Recurrent Urinary Tract Infections: Risk Factors and Effectiveness of
advertisement
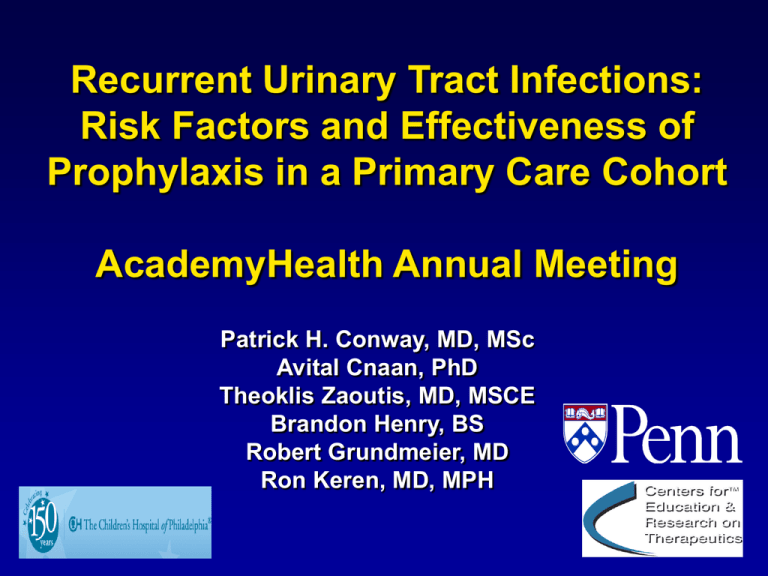
Recurrent Urinary Tract Infections: Risk Factors and Effectiveness of Prophylaxis in a Primary Care Cohort AcademyHealth Annual Meeting Patrick H. Conway, MD, MSc Avital Cnaan, PhD Theoklis Zaoutis, MD, MSCE Brandon Henry, BS Robert Grundmeier, MD Ron Keren, MD, MPH Epidemiology Urinary tract infection (UTI) is the most common serious bacterial infection in children Estimates of cumulative incidence in children 0 - 6 years suggest 70,000 to 180,000 of the annual U.S. birth cohort will have a UTI by age six Little data on recurrent UTI rate but previous estimates of 20 - 48% within 6-12 months Traditional Conceptual Model Figure 1 Conceptual Model Prophylactic antibiotics prevent recurrent UTI End Stage Renal Disease UTI(s) RENAL SCARRING Hypertension Surgery corrects VUR Pre-eclampsia VUR Controversy Cochrane report summarized that evidence “to support widespread use of antibiotics to prevent recurrent UTI is weak” Two small clinical trials found prophylaxis had no significant effect on risk of recurrent UTI or renal scarring Specific Aims 1. To determine the factors associated with risk of recurrent UTI in a primary-care based cohort and to estimate the risk reduction provided by prophylactic antibiotics 2. To determine the risk factors for antibiotic resistance among recurrent UTIs Methods: Data Source Data obtained from primary care based network of practices who contribute to CHOP’s Epic electronic health record 27 practices from urban, suburban, and semi-rural areas in 3 states Data contains laboratory, prescription, and radiology data from clinic and emergency room settings Cohort Inclusion Criteria Identified children 0 - 6 years of age with at least 2 office visits between 7/1/2001 and 5/31/2006 From these infants, identified cohort with first UTI based on positive urine culture (>50,000 CFU/ml single organism) Followed infants until last documented contact with the network or until they experienced the primary outcome, a recurrent UTI Aim 1 Design: Cohort Outcome variable: Time to recurrent UTI Covariates: Age at first UTI Gender Race Degree of reflux Antibiotic prophylaxis Antibiotic prophylaxis was considered as a time varying covariate Analysis: Cox survival time regression Aim 2 Design: Nested case-control Outcome variable: Resistant versus pansensitive recurrent infections Covariates: Age at first UTI Gender Race Antibiotic prophylaxis exposure (yes/no) Degree of reflux Analysis: Multivariable logistic regression Results 74,974 Children 0-6 years of age with at least 2 clinic visits 719 Children with any Urinary Tract Infection 628 Children with First UTI 611 Children with First UTI and not Excluded 83 Children with Recurrent UTI First UTI incidence rate: 0.007 per person-year Recurrent UTI incidence rate: 0.12 per personyear Observation time Mean observation time was 408 days with a median of 310 days (IQR 150 – 584 days), range of 24 - 1600 days First and Recurrent UTI First UTI (Number, %) Total Recurrent UTI (Number, %) 611 83 (13.6) Gender - Male - Female 68 (11.1) 543 (88.9) 8 (9.6) 75 (90.4) Race - Caucasian - Non-Caucasian 343 (56.1) 268 (43.9) 54 (65.1) 29 (34.9) 236 (38.6) 375 (61.4) 26 (31.3) 57 (68.7) VCUG - Not Performed - Normal - VUR Grade 1 - 3 - VUR Grade 4 - 5 400 (65.5) 154 (25.2) 50 (8.2) 7 (1.1) 52 (62.7) 20 (24.1) 8 (9.6) 3 (3.6) Exposure to antibiotic prophylaxis - No - Yes 483 (79.1) 128 (20.9) 64 (77.1) 19 (22.9) Age - Less than 2 years - 2 - 6 years Risk of Recurrent UTI1 Univariable Hazard Ratio (95% CI) Multivariable Hazard Ratio2 (95% CI) Gender (Ref. Male) - Female 1.20 (0.58 – 2.50) 1.08 (0.51 – 2.30) Race (Ref. Non-Caucasian) - Caucasian 1.99 (1.26 – 3.16)3 1.97 (1.22 – 3.16)3 Age (Ref. 0 - 1 year) -1 – 2 years -2 – 3 years -3 – 4 years -4 – 5 years -5 – 6 years 0.99 (0.43 – 2.27) 1.22 (0.51 – 2.95) 2.55 (1.33 – 4.81)3 2.17 (1.10 – 4.29)3 1.36 (0.66 – 2.80) 1.05 (1.20 – 3.37) 1.26 (0.51 – 3.07) 2.75 (1.37 – 5.51)3 2.47 (1.19 – 5.12)3 1.62 (0.73 – 3.62) VCUG (Ref. Normal) -Not Performed -VUR Grade 1-3 -VUR Grade 4-5 1.00 (0.60 – 1.68) 1.17 (0.52 – 2.66) 4.59 (1.36 – 15.47)4 0.70 (0.40 – 1.21) 1.05 (0.43 – 2.57) 4.38 (1.26 – 15.29)4 Antibiotic prophylaxis5 1.05 (0.57 – 1.94) 1.016 (0.50 – 2.02) 1 Time-to-event performed from date of first UTI until event, recurrent UTI, or last clinic visit within the primary care network Multivariable survival analysis controlling for gender, race, age, VCUG result, and prophylactic antibiotic exposure 3 p<0.01 4 p<0.05 5 Antibiotic prophylaxis exposure was modeled as time varying covariate in order to take into account total time exposed and intermittent nature of exposure 2 100 75 50 25 0 Percent without Recurrence Time To Recurrent UTI by Age 0 12 24 36 Observation Time (months) Age < 2 Years Age ≥ 2 – 6 Years Antibiotic Prophylaxis Propensity Score Analysis Developed a propensity score for likelihood of receipt of prophylactic antibiotics Analyses stratified by propensity score quintile demonstrated no significant effect of antibiotic prophylaxis Antibiotic prophylaxis still did not decrease risk of recurrent UTI when controlling for: • Propensity quintile (HR 1.03, 0.51 – 2.08 ) • Continuous propensity score (HR 1.02, 0.51 – 2.05 ) Risk of Antibiotic Resistance among Recurrent UTI Subjects Number of Resistant Infections (% of Recurrent UTI subjects) Odds Ratio of Recurrent UTI Being Antibiotic Resistant1 95% CI Gender - Male - Female 7 (87.5) 44 (58.7) Ref 0.20 0.02 – 1.73 Race - Non-Caucasian - Caucasian 24 (82.8) 27 (50.0) Ref 0.212 0.07 – 0.63 21 (80.8) 30 (52.6) Ref 0.263 0.09 – 0.80 VCUG - Normal - Not Performed - VUR Grade 1-3 - VUR Grade 4-5 14 (70.0) 27 (51.9) 7 (87.5) 3 (100.0) Ref 0.46 3.00 NA 0.15 – 1.39 0.30 – 30.02 NA Antibiotic prophylaxis - None - Exposed to prophylaxis 34 (53.1) 17 (89.5) Ref 7.502 1.60 – 35.17 Age - Less than 2 years - 2 – 6 years 1 Odds ratio of resistant versus pan-sensitive organism as cause of recurrent UTI p ≤ 0.01 3 p < 0.05 2 Probability of Recurrent UTI Being Antibiotic Resistant1 Prophylactic Antibiotic exposure 1 2 NonCaucasian Less than 2 Years of Age VUR Present Probability of Resistance (%)2 + + + + 98.0 + + + - 94.2 - + + + 92.4 + - + + 92.2 - + - + 89.6 + - - + 89.3 - + + - 79.9 + - + - 79.5 - - + + 74.5 - + - - 73.8 + - - - 73.3 - - + - 48.9 - - - - 40.4 For each exposure variable, a “+” represents that exposure being present Probability of causative organism being resistant to any antibiotic Summary Incidence rate for recurrent UTI of 12% per year is significantly lower than previous estimates Prophylactic antibiotics not associated with decreased risk of recurrent UTI but significantly associated with increased the risk of resistant infections Older 2-6 year old children, especially age 35, and Caucasian children had an increased risk of recurrent UTI VUR Grade 1-3 had no significant effect on