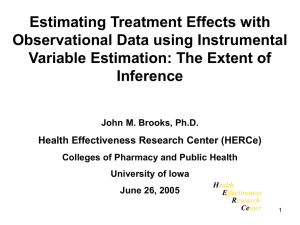
Estimating Treatment Effects with Observational Data using Instrumental
Estimating Treatment Effects with
Observational Data using Instrumental
Variable Estimation: The Extent of
Inference
John M Brooks. Ph.D.
Health Effectiveness Research Center (HERCe)
Colleges of Pharmacy and Public Health
University of Iowa
June 8, 2004
H ealth
E ffectiveness
R esearch
Ce nter
1
Research Goal:
Estimate casual relationships between
"treatment" and “outcome” in healthcare...
• treatment on outcome
• behavior on outcome
• system change on outcome
2
The best estimation method to make inferences about these relationships is a function of:
1. the manner in which the researcher collects data; and
2. the approach used to control for “confounding factors” confounding factors: factors related to both the treatment and outcome.
3
Research Environments and Estimation Methods
Statistical “Matching”
Techniques (Propensity Scores)
Secondary
Databases
ANOVA
Quasi-Experimental Designs
Logistic Regression
Instrumental Variables
Multiple Regression
– “Ex Post Design” – “Risk Adjustment”
Design Control of
Confounding Factors
Statistical Control of
Confounding Factors
Entirely Controlled
Experiment -
– Randomized
2
Tests
Controlled Trials
Weighted Regression
Techniques of Survey
Databases:
• NMES
• MEPS
Researcher-Collected
Databases
4
Sources of Treatment Variation in Health Care
1. Randomized Controlled Trials: study of patients with a given medical condition in which treatment is randomly assigned.
• Why randomly assign treatment to patients?
To help ensure that estimated treatment affects are attributable to the treatment and not unmeasured confounders.
The Gold Standard
5
• Why don’t we do more Randomized Controlled Trials between approved treatments?
→ ethical problems
→ expensive and time-consuming
→ little motivation
→ inability to generalize
6
2. Observational Healthcare Databases
• Database Types:
→ Claims: medical service treatment claims from individuals with health insurance
→ Provider-Specific: databases describing the utilization of a set of providers.
→ Health Care Surveys: surveys of patients or providers detailing health care utilization.
7
• Strengths:
→ plenty of variation in treatment choice;
→ potentially enhanced ability to generalize – reveals variation in treatment choice across a variety of clinical scenarios;
→ can assess treatments in practice – estimate
“effectiveness”;
→ unobtrusively collected;
→ the power of large numbers and time.
8
• Weaknesses:
→ data usually not collected for researcher purposes;
→ missing information;
- care not covered is not observed
- care not claimed is not observed
- claim form limitations
nuances of illness, treatment, and patient that can’t be recorded on claims forms
→ patient enrollment variation ;
→ confounding information may be unobserved.
9
Is the Main Source of Weakness with Observational Data
Unmeasured Confounders or Treatment Selection Bias?
1. Unmeasured Confounders
• Unmeasured Confounders argument:
→ homogenous treatment effect;
→ unmeasured factors related to both treatment and outcome is the source of bias.
10
• Assume true outcome relationship is:
Y = a o
+ a
1
•T + a
2
•L + e where:
Y = measure of outcome (e.g. 1 if survive to a certain time period, 0 otherwise);
T = 1 if receive treatment, 0 otherwise; and
L = additional factor (e.g. severity, other treatments).
Goal is to estimate a
1
– the effect of treatment on outcome.
11
• For Estimation Suppose:
→ L is not measured and the estimation model is:
Y = a o u
+ a
1
•T + u where:
= (a
2
•L + e)
→ L is related to Y (a
2
≠ 0); and
→ T and L are related (Cov(T,L) ≠ 0).
Cov(T,L) – covariance of T & L. Cov(T,L) ≠ 0 essentially means that T & L move together.
12
• Define the ordinary least squares (ANOVA) estimate of a
1
aˆ
aˆ a biased estimate of a
1 through its expected value:
E
[
a
1
]
= a
1
+ Cov(T,L) •a
2
E [ ]
1 if either:
-- Cov(T,L) = 0; or
-- a
2
= 0.
