Assessing the Role of the Physician and Practice Setting in
advertisement

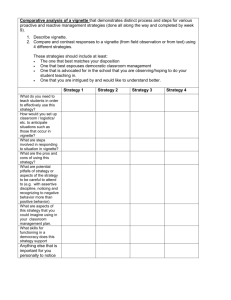
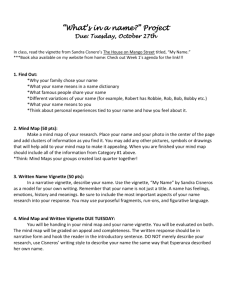
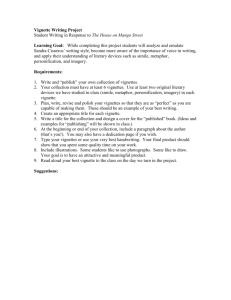
Assessing the Role of the Physician and Practice Setting in Child Health Disparities Lauren A. Smith1, Andrew Johnson2, Carol J. Simon2 1Boston University School of Medicine 2Abt Associates and Boston University School of Public Health Supported by grants from Agency for Healthcare Research and Quality, The California Endowment & The Commonwealth Fund Research Objectives To examine clinical decision making for 2 pediatric conditions with a high degree of clinical discretion To identify any racial/ethnic differences in clinical decision making To explore the association of physician and practice characteristics with decision making and any disparities Study Design & Population Studied Mixed-mode (mail, web) survey Random sample of 1,500 primary care physicians from AMA Physician Masterfile N=771 pediatric providers 5 states: CA, GA, IL, PA, TX Minority MDs over-sampled ~15% African American and/or Hispanic Fielded January-May 2007 65% response rate Practice questions plus clinical vignettes Survey Data Domains Practice & patient characteristics Location Payer types Racial/ethnic composition of patient population Limited English proficiency MD characteristics Race/ethnicity Gender Age Time since graduation Race/Ethnicity Variation in Vignettes Vignette Name Race/ethnicity 1a Elena Latina 1b Aisha African American 1c Kristen White 2a José Latino 2b Darnell African American 2c Todd White Vignette 1 NAME, a previously healthy 13 yo RACE/ETHNICITY girl, sees you for the evaluation of stomach pain, headaches and fatigue. Her mother says her daughter often complains about being sick. She had been an above-average student, but now gets poor grads. She often naps during the day and recently quit the school chorus because she was “too tired”. She has difficulty sleeping. She denied alcohol or drug use. Recent medical evaluation, including blood work was normal. The patient lives with brother and sister. PE: Height 50%ile; weight 75%ile, up 8 pounds since last year. She is quiet during the interview and says she “feels fine”. The remainder of PE is normal. Vignette 1 Results by Race Clinical management Total N=771 % White N=260 % Black N=251 % Latino N=260 % Dx=adolescent response very likely 23 25 22 22 Dx=depression very likely 39 42 36 39 Observe 17 14 16 19 Refer to mental health provider 70 71 68 70 No medical therapy 81 81 82 80 Start anti-depressant 18 18 16 19 Vignette 1 Results by Practice/Patient Characteristics Clinical management Latino Patients Black patients <20% 40% <20% N=296 N=211 N=466 % % % 40% N=73 % Dx=adolescent response very likely 23 27 23 23 Dx=depression very likely 37 40 42 32* Observe, reassess 16 18 16 19 Refer to mental health provider 73 67 72 60* No medical therapy 81 82 82 85 Start anti-depressant 18 15 18 15 Vignette 1 Results by Practice/Patient Characteristics Clinical management LEP Patients Medicaid patients <20% 40% <20% N=463 N=121 N=355 % % % 40% N=225 % Dx=adolescent response very likely 21 28* 21 29* Dx=depression very likely 40 43 40 36 Observe, reassess 14 24* 14 18 Refer to mental health provider 73 66* 74 64* No medical therapy 81 88** 84 81 Start anti-depressant 18 13 15 19 Vignette 2 NAME, a 9 yo RACE/ETHNICITY boy, arrives with his mother for a new patient visit. He was diagnosed with asthma 2 yrs ago. In the past year, he has had 2 ED visits, 1 hosp, and 1 short course of oral steroids. He has some wheeze & cough 2-3 times/week and awakes once or twice/month w/ cough. His mother states “it doesn’t seem to bother him.” He gets albuterol nebs for his coughing & wheezing episodes. One older sibling w/ history of wheezing. No drug, food or seasonal allergies. There is a cat at home. Mother smokes. PE: Wt for ht is above 75%ile. No audible wheezing. Vignette 2 Results by Race Clinical management Total White Black N=771 N=260 N=251 % % % Latino N=260 % Dx=mild persistent 33 35 30 32 Dx=mod persistent 59 56 61 59 Check peak flow 69 71 67 69 Asthma action plan 88 89 87 88 Refer to asthma specialist 21 20 22 21 Inhaled corticosteroids seasonally/short period 23 26 23 21 Inhaled corticosteroids year round 71 72 69 73 Vignette 2 Results by Practice/Patient Characteristics Clinical management Latino Patients Black patients <20% 40% <20% N=296 N=211 N=466 % % % 40% N=73 % Dx=mild persistent 32 30 32 41* Dx=mod persistent 60 56 59 58 Check peak flow 65 76* 73 56* Asthma action plan 84 91* 87 83 Refer to asthma specialist 24 19 23 13** Inhaled corticosteroids seasonally/short period 22 21 23 19 Inhaled corticosteroids year round 73 72 72 73 Vignette 2 Results by Practice/Patient Characteristics Clinical management LEP Patients Medicaid patients <20% 40% <20% N=463 N=121 N=355 % % % 40% N=225 % Dx=mild persistent 32 35 27 37* Dx=mod persistent 61 57 64 53* Check peak flow 65 79* 68 73 Asthma action plan 87 92 85 90** Refer to asthma specialist 22 20 25 17* Inhaled corticosteroids seasonally/short period 23 24 23 21 Inhaled corticosteroids year round 73 68 74 71 Conclusions Substantial variation reported in clinical management of childhood depression and asthma No variation noted based on race/ethnicity of patient in vignette Practice characteristics associated with differences in clinical decision making Physicians who had high proportion of black patients or Medicaid-insured patients were less likely to refer to specialists Limitations Vignettes may not reflect true decision making practices Triggers in vignettes may not have been sufficient to trigger differences in decision making Sample from 5 states may not be generalizable to all pediatricians