Is JCAHO Accreditation Associated with Better Patient Outcomes in Rural Hospitals?
advertisement
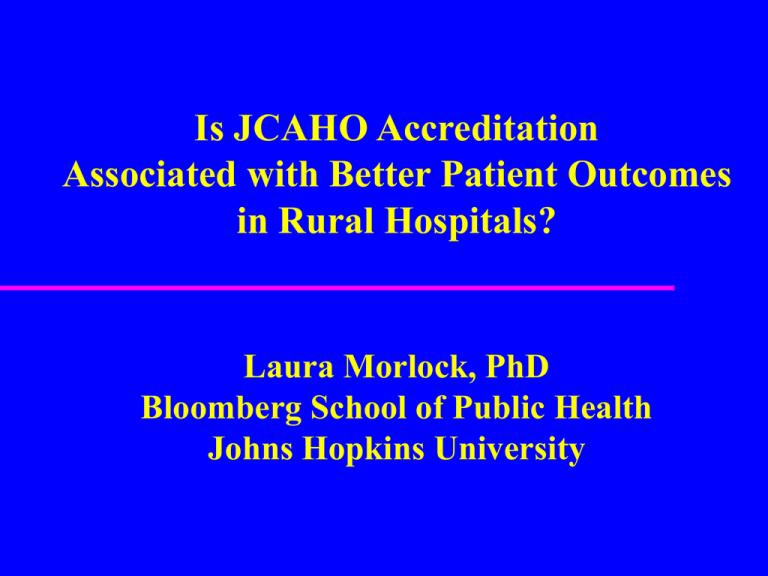
Is JCAHO Accreditation Associated with Better Patient Outcomes in Rural Hospitals? Laura Morlock, PhD Bloomberg School of Public Health Johns Hopkins University Project Sponsorship This analysis is part of a larger study: “Rural Hospitals: Environment, Strategy, and Viability” (RO1 HS011444) Funded by the Agency for Healthcare Research and Quality Research Team Johns Hopkins Bloomberg School of Public Health Laura Morlock, PhD David Salkever, PhD Peter Pronovost, MD, PhD Marlene Miller, MD, MSc Lilly Engineer, MD, MHA Cyrus Engineer, MHA,MHS Maureen Fahey, MLA Andrew Shore, PhD Rebecca Clark, BA Ann Skinner, MSW Research Team cont. Virginia Commonwealth University Stephen Mick, PhD and team Rural Policy Research Institute (RUPRI) Keith Mueller, PhD—Nebraska Medical Center Andrew Coburn, PhD—Univ. of Southern Maine Timothy McBride, PhD—St. Louis University A. Clinton MacKinney, MD, MS Mary Wakefield, PhD—Univ. of North Dakota Rebecca Slifkin, PhD—Univ. of North Carolina Overall Project Objective To assess the impact of Federal policy changes and healthcare market forces on the organizational and management strategies, financial viability and clinical performance of U.S. rural hospitals. Project Design Outcome Measures Federal Policy Legislation Healthcare Market Forces Rural Hospitals • Survival • Organizational & Management Strategies, including Conversion • Financial Viability • Clinical Performance Objective of This Analysis To examine whether rural hospitals accredited by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) have better patient outcomes than non-accredited rural hospitals. Background and Significance: Rural Hospitals Over 54 million people in the US live in rural areas and are served by about 2200 rural hospitals. Rural hospitals play a critical role in their communities by: – Providing access to health care; – Serving as a hub for public health, wellness, and social services; – Providing jobs, recruiting health practitioners, making communities more attractive places to live and work. Background and Significance: JCAHO Accreditation Fewer than 60% of rural hospitals seek JCAHO accreditation in contrast to 95% of urban hospitals. Cost is a major deterrent. It is not known whether JCAHO accreditation is associated with better quality as measured by patient outcomes. Study Design Study sample: All patients discharged from a random sample of about half of the rural hospitals (N=186) in 9 states. Time Frame: 1999-2001 Outcome variables: HCUP risk-adjusted inpatient mortality rates Independent (predictor) variable: Presence or absence of JCAHO accreditation Control variables: Hospital size, financial status, ownership, system membership, subsequent conversion to Critical Access Hospital States Included in the Analysis Arizona California Colorado Florida Iowa Kentucky New York Washington Wisconsin Outcome Measures Inpatient Quality Indicators (IQIs) Risk-adjusted in-hospital mortality rates during 1999-2001 for: – Congestive heart failure (CHF) – Stroke – Pneumonia Rationale for selection of specific indicators: Majority of both accredited and non-accredited rural hospitals met volume threshold of at least 30 patients with these conditions over the three year time period. Source of data: AHRQ-sponsored Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases for 9 states Independent (Predictor) Variable Hospital Accreditation Status Source of data: Information on the most recent accreditation status was provided by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) Control Variables* Hospital size: number of beds in operation Financial status: hospital total margins averaged over fiscal years 1999-2001 – Source of data: Medicare Cost Report files Multi-hospital system membership (yes/no) Ownership (public, private not-for-profit, private forprofit Subsequent conversion to Critical Access Hospital (CAH) (yes/no) * Source of data for all variables except financial status is the American Hospital Association. Methods of Analysis Multivariate regressions with bed size, average total margin, system membership, ownership and subsequent CAH conversion status used as control variables Generalized Estimating Equations (GEE) used to adjust for the clustering of hospitals within states Study Results 110 of 186 hospitals (59%) were accredited by the JCAHO JCAHO accreditation is positively associated with: – Larger number of beds (p<.0001) – Better financial condition (p<.05) – System membership (p<.001) – Private not-for-profit ownership (p<.001) JCAHO accreditation is negatively associated with: – Non-federal public ownership (p<.0001) – Subsequent conversion to CAH (p<.0001) Analysis Strategy Importance of using risk-adjusted rates that take into consideration severity of illness and risk of mortality based on the patient’s underlying condition (HCUP uses the All Patient Refined DRG software to do this) Importance of controlling for variables associated with seeking and obtaining JCAHO accreditation Differences by JCAHO Accreditation Status in Observed and Risk-Adjusted Mortality Rates Diagnoses Hospital Status Accredited Non-accredited Obs. R.A. Congestive heart failure 4.6% 5.2% Stroke 10.7% 12.9% Pneumonia 6.6% 8.1% Note: Obs.=Observed R.A.=Risk-Adjusted Obs. R.A. 4.8% 14.8% 6.0% 6.0% 16.6% 8.6% Multivariate Analysis Results After controlling for hospital size, financial status, ownership, system membership, and subsequent conversion to a CAH, JCAHO accreditation is significantly associated with lower risk-adjusted in-hospital mortality rates for: – Congestive heart failure (p<.02) – Stroke (p<.01) and – Pneumonia (p<.0001) A similar pattern is evident in within-state comparisons. Policy Implications These findings, if supported by further analyses, suggest that accreditation status may be a useful indicator of hospital clinical performance for rural health care consumers, payers and regulators. These findings may also be encouraging to the many rural hospitals with resource constraints that are considering the costs and benefits of embarking on the accreditation process.