13
• Suppose theory about the unmeasured variable “L” suggests:
→ “a
2
< 0” (patients with higher severity have lower cure rate).
→ Cov(T,L) > 0 (treated patients are generally more severe).
• Plug in “signs” into our expected value formula to find:
E [ a
1
]
a
1
(
)(
)
(
)
E
[
a
1
]
< a
1
.
14
• Problem with the Unmeasured Confounders argument to describe bias in observational data:
→ It does not provide a theoretical foundation to link treatments to unmeasured factors....
Why is Cov(T,L) ≠ 0?
→ In the case we just described, if treatment effect (a
1
) is the same for all patients, why would Cov(T,L) > 0?
Perhaps patients getting treatments:
-- live in areas with high/low poverty;
-- live in areas with more pollution; or
-- also tend to get other unmeasured treatments.
15
2. Treatment Selection Bias (the gestalt underlying most negative reviewer’s comments)
• Treatment Selection Bias argument:
→ heterogeneous treatment effect -- Cov(T,L) reflects the decisionmaker’s beliefs about the differences in treatment effectiveness across patients; and
→ bias comes from unmeasured factors (severity, other treatments) related to the treatment’s expected effectiveness that affects both
treatment choice and outcome.
16
• Assume true outcome relationship is:
Y = b o
+ (b
1
+ b
2
•L) •T + b
3
•L + e where:
Y = measure of outcome (e.g. 1 if survive to a certain time period, 0 otherwise);
T = 1 if receive treatment, 0 otherwise;
L = unmeasured factor (e.g. severity, other treatment); b
3
= the direct effect of L on Y; and
(b
1
+ b
2
•L) = effect of T on Y that depends on L.
17
→ L is now related to T through theory linking "treatment choice" to the decision-makers expectations of treatment benefits across patients with different “L”.
T = c o
+ c
1
•L + c
2
•W + v where:
T = 1 if receive treatment, 0 otherwise;
L = unmeasured factor (e.g. severity, other treatment) affecting treatment choice through
expected treatment effectiveness; and
W = other factors affecting treatment choice.
If decision makers use L in treatment decisions, c
1
≠ 0 and Cov(T,L) ≠ 0.
18
• Ultimate goal should be to estimate (b
1
+ b
2
•L) – the
effect of treatment T on outcome Y across levels of L.
• For estimation suppose:
→ L is not measured and it is wrongly assumed by the researcher that the effect of T is homogenous, the estimation model is:
Y = a o
+ a
1
•T + u where: u = (b
2
•L•T + b
3
•L + e)
19
• Define the ordinary least squares (ANOVA) estimate of a
1
aˆ
→
aˆ
1
E
1
b
1
b
2
E [ T ]
E var[ T
[
]
L ]
c
1
( b
2
b
3
E
1
→ If c
1
= 0 (no selection based on L), then becomes:
E
1
b
1
b
2
E [ T ]
E var[ T
[ L ]
]
)
Yields an average estimate that depends on the mix of
“L” in the population (e.g. RCT using a broad population).
20
• How does c
1
• (b
2
+ b
3
) affect this estimate?
→ Assume that L is unmeasured illness severity and that higher L means more severe illness.
→ Higher L lowers survival which implies b
3
< 0.
→ If treatment benefit is less for more severe cases
(e.g. surgery for heart attacks) then: b
2
0
c
1
0
c
1
b
2
b
3
0 benefit falls less treatment with higher in more severity severe cases
Estimate of average population treatment benefit will
21 be biased high.
→ If treatment benefit is greater for more severe cases
(e.g. antibiotics for otitis media) then: b
2
0
c
1
0
c
1
b
2
b
3
?
0 benefit increases more treatment with higher in more severity severe cases
Estimate of average population treatment affect is biased but sign can not be determined.
22
• So what do we have here?
→ Observational data contains enormous treatment variation.
→ Treatment choice may be related to the selection or sorting of patients using unmeasured (to the researcher) characteristics that are related to expected outcomes.
→ Under “selection”, standard statistical techniques yield biased estimates that don’t apply to anyone anyway.
Do we have any alternatives?
