Strategies to reduce inequalities in child health: Perspectives from Aotearoa/NZ
advertisement

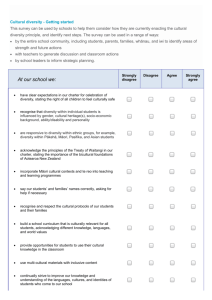
Strategies to reduce inequalities in child health: Perspectives from Aotearoa/NZ Annual Health Services Research Meeting Seattle, 25th June 2006 Dr Sue Crengle Overview • Briefly describe two examples of ethnic health disparities and strategies to address these • Identify general principles necessary for achieving desired outcome • SIDS prevention • Meningococcal vaccination SIDS mortality rates per 1000 live births by ethnicity 1980- 1986 (Source NZHIS 2005) Rate per 1000 live births 12 10 8 Mäori Other Total 6 4 2 0 1986 1984 1982 1980 SIDS case control study • 1987-1990 nation-wide case-control study • Number of ‘unmodifiable’ factors • Four ‘modifiable’ risk factors for SIDS – – – – Prone sleeping position Maternal smoking Not breast feeding Infant bed sharing Mitchell EA, Scragg R et al NZ Med J 1991;104:71-6 Mitchell EA, Taylor BJ et al J Paediatr Child Health 1992; 29(Suppl 1):S3-8 Scragg R, Mitchell E et al BMJ 1993; 307: 1312-1218 SIDS reduction campaign • Campaign to reduce these risk factors came out 1991/2 • Campaign to reduce these risk factors failed Mäori SIDS mortality rates per 1000 live births by ethnicity 1980- 1994 (Source NZHIS 2005) Rate per 1000 live births 12 10 8 Mäori 6 Other Total 4 2 0 1994 1992 1990 1988 1986 1984 1982 1980 Key messages didn’t reach Mäori • Inappropriate and ineffective messages for Mäori community • Inappropriate dissemination methods • No provision of culturally acceptable alternatives esp. with bed sharing SIDS prevention • 1994… – Mäori SIDS prevention team funded – Spent time listening and talking to community • 1996 – developed Mäori appropriate education / prevention • Sites • Messages • Staff SIDS prevention • 1996 – developed Mäori appropriate education / prevention • Sites • Messages • Staff Mäori SIDS prevention • 1996 – developed Mäori appropriate – Family assistance • Workers who go to SIDS death - work with family in short and sometimes longer term. – Work with coroners and others in sector to ensure safe and appropriate interactions between agencies and families SIDS mortality rates per 1000 live births by ethnicity 1980-99 (Source NZHIS 2003) 12 10 8 6 4 2 0 1998 prov 1997 Total 1996 1994 1993 Euro/Other 1992 1991 1990 1989 1988 1987 1986 1985 1984 1983 1982 1981 1980 Maori NZ meningococcal vaccine programme • My role of previous permanent advisor Māori • Sub-serotype specific Men B epidemic since 1991 • Three strands to delivery – Under 5 years – GP based delivery – 5 – 18 (at school) – school based delivery – Young people not at school – GP based delivery • MoH role • DHBs role NZ meningococcal vaccine programme • ‘General’ population programme – Some Māori ‘add ons’ • ‘communication’ strategy – Media, stakeholders, providers • Use of Māori providers already delivering immunisation outreach (no increase in these services) • General population programmes usually increase inequalities e.g. SIDS prevention NZ meningococcal vaccine programme • Māori advice largely unheeded until serious inequalities in coverage apparent (c. early 2005) – Further Māori media strategy – Increase outreach services • Accompanying discourses – ‘There are problems with the data’ – ‘Māori families are ‘low and slow’ to vaccinate their children’ • School based programme in CMDHB – Māori highest consent rate but lowest coverage National coverage dose 1 and 3 at 23 april 2006 by age and ethnicity 120 100 80 Mäori % 60 Pacific 40 Other 20 0 6w-4y 5-17y 18-19y 6w-4y 5-17y 18-19y dose 1 dose 1 dose 1 dose 3 dose 3 dose 3 Age and dose Doing it right… • Te Whānau ā Apanui health service • 1 doctor, 2 nurses, 1 receptionist • ~ 2000 registered patients – ~160 under 5 y olds • 92% Māori • HIGHLY deprived / low SE area • Rural – ~ 2 ½ hours by road to nearest hospital • LARGE catchment area • 100% coverage of < 5 year olds – Dose 1 and 2 over approx three weeks – Dose 3 over four to five weeks How? • Communication – Formal at sites in community several months before programme – With patients via newsletter – Informal communication with whānau in community • Appropriate service – Careful planning of approach – Sites of delivery • At all clinics • At kohanga reo • At home (planned and “drive-by’s”) kohanga reo - Māori language child care centres Hapū - How?? • Practice systems to foster efficient implementation • Staff • Positive reinforcement for children • They also ‘took over’ the school programme and had similar results Re-learning what we know… • ‘General’ programmes do NOT reduce disparities • Programme designed for those experiencing disparities works for all – Multiple points • Consultation, communication, service delivery etc • ‘80% of $ for last 20%’ – Maybe not if programme design approp