a mean retirement age g of 65.0 years (and a median age of 63.7 years). • Retirement age may be lower for dentists, e.g., intended retirement is 62 years. • Historically, female physicians retire four years earlier than their male counterparts Why is this Study Important? • Many rural areas already face shortages of generalist dentists (GDs) and primary care physicians (PCPs). • The additional strain that impending dentist and PCP retirement will cause in rural areas is not well understood. Goals • To begin e exploring ploring the impact of an aging rrural ral GD and PCP workforce, this study identifies rural locations with high proportions of these professionals nearing retirement age. • This study is the first national study to quantify the extent to which the problem of rural GD and PCP shortages may be exacerbated by an aging workforce. Study Design • Cross-sectional prevalence study of GDs and PCPs • Generalist G li t D Dentists ti t (GD (GDs)) – general practice – pediatric dentistry • Primary Care Physicians (PCPs) – family/general yg p practitioners – general internists – general pediatricians Study Design • Near-retirement age GDs and PCPs are defined as those 56 or older. • Young GDs and PCPs are defined as those 39 or younger Study Design • National -,, state-,, and county-level y analyses y performed. • Locations were categorized by the proportions o near-retirement providers. • Locations in the upper percentiles of the distribution were classified as “high-risk” high-risk areas. Study Design Data sources 1. 1 2. 3 3. 4. 2008 ADA Masterfile 2005 AMA and AOA Masterfiles 2005 and 2008 Area Resource Files 2005 and 2008 Claritas population estimates Study Populations • We identified 10,977 rural GDs and 27,681 , rural PCPs who were – clinically active; – not in residency training; – not federally employed; and – aged 74 or younger younger. Rural/Urban Designations • Metropolitan • Non Non-Metropolitan Metropolitan Overall •N Non-Metropolitan M t lit Adjacent Adj t tto M Metro t • Micropolitan p not Adjacent j • Remote Non-Core Analyses • Analyses presented today are descriptive. p Results Number of 2008 Generalist Dentists Metropolitan NonN Metropolitan Adjacent to Metro Micropolitan not Adjacent Remote Non-Core NonMetropolitan Overall All Dentists 92,743 7,469 3,039 1,727 12,235 GD GDs 75 999 75,999 6 777 6,777 2 603 2,603 1 652 1,652 10 977 10,977 Dentist Type: Number of 2005 Primary Care Physicians Metropolitan NonN Metropolitan Adjacent to Metro Micropolitan not Adjacent Remote Non-Core NonMetropolitan Overall All Physicians 517,859 35,132 15,357 7,127 57,616 PCP PCPs 178 331 178,331 17 191 17,191 6 220 6,220 4 270 4,270 27 681 27,681 Physician Type: Percentage of 2008 Dentists and 2005 Physicians Aged 56 Years or Older Provider Type: Metropolitan NonMetropolitan Micropolitan Adjacent to not Metro Adjacent Remote Non-Core NonMetropolitan Overall GDs 37.6% 42.7% 40.4% 43.9% 42.3% PCP PCPs 25 5% 25.5% 26 9% 26.9% 28 0% 28.0% 28 9% 28.9% 27 5% 27.5% Percentage of Generalist Dentists Aged 56 Years or Older and Aged g 39 or Younger, g 2008 50% 40% 44% 43% 42% 40% 38% 30% 20% 15% 15% 15% N M Non‐Metro L Large Rural R l 17% 15% 10% 0% M Metro > 56 years old < 39 years old SSmall ll Rural IIsolated l d Small Rural Percentage g of Primary y Care Physicians y Aged g 56 Years or Older and Aged 39 or Younger, 2005 30% 28.9% 28.0% 27.5% 26.9% 25.5% 25% 22.5% 20.8% 20.5% 20% 20.0% 20.2% 15% Metropolitan Non-Metropolitan Non Metropolitan Overall ³ 56 years old ² 39 years old Non-Metropolitan Non Metropolitan Micropolitan Adjacent to Metro Not Adjacent Remote Non-Core 4 2008 Rural County Characteristics by “Near NearRetirement GD” Upper Decile and “No GD” Status Near Retirement GD (n=297) No GD (n=335) Other Rural (n=1419) White 89.3% 85.2% 87.6% Low Education county* 26.6% 30.5% 24.4% Persistent Poverty county 14.5% 24.4% 18.1% Population Loss county* 32.0% 44.8% 20.2% Retirement Destination county * 15.8%. 8.9% 14.2% Population density* 44 9/sq mi 44.9/sq.mi. 11 8/sq mi 11.8/sq.mi. 51 1/sq mi 51.1/sq.mi. GDs per 100K population † 20.5 N/A 24.3 * p<0.01 † p<0.001 2005 Rural Countyy Characteristics byy “NearRetirement PCP” Upper Decile and “No PCP” Status Near Retirement PCP (n=184) No PCP (n=166) Other Rural (n=1514) White 83.5% 85.5% 85.2% Low Education county* 34.2% 20.5% 22.9% Persistent Poverty county† 25.5% 15.7% 15.2% Population Loss county* 38.6% 48.2% 20.9% Retirement Destination county † 10.3%. 7.8% 15.1% Population density* 22 2/sq mi 22.2/sq.mi. 34 5/sq mi 34.5/sq.mi. 49 8/sq mi 49.8/sq.mi. PCPs per 100K population † 37.9 N/A 57.8 * p<0.01 † p<0.001 Conclusions Conclusions • Nationally, rural counties have a significantly higher proportion of GDs and PCPs nearing retirement age. Conclusions • Recent trends in career choice and practice location indicate that shortages arising from provider attrition will grow. Conclusions • Rural counties with near-retirement near retirement GDs were characterized by: – Population loss • Rural counties with near-retirement PCPs were characterized by: – High rates of poverty – low levels of educational attainment – Population loss – Low population density – Low PCP densityy Conclusions • Rural counties in which no GDs/PCPs were identified have: - Low socioeconomic status – High rates of population loss – Low population density Potential Solutions • Bolster the numbers of graduates entering rural practice: – Improve K-12 and college student preparation for rurall h health l h care careers – Adopt admissions policies that serve rural health care needs – Expand rural health care training opportunities as core educational curricula – Provide financial and life life-style style support for practicing rural GDs and PCPs. Potential Solutions • Accurate data are needed to identify rural communities most at risk for shortages due to GD and/or PCP retirement. • Once high risk communities are identified, impending p g GD or PCP retirement-related shortages could be mitigated by…