23
Instrumental Variables (IV) Estimation and “Subset B”
• IV estimation offers consistent estimates for a subset of
patients (McClellan, Newhouse 1993):
Marginal Patients: patients whose treatment choices vary with measured factors called instruments that do not directly affect outcomes.
• McClellan and Newhouse argue that estimates of treatment effects for Marginal Patients are useful:
→ They are estimates for patients for whom the benefits of treatment are the least certain – patients least like those in
RCTs.
→ Estimates may be more suitable than RCT estimates to address the question of whether existing treatment rates
should change.
24
• Where do Marginal Patients come from?
Distribution of Patients by Prior Assessment of the Certainty of Treatment Benefit
A
0%
More certainty about treatment benefits
B
50%
C
100%
Less certainty about treatment benefits
A = subset of patients all providers agree to treat.
C = subset of patients all providers agree not to treat.
B = subset of patients whose treatment choice is situation/provider dependent.
25
• Patients in Subset B are interesting because:
→ the “best” treatment choice (treat or don’t treat) is least certain;
→ treatment or no-treatment for a patient in this subset is
not considered bad medicine – the “art” of medice;
→ the possibility of gaining new RCT evidence for patients in this subset is remote (ethics, motivation);
→ McClellan et al. 1994 argue that policy interventions affect mainly the treatment choices for patients in this subset; and
→ Non-clinical factors (e.g. provider access, market pressures) affect mainly the treatment choices of patients in this subset.
26
• Size and location of Subset B varies with clinical scenario.
treatment with little consensus (e.g. aggressive treatment
for early-stage prostate cancer):
A
0%
More
Certainty
B
50%
C
100%
Less
Certainty
off-label use for new treatment (e.g. new anti-cancer
drugs used in non-tested cancer populations):
B
0%
More
Certainty
C
50% 100%
Less
Certainty
27
• Changes in the underlying population definition will affect
the location of Subset B.
aggressive treatment for early-stage prostate cancer for
50-60 year-olds with no comorbidities:
0%
More
Certainty
A
50%
B C
100%
Less
Certainty
aggressive treatment for early-stage prostate cancer for
70-80 year-olds with one comorbidity:
A
0%
More
Certainty
B
50%
C
100%
Less
Certainty
28
• IV estimation involves:
1. Finding measured variables or “instruments” (Z) that: a. are related to the possibility of a patient receiving treatment (cov(T,Z) ≠ 0); and b. are assumed (through theory) unrelated directly to Y or to unmeasured confounding variables (cov(Z,L) = 0).
The theoretical basis for “Z” variables should come from a model of treatment choice – the “W” variables in:
T = c o
+ c
1
•L + c
2
•W + v where:
W = other factors affecting treatment choice.
29
• IV estimation involves con’t:
2. Grouping patients using values of the “instrument”.
3. Estimate treatment effects for marginal patients by exploiting treatment variation rate differences across patient groups.
Local Average Treatment Effect --
(Imbens & Angrist 1994)
30
• For example, if an instrument divides patients into two groups, a simple IV estimate can be found by calculating:
1. the overall treatment rate in each group (t i rate in group “i”); and
= treatment
2.
the overall outcome rate in each group (y i rate in group “i”); and estimate:
= outcome a
ˆ
1 IV
difference in outcome rate difference in treatment rate
y
1 t
1
t y
2
2 where:
ˆ
1 IV
= average treatment effect for the “marginal patients” specific to the instrument used in the analysis – only those patients whose treatment choices were affected by the instrument who must have come
31 from Subset B .
• Hypothetical Treatment Choices Across Patients
Grouped by Access to Providers Required for Treatment
Patient Group Closer to Providers Required for Treatment: treated
A B M C
0%
More Certainty
100%
Less Certainty
Patient Group Further From Providers Required for Treatment:
A treated
B M
50% 60%
C
0%
More Certainty
100%
Less Certainty
M = patients within Subset B whose treatment choices are affected by the instrument – the Marginal
Patients for that instrument .
32
• We have treatment rates for each group:
Closer Group Treatment Rate: .60
Further Group Treatment Rate: .50
Suppose we also measured “cure” rates in both groups:
Closer Group Cure Rate: .40
Further Group Cure Rate: .38
• Four numbers lead to the following IV estimate: aˆ
1 IV
.
