New Zealand’s no-fault system Ron Paterson NZ Health and Disability Commissioner
advertisement

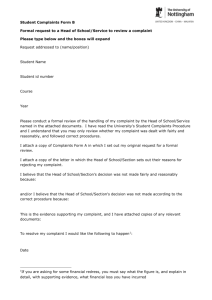
New Zealand’s no-fault system Ron Paterson NZ Health and Disability Commissioner San Diego, June 2004 Case study: Misdiagnosed MI Mr A, a 36-year old man, presented to a medical centre with chest tightness and shortness of breath. He had a strong family history of heart disease The nurse took an ECG which indicated significant myocardial infarction Dr B, the on-call doctor, diagnosed a chest infection and sent Mr A home Case study: Misdiagnosed MI Mr A died at home 2 hours later Post-mortem showed the cause of death to be ischaemic heart disease Image: www.ecglibrary.com Why can’t Mr A’s family sue Dr B? Since 1974, medical malpractice claims have been effectively prohibited in New Zealand, even for gross negligence Why can’t Mr A’s family sue Dr B? Compensation for medical injury is provided by the Accident Compensation Corporation, a state-funded insurer Concerns about the quality of medical care are resolved by an independent Ombudsman, the Health and Disability Commissioner Unhappy patient Claim Accident Compensation Corporation Compensation Complaint Health care provider Health and Disability Commissioner Complaint resolution Professional discipline Competence review Which medical injuries get cover? Currently, compensation is available for: (1) medical error (the failure to observe a standard of care reasonably to be expected in the circumstances); and (2) medical mishap (a rare and severe adverse outcome of treatment that is properly given) Are any reforms planned? Ruth Dyson, ACC Minister In 2005, medical compensation will be widened to cover ‘treatment injuries’ The reforms will remove any consideration of fault, rarity or severity These reforms will cost US$5.37 million per year on top of the US$29 million spent currently Case study: Misdiagnosed MI The Accident Compensation Corporation accepted that Mr A’s death was the result of medical error Mr A’s widow received compensation for funeral costs and loss of income Who can complaint to HDC? Any person can complain to the Health and Disability Commissioner, orally or in writing, alleging breach of a patient’s rights Which rights are in the Code? The Code of Consumers’ Rights sets out ten rights relating to the quality of care The Commissioner’s jurisdiction does not extend to issues of access of funding What is the Commissioner’s role? Education Learning, not lynching Complaints resolution Resolution, not retribution Case study: Misdiagnosed MI Mr A’s wife complained to the Health and Disability Commissioner about the poor standard of care provided to her late husband by Dr B How are complaints resolved? HDC supports low-level complaints resolution Advocacy and mediation are often successful Investigation is reserved for serious complaints Judi Strid, Director of Advocacy What is the investigation process? Inquisitorial, not adversarial Expert advice on clinical issues Can examine systems issues Cases are decided “on the papers” – usually no face to face hearing Case study: Misdiagnosed MI HDC asked Dr B to respond to Mrs A’s letter of complaint Dr B accepted that he had misread the ECG and failed to recognise the seriousness of Mr A’s condition Dr B provided evidence that, at the time of the consultation, he had been suffering from undiagnosed concussion following an altercation with his neighbor Case study: Misdiagnosed MI The evening of the death, Dr B had visited Mr A’s widow to apologise and offer his condolences Dr B normally had no problem reading ECGs, but he nevertheless undertook further training following this incident Case study: Misdiagnosed MI Mrs A’s complaint was upheld – Dr B had failed to exercise reasonable care and skill when assessing Mr A’s chest pain Dr B’s personal circumstances (the concussion) did not dilute his professional duty of care, but were relevant in deciding what further actions were needed Do many complaints end in discipline? 714 complaints to HDC 337 investigations 106 breach findings 8 disciplinary hearings 2002/2003 Professional discipline Health and Disability Commissioner acts as gatekeeper to disciplinary proceedings Medical Practitioners Disciplinary Tribunal may remove a doctor’s name from the Medical Register, place conditions on a doctor’s practice, and/or impose a fine Case study: Misdiagnosed MI HDC decided not to refer this case forward for possible disciplinary action HDC sent a copy of the report to Dr B’s professional body, the Medical Council, to keep on their records HDC also sent a copy to Dr B’s employer, the Medical Centre, which confirmed new procedures for sick staff Medical Discipline in NZ 1994-2003 90 Number of doctors facing disciplinary charges 80 70 60 50 40 30 20 10 0 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 MPDC l MPDT Building a fence at the top of the cliff Individual complaints offer a window of opportunity to improve health services generally. Case study: Misdiagnosed MI In response to Mrs A’s complaint, the Medical Centre implemented a policy on staff impairment and illness, including a stand-down period after head injury The anonymised report was widely disseminated for educational purposes, discussed in a medical journal, and placed on HDC’s website www.hdc.org.nz (02HDC01833) No greener pastures New Zealand remains the safest place in the world to practise medicine. Professor Peter Skegg, 2003 The bottom line New Zealand’s ‘no fault’ compensation system is consistent with efforts to improve the quality of health care but needs to be complemented by a flexible and effective complaints system. Peter Davis, Inaugural lecture, 2000