recurrence risk Limitations – Antibiotic exposure Antibiotic exposure was based on prescription data Likely overestimates the exposure in both subjects with and without recurrent UTI Potential confounding by indication and residual unobservable confounding Limitations – Sparse or Missing Data Missing data due to VCUG not being performed Possibility of missing data from outside network • Attempted to minimize through chart review including correspondence from outside hospitals and clinics Strengths Based on primary care population Cohort design with large sample size that followed subjects for on average over 1 year in “natural experiment” Concurrently investigates potential risks and benefits of prophylactic antibiotics in same cohort Implications – Antibiotic Prophylaxis Given potential lack of prevention benefit and demonstrated harm due to resistant infections, this study in combination with other negative RCTs raises doubts about the effectiveness of prophylactic antibiotics Close monitoring without prophylaxis after first UTI may be a reasonable management strategy Implications - VUR and Antibiotic Prophylaxis Subjects with Grade 1-3 VUR had no significant increased risk of recurrence and Grade 4-5 VUR had increased recurrence risk Antibiotic prophylaxis did not effect the risk of recurrence in either group in stratified or multivariable analysis Unclear if VUR, especially lower grade VUR, should be sole factor considered in prophylaxis recommendations Implications – Other Risk Factors Non-Caucasians had decreased risk of recurrence but increased risk of resistant infections Older children (age 2-6 years) had increased risk of recurrence; this may represent dysfunctional elimination syndromes Next Steps and Considerations RCT of antibiotic prophylaxis versus close monitoring Should UTI be considered as 2 hits necessary prior to long-term treatment? • Child with first UTI and no major urinary tract anomalies watched closely off treatment Future studies should validate whether older age and Caucasian race are risk factors for recurrence and explore mechanisms (e.g. dysfunctional elimination, genetic markers) Acknowledgments University of Pennsylvania CERTS grant Dr. Ron Keren Dr. Avital Cnaan Mr. Brandon Henry and Chris Bell, research assistants University of Pennsylvania Clinical Scholars Program Practice-Based Research Network at CHOP, its physicians, staff, and patients Males by Circumcision Status First UTI (Number) Recurrent UTI (Number, %)1 Uncircumcised 26 5 (19.2) Circumcised 10 0 (0) Unknown 32 3 (9.4) Total 68 8 (11.8) 1 Differences were not statistically significant Effect of Antibiotic Prophylaxis Stratified by VUR Status1 Hazard Ratio for Antibiotic Prophylaxis2 (95% CI) VCUG - Normal - Not Performed - VUR Present 1 0.27 (0.04 – 2.02) 1.44 (0.57 – 3.64) 0.95 (0.29 – 3.13) Time-to-event performed from date of first UTI until event, recurrent UTI, or last clinic visit within the primary care network 2 Antibiotic prophylaxis exposure was modeled as time varying covariate in order to take into account total time exposed and intermittent nature of exposure Risk of Recurrent UTI in Females1 Multivariable Hazard Ratio2 (95% CI) 1 Race (Ref. Non-Caucasian) - Caucasian 2.12 (1.27 – 3.54)3 Age (Ref. Less than 2 years) - 2 - 6 years 1.94 (1.11 – 3.38)4 VCUG (Ref. Normal) - Not Performed - VUR Grades 1 - 3 - VUR Grades 4 - 5 0.69 (0.39 – 1.22) 1.03 (0.39 – 2.66) 2.51 (.33 – 19.3) Antibiotic prophylaxis5 1.04 (0.49 – 2.18) Time-to-event