40
.
6
.
38
.
5
.
02
.
1
.
2
33
• Strict Interpretation:
→ If the treatment rate in the Further Group was increased .01
percentage point (e.g. .50 to .51) by increasing treatment for the M patients in the Further Group , the Cure rate in the
Further Group would increase .002 (.01 • .2) – from .38 to
.382.
• Stretched “Policy-Relevant” Interpretation (McClellan et al.
1994)
→ A behavioral intervention that increases the overall treatment rate by .01 percentage point (e.g. .55 to .56) would lead to an increase in the cure rate of .002 (.01 • .2).
34
• Stretched interpretation assumes that the treatment effect for patients in Subset B is fairly homogenous and an IV estimate from a single instrument can be generalized to all patients in Subset B. This allows one to say:
• Stretched interpretation is not perfectly accurate if treatment effects are heterogeneous within Subset B and different instruments affect treatment choices from different patients within Subset B.
→ Results from a single instrument may still be more appropriate than assuming RCT results apply to Subset B.
→ Ability to generalize results may increase if more than one instrument is used in an IV analysis.
35
• IV qualifiers to remember:
→ second property of IV variables (cov(Z,L) = 0) is forever an assumption (unless more data are obtained); and
→ unmeasured but correlated treatments may still bias estimated treatment benefits.
Researchers should fully qualify their IV estimates – don't oversell.
36
Hypothetical Example to Demonstrate “4-Number” Result
Suppose:
• 2100 children with Acute Otitis Media (AOM) in a population.
• Two treatment possibilities:
1.
2.
antibiotics; watchful waiting.
• The patients in our sample are in one of three severity types “low”, “medium”, and “high”
• Severity type is observed by the provider/patient but is not observed by the researcher.
37
• The 2100 patients are distributed across severity type in the following manner: number of patients
High
800 severity type
Medium
800
Low
500
• The actual underlying cure rates for each severity type by treatment are: treatment antibiotics watchful waiting
High
.95
.80
severity type
Medium
.97
.90
Low
.98
.98
38
→ Higher severity means a lower the cure rate in general
(b
3
< 0).
→ Antibiotics have a higher curative effect in more severe patients and offer no advantage to the less severe (b
2
> 0).
ASSUMPTION: Treatment effects are heterogenous.
→ All providers have inclination that antibiotics work well in the "high" severity patients; have little effect on the "low" severity patients; but the effect in the "medium" type is unknown to providers.
Leads to selection bias...the more severe kids are treated (c
1
> 0).
39
Potential Methods to analyze:
1. Randomize Patients Into Treatments -- ANOVA
2. Providers Assign Treatments -- ANOVA
3. Instrumental Variable Grouping
40
1. Randomize Patients Across Population – ANOVA.
Patient Treatment Assignments After Randomization by Severity Type patient groups antibiotics watchful waiting
High severity type
Medium
400
400
400
400
Low
250
250
41
Expected average cure rates for each group:
Antibiotic Cure Rate
400
1050
.
95
400
1050
.
97
250
1050
.
98
.
965
W .
W .
Cure Rate
400
1050
.
80
400
1050
.
90
250
1050
.
98
.
881
• Unbiased average antibiotic treatment rate for the entire population (.965-.881 = .084), but
• To whom does it apply? A patient randomly chosen from an urn? Are patients chosen from urns?
42
2.
Providers Assign Treatments -- ANOVA
If providers follow “inclinations”, we may end up with something like:
Number of Patients Assigned by Providers to Each
Treatment Group by Severity Type patient group antibiotics watchful waiting
High
800
0 severity type
Medium
400
400
Low
0
500
43
Expected average cure rates for each group:
Antibiotic Cure Rate
800
1200
.
95
400
1200
.
97
0
1200
.
98
.
957
W .
W .
Cure Rate
0
900
.
80
400
.
90
900
500
900
.
98
.
944
• For this population the average treatment effect is (≈.084).
We find a biased low estimate of the antibiotic treatment effect for the average patient (.957 - .944 = .013 < .084).
• To which patients does this estimate apply?
44
3. Instrumental Variable Grouping -- Further: a.
Assume information is available to approximate distances from patients to providers
• address of patient
• supply of providers in area around patients b.
