Rural Public Health Preparedness: Setting the Agenda for Change
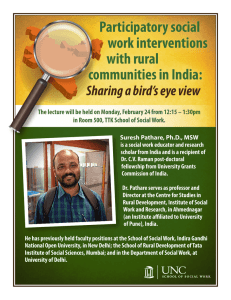
advertisement

Rural Public Health Preparedness: Setting the Agenda for Change Michael Meit, MA, MPH, Director, University of Pittsburgh Center for Rural Health Practice; Co-Director for Rural Preparedness, University of Pittsburgh Center for Public Health Preparedness Developing an Agenda for Change Topics & Facilitators: Building Capacity Barbara Quiram, PhD, Texas A&M School of Rural Public Health Research Michael Meit, MA, MPH, University of Pittsburgh Center for Rural Health Practice Advocacy Janet Place, MPH, University of North Carolina School of Rural Public Health Setting an Agenda for Change Building Capacity Issues: Limited human and financial resources to build necessary infrastructure Limited understanding of “rural public health” and how it is practiced Absence of leadership Setting an Agenda for Change Building Capacity Recommendations: Workforce and Leadership Development Integration of rural PH preparedness knowledge into all health professions training Educational development beginning in K-12 Workforce development that extends beyond health professionals Identify and engage stakeholders in the rural preparedness dialogue Identify model training/leadership development programs Educational Outreach Direct educational initiatives toward government agencies and personnel to enable them to make informed decisions Inform policy-makers on best practices that demonstrate importance and value of strategies utilizing rural resources Setting an Agenda for Change Research Initial work for the research topic was taken from the Rural PH Research Agenda, developed in 2004. Preparedness was one of 6 topics in this report, which formed the basis for the research discussion in St. Paul. Setting an Agenda for Change Research Issues: Lack of state and local PH response capacities in some rural areas Lack of uniformity in state and local PH systems for planning consistency Identification of the expanded rural PH system for PH response Identification of necessary competencies in rural PH response Perceived low threat of rural PH emergencies Need for model practices in rural PH response Lack of an organized rural PH constituency Setting an Agenda for Change Research Priority Research Questions 1. How is government organized (i.e., different state/regional/local models) across the U.S. to assure accountability for preparedness in rural areas and what are the implications for incident command, allocation of funding, cross-jurisdictional response, etc.? 2. What components/functions of preparedness are currently and should be provided by rural communities? How are rural communities mobilizing and organizing resources (including people to fulfill those roles and responsibilities? 3. Who comprises the response network and what competencies are necessary for readiness? What are the most effective training methods? Setting an Agenda for Change Research Priority Research Questions 4. Is the perception of the likelihood of bioterrorist and other public health emergency threats different in rural vs. non-rural (urban, suburban) areas? Between rural areas? Does the perception of threat affect the level of preparedness? 5. What lessons have been learned from previous public health response experiences/events that are applicable to our currents efforts to strengthen rural preparedness? How can those lessons influence/inform models of preparedness, readiness evaluation tools, training strategies, etc? Setting an Agenda for Change Research Recommendations: Development of Infrastructure to Support Research Need for dedicated funding to support “Rural Public Health” research activities, both from federal agencies and foundations Specific CDC focus on rural public health issues; specific focus among agencies such as FEMA, DHS, DOJ and others on rural PH preparedness Enhance “prestige” of rural research through development of dedicated rural public health journal and encouraging existing RH and PH journals to include more rural PH content, creation of a national rural PH conference, and enhanced funding opportunities for rural PH researchers. Setting an Agenda for Change Research Recommendations (Cont.): Research Strategies Demonstration projects, including across jurisdictions Highlighting case studies and best practices Developing adaptable templates for program implementation Focusing on community-participatory strategies Increasing linkages among researchers, and between researchers and community partners, including elected officials “Mining” current data sets and summarizing current information Conducting research that can be easily translated into policy Enhancing communications among researchers with an interest in rural PH – creating a network of rural PH reseachers Creating measurable objectives for rural PH research with easily identifiable goals Setting an Agenda for Change Research Recommendations (Cont.): Research Advocacy Need to advocate for rural PH research as a unique and necessary priority area within the field of public health Work with the Federal Office of Rural Health Policy to advocate within the federal government Work with national RH and PH organizations to create a strong legislative recognition of (and focus on) rural PH issues. Create a rural PH constituency/voice. Educate legislators, the rural caucus, agency heads, and PH researchers themselves on rural health issues Ensure a particular focus on CDC, which should be a much stronger voice for rural PH Setting an Agenda for Change Advocacy Issues: Lack of an organized rural PH constituency Rural citizens are a large, disparate group Lack of understanding of PH in general, much less how it can be applied in rural settings Setting an Agenda for Change Advocacy Recommendations: Need for broad focus on rural PH, with preparedness as a subset of that focus – e.g., highlight general surveillance and epidemiology challenges in rural areas, highlighting implications for preparedness Broadly define preparedness to include infectious disease, food safety, and natural disasters. Do not create an “us vs. them” mentality Focus on unique rural concerns such as water and food supply, access to healthcare, energy sources, etc. Highlight challenges related to the public health workforce, including recruitment and retention issues Enhance general understanding of public health among policy makers – if they don’t understand PH, there’s little opportunity to educate about rural PH Create a grass-roots rural public health movement – from there create and organized constituency at the local, state and federal levels Use business models to frame importance of investing in rural PH For more information contact: Michael Meit Director University of Pittsburgh Center for Rural Health Practice 300 Campus Drive Bradford, PA 16701 Phone: (814) 362-5050 Fax: (814) 362-5044 Email: meit@pitt.edu www.upb.pitt.edu/crhp