? Linking 25% of UK FP’s pay to in quality improvement
advertisement

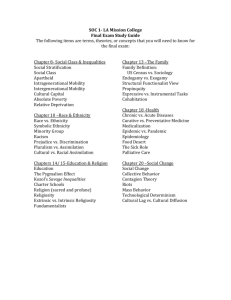
Linking 25% of UK FP’s pay to quality of care: a major experiment in quality improvement Martin Roland Director National Primary Care Research and Development Centre University of Manchester UK 100% quality Baseline quality these things MajorAll UK of initiatives • National - nostandards magic bullet • Clinical governance • Annual appraisal • Public release • Patient safety • Collaboratives • Inspection • Contracts ? Guidelines Audit / feedback Opinion leaders Financial incentives Changes in doctors’ views 1980-2002 “With one mighty leap, the NHS vaults over anything being attempted in the 1980s • Quality can’t be measured • There’s no such thing as a bad doctor United States, the previous leader in quality improvement initiatives.” Shekelle P. British Medical Journal (editorial) 2003; 326: 457-8 2002 • Care is too variable • Quality can be measured • Care can be improved • It’s expensive to provide high quality care • We want to be resourced and rewarded for providing high quality care Quality incentive scheme offering up to 25% increased income to FPs New FP contract: Quality and Outcomes Framework Collaboration between 25% of income from quality incentives • Chronic disease management •Government • Health care quality = electoral liability •Academics • Methods of measuring quality • Practice organisation • Cultural shift: Quality needs to be improved + opportunity for increased income • Patient experience •Physicians (Ten conditions) (Five areas) Roland M. Linking physician pay to quality of care. New England Journal of Medicine 2004; 351: 1448-54. 1 Seventy six clinical indicators covering: Coronary heart disease and heart failure (15) Stroke and transient ischemic attack (10) Hypertension (5) Diabetes (18) Epilepsy (4) Hypothyroidism (2) Mental health (5) Asthma (7) Chronic obstructive pulmonary disease (8) Cancer (2) CHD 7. The percentage of patients with coronary heart disease whose notes have a record of total cholesterol in the previous 15 months. Point score: from 1 point (25%) to 7 points (90%) CHD 8. The percentage of patients with coronary heart disease whose last measured total cholesterol (measured in the last 15 months) is 290mg/dl or less Point score: from 1 point (25%) to 16 points (60%) Exception reporting for clinical indicators 56 organisational indicators: • Patient refused / not attended despite three reminders Records (19) • Not appropriate e.g. supervening clinical condition, extreme frailty, adverse reaction to medication, contraindication etc Information to patients (8) Education and training (9) • Newly diagnosed or recently registered • Already on maximum tolerated doses of medication Practice management (10) Medicines management (10) • Investigative service is unavailable Examples of organisational indicators Records Smoking status is recorded for 75% of patients between 15 and 75 Medicines management A medication review is recorded in the preceding 15 months for 80% of patients who receive regular prescriptions but do not need to see the physician each time Four indicators relating to patient experience: Conducting and acting on the results of patient surveys (3) Booking consultations intervals of 10 minutes or more (1) 2 What might the effects be? What might the effects be? • Increased computerization / admin costs • Increased computerization / admin costs • More nurses, larger teams, more specialization • More nurses, larger teams, more specialization • Improved health outcomes • Improved health outcomes • Reduced health inequalities • Reduced health inequalities • More medicalization, less holistic approach • More medicalization, less holistic approach • Worse care for un-incentivized conditions • Worse care for un-incentivized conditions • Gaming or misrepresentation • Gaming or misrepresentation • Change in professional motivation • Change in professional motivation What might the effects be? • Increased computerization / admin costs • More nurses, larger teams, more specialization Potential health impact of new incentives Impact of increasing quality of care from present levels to highest levels specified in contract No of cardiovascular events prevented per 5 years per 10,000 • Improved health outcomes • Reduced health inequalities • More medicalization, less holistic approach Cholesterol lowering in CHD 15.5 • Worse care for un-incentivized conditions Blood pressure control in Hypertension 15.4 • Gaming or misrepresentation • Change in professional motivation What might the effects be? • Increased computerization / admin costs • More nurses, larger teams, more specialization McElduff P. et al. Will changes in primary care improve health outcomes. Quality and Safety in Health Care 2004; 13: 191-197 100 90 80 • Improved health outcomes • Reduced health inequalities • More medicalization, less holistic approach 70 60 • Worse care for un-incentivized conditions • Gaming or misrepresentation • Change in professional motivation 50 1991 1992 1993 1994 1995 1996 1997 1998 1999 Percentage of practices reaching 80% cervical cytology target Baker et al. J. Epidemiology and Community Health 2003; 57: 417-423 3 What might the effects be? 100 90 • Increased computerization / admin costs • More nurses, larger teams, more specialization 80 Affluent areas Deprived areas 70 • Improved health outcomes • Reduced health inequalities • More medicalization, less holistic approach 60 • Worse care for un-incentivized conditions 50 1991 1992 1993 1994 1995 1996 1997 1998 1999 Percentage of practices reaching 80% cervical cytology target • Gaming or misrepresentation • Change in professional motivation Baker et al. J. Epidemiology and Community Health 2003; 57: 417-423 What might the effects be? What might the effects be? • Increased computerization / admin costs • Increased computerization / admin costs • More nurses, larger teams, more specialization • More nurses, larger teams, more specialization • Improved health outcomes • Improved health outcomes • Reduced health inequalities • Reduced health inequalities • More medicalization, less holistic approach • More medicalization, less holistic approach • Worse care for un-incentivized conditions • Worse care for un-incentivized conditions • Gaming or misrepresentation • Gaming or misrepresentation • Change in professional motivation • Change in professional motivation What might the effects be? • Increased computerization / admin costs • More nurses, larger teams, more specialization • Improved health outcomes • Reduced health inequalities • More medicalization, less holistic approach • Worse care for un-incentivized conditions • Gaming or misrepresentation • Change in professional motivation “My collective noun for GPs is a grasp of GPs” “The inter-personal side is going to go because the ticks in boxes are going to be all that’s important ..... it’ll be the death of generalism and holistic care …” “The idea of putting the resources where the morbidity is strikes me as a big advance … and I’m only sorry that it has been softened by the bleatings of those who’ve had it too soft for too long” 4 Paying physicians: economic theory Salary Do as little as possible for as few people as possible Capitation Do as little as possible for as many people as possible FFS Do as much as possible, whether or not it helps the patient Quality Carry out a limited range of highly commendable tasks, but nothing else 0 10 % of practices 20 30 40 50 Early results – Scotland % of maximum available points scored 0 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 85 90 95 100 Total points scored Changes in management of diabetes 1998-2003 60 50 40 30 20 10 0 Serum cholesterol 5mmol/l or less BP 150/90 or less 1998 HbA1c <7.4% 2003 5