Evidence suggests that patients in areas with more physicians per capita have a higher probability of being treated with antibiotics for their AOM than patients in areas with fewer physicians per capita.
45
If “b” is true, divide 2100 patients into two groups based on the physicians per capita in the area around their home:
Group 1: the group of patients living in areas with a higher number of physicians per capita;
Group 2: the group of patients living in areas with a lower number of physicians per capita;
46
Using our assumptions, does this grouping qualify as an instrument?
1. Doc supply related to treatment? Yes, if patients tend to go to the closest provider for treatment.
If true, and providers follow inclinations we may see treatment patterns something like:
Patient Treatment Assignments by Severity Type patient group High severity type
Medium Low
Group 1 100% antibiotics 80% antibiotics 100% W.W.
20% W.W.
Group 2 100% antibiotics 30% antibiotics 100% W.W.
70% W.W.
47
2. Is grouping related to unmeasured confounding variables
(e.g. severity)? Related to severity only if parents chose residences in expectation of the severity of a future acute condition.
If not related to severity, we assume equivalent severity distributions across groups:
Number of Patients in Each Group by Severity Type patient group High
Group 1
Group 2
400
400 severity type
Medium
400
400
Low
250
250
48
Expected average estimated cure rates for these groups:
Group 1 Cure Rate
400
1050
.
95
320
1050
.
97
80
1050
.
90
250
1050
.
98
.
959428
Group 2 Cure Rate
400
1050
.
95
120
1050
.
97
280
1050
.
90
250
1050
.
98
.
946092
Well, (.959428 - .946092) = .013336 doesn't appear to reveal much of anything…
49
Now look at the antibiotic treatment rate in each group:
720/1050 = .68571 in Group 1
520/1050 = .4952381 in Group 2
These differences also don't look very informative….
The IV change in the cure rates resulting from a one unit increase in the drug treatment rate equals: a
1 IV
.
959428
.
946092
.
68571
.
4952381
.
013336
.
190471905
.
07
• This estimate is the average difference in the antibiotic cure rate for the marginal or in this example the “Medium” severity patients.
50
• Remember the actual “unknown” cure rates for each group by treatment are: treatment antibiotics watchful waiting
High
.95
.80
severity type
Medium
.97
.90
.07
Low
.98
.98
• This estimate was found using only measured treatment rates and outcome rates across “groups” that are defined by the instruments.
• Which of the estimates above is the most important for policy-makers wondering about over/underutilization of a treatment?
51
IV Brass Tacks
• Where do instruments come from?
→ Theory on what motivated choices, not theory on how choices can be motivated.
→ Observed differences in:
-- guideline implementation (timing/interpretation)
-- product approval rules across payers
-- reimbursement across payers/geography
-area provider “treatment signatures”
-- geographic access to relevant providers
-- provider market structure/competition
→ Generally, “Natural Experiments” (Angrist and Krueger,
2001)
52
• General IV Estimation Model
Treatment Choice Equation (1st stage):
T i
c
0
c
2
X i
c
3
Z i
v i
c
1
L i
Outcome Equation (2nd stage):
Y i
a
0
a
1
T
ˆ
i
a
2
X i
e i
a
3
L i
Y i
= 1 if health outcome occurs, 0 otherwise;
X i
= measured patient clinical characteristics;
T i
= 1 if patient received treatment, 0 otherwise;
Tˆ i
= predicted treatment from 1st stage;
Z i
= a set of binary variables to grouping patients based on values of instrumental variables (from W); and
L i
= unmeasured confounding variables assumed related to both Y and T but not Z (from W).
The only variation in T used to estimate a
1 comes from Z.
53
→ The estimate of a
1 can only be definitively generalized to the patients whose treatment choices were affected by Z (Angrist, Imbens, Rubin 1996).
→ F-test of whether the parameters within c
3 are simultaneously equal to zero provides a test of the first instrumental variable criterion:
Finding measured variables or “instruments” (Z) that: a. are related to the possibility of a patient receiving treatment (cov(T,Z) ≠ 0)
54
→ Model can be estimated via:
-- Two-Stage Least Squares (2SLS) – PROC
SYSLIN in SAS.
