Analytic Considerations for Collecting Data on Race, Ethnicity, and Language November 30, 2010
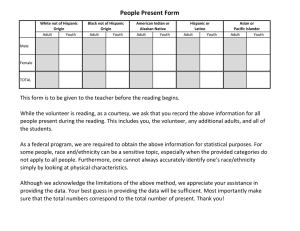
advertisement

Analytic Considerations for Collecting Data on Race, Ethnicity, and Language Romana Hasnain-Wynia, Ph.D., Northwestern University November 30, 2010 AcademyHealth The professional society of health services research and health policy analysis. AcademyHealth represents a broad community of people with an interest in and passion for using health services research to improve health care. We promote interaction across the health research and policy arenas by bringing together a broad spectrum of players to share their perspectives, learn from each other, and strengthen their working relationships. www.academyhealth.org Aetna Foundation The Aetna Foundation is a national health foundation that promotes wellness, health, and access to high-quality health care for everyone. Our giving is focused on addressing the rising rates of adult and childhood obesity in the U.S.; promoting racial and ethnic equity in health and health care; and advancing integrated health care. Originally founded in 1972 as the independent charitable and philanthropic arm of Aetna Inc., Aetna and the Aetna Foundation have contributed over $379 million in grants and sponsorships since 1980. This work is enhanced by the time and commitment of Aetna employees, who have volunteered nearly 2 million hours since 2003. For more information, visit http://www.aetnafoundation.org. Learning Objectives The goals of this session are to: – Discuss why collecting data to reduce health care disparities is important – Address patient/enrollees concerns – Discuss broad and granular categories – Address the use of the data and data standards The audio and slide presentation will be delivered directly to your computer Speakers or headphones are required to hear the audio portion of the webinar. If you are having difficulties with the audio-stream, please dial (888)-632-5061 and enter the Conference ID number: 92065340 followed by the # sign. Technical Assistance If you require technical assistance, or are having difficulties with the audio portion of this webinar, please click on “Help” Submitting Questions Questions, both substantive & technical in nature, may be submitted at any time during the presentation. Click on “Ask a Question” below this presentation. Complete the form and click “Submit.” Responses will only be sent if related to a technical issue; otherwise you will not receive a confirmation that your question has been received. Faculty Romana Hasnain-Wynia, Ph.D Director, Center for Healthcare Equity Associate Professor, Research Institute for Healthcare Studies Division of General Internal Medicine Northwestern University Feinberg School of Medicine Analytic Considerations for Collecting Data on Race, Ethnicity, and Language Romana Hasnain-Wynia, Ph.D. Northwestern University, Feinberg School of Medicine Agenda Why is collecting data to reduce health care disparities important? Address patient/enrollees concerns Broad and granular categories Use of the data Questions and comments Health Care Should Be Safe Effective Patient-Centered Timely Efficient Equitable Major Reports on Disparities: Plenty of Evidence that Disparities Exist The “Usual” Explanations Patient-Level Patient “preferences”: Treatment refusal, clinical presentation of symptoms, mistrust Communication barriers Provider-Level Beliefs/stereotypes re: patient health and behaviors Inadequate communication Bias/prejudice Organizational –Level Structural and resource differences in where different groups receive care Reducing Disparities Within the Health Care System Kilbourne AM, et al. American Journal of Public Health. 96; 2113-2121: 2006. Why Detecting/Understanding is Important For Health Care Organizations B. Siegel et al. Journal of Healthcare Quality (2007) Hospital and Health Care Leaders--- “NIMBY” N. Lurie, et al. Circulation (2005) 344 Cardiologists: 34% agree disparities exist overall 12% believe disparities exist in own hospital 5% believe disparities exist in own practice S. Taylor, et al. Annals of Thoracic Surgery (2005) 208 Cardiovascular Surgeons: 13% believe disparities occur often or very often 3% believe disparities occur often or very often in own practice T. Sequist, et al. 2008, Journal of General Internal Medicine (2008) 169 Primary Care Clinicians 88% acknowledged that disparities in diabetes care existed in