Crossing the Quality Chasm
advertisement
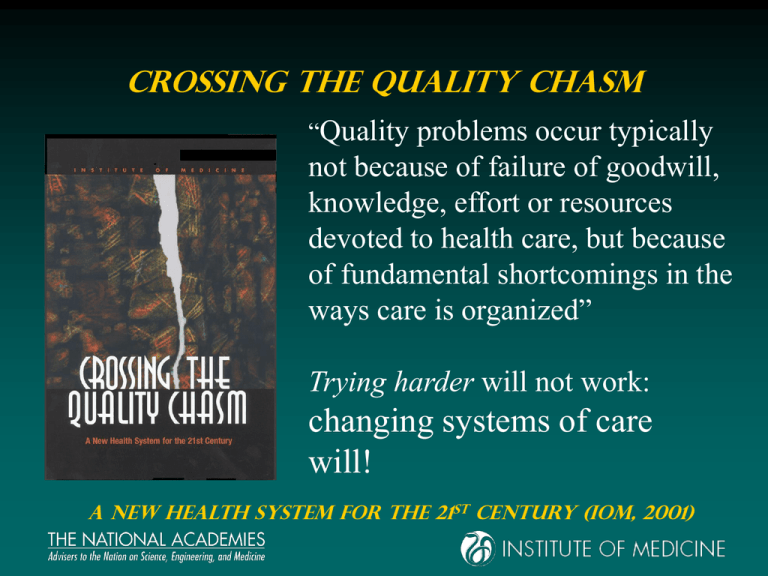
Crossing the Quality Chasm “Quality problems occur typically not because of failure of goodwill, knowledge, effort or resources devoted to health care, but because of fundamental shortcomings in the ways care is organized” Trying harder will not work: changing systems of care will! a new HEALTH system for the 21st century (IOM, 2001) The Crossing the Quality Chasm Series To Err is Human (1999) Crossing the Quality Chasm - A New Health System for the 21st Century (2001) Leadership by Example (2002) Fostering Rapid Advances in Health Care (2002) Priority Areas for National Action (2003) Health Professions Education (2003) Keeping Patients Safe – Transforming the Work Environment of Nurses (2004) Patient Safety – Achieving a New Standard for Care (2004) Quality through Collaboration – the Future of Rural Health (2005) Improving the Quality of Health Care for Mental and Substance-use Conditions (2005) Six Aims of Quality Health Care 1. Safe – avoids injuries from care 2. Effective – provides care based on scientific knowledge and avoids services not likely to help 3. Patient-centered – respects and responds to patient preferences, needs, and values Six Aims (cont.) 4. Timely – reduces waits and sometimes harmful delays for those receiving and giving care 5. Efficient – avoids waste, including waste of equipment, supplies, ideas and energy 6. Equitable – care does not vary in quality due to personal characteristics (gender, ethnicity, geographic location, or socioeconomic status) OVERARCHING CONCLUSION It is not possible to deliver safe or adequate healthcare without simultaneous consideration of general health, mental health and substance use issues. Overarching Recommendation 1 The aims, rules, and strategies for redesign in Crossing the Quality Chasm apply equally to M/SU health care. In particular, “Patient Centered Care” also applies to M/SU Care. Overarching Conclusion But…. Mental and Substance Use Care are different in important ways…… M/SU Health Care Compared to General Health Care • More stigma, coercion & discrimination • Less patient decision-making • Diagnosis more subjective • Less developed QI infrastructure M/SU Health Care Compared to General Health Care • More separate care delivery arrangements • Less use of IT • More diverse workforce & more solo practice • Differently structured marketplace Overview The Problem Patient Centered Care vs Effective Care Issue 1: Patient-Centered Care Hallmark of Ethical Care • Patient is the source of control on: – information sharing & decision making • Care based on patient needs and values • Care is transparent to the patient • Ethical care provides full disclosure/discussion of all care options – for patient to decide Issue 2: Effective Care • FDA standards of effectiveness • Do substance abuse treatments meet those standards? An FDA Perspective A Drug is Approved for “An Indication” 2 -Randomized Clinical Trials: Often ask for separate investigators Placebo Control: Movement to test vs approved medication Treatment Research Institute • Therapies – Cognitive Behavioral Therapy – Motivational Enhancement Therapy – Community Reinforcement and Family Training – Behavioral Couples Therapy – Multi Systemic Family Therapy – 12-Step Facilitation – Individual Drug Counseling • Medications – Alcohol (Disulfiram, Naltrexone, Accamprosate) – Opiates (Naltrexone, Methadone, Buprenorphine) – Cocaine (Disulfiram, Topiramate, Modafinil) – Marijuana (Rimanoban) – Methamphetamine – Nothing Yet So… Given effective options: • What if patients don’t want them? • How can we implement them? Improving the Quality of Health Care for Mental and Substance-Use Conditions Defining and Measuring Quality and Effectiveness Effectiveness, Performance, Quality: What’s the Difference? Effectiveness – Patient outcomes following treatment - patient symptoms and function Methods - Usually patient follow-up 6 – 12 months post discharge. Measures -Patient substance use, employment, crime – health, family & social function “Recovery”. Characteristics – Definitive, relevant, but slow, expensive, not management-relevant Performance – System function during treatment – “Indicators” of effectiveness. Methods - Examine admin databases for processes and interim results consistent with & indicative of effectiveness Measures – Usually identification, initiation, engagement, retention Characteristics - Fast, intuitive, face-valid, management-relevant, but not definitive Performance Indicator Examples Premise 1 – Patients who stay in treatment longer are likely to have better outcomes. Premise 2 - Care systems that perform better in engaging and retaining patients longer are likely to have better outcomes Then: Easily collected, analyzed and interpreted measures of the care system’s ability to engage and retain patients are one indicator of potential effectiveness. Performance Indicator Examples 1 – Initiation = % of patients who need care, that attend at least one session or day 2 – Engagement - % of patients who initiate, that stay for three days or visits 3 – Linkage - % of patients who complete early stage of care (ie. detox), that engage in the next stage of care (ie. OPT or Residential). Summary: Effectiveness Quality Performance Effective Care: Produces favorable patient outcomes. “Recovery” Quality Care: Uses evidence-based methods, delivered by credentialed staff, within licensed, accredited programs, and meets or exceeds the patient’s expectations. High Performance Systems: Identify those who need care; Initiate care for those who need it; Engage and retain those who initiate across modalities and between primary and specialty types of care. Other “Indicators” of Quality Licensing – indicates safety, legitimacy Accreditation – indicates contemporary standards of care Credentials –indicates proficiency in accepted practices Satisfaction –indicates appeal and value Evidence Based Practices – indicates use of state of the art care, professionalism Mechanisms for Coordinating Care • Inter-agency sharing agreements for patient information with patient consent. – Co-location of services – Shared patient records • Higher level policy coordination – Uniform record standards – Uniform information protection standards. A Differently Structured Marketplace • Government is major purchaser, • Carve-out purchases • Private insurance avoids covering or offers more-limited coverage Strategies • Purchasers offering enrollees a choice of health plans should use one or more tools for reducing adverse selection of individuals with M/SU conditions: – risk adjustment, – payer “carve-outs,” – risk-sharing or mixed-payment contracts, and – benefit standardization across the health plans • Congress and state legislatures should enact coverage parity. • Reorient State procurement to give greatest weight to quality. • Use M/SU health care quality measures in procurement and accountability processes. • State and local governments should reduce emphasis on grantbased systems of financing and increase use of funding mechanisms that link some funds to measures of quality.