Hospital EMR Use and Performance
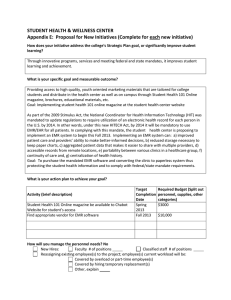
advertisement

Hospital EMR Use and Performance Abby Swanson Kazley Medical University of South Carolina Academy of Health Annual Research Meeting June 5, 2007 EMRs • Use • Expected Benefits • Barriers to Implementation The Promise of EMRs in the United States • Medicals errors often lead to the escalation of health care costs while decreasing the quality of care (Zwillich 2005) • Questions of duplication and appropriateness of health care services • Geographic variation in care may decrease with standardized clinical protocol (Hannan 1999) • Natural Disasters such as Hurricane Katrina Theoretical Framework • Donabedian’s Structure, Process, Outcome Model Structure (EMR adoption and years of use) Overall Process (Efficiency as measured through DEA score) Outcome (Quality) Hospital EMR Use • HIMSS Definition – “Comprehensive database system used to store and access patients’ health care information electronically. The computerbased patient record replaces the paper medical record as the primary source of information for health care meeting all clinical, legal, and administrative requirements…” • Automated, Contracted, or Not Automated Methods • Unit of analysis: Individual acute care hospital • Population: all general medical and surgical acute care non-federal hospitals in the United States • Includes 4,606 hospitals. • Of these, 479 hospitals used EMRs in 2004 • There is some limitation with regard to quality comparisons based on the number of stable measures in the data. For this analysis, n=2,891. • Observation takes place in 2004 for this retrospective cross sectional study • Bivariate Probit with Marginal Effects Hospital Performance • Efficiency – Data Envelopment Analysis (DEA) – CRS input oriented model • Quality – Hospital Quality Alliance data (2004) – 10 process measures of 3 clinical conditions Quality Measures Condition Measures Acute Myocardial Infarction Use of aspirin within 24 hours of arrival at hospital Use of aspirin at discharge Use of beta-blockers within 24 hours of hospital admission Use of beta-blockers at hospital discharge Use of angiotensin-converting-enzyme inhibitor Congestive Heart Failure Assessment of left ventricular function Use of angiotensin-converting-enzyme inhibitor Pneumonia Time of antibiotic therapy Availability of pneumoncoccal vaccine Assessment of Oxygenation Performance Classification Scheme Quality Low High Total Efficiency Low 989 1017 2,006 High 391 494 885 Total 1380 1511 2,891 Chi-square(1d.f.)=6.456 p<.05 Hospitals with EMRs Quality Low High Total Efficiency Low 85 (24.4%) 135 (38.8%) 220 (63.2%) High 50 (14.4%) 78 (22.4%) Total 135 (38.8%) 213 (61.2%) 348 (100.0%) 128 (36.8%) Model Biprobit (efficiency ) EMR Size Nonprofit Public SystemMembership teachingStatus PayerMix CaseMix error Biprobit (quality ) EMR Size Nonprofit Public SystemMembership teachingStatus PayerMix CaseMix error [95% Conf. Interval] Efficiency Coefficient Lower Upper EMR 0.095 -0.060 0.250 Bed Size 0.000 0.000 0.000 Teaching Status -0.014 -0.216 0.188 Payer Mix -1.466***' -2.931 -1.070 Non-profit -0.022 -0.173 0.128 Public -0.050 -0.239 0.139 1.100*** 0.841 1.136 0.078 -0.035 0.190 -1.007** -1.670 -0.347 EMR 0.178* 0.027 0.328 Bed Size 0.000 -0.001 0.000 Teaching Status 0.309** -0.618 -0.104 Payer Mix -0.643** -1.285 -0.269 Non-profit 0.413*** 0.271 0.555 Public 0.239** 0.062 0.415 Case Mix .644*** 0.390 0.898 System Member 0.077 -0.028 0.181 Constant -0.087 -0.735 0.562 Case Mix System Member Constant Quality Log Likelihood=-3580.786 *** p<.001, ** p<.01, * p<.05 Marginal Effects Quality Efficiency Low High Low (-) NS High NS (+) Implications and Conclusions • EMRs are associated with greater quality of care in hospitals • There is no clear relationship between EMR use and efficiency performance in hospitals • EMRs may influence the structure, process, and outcomes of care