-- Bivariate Probit – BIPROBIT function in STATA.
-- Two-Stage Replacement (e.g. Beenstock &
Rahav, 2002).
→ 2SLS offers consistent estimates that are asymptotically normal with the fewest assumptions
(Angrist 2001).
-- essentially regressing group-level outcome rate changes on group-level treatment rate changes.
55
• How many groups?
→ Z can be specified as a continuous variable, but results are then conditional on this assumption and is less interpretable.
→ Creating many groups from an instrument (more binary variables in Z) uses more information and yields a weighted average of many two-group comparisons, e.g.
-- low/high groups using the median of the instrument
VS
-- low/med low/med high/high groups using the quartiles of the instrument.
→ Too many groups may introduce bias.
→ Best to report estimates for several grouping strategies.
56
• Example: The effect of breast-conserving surgery
(BCS) relative to mastectomy (MAS) for stage
II breast cancer patients (Brooks et al. 2003).
→ Sample: ESBC Stage II patients (N = 2,905) from the
Iowa SEER Cancer Registry, 1989-1994 that had either BCS or MAS.
→ Measures:
-- Treatment: Had BCS plus irradiation.
-- Outcomes: Survival 1, 2, 3 and 4 years.
→ Instrument: BCS percentage for all other early-stage breast cancer patients in 50-mile radius of patient zip code in diagnosis year.
57
Comparison of Characteristics of ESBC Patient Groups
In Iowa, 1989-1994: Treatment vs. Area BCS Rates
Group based on actual treatment choice
Group based on area treatment signature
Patient
Char’s BCS Mastectomy
High
BCS area a
Low
BCS area
BCS % 100 0 12*** 8 a .
Under 65 % 67*** 44 53*** 48
65 to 74 % 22 25 23 25
Over 74 % 9*** 27 24 27
Stage IIb % 21*** 35 35 33
Comor Index b .15*** .31 .31 .28
Number 2622 283 1225 1680
***,**,* significant differences at the .01, .05 and .10 percent confidence levels, respectively.
a. Based on 50mile radius around patient’s zip code in year of diagnosis. High areas have BCS percentage greater than or equal to 22% (includes stage I patients). Low areas have BCS percentages less than 22%. Rates are calculated excluding the patient. b. Modified version of Charlson Co-morbidity index using non-cancer ICD9 codes from patient’s hospital discharge abstracts. Equals one if index is greater than zero, zero otherwise.
58
Marginal Stage II Early Stage Breast Cancer
Patients in Iowa, 1989-1994
M
0% 8%
More
Certain
For BCS
12% 50% 100%
Less
Certain for
BCS
M = patients whose treatment choice is dependent on the practice inclinations of local providers – Marginal
Patients.
59
→ IV estimates using area BCS rate as instrument.
Number of groups
Instrument
F-statistic
2
4
8
12
8.57***
5.19***
3.43***
3.00***
After diagnosis, effect of BCS on patient survival:
1 year 2 years 3 years 4 years
-0.32
-0.68
-0.37** -0.54**
-0.57
-0.45
-0.33** -0.50** -0.46*
-0.23** -0.41** -0.33
-0.51
-0.65*
-0.52*
-0.11
***,**,* statistically significant at .99, .95, and .90 confidence, respectively.
60
• How many instruments?
→ Patients in Subset B affected by instruments may vary across instruments, so IV estimates may vary.
→ IV estimates using Distance to Radiation as an instrument:
Number of groups
2
4
8
12
Instrument
F-statistic
21.79***
7.52***
3.30***
2.94***
After diagnosis, effect of BCS on patient survival:
1 year 2 years 3 years 4 years
-0.21*
-0.14
-0.14
-0.05
-0.12
-0.22
-0.19
-0.14
-0.33
-0.39
-0.35
-0.33
-0.23
-0.38
-0.28
-0.40*
***,**,* statistically significant at .99, .95, and .90 confidence, respectively.
61
→ IV estimates using both area BCS rate and distance to radiation:
Number of groups
8
12
2
4
Instrument
F-statistic
13.08***
4.99***
2.76***
2.74***
After diagnosis, effect of BCS on patient survival:
1 year 2 years 3 years 4 years
-0.24** -0.25
-0.24** -0.32*
-0.38*
-0.39*
-0.24** -0.31** -0.34*
-0.12* -0.23** -0.30**
-0.30
-0.45*
-0.27
-0.15
***,**,* statistically significant at .99, .95, and .90 confidence, respectively.
→ Each instrument remained independently significant.
