Innovations and Challenges in Coordinated Care for Chronically ill Children
advertisement

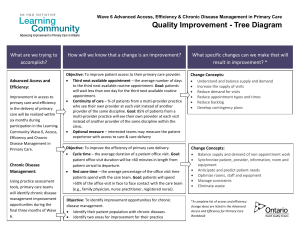
Innovations and Challenges in Coordinated Care for Chronically ill Children John M. Neff, M.D. Professor of Pediatrics University of Washington School of Medicine Center for Children with Special Needs Children’s Hospital and Regional Medical Center Seattle, Washington Acknowledgements • National Association of Children’s Hospitals and Related Institutions, NACHRI • Maternal Child Health Bureau HRSA Grant • Co-investigators: Virginia Sharp, Ctr for Children with Spec. Needs Jean Popalisky, Ctr for Children with Spec. Needs Tracy Fitzgibbon, Regence Blue Shield John Muldoon, NACHRI Acknowledgements Information on spectrum of children with chronic conditions and care coordination activities is based on recently completed work of the Center for Children with Special Needs with Regence Blue Shield of Washington (MCHB grant). • 31,000 children were tracked over four consecutive calendar years 2002-2005. • Children with chronic conditions were identified using CRGs, a soft ware developed by 3m. • Care coordination practices were analyzed. Outline of Topics Covered • Similarities between chronically ill adults and children. • Differences that are unique to the childhood population. • The Medical Home Concept. • Success and Challenges in the pediatric model. • Issues that need to be addressed. Similarities between chronically ill adults and chronically ill children • Chronic conditions account for a large proportion of costs. • Optimal care coordination requires collaboration among many disciplines. • Success of care coordination activities are impacted by co-morbid mental health conditions. • Many care coordination functions are not reimbursed. Differences unique to the childhood population 1. Spectrum of chronic conditions. 2. Pediatric specialists. 3. Insurance coverage 4. Families role. 5. Transition to adult care. 1. Spectrum of chronic conditions • Approximately 10% - 16% of children have chronic conditions that require added services and account for >50% of costs • Asthma occurs in 4-6% and ADHD in 2-4% of all children. • Emotional and behavioral conditions occur in 6-12% of all children; in about 30% of children with chronic conditions and 13% of other family members. • Other individual chronic conditions occur <1% of the childhood population. Spectrum of chronic conditions (cont) • Most chronic conditions in children have variable manifestations that change year by year and may not progress to chronic conditions in adults. • Asthma and ADHD, the conditions that account for 30% of children with chronic conditions, are highly variable, change and often improve with age. Spectrum of chronic conditions (cont) Based on our work with Regence Blue Shield of Wash. 31000 children were tracked over four consecutive years using administrative data and CRGs for identification: 7.5% children were identified to have a chronic condition in year one. 73.1% of these showed condition improvement. 5.7% showed progression to a more complex condition. Spectrum of chronic conditions (cont) • A small percentage of children, approximately 1% or less have chronic conditions that are known to be life long and in all probability progressive. These conditions account for over 10% of all health care costs for children. (Washington State Health Plan, Neff, Sharp and Popalisky) Spectrum of chronic conditions The principal examples of life long progressive conditions: • cerebral palsy • type one diabetes • muscular dystrophy • spinal cord defects • cystic fibrosis • variety of unusual neurological, immunologic, metabolic and genetic conditions 2. Pediatric Specialists • Many chronic conditions is childhood occur infrequently. • Primary care pediatricians may have limited personal experience in many chronic conditions in childhood. • There are a limited number of pediatric specialists and most are located at academic centers. • Specialists are not trained in primary care. • Part of care coordination is education of primary care pediatrician. 3. Insurance Coverage • Children are entirely dependent on parent’s insurance coverage or on Medicaid. • Medicaid coverage depends on income status of parents. • Coverage and practices are dependent primarily on state initiatives. 4. Family Role • Family centered care is an essential component to pediatric care at all levels. Families are partners in care coordination. • Success of family centered care model dependents considerably on the cultural, emotional and financial status of the family. 5. Transition to Adult Care • Involves issues of self care, independence, changes in support and coverage, education and living environment. • Transition to self care follows developmental stages of children and is highly dependent on the cognitive and emotional state. • Essential issues: sexuality, drug and alcohol use. • Requires considerable coordination between adult and pediatric providers. Medial Home Concept • Defined in 1992 and standardized in 2002 by the American Academy of Pediatrics • Medical Home provides care that is accessible, continuous, comprehensive, family centered, coordinated, compassionate and culturally effective. • A major national agenda of US MCHB: “All children with special needs have a medical home by 2010”. Medical Home Components 1. Plan of care. 2. Central record. 3. Shares information among the child, family, and consultants. Medical Care Components 4. Families linked to family support groups. 5. Assists the child and family in understanding clinical issues. Medical Care Components 6. Evaluates and interprets consultants' recommendations for the child. 7. Plan of care is coordinated with educational and other community organizations. Medical Home Components carried out by plan and practices Health Plan care coordination components 123 children with chronic problems selected for care coordination activities by plan. (n-165 encounters) Two practices that follow Medical Home model components 167 children with chronic problems selected by the practices. (n-1083 encounters). (Washington State Health Plan Neff, Sharp and Popalisky) Medical Home Components carried out by plan • • • • • • Education: health care system& serv. Needs and assessment. Community services, ref. and cord. Assistance with health plan issues. Financial planning and assist. Transition assistance. 32% 30% 22% 13% 2% 1% (Washington State Health Plan Neff, Sharp and Popalisky) Medical Home Components carried out by practice • • • • Family support. Disease management. Medication & equipment Referrals for specialty care 49% 28% 13% 10% (Washington State Health Plan Neff, Sharp and Popalisky) Findings • Plan and practice activities are appropriate and generally not duplicated. • Poor documentation of care coordination process by the practices. • Plan activities are financially supported by the plan. • Practice activities are not financially supported by the plan. Strengths in the Pediatric Model • Concept is endorsed by and a major goal of the American Academy of Pediatrics and US Maternal Child Health Bureau. • Care coordination is possible because of infrequency of complicated chronic conditions and somewhat of a regional system of care for children. • Health plans are required do care coordination of children with special health care needs as a part of Medicaid contracts. Challenges in the Pediatric Model • To identify and agree on children who would benefit most from care coordination. • To improve documentation of care coordination activities. • To improve coordination of care management between primary and specialty care. Challenges in the Pediatric Model • Success is heavily dependent on emotional and financial strengths of family, yet current health care environment drains families’ resources. • Success is heavily dependent on coordinated treatments of co-morbid mental and physical conditions yet the mental health care system is separate from the medical care system. . Challenges in the Pediatric Model • Appropriate coordination of activities between the practice and the plan. • Appropriate reimbursement of care management activities between the practice and the plans. • Care coordination for children with chronic conditions is not a focus of health plans and is often lost within the adult system. Essential Issues that Need to be Addressed • Identify the children who will benefit most from care coordination. • Define who is responsible for specific aspects of care coordination. • Documentation of care coordination. Essential Issues that Need to be Addressed • Financial support for care coordination activities. • Support for families with children with chronic conditions. • Coordinate mental and physical health systems. Essential Issues that Need to be Addressed • Improve information technology to assist care coordination. • Medical and pediatric disciplines collaborate in improving transition of children to adulthood.