U.S. 40% acknowledged disparities in own practice Detecting and Understanding Quality improvement requires high-quality data. “The first and most critical step for Expecting Success was helping hospitals gather data on patient race, ethnicity and primary language so that they had accurate and complete information about their patients.” Hospital leaders need to be willing to discuss the possibility of disparities. “Physicians and hospital leaders are committed to doing the right thing by their patients, but there is a troubling reluctance among some leaders to consider gaps in the quality of care by patient demographics. Hospital staff must be brave enough to gather data and critically examine the evidence to learn if they are providing care that is high quality and equitable.” Source: Robert Wood Johnson Foundation, Expecting Success: Excellence in Cardiac Care Program The Basic Building Block To eliminate disparities, we need to collect reliable data and then use these data to improve care The Case for Collection of Race, Ethnicity, and Language Data Race, ethnicity, and language data are needed to: Stratify quality performance metrics Organize and focus quality improvement and disparity reduction initiatives Track progress over time, locally and as a nation The Case for Standardization Standardized race, ethnicity and language data: Support comparisons across organizations and regions and over time Support combination of data across organizations or regions to create pooled data sets Support reporting of, and replication of, successful disparity-reduction initiatives Institute of Medicine, 2009 What do patients and health plan enrollees think? “It is important for hospitals and clinics to collect information from patients about their race or ethnic background” Strongly agree Somewhat agree Unsure Somewhat disagree Strongly disagree 43% 37% 6% 10% 4% Baker DW, Cameron KA, Feinglass J, Georgas P, Foster S, Pierce D, Thompson JA, Hasnain-Wynia R. “Patients' attitudes toward health care providers collecting information about their race and ethnicity.” J Gen Intern Med. 2005 Oct;20(10):895-900. “It is important for hospitals and clinics to conduct studies to make sure that all patients get the same high-quality care regardless of their race or ethnic background” Strongly agree Somewhat agree Unsure Somewhat disagree Strongly disagree 93% 4% 2% 1% 0% Baker DW, Cameron KA, Feinglass J, Georgas P, Foster S, Pierce D, Thompson JA, Hasnain-Wynia R. “Patients' attitudes toward health care providers collecting information about their race and ethnicity.” J Gen Intern Med. 2005 Oct;20(10):895-900. “How concerned would you be that this data could be used to discriminate against patients” Not concerned at all A little concerned Somewhat concerned Very concerned 34% 15% 20% 31% Baker DW, Cameron KA, Feinglass J, Georgas P, Foster S, Pierce D, Thompson JA, Hasnain-Wynia R. “Patients' attitudes toward health care providers collecting information about their race and ethnicity.” J Gen Intern Med. 2005 Oct;20(10):895900. Health Plan Enrollees •Collection of language data is not worrisome •Concerns about how health plans would use race/ethnicity data •Concerns about privacy/confidentiality •Despite concerns, could consider ways that data would be useful to plans Hasnain-Wynia R, Taylor-Clark K, Anise A. Medical Care Research and Review. October 2010 Addressing Patients/Enrollees Concerns Tell People Why You are Asking “Now I would like you to tell me your Race and Ethnic Background. We use this to review the treatment patients receive and make sure everyone gets the highest quality of care.” Testing introductions Of the participants who were not completely comfortable reporting their race and ethnicity 25.0% said that the quality statement made them somewhat more comfortable 25.6% said the quality statement made them much more comfortable Far better than the results for the other 3 statements Baker DW, Cameron KA, Feinglass J, Georgas P, Foster S, Pierce D, Thompson JA, Hasnain-Wynia R. “Patients' attitudes toward health care providers collecting information about their race and ethnicity.” J Gen Intern Med. 2005 Oct;20(10):895-900 Broad Categories Granular Categories Race and Ethnicity Institute of Medicine Recommendations Health care organizations must have data on the race, ethnicity, and language of those they serve in order to identify disparities and to provide high quality care. Detailed “granular ethnicity” and “language need” data, in addition to the OMB categories, can inform point of care services and resources and assist in improving overall quality and reducing disparities. Existing Guidance OMB Directive – 1997 Hispanic/Latino Ethnicity 5 Race Categories Progress has been made in incorporating the OMB categories into many data collection activities – not all are aligned The OMB categories are insufficient to illuminate many disparities and to target QI efforts efficiently The Affordable Care Act: Section 4302 Understanding Health Disparities: Data Collection and Analysis Focuses on federal national data collection efforts and the analysis and reporting of these data Race and Ethnicity Guided by OMB standards for race and ethnicity Consultations with OMB, Dept of Labor, Bureau of Census and other federal partners Informed by recent IOM reports on data granularity Section 4302 has great potential to improve data collection by Requiring the DHHS Secretary to establish data collection standards Calling for the use of the standards in federal data collection Instructing that the data be used for analyses and that the results be reported Articulating some important language about funding Data Standards Must be for self-reported measures Or for parents to report for children and guardians to report for legally incapacitated adults Must comply with OMB standards The law states current OMB standards for race and ethnicity must be used at a minimum Modified Office of Management and Budget (OMB) Categories RACE QUESTION: Which category best describes your race? American Indian/Alaska Native Asian Black or African American Native Hawaiian/Other Pacific Islander White Multiracial Declined Unavailable/Unknown ETHNICITY QUESTION: Do you consider yourself Hispanic/Latino? Yes No Declined Unavailable/Unknown Problems with Splitting Race and Ethnicity—OMB Categories Using OMB Categories Without Splitting Race/Ethnicity -African American/ Black -Asian -Caucasian/White -Hispanic/Latino/White -Hispanic/Latino/Black -Hispanic/Latino/Declined -Native American -Native Hawaiian/Pacific Islander -Multiracial -Declined -Unavailable/Unknown Broad Categories Process -Ethnicity first Ethnicity Hispanic or Latino Not Hispanic or Latino Declined Patient unavailable Source: Rohit Bhalla, MD, MPH Montefiore Medical Center Bronx, NY, Expecting Success Site Race American Indian or Alaskan Native Asian Black or African American Native Hawaiian or Other Pacific Islander White Multiracial: Asian/Black-African American Multiracial: Asian/White Multiracial: Black-African American/White Multiracial: Other combination Declined Patient unavailable The Rationale for Granular Ethnicity Data Disparities exist within the OMB categories Differential pap screening rates among Asian subgroups even when insured Higher rates of childhood asthma and recent attacks among Puerto Rican than Mexican ethnic groups It is still important to use OMB race and Hispanic ethnicity categories Institute of Medicine, 2009 Granular Ethnicity - Mammography Source: University of California, Los Angeles, Center for Health Policy Research, California Health Interview Survey Mother’s ethnicity and cesarean rates all deliveries,* MA, 2004 10% 15% 20% 25% 30% 35% 40% 45% Brazilian 40% African 37% Haitian 35% Asian Indian 34% W. Indian/Caribean 32% European 32% Dominican 31% All Other 31% Oth Port 31% African Amer 30% Native Amer 28% Vietnamese 28% Other Asian 27% Middle Eastern 27% Oth Hispanic 27% Chinese 26% Puerto Rican 26% Oth Central Amer 25% Cape Verdean 25% Salvadoran 22% Cambodian 15% * A delivery of multiples is counted once Center for Health Information and Statistics, MDPH Variation in Breastfeeding Rates by Asian Ethnicity 91% Asian Indian Japanese Pakistani Korean Filipino Thai 71% MA TOTAL Chinese Vietnamese Laotian 35% Cambodian 0% 20% 40% 60% Source: Asian Births in Massachusetts: 1996-1999; Hispanic Births in Massachusetts: 1996-1999; and Black Births in Massachusetts: 1997-2000 80% 100% Definition of Granular Ethnicity Ancestry, which the Census Bureau defines as “a person’s ethnic origin or descent, ‘roots,’ or heritage, or the place of birth of the person or the person’s parents or ancestors before their arrival in the United States” is the ethnicity concept adopted by the subcommittee as the level of detail necessary for quality improvement Institute of Medicine, 2009 Granular Ethnicity Collect granular ethnicity data as a separate variable from the OMB race