Study Objective Trends across institutional settings in cost and service intensity for
advertisement

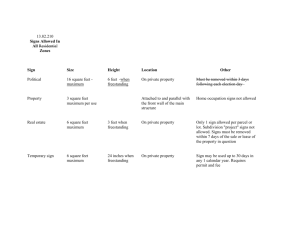
Trends across institutional settings in cost and service intensity for Medicare SNF care 1997 – 2003 Study Objective Kathleen Dalton, PhD , RTI International CoCo-authors Jeongyoung Park, doctoral candidate, University of North Carolina School of of Public Health To examine changes in average costs and intensity of services, before and after Medicare SNF Prospective Payment (PPS), across each of three institutional settings Part of larger funded study of rural hospital participation in SNF care Part of author’ author’s ongoing investigations of institutional responses to Medicare payment Rebecca T. Slifkin, Slifkin, PhD, University of North Carolina, Cecil G. Sheps Center for Health Health Services Research Funded through the federal Office or Rural Health Policy, under cooperative agreement with the N.C. Rural Health Research and Policy Analysis Center. Working Paper available at: www.shepscenter.unc.edu/research_programs/rural_program June 26, 2006 2 SNF services not necessarily similar across settings Background Academy Health Annual Research Meeting Medicare payments for inpatient skilled nursing payable to: Freestanding facilities HospitalHospital-based units (distinct, certified) “SwingSwing-beds” beds” – routine acuteacute-care beds in qualifying rural hospitals Freestanding (about 13,000) (about 1,500) 2002 Admissions (2.2 mill) 76% Covered Days (54.6 mill) Average Length of Stay 87% 28.3 days HospitalHospital-based 19% 11% 14.1 days SwingSwing-beds 6% 2% 8.9 days (about 1,000) Source: CMS Statistical Supplement, 2004. June 26, 2006 Academy Health Annual Research Meeting 3 Freestanding and HB units: began phasephase-in to SNF PPS rates payments in July 1998. SwingSwing-beds started SNFSNF-PPS in 2003. Swing beds in Critical Access Hospitals exempt from PPS Ancillary services continue as costcost-based Routine care had been under a fixed perper-diem but became costcost-based in 2002 (same rates as acute routine) June 26, 2006 Academy Health Annual Research Meeting Academy Health Annual Research Meeting 4 Presumption: HopedHoped-for responses to transition from costcost-based to prospective payment: Payment systems June 26, 2006 5 Reduce unneeded services (improved care efficiency) Reduce unit costs per service delivered (improved production efficiency) Eliminate inefficient providers (mergers, acquisitions or closures) Retain / attract new efficient providers June 26, 2006 Academy Health Annual Research Meeting 6 1 PostPost-PPS changes in number of certified skilled nursing facilities Percent change 1997 to 2004 -43% HospitalHospital-based: urban rural Freestanding: Study Design urban rural Descriptive Population: Outcomes: -20% +4% all SNFs filing Medicare cost reports 19961996-2003 Medicare costs, payments and margins Per diem costs: Therapy +11% All NonNon-therapy +6% Academy Health Annual Research Meeting June 26, 2006 ancillary services nursing Routine 7 Academy Health Annual Research Meeting June 26, 2006 Costs and Payments under SNFSNF-PPS: Costs and Payments under SNFSNF-PPS: FREESTANDING FACILITIES HOSPITAL-BASED UNITS Non-profit For-p rofit 2002 2004 500 0 19 98 2000 2002 2004 P ublic 0 0 250 500 dollars per day 250 250 0 2000 250 1998 2004 2002 2004 9 PPS responses: Change in median ancillary costs per day SNFPPS p ayme nt per day Academy Health Annual Research Meeting June 26, 2006 10 unadjusted cost per day 50 100 150 Median Part A rehab therapy costs per day 20 03 20 01 20 02 20 03 20 01 20 02 19 99 20 00 19 98 0 19 97 20 00 hospital-based 1.00 Hospital-Based 19 99 swing 1.50 Freestanding 19 98 2.00 unadjusted cost per day 50 100 150 Academy Health Annual Research Meeting June 26, 2006 20 