→ Estimates are “weighted average”.
62
• Which Sample?
→ Estimates for Marginal Patients may vary by sample.
stage II state I
8-Group Estimates by Cancer Stage and Instrument
After diagnosis, effect of BCSI on patient survival:
Cancer
Stage Instrument
BCS Rate
Rad Dist
Both
BCS Rate
Rad Dist
Both
Instrument
F-statistic
3.43***
3.30***
2.76***
0.69
3.36***
1.77**
1 year
-0.33** -0.50** -0.46* -0.52*
-0.14
-0.19
-0.35
-0.28
-0.24** -0.31** -0.34* -0.27
-0.06
-0.09
-0.09
2 years
-0.07
0.04
-0.02
3 years
-0.04
0.22*
0.19
4 years
0.18
0.16
0.18
***,**,* statistically significant at .99, .95, and .90 confidence, respectively.
63
• Which Sample (Example 2)?
→ Effects of Catheterization on AMI Patient Mortality by Insurance Status using Differential Distance as an Instrument (Brooks et al. 2000).
→ Data from Washington State 1989-1993
Insurance
Group Obs
Private – Non HMO 6,121
Private HMO
Medicaid
Self-Pay
1,408
1,285
765
Average
Age
Cath
Rate
54.8
77.8
54.5
69.6
53.2
67.3
54.0
64.7
IV Estimate of Cath on 1-
Year Mortality Rates
-0.104***
-0.132***
-0.119*
-0.194***
***,**,* statistically significant at .99, .95, and .90 confidence, respectively.
→ Lower catheterization rate reveals higher benefit for marginal patients.
64
Summary
• The foundation of IV estimation is theory that suggests instruments – what factors motivated treatment choices.
• Ability to generalize is limited, but IV estimates offer a more natural estimate of the effects of rate changes than
RCT estimates.
• Estimates can vary by sample and instrument used.
• Estimates are conditional on the truth (and acceptance) of a known identification restriction. The source of the treatment variation is known. The relationship between this variation and unmeasured confounders can be debated.
65
References
Angrist JD, 2001. Estimation of Limited Dependent Variable Models with Dummy Endogenous Regressors: Simple
Strategies for Empirical Practice. Journal of Business & Economic Statistics. 19(1):2-16
Angrist, JD, Imbens GW, Rubin, DB. 1996. Identification of Causal Effects Using Instrumental Variables. Journal of the
American Statistical Association. 91:444-454.
Angrist JD, Krueger AB. 2001. Instrumental Variables and the Search for Identification: From Supply and Demand to
Natural Experiments. Journal of Economic Perspectives. 15(4): 69-85.
Brooks JM, Chrischilles E, Scott S, Chen-Hardee S. 2003. Was Lumpectomy Underutilized for Early Stage Breast
Cancer? – Instrumental Variables Evidence for Stage II Patients from Iowa. Health Services Research, 38(6):1385-
1402.
Brooks JM, McClellan M, Wong H. 2000. The Marginal Benefits of Invasive Treatment for Acute Myocardial Infarction:
Does Insurance Coverage Matter? Inquiry, 37(1):75-90.
Imbens GW, Angrist, JD. 1994. Identification and Estimation of Local Average Treatment Effects, Econometrica.
62(2):467-475.
McClellan M, McNeil BJ, Newhouse JP. 1994. Does More Intensive Treatment of Acute Myocardial Infarction in the
Elderly Reduce Mortality: Analysis Using Instrumental Variables", Journal of the American Medical Association.
272:859-866.
McClellan M, Newhouse JP. 1993. The Marginal Benefits of Medical Treatment Intensity. Cambridge,Mass: National
Bureau of Economic Research: Working Paper.
McClellan M, Newhouse JP. 1997. The Marginal Cost-Effectiveness of Medical Technology - a Panel Instrumental
Variables Approach, Journal of Econometrics. 77:39-64.
66