Putting providers at-risk: How strong are incentives for upcoding and undertreating?
advertisement
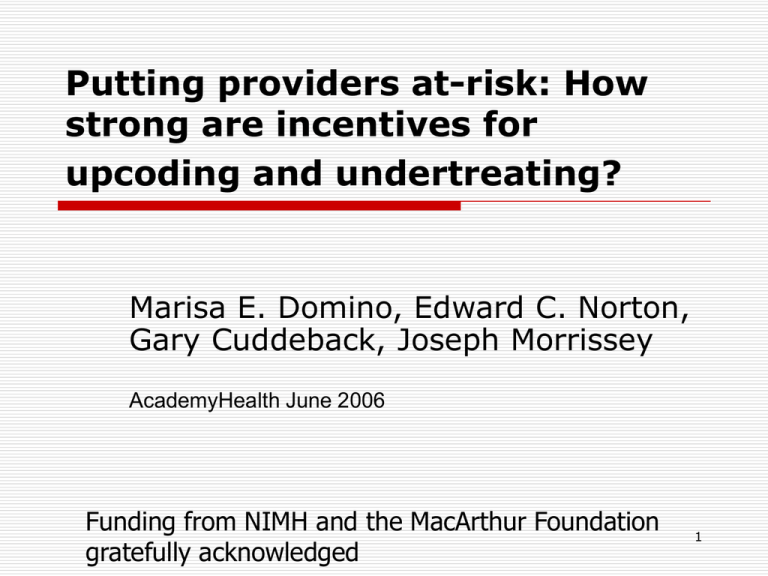
Putting providers at-risk: How strong are incentives for upcoding and undertreating? Marisa E. Domino, Edward C. Norton, Gary Cuddeback, Joseph Morrissey AcademyHealth June 2006 Funding from NIMH and the MacArthur Foundation gratefully acknowledged 1 Background & Policy Context Capitation payments to providers are common in health care Distinction between pure capitation, applied to a population of users and non-users and case-rate payments, applied to users only 2 Background & Policy Context Case-rate systems, while sharing risk between agencies/sponsors and health care providers, change the incentives for treatment over pure capitation or fee-forservice Rosenthal (HA 1999; JHE 1999) examined case-rate payments which did not vary with patient characteristics such as diagnosis or severity. Little is known about the effect of changes in case-rate payments on provider behavior 3 Research Questions Do changes in case-rate, or tier payments over time affect the tier assignment for new cases? Do changes in tier payments over time affect the number of services provided within each tier? 4 The King County Innovation On April 1, 1995: The State put the county at risk for all outpatient mental health services The County hired UBH on an ASO contract The County passed the risk on to local providers through the use of capitated case-rate contracts 5 Data Source King County Outpatient Mental health system County outpatient records for individuals assigned to a tier at some point during the study period First tier assignment for each individual used for the present analysis (n=8976) Focus on period from April 1995 to August 1996 Tier categories were collapsed in September 1996 6 Changes in Tiered payments April 1995 - August 1996 45 40 Dollars per Day 35 30 1A 1B 2A 2B 3A 3B 25 20 15 10 5 0 Apr-99 May-99 Jun-99 Jul-99 Aug-99 Sep-99 Oct-99 Nov-99 Dec-99 Jan-00 Feb-00 Mar-00 Apr-00 May-00 Jun-00 Jul-00 7 Methods Tier assignment model: ordered logit on the severity assignment (1-6) of those newly assigned to the case-rate system (n=8796) Second analyses conducted on those with severe mental illness (n=6605) Intensity of service use model: OLS on number of days per month with services use within each tier, robust clustered standard errors Key explanatory variable for both models is the daily tier payment 8 Results Increases in case-rate payment are associated with: increases the probability of classifying individuals at higher severity levels increases the number of services used in four of the six severity categories. A ten dollar increase in the daily case-rate is associated with between 1.2 and 4.6 more mental health visits per patient per month Because those with severe mental illness comprise the majority of individuals in the tiered system, results were almost identical for the severely mentally ill 9 Limitations First year of tier use Can’t rule out competing explanations Appropriateness of the level of service use within tiers not assessed Daily tier payments may not be as advertised because of recoupments and special payment categories Some oversight/audits on service use was conducted 10 Conclusions Provider payment mechanisms have the potential to substantially influence treatments received Assessment of severity by at-risk providers has the same incentive problems noted decades earlier in the Medicare DRG literature 11