00 SNFPPS cost per day SNFPPS payment per day 0 2002 19 97 20 00 SNFPPS cost per day unadjusted cost per day 50 100 150 freestanding 0.00 2001 2002 2003 Pt A only June 26, 2006 Academy Health Annual Research Meeting 11 June 26, 2006 20 03 2000 19 97 Pt A&B 20 01 20 02 1999 19 99 1998 0 1997 Swing-bed 20 00 0.50 19 98 dollars per day 19 98 P ublic 1998 index Non-profit 500 500 For-p rofit 8 Academy Health Annual Research Meeting 12 2 unadjusted cost per day 200 400 20 03 20 01 20 02 20 00 19 99 19 98 0 7 3 2 20 0 20 01 20 0 8 9 20 00 19 9 03 20 1 02 20 00 20 0 20 7 99 19 19 Absorbing demand Immediate market exit (mostly urban), but No apparent cost control among remaining providers SNFSNF-PPS losses = business as usual Watch 15 June 26, 2006 Surprisingly unrelated to type of ownership for trends in PPS vs. CAH swing Academy Health Annual Research Meeting 16 Measurement limitations? “accounting costs” costs” ≠ “true costs” costs” In freestanding settings Immediate reduction in rehab services in forfor-profit and nonnon-profit institutions In hospitalhospital-based settings Routine cost perper-diems are systematically understated due to averaging of skilled with unskilled patients in “dual” dual” units. But… But… Closure was associated with forfor-profit status and higher cost, higher Medicare utilization But continued operations with severe SNFSNF-PPS losses still common in profit and nonnon-profit; also in metro and micropolitan areas Academy Health Annual Research Meeting from closed HB units? Maybe Needs a detailed study from SNF claims and MDS data Costs could decline in future years with PPS implementation June 26, 2006 98 0 19 9 SwingSwing-beds Academy Health Annual Research Meeting 14 Still the setting with shortest stays, but no longer least intensive Increase in services could reflect change in patients HospitalHospital-based: June 26, 2006 Academy Health Annual Research Meeting Immediate reduction in overover-used services Control of unit costs elsewhere (reduction in real dollars) Healthy PPS surplus Text text text June 26, 2006 Freestandings: Swing-bed (carve-out rates only) 03 13 Hospital-based 20 1 02 20 20 0 99 98 00 20 19 19 19 9 7 0 Academy Health Annual Research Meeting What is going on? 19 9 19 97 unadjusted cost per day 200 400 20 03 20 01 20 02 20 00 19 99 19 98 0 19 97 20 03 20 01 20 02 20 00 19 99 19 98 Swing-bed June 26, 2006 Freestanding 0 Hospital-Based 19 9 unadjusted cost per day 50 100 150 unadjusted cost per day 50 100 150 unadjusted cost per day 50 100 150 19 97 0 Freestanding unadjusted cost per day 200 400 Median Part A routine costs per day Median Part A non-therapy ancillary costs per day HospitalHospital-based per diems include more fixed overhead costs. But… But… 17 Overstates profit in freestanding – HB units have fewer unskilled days Explains only part of the difference HB units truly have more and better paid nurses June 26, 2006 Academy Health Annual Research Meeting 18 3 Question: what is the business objective of a hospitalhospital-based SNF? Meeting clinical demand for services at more complex end of SNF care spectrum If so, unclear why SNFPPS casecase-mix adjustment doesn’ doesn’t adjust for this Accepted wisdom, but not borne out by lengthlength-ofof-stay differences Put unused beds & space to “productive” productive” use? (Well, not too productive given these losses… losses…) June 26, 2006 Academy Health Annual Research Meeting Some of it explainable by accounting artifact? Discharge management for DRG patients? Interpreting apparently nonrational responses 19 In aggregate, do we know if marginal income from SNF services is greater than marginal costs? Turning to organization theory to generate alternative explanations/ models of strategic response June 26, 2006 Academy Health Annual Research Meeting 20 4