Introduction Does Hospital Price Competition Influence Nurse Staffing and Quality of Care?
advertisement
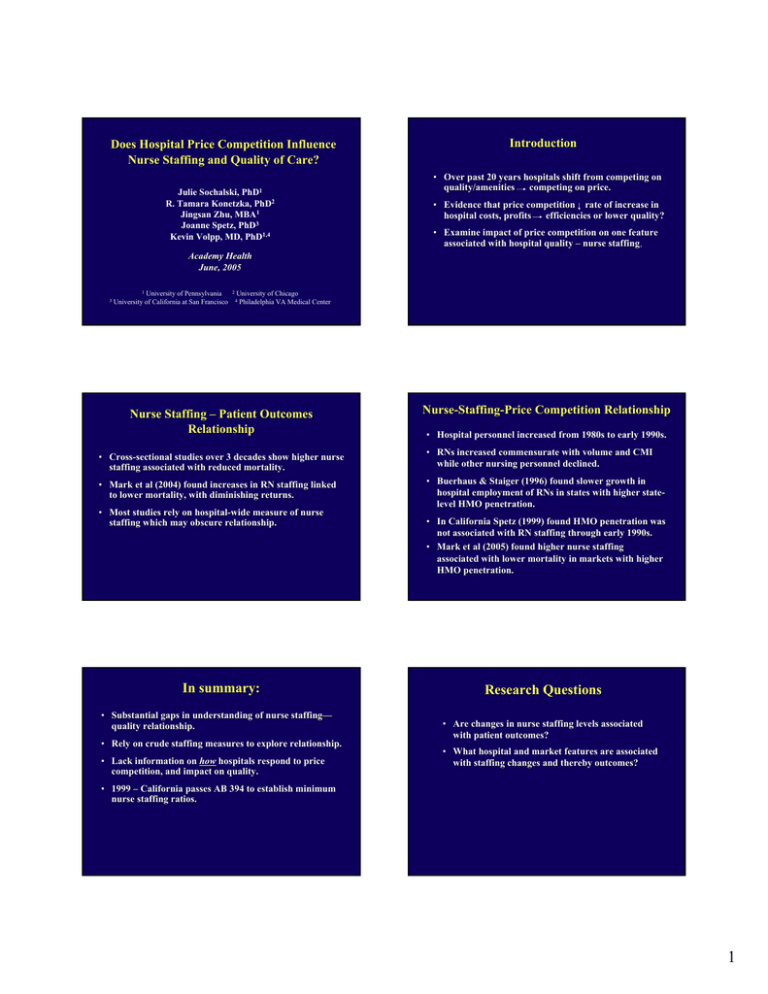
Does Hospital Price Competition Influence Nurse Staffing and Quality of Care? Julie Sochalski, PhD1 R. Tamara Konetzka, PhD2 Jingsan Zhu, MBA1 Joanne Spetz, PhD3 Kevin Volpp, MD, PhD1,4 Introduction • Over past 20 years hospitals shift from competing on quality/amenities competing on price. • Evidence that price competition rate of increase in hospital costs, profits efficiencies or lower quality? • Examine impact of price competition on one feature associated with hospital quality – nurse staffing. Academy Health June, 2005 3 1 University of Pennsylvania University of California at San Francisco 2 University of Chicago Philadelphia VA Medical Center 4 Nurse Staffing – Patient Outcomes Relationship NurseNurse-StaffingStaffing-Price Competition Relationship • Hospital personnel increased from 1980s to early 1990s. • CrossCross-sectional studies over 3 decades show higher nurse staffing associated with reduced mortality. • RNs increased commensurate with volume and CMI while other nursing personnel declined. • Mark et al (2004) found increases in RN staffing linked to lower mortality, with diminishing returns. • Buerhaus & Staiger (1996) found slower growth in hospital employment of RNs in states with higher statestatelevel HMO penetration. • Most studies rely on hospitalhospital-wide measure of nurse staffing which may obscure relationship. In summary: • Substantial gaps in understanding of nurse staffing— staffing— quality relationship. • Rely on crude staffing measures to explore relationship. • Lack information on how hospitals respond to price competition, and impact on quality. • In California Spetz (1999) found HMO penetration was not associated with RN staffing through early 1990s. • Mark et al (2005) found higher nurse staffing associated with lower mortality in markets with higher HMO penetration. Research Questions • Are changes in nurse staffing levels associated with patient outcomes? • What hospital and market features are associated with staffing changes and thereby outcomes? • 1999 – California passes AB 394 to establish minimum nurse staffing ratios. 1 Data Study Design • California acute care hospitals, 19911991-2001 – 1983 selective contracting legislation passed allowing price competition • California’s Office of Statewide Health Planning and Development (OSHPD) discharge data from 1991-2001. • OSHPD annual disclosure (financial) data 1991-2001 • State death certificates 1991-2001. – 1990s represents maturing managed care market – Administrative data has more refined measures of nurse staffing. Sample Key Study Variables • Nurse staffing – RN, LVN, Nurse Aide – Nursing productive hours per patient day – Acute medicalmedical-surgical units • Hospitals: n = 421 short-term acute hospitals (non-federal, non-Kaiser) • Patients: • AMI: • Market factors – Managed care penetration for hospital market area (fixed radius) – Interaction between managed care penetration and market competition n = 352,536 (15.5%) • Stroke: Stroke n = 592,651 (14.1%) • Hip fracture: n = 276,628 (5.3%) • Patient outcomes – AHRQ inpatient quality indicators: 3030-day mortality for AMI, stroke, hip fracture Control Variables Model #1: StaffingStaffing-Outcomes Relationship ∗ Age * Source of payment ∗ Gender * Elixhauser comorbidities ∗ Race * Hospital CMI ∗ Ethnicity * Year dummy variables Generalized linear model with hospitalhospital-level fixed effects + time fixed effects Model 1 Pr( Death) pht = β 0 h + β v Staffing ht + β wYeart + β1HospitalCMI ht + β x PatientSeverity pht + #2: StaffingStaffing-Price Competition relationship ∗ All above + wages β y PatientDemographics pht + β z PaymentSource pht + ε pht Model 2 RNhppd ht = β 0 h + β v Staffing ht + β wYeart + β1HospitalCMI ht + β 2 MCPht + β 3 MCP * COMPht + β 4WageIndexht + β x PatientSeverityht + β y PatientDemographicsht + β z PaymentSourceht + ε ht 2 Hospital Summary Statistics Change in CMCM-adjusted RN medicalmedical-surgical hours per patient day, 19911991-2001 20.0% No. of hospitals: Avg. # beds: Urban: Teaching: Ownership: Non-profit: Government: For-profit: Avg. CMI 421 192 88% 18.7% 15.0% 75th 10.0% 5.0% 0.0% 52.7% 20.7% 26.6% 1.114 1992 1993 1994 1995 1996 1997 1998 1999 2000 2001 -5.0% 25th -10.0% -15.0% Effects of nurse staffing on 3030-day mortality AMI Stroke Hip Fracture RN -0.004* (0.001) -0.002* (0.001) 0.002 (0.001) LVN -0.003 (0.002) 0.0004 (0.001) 0.0008 (0.001) Aide 0.001 (0.001) -0.0002 (0.0007) -0.0001 (0.0007) RN*baseline 0.0004† (0.0002) -0.0001 (0.0001) -0.0004 (0.0003) Model: * p < .05 † Effects of price competition on nurse staffing Managed care penetration 2.479** (0.696) Managed care penetration x Market competition -3.192* (1.245) ** p < .001 * p < .01 p < .1 Caveats/Limitations • Changes over time in DRGs, DRGs, coding, zip codes (but smoothed/corrected to the extent possible) • Limited to California – generalizable to other states? • Limited to mortality– mortality– generalizable to other quality measures? • Are there thresholds to staffingstaffing-quality relationship? Conclusions • Extent to which changes in RN staffing levels are associated with lower mortality varies by condition. • Increasing managed care penetration is associated with higher RN staffing except in most competitive markets. • Limiting the number of patients per nurse may improve quality outcomes. 3