performed from date of first UTI until event, recurrent UTI, or last clinic visit within the primary care network 2 Multivariable survival analysis controlling for gender, race, age, VCUG result, and prophylactic antibiotic exposure 3 p<0.01 4 p<0.05 5 Antibiotic prophylaxis exposure was modeled as time varying covariate in order to take into account total time exposed and intermittent nature of exposure Risk of Recurrent UTI in Males1 Multivariable Hazard Ratio2 (95% CI) 1 Race (Ref. Non-Caucasian) - Caucasian 0.59 (.10 – 3.74) Age (Ref. Less than 2 years) - 2 - 6 years 2.30 (.48 – 11.1) VCUG (Ref. Normal) - Not Performed - VUR Grades 1 - 3 - VUR Grades 4 - 5 1.24 (0.19 – 8.21) 1.36 (0.48 – 11.1) 16.1 (1.91 – 136) Antibiotic prophylaxis5 1.73 (0.18 – 16.52) Time-to-event performed from date of first UTI until event, recurrent UTI, or last clinic visit within the primary care network 2 Multivariable survival analysis controlling for gender, race, age, VCUG result, and prophylactic antibiotic exposure 3 p<0.01 4 p<0.05 5 Antibiotic prophylaxis exposure was modeled as time varying covariate in order to take into account total time exposed and intermittent nature of exposure Risk of Recurrent UTI by 1 Year Age Groups1 Multivariable Hazard Ratio2 (95% CI) Gender (Ref. Male) - Female Race (Ref. Non-Caucasian) - Caucasian 1.97 (1.22 – 3.16)3 Age (Ref. 0 – 1 year) - 1 – 2 years - 2 – 3 years - 3 – 4 years - 4 – 5 years - 5 – 6 years 1.05 (.45 – 2.47) 1.26 (.51 – 3.07) 2.75 (1.37 – 5.51)3 2.46 (1.19 – 5.11)4 1.62 (.73 – 3.62) VCUG (Ref. Normal) - Not Performed - VUR Grades 1 - 3 - VUR Grades 4 - 5 0.68 (0.39 – 1.21) 1.14 (0.47 – 2.82) 4.38 (1.25 – 15.29)4 Antibiotic prophylaxis5 1 1.08 (0.51 – 1.96) 0.97 (0.48 – 1.96) Time-to-event performed from date of first UTI until event, recurrent UTI, or last clinic visit within the primary care network Multivariable survival analysis controlling for gender, race, age, VCUG result, and prophylactic antibiotic exposure 3 p<0.01 4 p<0.05 2 Other Recurrent UTI Studies Winberg studies published in ‘73 and ‘74 based on children 0-16 years who presented to Children’s Hospital in Goteborg from 1960-66 Proposed it was population based as “few other clinics” in the area After first UTI, children had urine tested at 13, 30, 60, and 90 days after first UTI and then at 1, 3, and 5 years after first UTI (not necessarily based on symptoms) Recurrence rate of 29% overall Decreasing “recurrence” rate with boys over time but no comment on circumcision status of males Other Recurrent UTI Studies (cont) Panaretto et al (J Paed Child Health 99) • 290 children 0-5 years diagnosed with UTI in ED, then had follow-up with 261 that consisted of phone call to parents at 6 and 12 months after UTI • If parents reported UTI recurrence, then investigators attempted to confirm via culture • Found 13% recurrence rate Other Recurrent UTI Studies (cont) Garin et al 2006 demonstrated no significant different recurrence risk in prophylaxis group versus no prophylaxis group (17 vs 23% overall) 9% pyelonephritis in prophylaxis group versus 3% in no prophylaxis group Among children on prophylaxis, recurrence rate of 8.8% for subjects without VUR versus 23.6% for those with VUR Cochrane Review • Trials by Savage, Smellie, Stansfield in 70’s of prophylaxis versus placebo • Often included children with multiple previous UTIs, no blinding, and testing of urine without symptoms • Recurrence rate as high as 69% in control arm (savage)