and Hispanic ethnicity categories Granular ethnicity categories should be selected from a national standard list Lists should include an “Other, please specify:__” option for additional selfidentification Institute of Medicine, 2009 Selecting Locally Relevant Granular Ethnicity Categories Local circumstances can dictate whether an entity uses 10 or 100 categories from the national standard list; criteria for selection: Health and health care quality issues Evidence or likelihood of disparities Size of subgroups within the population Analyses of relevant data on the service or study population Institute of Medicine, 2009 Further investigation needed to: •Examine different ways of framing the questions and response categories at the level of the OMB standards •Monitor implementation of granular ethnicity data collection to elicit “promising practices” Treating Patients with Limited English Proficiency 80% of hospitals encounter LEP patients frequently – 63% daily/weekly; 17% monthly 81% of general internal physicians treat LEP patients frequently – 54% at least once a day or a few times a week; 27% a few times per month 84% of FQHCs provide clinical services daily to LEP patients – 45% see more than ten patients a day; 39% see from one to 10 LEP patients a day. Collecting Data on Language Need Identify language need by determining: how well an individual believes he/she speaks English what language he/she needs for a health-related encounter Less than “very well” is defined as LEP Where possible, also could collect language spoken at home and language preferred for written materials IOM Recommendations for standardized collection of race, ethnicity, and language need Hispanic or Latino Not Hispanic or Latino OMB Race (Select one or more) Black or African American White Asian American Indian or Alaska Native Native Hawaiian or Other Pacific Islander Some other race Spoken English Language Proficiency Language Need Race and Ethnicity OMB Hispanic Ethnicity Very well Well Not well Not at all (Limited English proficiency is defined as “less than very well”) Granular Ethnicity Locally relevant choices from a national standard list of approximately 540 categories with CDC/HL7 codes “Other, please specify:___” response option Rollup to the OMB categories Spoken Language Preferred for Health Care Locally relevant choices from a national standard list of approximately 600 categories with coding to be determined “Other, please specify:__” response option Inclusion of sign language in spoken language needs list and Braille when written language is elicited ALL patients/enrollees should be asked about their race/ethnicity, and language Self-reporting is the most accurate source of information Self-reporting will increase consistent reporting within a health care institution Patients are more likely to select the same categories to describe themselves over time than staff who are assuming or guessing Systematic Implementation and Practical Concerns Conduct education and feedback sessions with leadership and staff Define issues and concerns and identify how you will respond to them Training and education components should include Policy context Revised policies New fields Screens Leadership-staff materials Staff scripts FAQs and potential answers Specific scenarios Staff questions Monitoring Two Approaches to Using Broad Categories National Health Plan Collaborative: Toolkit to Reduce Racial and Ethnic Disparities in Health Care Data Collection Methods National Health Plan Collaborative: Toolkit to Reduce Racial and Ethnic Disparities in Health Care Staff will feel more comfortable asking patients/enrollees these questions if: They understand How these data will be used What disparities are Why they occur Their vital role in identifying and addressing disparities and improving the quality of care for everyone Invest in Staff Training Palaniappan, LP et al. Health Services Research, October 2009. Hasnain-Wynia R, Taylor-Clark, Anise. Medical Care Research and Review. October 2010 What will change? Standardizing Direct Data Collection Who: information should always be asked of patients or their caretakers and should never be gathered by observation alone When: information should be collected upon admission or patient registration to ensure that appropriate fields are completed when the patient begins treatment or for plans, when the individual enrolls (as permitted by state law) What: Questions about the OMB race and