Does Hospital Price Competition Influence Nurse Staffing and Quality of Care?
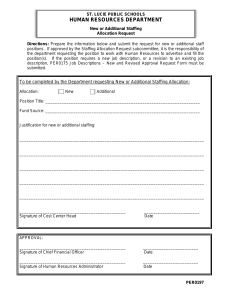
advertisement

Does Hospital Price Competition Influence Nurse Staffing and Quality of Care? Julie Sochalski, PhD1 R. Tamara Konetzka, PhD2 Jingsan Zhu, MBA1 Joanne Spetz, PhD3 Kevin Volpp, MD, PhD1,4 Academy Health June, 2005 1 University of Pennsylvania 3 University of California at San Francisco 2 University of Chicago 4 Philadelphia VA Medical Center Introduction • Over past 20 years hospitals shift from competing on quality/amenities competing on price. • Evidence that price competition rate of increase in hospital costs, profits efficiencies or lower quality? • Examine impact of price competition on one feature associated with hospital quality – nurse staffing. Nurse Staffing – Patient Outcomes Relationship • Cross-sectional studies over 3 decades show higher nurse staffing associated with reduced mortality. • Recent longitudinal study found increases in RN staffing linked to lower mortality, with diminishing returns. • Most studies rely on hospital-wide measure of nurse staffing which may obscure relationship. Hospital Responses to Price Competition • Hospital personnel increased from 1980s to early 1990s. • RNs increased commensurate with volume and CMI while other nursing personnel declined. • Spetz (1999) found HMO penetration was not associated with RN staffing through early 1990s. In summary: • Substantial gaps in understanding of nurse staffing— quality relationship. • Rely on crude staffing measures to explore relationship. • Lack information on current hospital responses to price competition. • 1999 – California passes AB 394 to establish minimum nurse staffing ratios. Research Questions • Are changes in nurse staffing levels associated with patient outcomes? • What hospital and market features are associated with staffing changes and thereby outcomes? Study Design • California acute care hospitals, 1991-2001 • Three AHRQ inpatient quality indicators: – 30-day mortality for AMI, stroke, and hip fracture Data • California’s Office of Statewide Health Planning and Development (OSHPD) discharge data from 1991. • OSHPD annual disclosure (financial) data 1991-2001 • State death certificates 1991-2001. • Sample: – Hospitals: n = 421 short-term acute hospitals (non-federal, non-Kaiser) – Patients: • AMI: n = 352,536 (15.5%) • Stroke: n = 592,651 (14.1%) • Hip fracture: n = 276,628 (5.3%) Key Study Variables • Nurse staffing – RN, LVN, Nurse Aide – Nursing productive hours per patient day – Acute medical-surgical units • Market factors – HMO penetration for hospital market area (fixed radius) – High vs. low competition market areas Control Variables • Age • Gender • Race • Ethnicity • Expected source of payment: Medicare, Medicaid, uninsured, private • Elixhauser comorbidities • Hospital case-mix index • Year dummies 1991-2001 (1991 is reference) • Hospital fixed effects controls for timeinvariant hospital and market factors Model Generalized linear model with hospital-level fixed effects + time fixed effects Model 1 Pr( Death) pht 0 h v Staffinght wYeart 1HospitalCMI ht x PatientSeverity pht y PatientDemographics pht z PaymentSource pht pht Model 2 RNhppd ht 0 h v Staffinght wYeart 1HospitalCM I ht 2 MCPht 3 MCP * COMPht 4WageIndexht x PatientSeverityht y PatientDemographics ht z PaymentSourceht ht Hospital Summary Statistics No. of hospitals: Avg. # beds: Urban: Teaching: Ownership: Non-profit: Government: For-profit: Avg. CMI 421 192 88% 18.7% 52.7% 20.7% 26.6% 1.114 Change in CM-adjusted RN medical-surgical hours per patient day, 1991-2001 20.0% 15.0% 75th 10.0% 5.0% 0.0% 1992 1993 1994 1995 1996 -5.0% 25th -10.0% -15.0% 1997 1998 1999 2000 2001 Effects of nurse staffing on 30-day mortality AMI Stroke Hip Fracture RN -0.004* (0.001) -0.002* (0.001) 0.002 (0.001) LVN -0.003 (0.002) 0.0004 (0.001) 0.0008 (0.001) Aide 0.001 (0.001) -0.0002 (0.0007) -0.0001 (0.0007) RN*baseline 0.0004† (0.0002) -0.0001 (0.0001) -0.0004 (0.0003) Model: * p < .05 † p < .1 Effects of price competition on nurse staffing HMO Penetration 2.479** (0.696) HMO Penetration*HHI -3.192* (1.245) ** p < .001 * p < .01 Caveats/Limitations • Changes over time in DRGs, coding, zip codes (but smoothed/corrected to the extent possible) • Limited to California – generalizable to other states? • Limited to mortality– generalizable to other quality measures? • Are there thresholds to staffing-quality relationship? Conclusions • Extent to which changes in RN staffing levels are associated with lower mortality varies by condition. • Increasing managed care penetration is associated with higher RN staffing except in most competitive markets. • Limiting the number of patients per nurse may improve quality outcomes.