Medicare Managed Care and Primary Care Quality: Examining Racial/Ethnic Effects across States
advertisement

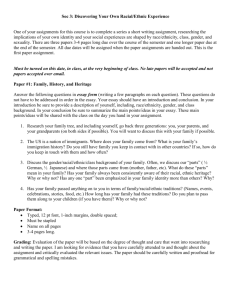
Medicare Managed Care and Primary Care Quality: Examining Racial/Ethnic Effects across States Jayasree Basu, Ph.D. AcademyHealth, 2009 Session title: Disparities Background Medicare Modernization Act of 2003 sparked renewed interest in Medicare managed care (MMC) Medicare spends about $10 billion more each year on beneficiaries enrolled in MMC plans —calls for evaluation Understudied topic: program’s effectiveness in reducing racial and ethnic disparities in quality of health care delivery and access Study Objective To assess the role of MMC plans in providing quality primary care compared to FFS Medicare in three states (NY, CA, FL) across three racial ethnic groups (White, African American, and Hispanic) The performance will be measured in terms of providing better quality primary care, defined as lowering the risk of preventable hospital admissions Hypotheses Managed care plans will reduce preventable hospitalizations (PH) across racial groups through care coordination and provision of preventive care Relative to FFS, improved care coordination in HMO plans will reduce PH for minorities more than whites H1: PHMA < PH FFS H2: PHMA(Minorities|Whites) < PH FFS(Minorities|Whites) Patient Selection States : NY, CA, FL, Year: 2004 Hospitalized Medicare FFS and Medicare advantage (MA) plan enrollees (Age 65 and over) Patient level data on MA versus FFS enrollment as recorded in the confidential files of discharge database of the three states All three states had higher penetration than US average in 1994 increasing further by 2000. CA reached 54% penetration rate By 2000. MMC penetration by State and US 2000 CA NY FL US 1998 1996 1994 0% State source: InterStudy 20% 40% 60% Data NY CA FL Hospital discharge data (HCUP-SID, AHRQ) for elderly Medicare (age 65+), 2004 Medicare managed care plans available in 2004 were predominately HMO types (96-99%) Inpatient discharge data linked to area resource files, US Census, AHA, Interstudy, HRSA’s spatial data warehouse Multivariate cross sectional framework with patient-level data for each State Variables Individual patient characteristics: – – Three Racial ethnic groups Whites African Americans (AA) Hispanics Type of insurer, age groups, gender, severity of illness, indirect severity indicators, severity*HMO, race*HMO Contextual data: socio-demographic conditions and provider characteristics in each Primary care service area (PCSA) where patients live – PCSA : smallest geographic area considered as discrete service area for primary care--validated in previous research Design PH admissions compared with admissions for “marker conditions” for each State in each Racial group PH Marker • Sensitive to primary care • Urgent, insensitive to primary care • Ex: Severe ENT infections, UTI, COPD, Tuberculosis, Hypertension etc., • Appendicitis with appendectomy, acute MI, gastrointestinal obstruction, fracture of hip/femur Analysis Unit of analysis = patients Multivariate Logistic regression models with odds of PH admission compared to marker admission – by each Racial group and Pooled models – multilevel data, adjusting for area-level clustering, by state RESULTS Odds ratios < 1 in all racial groups in each state, and lower for minorities than whites Odds Ratios CA FL PH versus marker 0.85 0.93 0.89 0.82 0.75 (PH/marker) MA = (PH/marker) FFS ---------------------------------------------------------0.82 0.70 0.71 1.30 1.20 1.10 1.00 0.90 0.80 0.70 0.60 0.50 0.40 NY White AA Hispanic % Difference in Odds of PH Admissions: MA versus FFS Enrollees White AA Hispanic CA -18 -30 -29 NY -7 N.S. -15 FL -11 -18 -25 CA and FL had greater reductions in PH among MA enrollees by racial groups, minorities in particular Odds Ratios of PH Admissions versus Marker Admissions: Race*HMO Interactions AA / White CA NY FL 0.83 (p=.000)* N.S. 0.90 (p=.153) Hispanic / White 0.87 (p=.012)* N.S. 0.81 (p=.000)* *MA plans significantly reduced racial gaps in PH/marker in CA and FL Summary MA plans reduced PH rates relative to marker rates In all racial groups, minority MA enrollees had lower risks of PH admissions (versus marker admissions) relative to their FFS counterparts Minority MA enrollees had greater reductions in PH admissions relative to white MA enrollees CA and FL: Interaction effect in pooled model shows statistically significant difference between minorities and white MA enrollees in PH rates Conclusion MA plans had beneficial impacts in terms of improving quality primary care by reducing preventable hospitalizations in all three states The benefit also spilled over to different racial and ethnic subgroups In CA and FL, MA plans resulted in significant reductions in racial and ethnic differences in preventable hospitalization rates Implications MA plans added value to the quality of primary care to the elderly by racial groups Greater reduction of PH rates among minority subgroups indicates favorable role of MA plans in achieving racial/ethnic equalities Care management provided in Medicare HMOs may have implications for future strategies to reduce racial ethnic gaps and improve quality of primary care Future research should evaluate the MMC programs by plan types using more recent data APPENDIX RESULTS Odds Ratios of PH Admissions (relative to Marker): MA VS. FFS enrollees CA NY FL White AA Hispanic 0.82 0.70 0.71 0.93 N.S. 0.85 0.89 0.82 0.75 PH Admissions severe ENT infections chronic obstructive pulmonary disease diabetes convulsions hypoglycemia kidney infection asthma angina congestive heart failure bacterial pneumonia tuberculosis hypertension cellulitis gastroenteritis requiring hospitalization urinary tract infection dehydration pelvic inflammatory disease nutritional deficiencies certain dental conditions Marker Admissions: The Comparison Group Diagnoses for which provision of timely and effective outpatient care is likely to have little impact on the need for hospital admission Agreement among practitioners on clinical criteria for admission: appendicitis with appendectomy acute myocardial infarction gastrointestinal obstruction fracture of hip/femur