Hispanic ethnicity categories (one- or twoquestion format permitted) A question about granular ethnicity with locally relevant response categories selected from a national standard set A question to determine English-language proficiency A question about language preference needed for effective communication. Where: data should be stored in a standard format for easy linking to clinical data How: patient concerns should be addressed when the information is being obtained, and staff should receive ongoing training and evaluation. How Organizations Can Use the Data to Improve Care Gain knowledge about the patient/enrollee population served Identify populations at increased risk of adverse outcomes Strengthen your organizations ability to develop culturally appropriate materials to improve care Track progress toward providing equitable care Stratify distribution, utilization, process, outcome and patient experiences with care measures Improve outreach to local communities Develop better data necessary for P4P and other programs Weinick R, Flaherty K, Bristol S. Creating Equity Reports, 2008. Wynia, Ivey, Hasnain-Wynia,. Collection of data on patients’ race and ethnic group by physician practices. New England Journal of Medicine, 2010; 362:846-50 •Ensure patients from different backgrounds get proper care •Devise campaigns that tailor treatment and counseling to patient ethnicities •Tactics include -Multilingual hand-outs -On-site cooking lessons -Culturally relevant discussion of portion sizes -Tracking patients in electronic data systems to target health tips and patient education materials Effective Communication with Diverse Populations as a Target for QI Multi-stakeholder consensus report Established specific measurable expectations for organizational performance – including data collection To guide quality improvement in patient-centered communication Focuses on needs of diverse populations Available at: www.EthicalForce.org Using Assessments of Race/Ethnicity/Language of Populations for Within-Institution QI To monitor quality of care for all groups To design innovative programs to eliminate disparities and rigorously test them To know patients, better meet their needs, and work with the community to deliver the best care possible To satisfy legal, regulatory and accreditation requirements (e.g., Joint Commission, CMS, NCQA State Mandates, etc.) To take the leadership position in eliminating health care disparities and providing patient-centered care Place-Based Disparities Exist: Use Data to Make a Case for Resources Disparities are multi-factorial—who you are and where you go Continued segregation in health care Under-resourced institutions serve minority communities Focus incentives toward institutions serving a large % of minority patients. Target resources to areas of greatest impact Implications for Research Currently race/ethnicity data are on a sandy foundation—implementing standardized collection methods and categories will strengthen and solidify the foundation—more confidence in the data and in the ability to draw conclusions. Improving collection methods Using national data sets for disparities research Direct methods: how to collect race/ethnicity data and what categories to use (both by providers and through surveys for research purposes) Indirect methods (e.g., geocoding, surname recognition): specify when these approaches are applicable and when they are not Opportunities to link national databases and to conduct regional surveys including over-sampling for racial/ethnic minorities. Improving the availability and utility of patient-level administrative data for disparities research Ensure privacy and confidentiality and address sample size challenges by pooling data Thank You! r-hasnainwynia@northwestern.edu www.iom.edu/datastandardization/ Discussion Questions for our speaker can be submitted now. Click on “Ask a Question” below this presentation. Complete the form and click “Submit.” Methods Session: Register Today! Community Based Participatory Research: Strategies for Reducing Health Disparities Date: Wednesday, December 8, 2010 - 1:00 - 2:30pm (Eastern) Faculty: Nina Wallerstein, Dr.P.H. and Lorenda Belone, Ph.D., Robert Wood Johnson Foundation Center for Health Policy at the University of New Mexico; Kevin R. Shendo, Director of Education, Pueblo of Jemez Visit www.academyhealth.org/training for more information. Thank You! Please take a moment to fill out the online evaluation.